
Hirsutism and virilism
DR Shaimaa Kadhim Al-Khafajy

• Hirsutism is defined as the excessive growth of
thick dark hair in an androgen-dependent
pattern where hair growth in women is usually
minimal or absent - eg, the face, chest, and
areolae. It occurs as a result of increased
androgen production, increased skin
sensitivity to androgens, or both.
• Idiopathic hirsutism and
causes.
When hirsutism in women is
accompanied by other signs of virilism, it may
be a manifestation of a more serious
underlying disorder causing
hyperandrogenism, such as an ovarian tumour
or adrenal neoplasm.

•
Normal hair growth : human hair grows in three phases :
•
1. Anagen : growing phase , lasts for several months to 2-
5 years on the scalp .
•
2. Catagen : follows anagen and lasts for about 2 weeks ;
during this period the hair stops growing and the lower
portion of the hair follicles involutes .
•
3. Telogen : resting phase that lasts about 3 months .
Epidemiology
•
• Hirsutism is a common disorder affecting between 5%
and 15% of women of reproductive age.
• It is less common in Asian people.
• There is racial variation in amount of terminal body
hair.
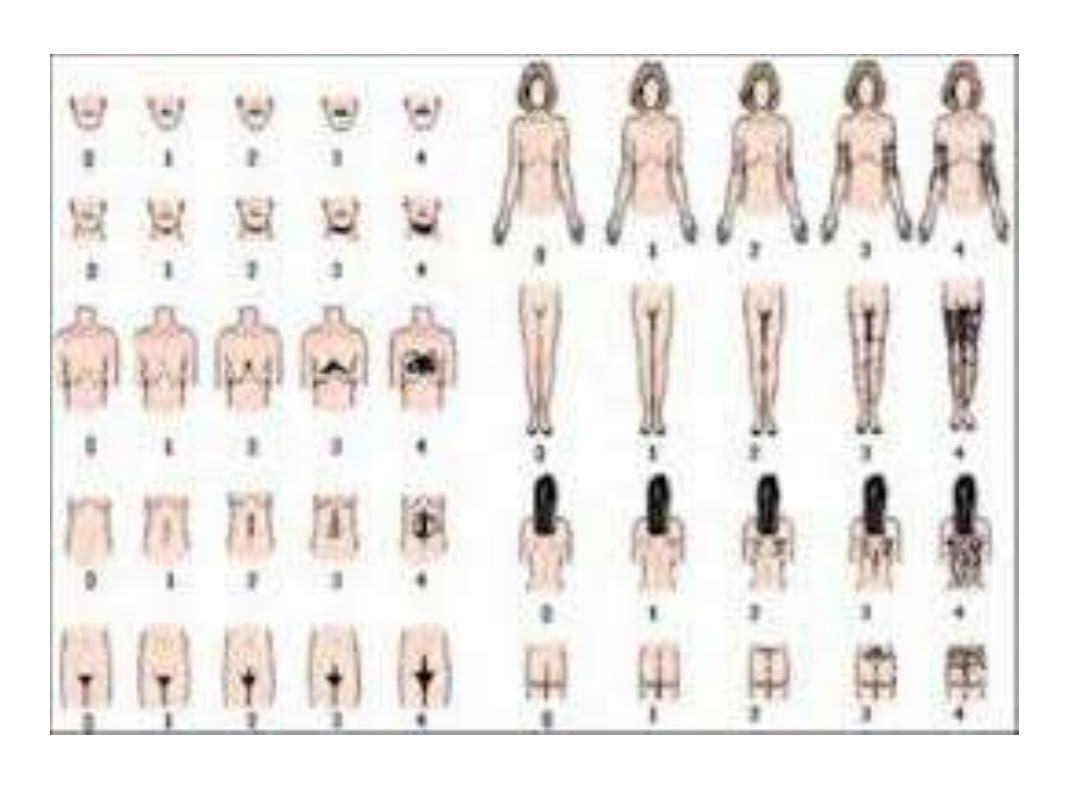
• The Ferriman-Gallwey score is used in evaluation of
hirsutism, and reflects the amount of hair over
different body areas. This may require adjustment for
racial variation.
•

* Pathogenesis : The dermal papillas androgen
receptors interact with dihydrotestosterone ,
the active metabolite of testosterone , this
interaction results in an increase in the size of
the hair follicle and the type of hair produced by
the follicle .



