Growth & Development

Objectives
•
To understand the related definitions,
Nutrition
for Health &Development, Malnutrition & Infection
,
prognosis, etiology.
•
To memorize the protein energy malnutrition;
its types;(marasmas & kwashiorkor) ,
indicators, prevention & control

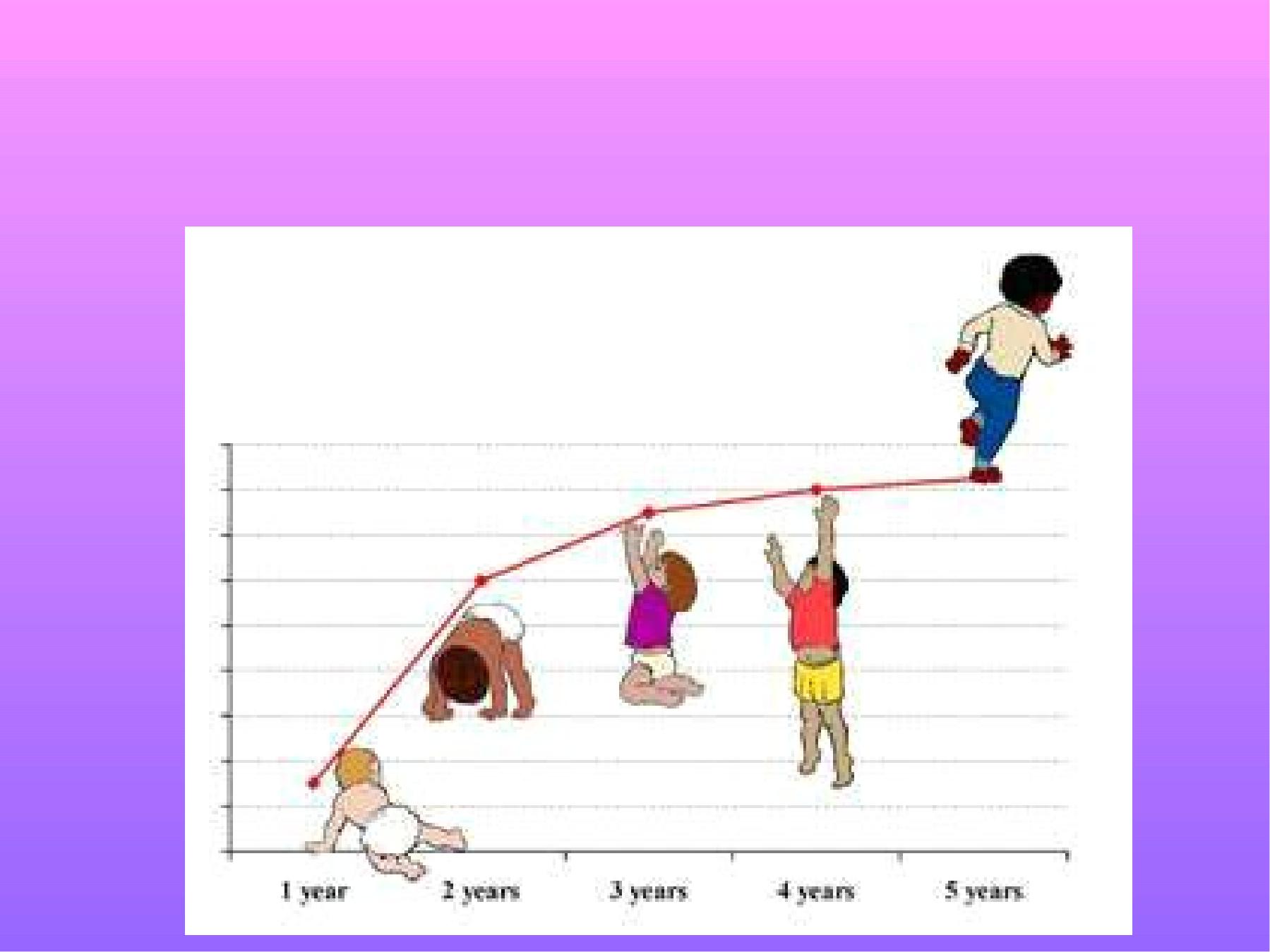
Growth &development
Childhood is a time of active growth in terms of
physical size, mental, emotional, sexual
maturation and psychological development.
Normal growth is dependent on adequate
nutrition.
Human body can use carbohydrates, fat,
proteins as a source of energy.
When the intake of energy is not optimum, this
can lead to malnutrition in the long run.

