Opportunistic Mycoses
Infections due to fungi of low
virulence in patients who are
immunologically compromised
Medical Mycology Iceberg
PATHOGENIC FUNGI
•
NORMAL HOST
•
Systemic pathogens
- 25 species
•
Cutaneous pathogens
- 33 species
•
Subcutaneous pathogens - 10 species
•
IMMUNOCOMPROMISED HOST
Opportunistic fungi
- 300 species
HOST-PATHOGEN EQUILIBRIUM
NUMBER OF ORGANISMS X VIRULENCE
=
DISEASE
HOST RESISTANCE
Opportunistic Fungi
1. Saprophytic - from the environment
2. Endogenous – a commensal organism
Opportunistic Fungi
Include many species from:
A (Aspergillus)
To
Z (Zygomyces)

MOST SERIOUS
OPPORTUNISTIC INFECTIONS
• CANDIDA SPECIES
• ASPERGILLUS SPECIES
• MUCOR SPECIES (ZYGOMYCES)
Upward Trend In
Opportunistic Mycoses
1. Increased clinical awareness
2. Improved clinical diagnostic tools
3. Improved laboratory diagnostic technics
4. An increase in susceptible hosts.
5. More invasive diagnostic and therapeutic
procedures
Must distinguish between
1. Transient fungemia
2. Colonization
3. Infection
Transient fungemia
The fortuitous isolation of a commensal or
environmental organism
EYE
SKIN
UROGENITAL TRACT
ANUS
MOUTH
RESPIRATORY
TRACT
COLONIZATION
Multiplication
of an organism
at a given site
without harm
to the host
EYE
SKIN
UROGENITAL TRACT
ANUS
MOUTH
RESPIRATORY
TRACT
INFECTION
Invasion and
multiplication
of organisms
in body tissue
resulting in
local cellular
injury.
Predisposing Factors
Malignancies
• Leukemias
• Lymphomas
• Hodgkins Disease
Predisposing Factors
Drug therapies
• Anti-neoplastics
• Steroids
• Immunosuppressive drugs
Predisposing Factors
Antibiotics
Over-use or inappropriate use of
antibiotics alter the normal flora
allowing fungal overgrowth
Predisposing Factors
Therapeutic procedures
• Solid organ or bone marrow transplant
• Open heart surgery
• Indwelling catheters
• Artificial heart valves
• Radiation therapy
Predisposing Factors
Other Factors
• Severe burns
• Diabetes
• Tuberculosis
• IV Drug use

CD4 helper T cells are the basis of cell
mediated immunity and play a role in host
defenses against fungal diseases
ERGO

Virtually all AIDS patients will have a fungal
infection sometime during the course of
their illness
• Direct Microscopical Examination:
• 1. Wet Mount by KOH (10-20%): Skin scrapings
suspected to contain dermatophytes or pus from a
lesion can be mounted in KOH on a slide and
examined directly under the microscope.
• 2. Gram Stain: Fungi are Gram positive reaction.
• 3. India ink Stain (Negative Stain): To
demonstrate the capsule of Cryptococcus.
• Culture on sabroud agar in20C and 37C
• Serological and molecular Dx as PCR
Diagnosis of opportunistic
infections requires a
high index of suspicion
1.
Atypical signs or symptoms
2.
Unusual organ affinity
3.
Outside the endemic area
4.
Unusual Histopathology
5.
Etiologic agent may be a saprophyte