Causes of hirsutism
• Idiopathic hirsutism:
– Common and often familial.
– Is a diagnosis of exclusion and thought to be
related to disorders in peripheral androgen
activity.
– Onset occurs shortly after puberty with slow
progression.
– There are no other signs of virilism, and menstrual
function and investigations are normal.
• Drug-induced hirsutism - eg, anabolic steroids,
danazol, minoxidil, metoclopramide, methyldopa,
phenothiazines and progestogens.
• Ovarian causes:
–
: virilisation is minimal, and hirsutism is often
prominent. This is the most common cause and is
present in approximately 70% of cases.
–
Menopause.
– Androgen-producing ovarian tumours - eg, luteoma of
pregnancy, arrhenoblastomas, Leydig cell tumours,
hilar cell tumours, thecal cell tumours.
• Adrenal causes:
– Androgen-producing adrenal tumour.
–
Congenital adrenal hyperplasia (CAH)
–
• Other causes include severe insulin resistance,
anorexia nervosa, prolactinoma, acromegaly,
hypothyroidism and porphyria.

• Presentation
• Excess terminal hair in a masculine pattern:
face (particularly the moustache, beard and
temple areas), chest, areolae, linea alba,
upper and lower back, buttocks, inner thighs,
external genitalia.

Virilism
• Signs of associated virilism (hyperandrogenism) may be present,
and include:
– Acne
– Alopecia, temporal hair recession
– Male-pattern (truncal) obesity
– Clitoromegaly
– Deepening of voice
– Increased libido
– Increased muscle mass (primarily shoulder girdle)
– Loss of breast tissue or normal female body contour
– Malodorous perspiration
– Infertility
– Menstrual dysfunction
•

Differential diagnosis
• Hypertrichosis: this is androgen-independent
and causes uniform growth of vellus hair over
the body, especially in non-sexual areas. The
aetiology of hypertrichosis includes:
1-Familial.
2-Related to drugs - eg, phenytoin, ciclosporin or
topical steroids.
3-Non-endocrine causes such as anorexia
nervosa.

Management
• It is important to investigate to establish the
cause of hirsutism, even when mild, as the
degree of hirsutism does not correlate well
with the magnitude of androgen
excess. However, the first stage is careful
history and examination, and if there is no
suggestion of hyperandrogenism, full
endocrine evaluation may not be required

• History
• Age of onset, rate of progression.
• Menstrual history, age of menarche.
• Medication including over-the-counter
preparations and anabolic steroids.
• Family history of hirsutism.
• Level of distress caused by hirsutism
• Examination
• For signs of hyperandrogenism.
• For signs of
stretch marks, easy bruising, proximal muscle
weakness).
• To exclude pelvic masses.
• Blood pressure.
• BMI.

• Initial investigations
These include:
• Testosterone:
– A high total testosterone concentration indicates
that hyperandrogenaemia may be caused by an
ovarian or adrenal tumour.
– If the total testosterone is normal or only slightly
raised, an androgen-secreting tumour can be
excluded.

– Free testosterone is more sensitive and may be
raised in PCOS.
– Testosterone concentrations more than 1.5-2
times the upper limit of normal or a history of
rapid virilisation are likely to be associated with
tumour-associated hyperandrogenism.
– Dehydroepiandrosterone sulfate and
androstenedione should then be measured to
identify an adrenal or ovarian source of the
hyperandrogenaemia.

• Free androgen index:
– Total testosterone is often normal in PCOS but the
free androgen index is raised because sex
hormone-binding globulin is suppressed.
– The free androgen index is calculated by also
measuring sex hormone-binding globulin (free
androgen index is total testosterone concentration
divided by sex hormone-binding globulin
concentration multiplied by 100).