Malnutrition is associated with poor
developmental achievement, poor school
performance and malnourished children face
long -term sequels such as impairment of
mental and intellectual capacity.
WHO estimates that 175 million children in the
developing world are malnourished as
indicated by low weight for age and 230 million
are stunted as indicated by height for age.
It is recognized that the vast majority of deaths
among children in the developing world is
associated with malnutrition.
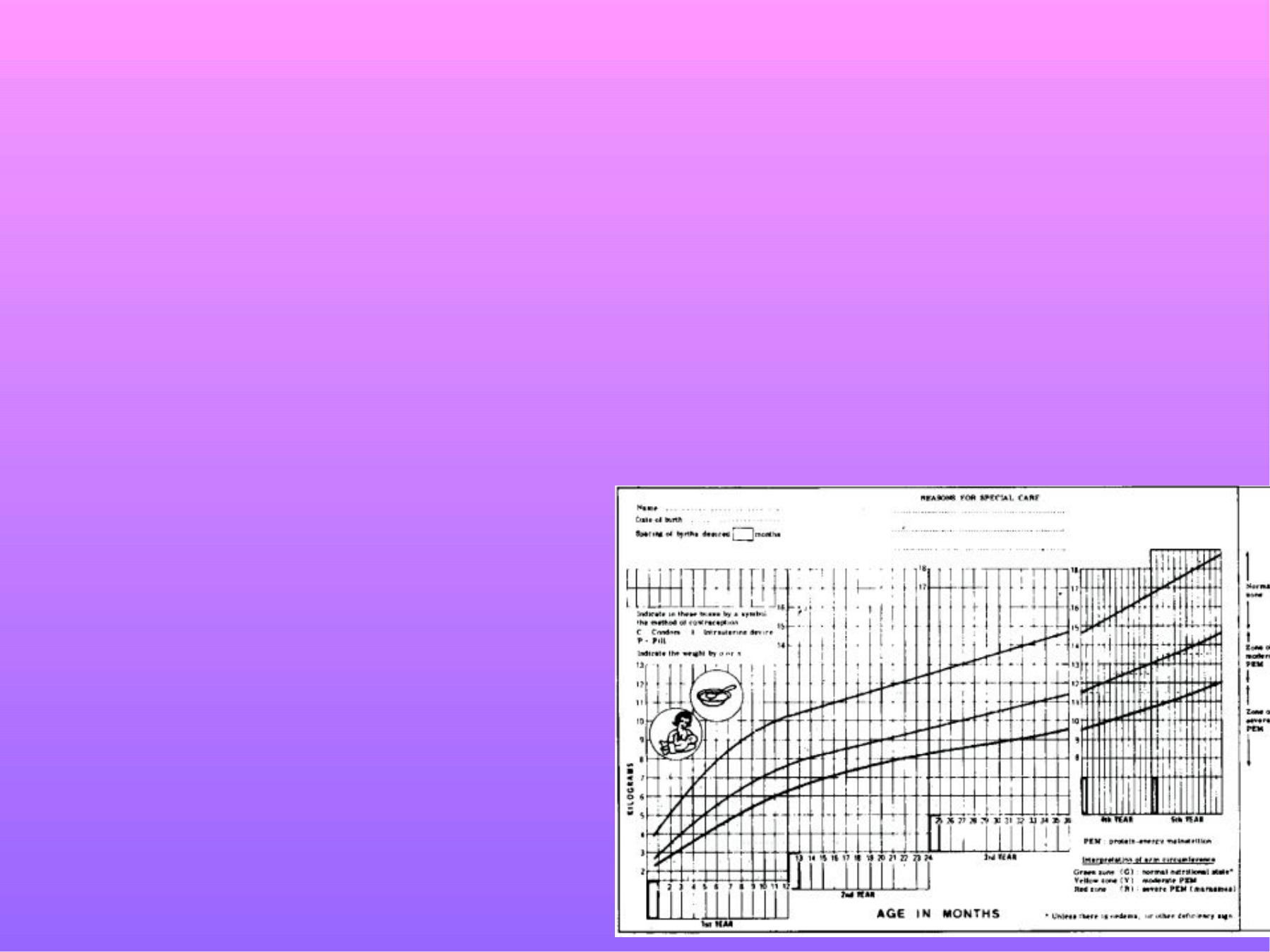
Growth monitoring
Using growth standards for two purposes;
1-Identifies and classifies malnourished
children& early detect those at risk for becoming
malnourished, and those who need special
intervention and referral for management of
severe malnutrition.
2- It provides an
opportunity to educate&
motivate individuals,
specifically mothers&
caretakers.