CLINICAL PRESENTATION
1. Atypical Signs and Symptoms
2. Unusual Organ Affinity
3. Outside Endemic Area
4. Unusual histopathology
5. Unusual Pathogens
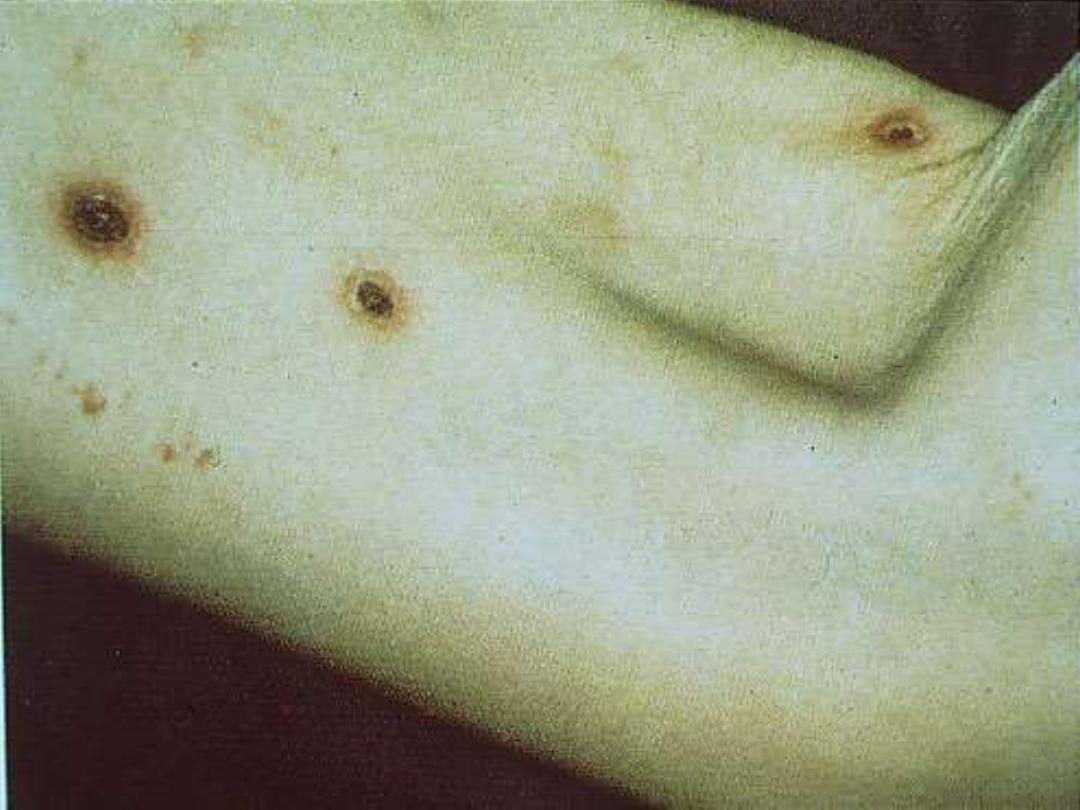
NORMAL PATIENT
Malasezzia furfur
Tinea versicolor
(mild disease)

COMPROMISED PATIENTS
Malasezzia furfur can cause disseminated
infection--------Particularly in patients
receiving hyperalimentation.
COMPROMISED IMMUNE
SYSTEM
Malasezzia furfur
NUMBER OF ORGANISMS x LOW VIRULENCE
=
DISEASE
HOST RESISTANCE

CLINICAL PRESENTATION
1. Atypical Signs and Symptoms
2. Unusual Organ Affinity
3. Outside Endemic Area
4. Unusual histopathology
5. Unusual Pathogens

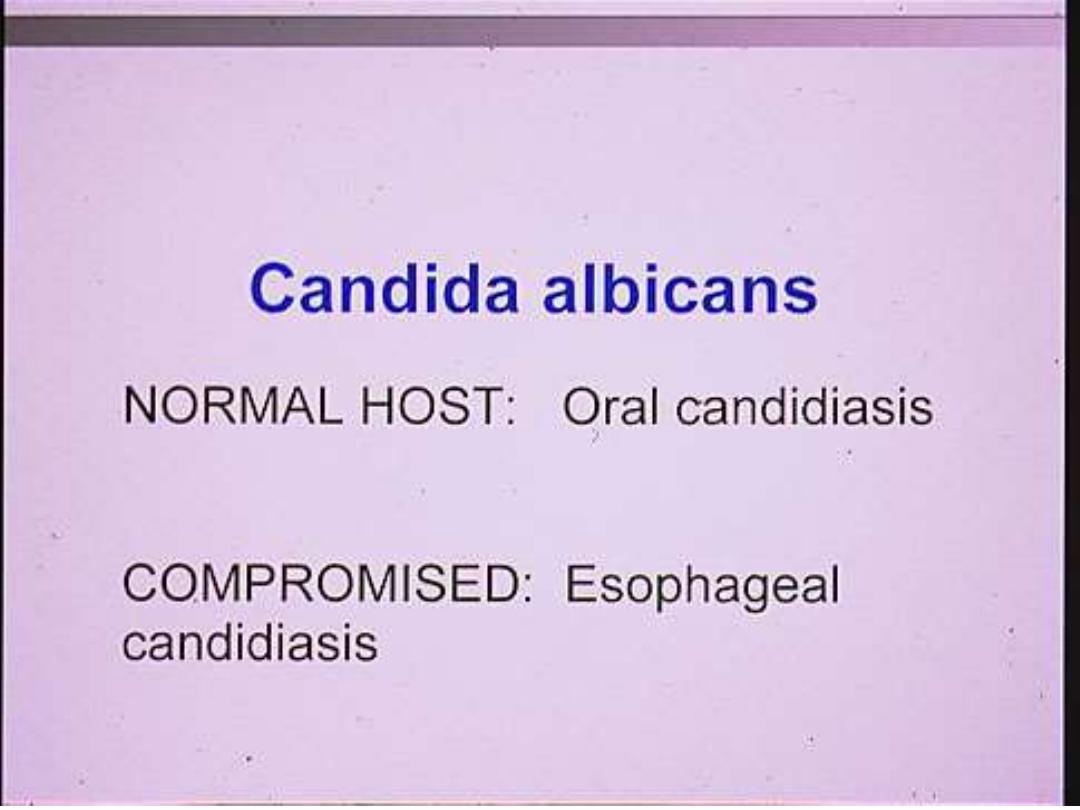
Candida species
Endogenous
Normal Flora
The population of microorganisms that may
be found residing in or on the human body
without causing disease.