• Follicle stimulating hormone (FSH), luteinising hormone
(LH): Women with PCOS may have an increased LH/FSH
ratio (>2 is common).
• 17-hydroxyprogesterone:
– Blood should be taken at about 9 am in the first half of the
menstrual cycle.
– A 17-hydroxyprogesterone value of 5 nmol/L has a sensitivity of
100% and specificity of 88.6% for diagnosing non-classical CAH.
• 24-hour urine cortisol (to rule out Cushing's syndrome if
suspected):
– Cushing's syndrome is a rare cause of hirsutism and exclusion is
not necessary unless the patient has Cushingoid features.

• Pregnancy should be ruled out in women with
irregular or absent menstrual cycles.
• Prolactin:
• Prolactin affects the menstrual cycle and
hyperprolactinaemia can be associated with
hirsutism.

• TFTs: thyroid dysfunction can affect
menstruation and hypothyroidism is
associated with changes in hair.
• Ultrasound: patients with either menstrual
disturbances or clinical or biochemical
evidence of hyperandrogenism alone should
have transvaginal ultrasound imaging of the
ovaries.

• Further investigations as indicated:
– Glucose tolerance test with serial growth
hormone measurements if
suspected.
– Lipid profile.
– HbA1c.
– Ultrasound, CT, MRI: if an adrenal or ovarian
tumour is suspected. MRI brain scan: if a pituitary
tumour is suspected.
TREATMENT
• Treatment for hirsutism is unnecessary if no
abnormal aetiology can be diagnosed and if
the patient is not concerned about the
cosmetic appearance. Management is mainly
directed at any underlying cause if present.

• Lifestyle modification:
– Encourage weight loss if overweight:
• Weight loss increases steroid hormone-binding globulin levels
and decreases insulin resistance and the levels of serum
androgens and luteinising hormones.
• Obesity has an adverse effect on the outcome of all systemic
treatments.

– Women who are overweight, hyperandrogenic or
hyperinsulinaemic are at increased risk of diabetes
mellitus and cardiovascular disease.
– Smoking cessation advice.
• Because of the cyclical nature of hair growth, any
systemic treatment may take up to six months to
be effective.
• Treatment of hirsutism is not usually curative,
unless a treatable underlying cause has been
found.

• Topical cosmetic therapies
• Shaving, threading, waxing, using depilatory
creams, electrolysis and laser epilation or
photo-epilation do not exacerbate hair growth
and are effective, at least in the short-term
• Bleaching.
• Shaving: Removes all hairs superficially but
regrowth produces a rough stubble. Most
women prefer not to shave facial hair.
• Chemical depilation may be suited to
treatment of large hairy areas in patients
unable to afford more expensive treatments
such as electrolysis and laser epilation.
• Temporary epilation:
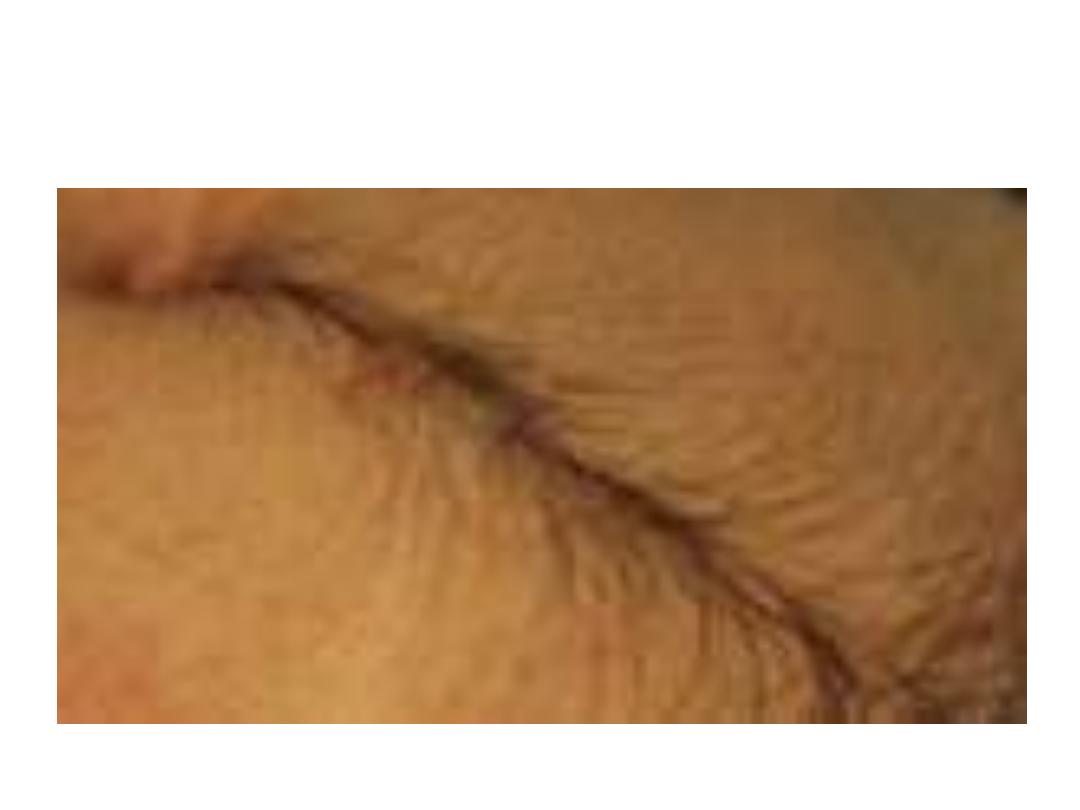
– Plucking: this may result in irritation, damage to
the hair follicle, folliculitis, hyperpigmentation,
and scarring.
– Waxing: this can be painful and sometimes results
in folliculitis. With repeated treatments it may
reduce the number of hairs permanently.
– Home epilating devices that remove hair by
rotation or friction: these may produce traumatic
folliculitis.