for improving their understanding about feeding
and caring practices in order to enhance the
child’
s health and nutritional status.
The advantage of growth monitoring is that it has
made the issue of child malnutrition
visible
,
treatable
and
disappearance
of severe
malnutrition in many countries.
Monitoring the growth of infants and young
children becomes critical as malnutrition
is often not recognized by the mother until
it has become severe and then reversing
the condition becomes expensive and often
difficult.

Nutrition for Health &Development
Nutrition is a foundation for health&
development.
Interaction of infection& malnutrition is well-
documented.
Better nutrition means stronger immune systems,
less illness & better health.
Healthy children learn better. Healthy people are
stronger, are more productive and more able to
create opportunities to gradually break the
cycles of both poverty and hunger in a
sustainable way. Better nutrition is a prime
entry point to ending poverty and a milestone to
achieving better quality of life.

Malnutrition:
Definition: pathological state resulting from
relative or absolute deficiency or excess of
essential nutrients.
This could be detected by; biochemical,
physiological tests, clinical manifestations, or
anthropometric measurements.
Malnutrition & Infection
Depression of nutritional status will intensify the
risk of infection in term of course& severity.
In under nourished person when infected, this
intensify the malnutrition, (repeated infection
leads to progressive nutritional depletion).
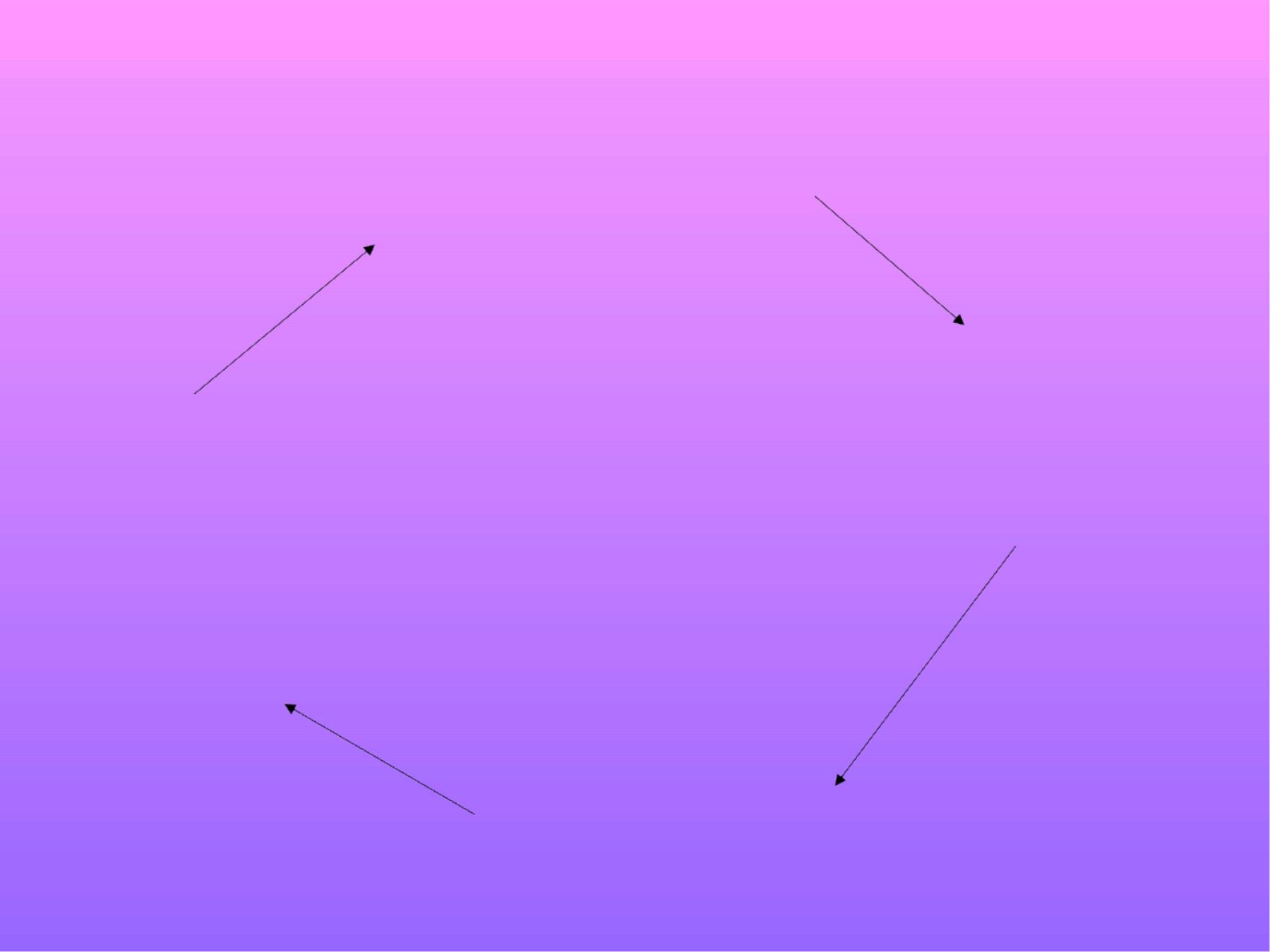
The Malnutrition-Infection Cycle
Inadequate intake
Weight loss