COMPETENT IMMUNE
SYSTEM
Candida albicans
NUMBER OF ORGANISMS x VIRULENCE
=
NO DISEASE
HOST RESISTANCE
COMPROMISED IMMUNE
SYSTEM
Candida albicans
NUMBER OF ORGANISMS =
DISEASE
HOST RESISTANCE


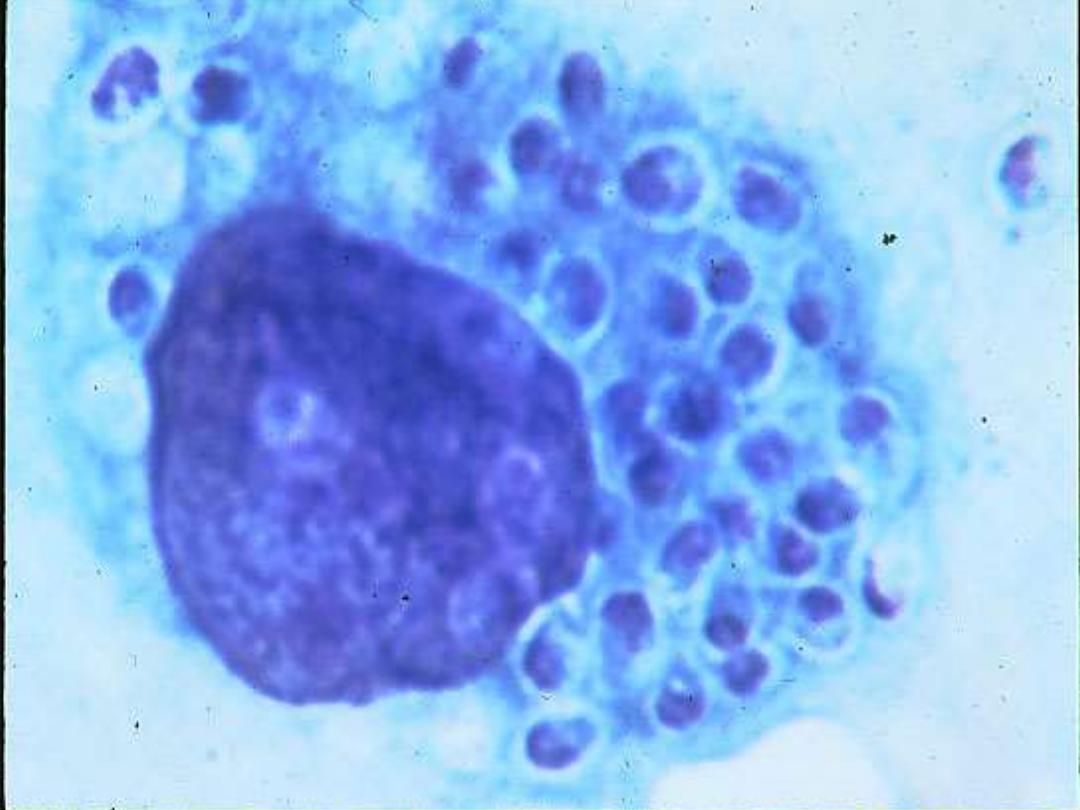
IMMUNOCOMPROMISED PATIENTS
CAN DEVELOP HEPATIC
CANDIDIASIS

Candida species
In the previous lecture I only mentioned
Candida albicans. There are several
Candida species that infect the
compromised host.
Candida species
• C. glabrata
• C. krusei
• C. torulopsis
• C. parapsilosis
• C. lusitaniae
• C. dubliniensis