• Permanent epilation:
– Electrolysis and thermolysis:
• Thermolysis (diathermy) is much faster than the traditional
electrolysis method.
• Electrolysis and thermolysis can be used on all skin and hair
colours, but they require multiple treatments.
• Results depend on the skill of the operator.
• Electrolysis and thermolysis can be
uncomfortable and may produce folliculitis and
post-inflammatory pigmentary changes in the
skin

– Laser epilation:
• Can treat larger areas faster than electrolysis and
thermolysis.
• Is most effective on dark hairs in fair-skinned people.
• Multiple treatments may be necessary for long-term
hair destruction.
• Folliculitis, discomfort and pigmentary
changes may occur

• Drug therapy
• The following drugs are effective: finasteride,
oral contraceptive pills, thiazolidinediones,
cyproterone acetate and ethinylestradiol in
combination, spironolactone, and
flutamide. However, a systematic review of
trials of insulin sensitisers concluded that this
group of drugs is of limited use as sole
treatment for hirsutism

• Combined oral contraceptives:
– Recommended as first-line treatment.
– Pills containing progestogens with anti-androgenic
properties (eg, Co-cyprindiol (Dianette®) or
Yasmin®) are effective but those containing
levonorgestrel and norethisterone are more
androgenic and could potentially exacerbate
hirsutism.

• Third-generation progestogens (eg, desogestrel or
gestodene) have relatively neutral androgenic effects
and oral contraceptives containing these
progestogens can be combined with an anti-
androgen such as spironolactone.

• Anti-androgens:
– Flutamide, finasteride and spironolactone have all
been found to be effective in the management of
hirsutism.
– May be combined with oral contraceptives for the
treatment of hirsutism.
– Cannot be used in pregnancy, and should be
prescribed with secure contraception.
– May be associated with side-effects.

• Gonadotrophin-releasing hormone (Gn-RH)
agonists:
– For severe cases, these are occasionally used in
secondary care.
– Gn-RH agonists such as leuprorelin should be
reserved for use in women who do not respond to
combination hormonal therapy or those who
cannot tolerate oral contraceptives.
– Long-term adverse effects include hot flushes,
bone demineralisation, atrophic vaginitis.

• Metformin has been shown to improve insulin
sensitivity and decrease testosterone levels in
patients with PCOS but the evidence is
currently against it being effective for
hirsutism alone.

• Eflornithine, a topical hair growth retardant,
inhibits the enzyme ornithine decarboxylase.
It may reversibly slow facial hair growth in up
to 70% of patients:
– It must be used indefinitely to prevent regrowth.
– It is only licensed for facial hair.
– Continuous use for eight weeks is required before
benefit is seen.
– It should be discontinued in the absence of
improvement after treatment for four months.