Mucosal damage
Anorexia
Malabsorption
Immune deficiency
Incr. Nutrient losses
Incr. Nutrient requirements
Susceptibility
to infection

Protein Energy Malnutrition:
PEM: is a spectrum of clinical disorders caused
by various degrees of deficiency & additional
physiological insults & stress.
It is considered as Silent emergency of the
world,& it is most important nutritional
problem in most of the developing countries,
it cause permanent disabilities because most
of brain growth occur in early years of life with
decrease resistance to infection.
In children PEM may result in wasting, stunting,
underweight.

Types of malnutrition:
1-Under nutrition: result from consumption of
inadequate quantity of food over an extended period
of time, e.g. marasmus, &kwashiorkor.
2-Over nutrition: result from consumption of excessive
quantity of food (excessive caloric intake) over an
extended period of time, e.g. obesity.
3-Specific deficiency: result from relative or absolute
lack of an individual nutrient, e.g.
Vit. A deficiency, iron deficiency anemia---- .
4-Nutritional imbalance: result from disproportion
among essential nutrients with or without absolute
deficiency of any nutrient as determined by
requirement of balanced diet.

Indicators of malnutrition:
•
Low wt. for ht. = wasting= acute malnutrition
(wt./ht.< -2SD of the reference table).
It is most easily reversed &treated but often
recurs due to infection. Prevalence of wasting in
Iraq for <5y. children =9.3% (Unicef survey).
•
Low ht. for age= stunting= chronic malnut.
(ht./age below-2SD of the ref. table).
Difficult to reverse in child after 2-3y old.
Prevalence of stunting in Iraq for<5y.children=
20.4%