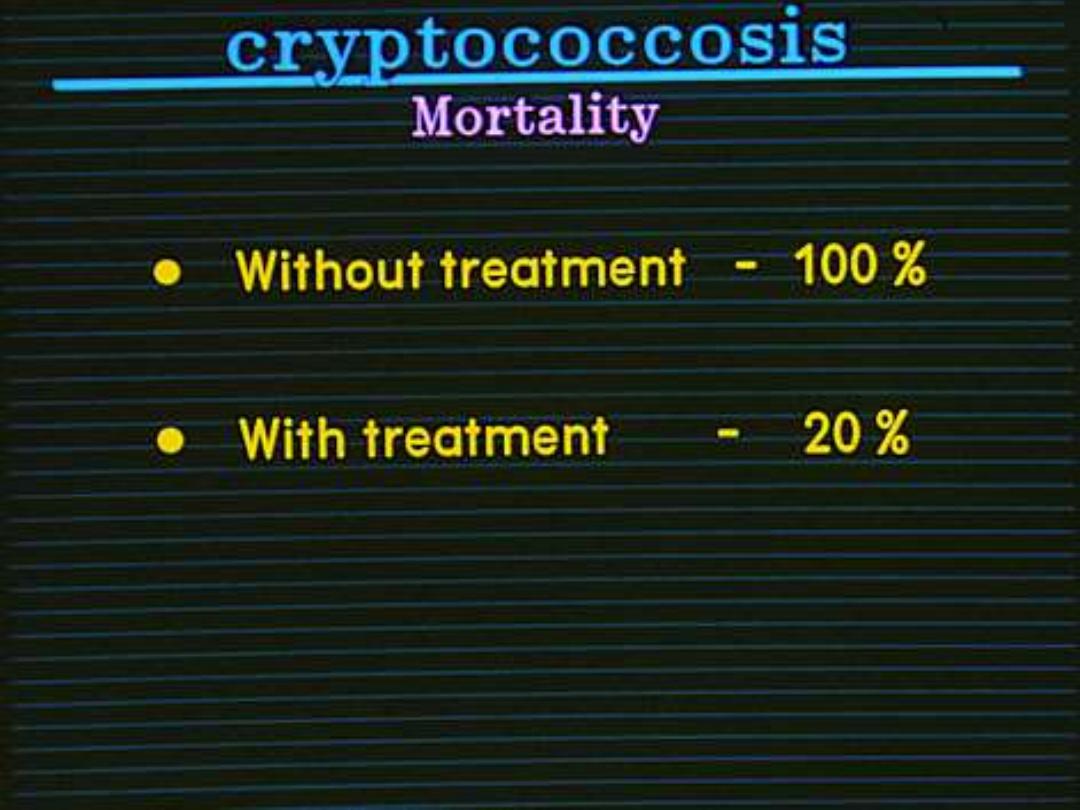
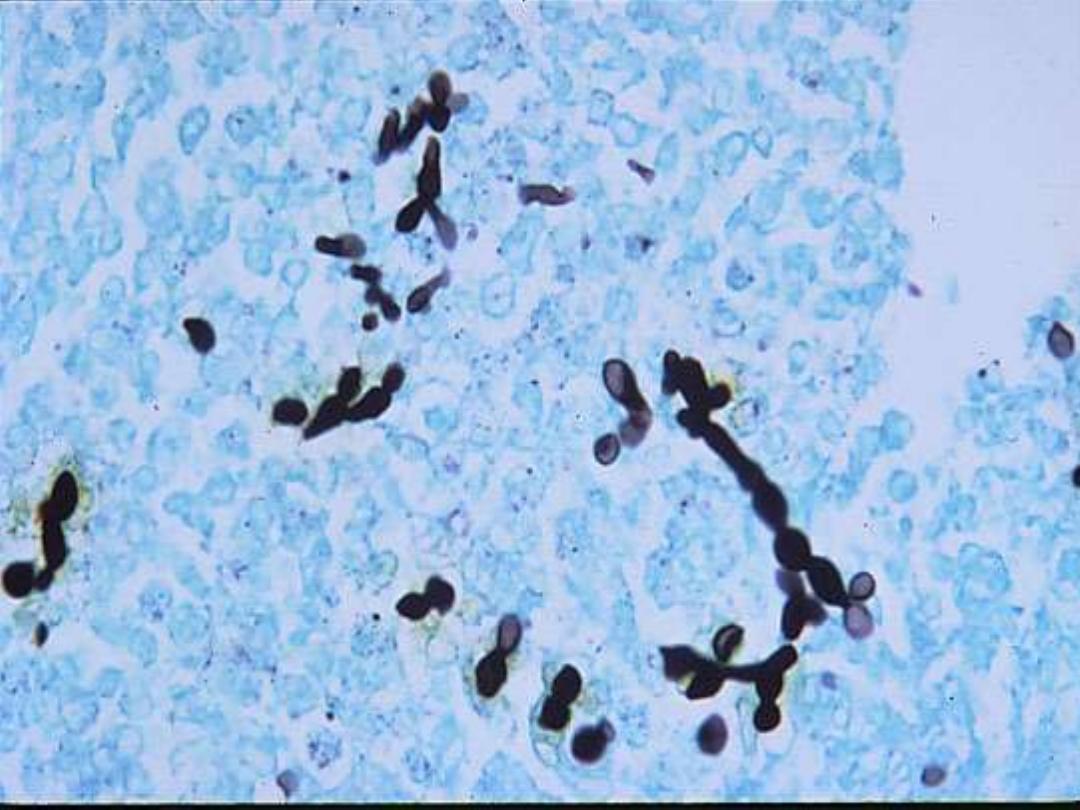
Cryptococcosis
A sub-acute or chronic infection which
may affect the lungs or skin but most
commonly manifests as a meningitis
Ecological Niche
Cryptococcus neoformans
• pigeon droppings
• Chicken droppings