•
Low wt. for age= under wt.= general
malnutrition (wt. /age below-2SD of the ref.
table).
Prevalence of underweight in Iraq for <5y.
children =21.3%.
PEM has been categorized according to the
severity; severe, moderate or mild type.
Severe PEM may presented as:
marasmus, Kwashiorkor, marasmic-
Kwashiorkor
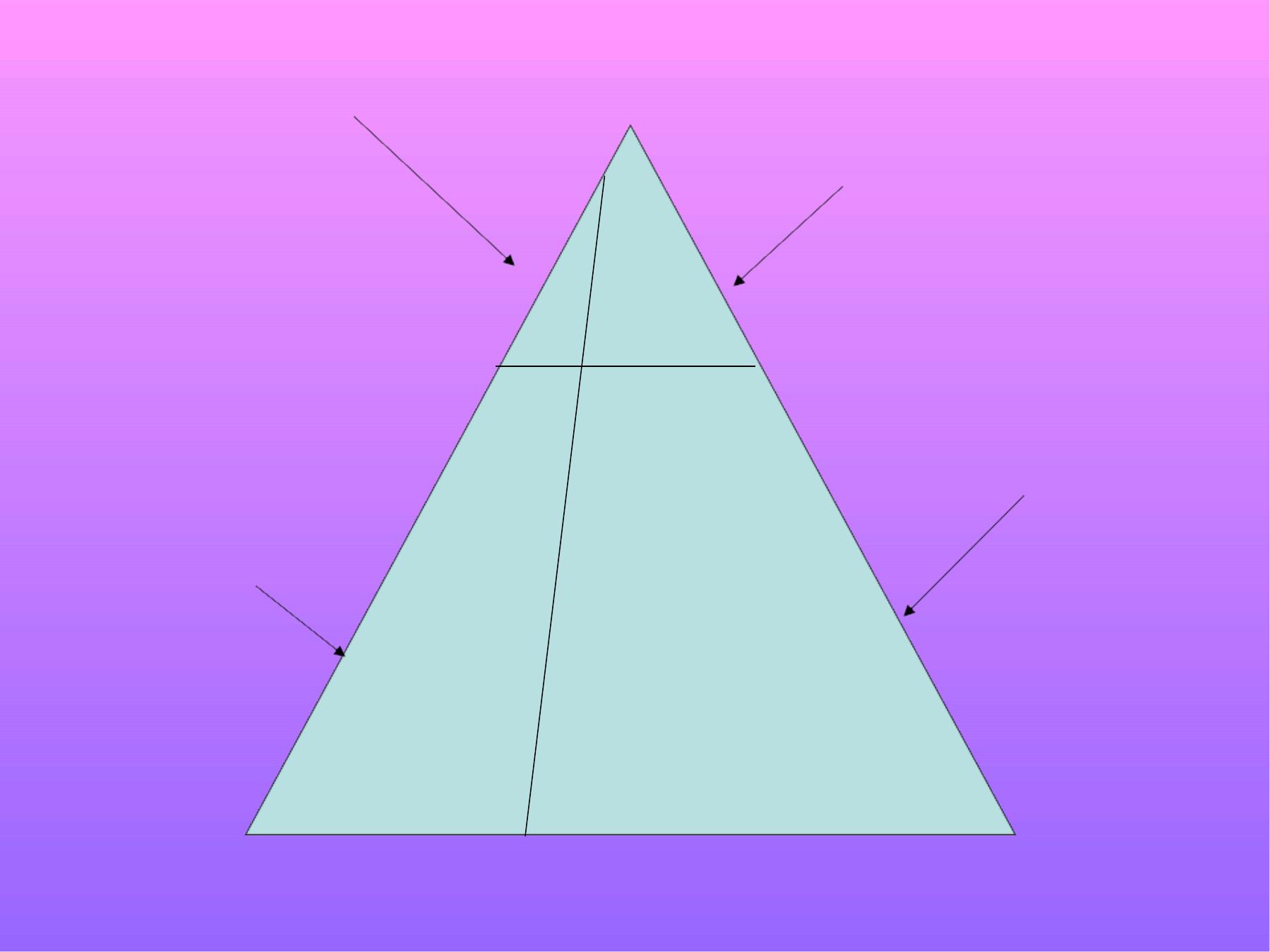
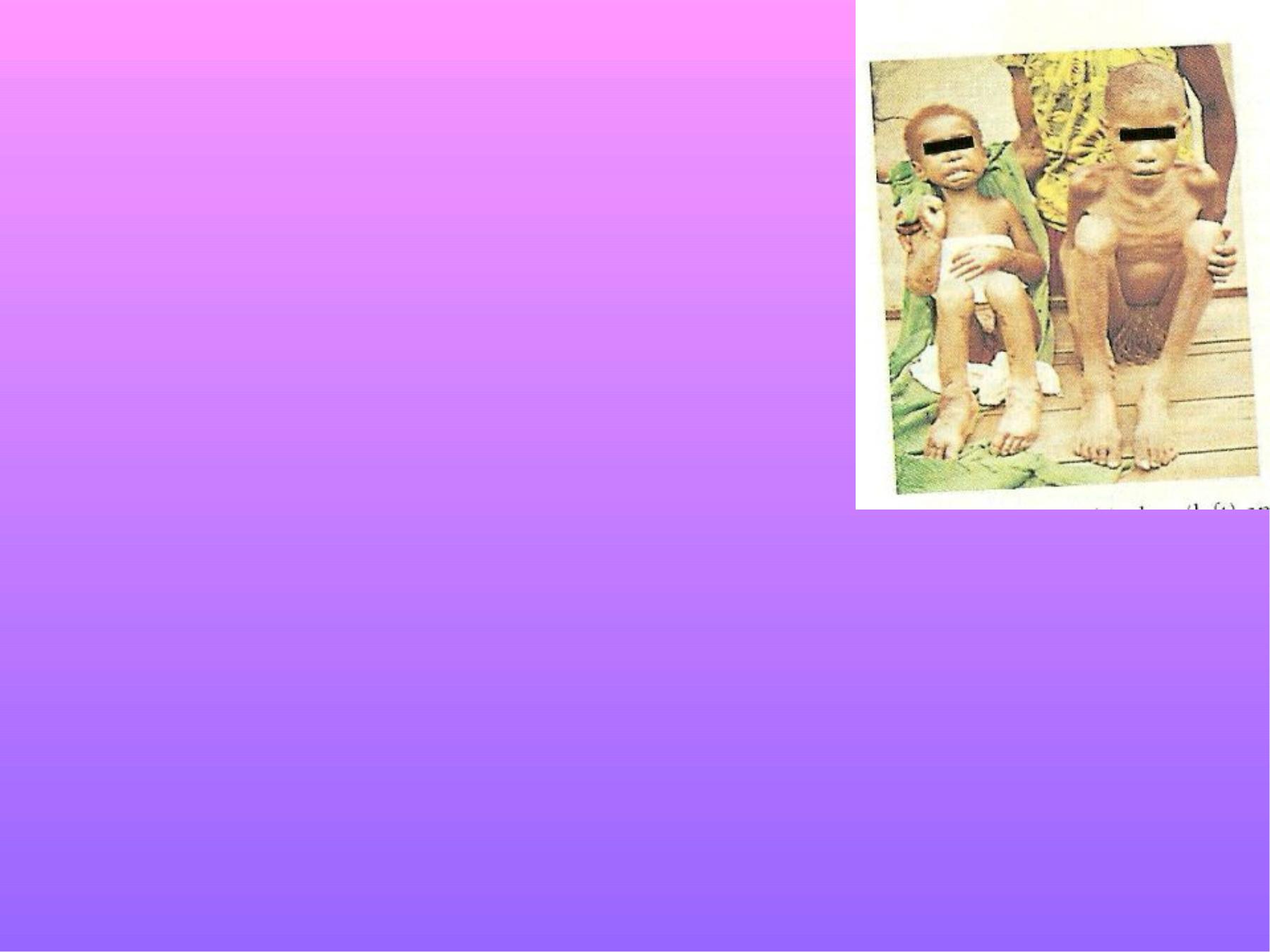
Kwashiorkor
Marasmus
&severe PEM
Pre-kwashiorkor
Under wt.
&low plasma
albumin
Ice burg phenomenon

Nutritional Marasmus:
•
Child age: usually <1 year.
•
Wt/age:<-3SD below reference
wt./age table = small for his age.
•
Wasting of the muscles &
subcutaneous fat (leads to hypotonia & wrinkled
skin).
•
Diminish ht./age.
•
Looks emaciated (skin & bone)= absence of
adipose t.

•
Abdomen distended or flat.
•
Edema is not noticeable.
•
Subnormal body temp., slow pulse rate, with
reduced BMR.
•
Constipation usually but s.t. starvation
diarrhea ( frequent small B.M. with mucus).
•
Retarded Bone age.

Kwashiorkor:
•
Severe PEM caused by severe
protein deficiency.
•
Early clinical finding are not
specific (apathy, lethargy, irritability).
•
Age usually >1y.
•
Wt./age: normal to -2SD
•
Edema (non pitting), plump appearance,
round cheeks & belly, because of low protein
& inadequate water balance.
•
Retarded growth.
•
Loss of muscle tissues &loss of muscle tone.
•
Anorexia.

•
Dermatitis, darkening of skin in irritated
areas, dyspigmentation may occur in these
areas, ulceration &skin fissures.
•
Loss of hair elasticity, thin, dyspigmented,
streak, red or grey in color.
•
Mental changes, irritability& restlessness.
•
Loose stool is common( diarrhea).
•
Liver enlargement (fatty infiltration, reduce of
fat mobilization due to decr. Lipoprotein
synthesis).
•
Growth failure.
•
Moderate anemia.
•
Retarded bone age.
•
Low plasma protein&
albumin.
Marasmus-Kwashiorkor:
•
Present with clinical findings of both
marasmus & kwashiorkor.
•
Edema.
•
Gross wasting.
•
Mild hair &skin changes.

Prognosis of severe PEM
:
-
Mortality rate 10-60%.
-Case fatality rate depend on many factors;
associated infection, other concomitant
nutritional deficiencies, delay in seeking
treatment, seriousness of the child condition at
time of admission.
Mild &Moderate PEM:
Mild PEM: wt. between -1 to -2SD below the
reference wt./ age.

Moderate PEM: wt. < -2 to-3SD below the
reference wt./ age.
These children usually misdiagnosed unless
their growth has been monitored.
Etiology of PEM:
I-Immediate causes;
Diseases, inadequate dietary intake.

II-Underlying causes;
A-Insufficient food intake.
1.Low energy &protein (essential a.a.) staple diet.
2.Poor lactation (no breast feeding).
3.Inappropriate use of infant formula(over dilution).
4.Inappropriate weaning practices.
5.Mal-distribution of the food within the family.
6.Lack of food.
7.Ignorance.
8.Inadequate care (social factors).

B-Inadequate maternal &child care practices;
1.Maternal malnutrition.
2.LBW, prematurity, multiple pregnancy.
3.Large family size,
4.Short birth interval.
5. No immunization.
6. No growth monitoring.
C-Insufficient health services& unhealthy
environment;
1.No safe water.
2.Unhealthy environment.

3.Unavailability of drugs.
4.H. services (availability, accessibility,
acceptability).
III-Basic causes:
1. Poverty
2.Wars
3. Economic structure
4.Political

Prevention& control of PEM
1.Encourage breast feeding.
2.Adequate complementary feedings.
3.Extra meal & good feeding for sick child.
4.Health education &nutritional education.
5.When there is inadequate amount of animal
milk, select a good mixture of available plant
protein (protein complementarity).
6.Prevention & control of infection (immunization,
H. education, proper use of antibiotics).
7. Socioeconomic improvement & better food
distribution.

8.Growth monitoring (early detection of growth
faltering).
9.Adequate maternal &child care (MCH) services.
10.Provision of safe water &good environmental
sanitation.
11.At home, proper management of food budget.
12.Improvement of food basket.
13.Community participation for early diagnosis;
(community care centers).
14.Good health services through PHC, Nutritional
Rehabilitation Centers in pediatric unites.
15.Good food & agricultural policies.