Cryptococcus neoformans
PORTAL OF ENTRY
•INHALATION
•INOCULATION



Cryptococcus neoformans
LOW NUMBER X HIGH VIRULENCE =
NO DISEASE
NORMAL HOST
Cryptococcus neoformans
LOW NUMBER X HIGH VIRULENCE = INFECTION
COMPROMISED HOST
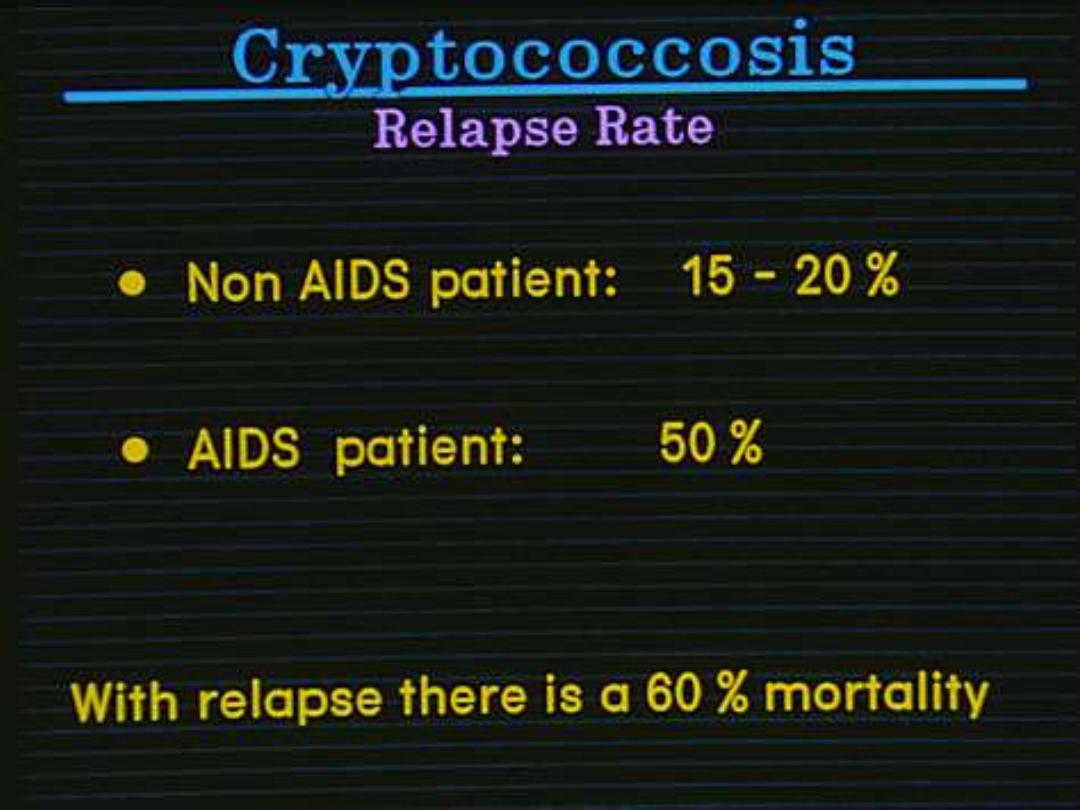
Cryptococcosis
In the Compromised patient:
•
Amphotericin B
•
5 FC
Then Fluconazole the remainder of their life.
Fluconazole penetrates the CSF

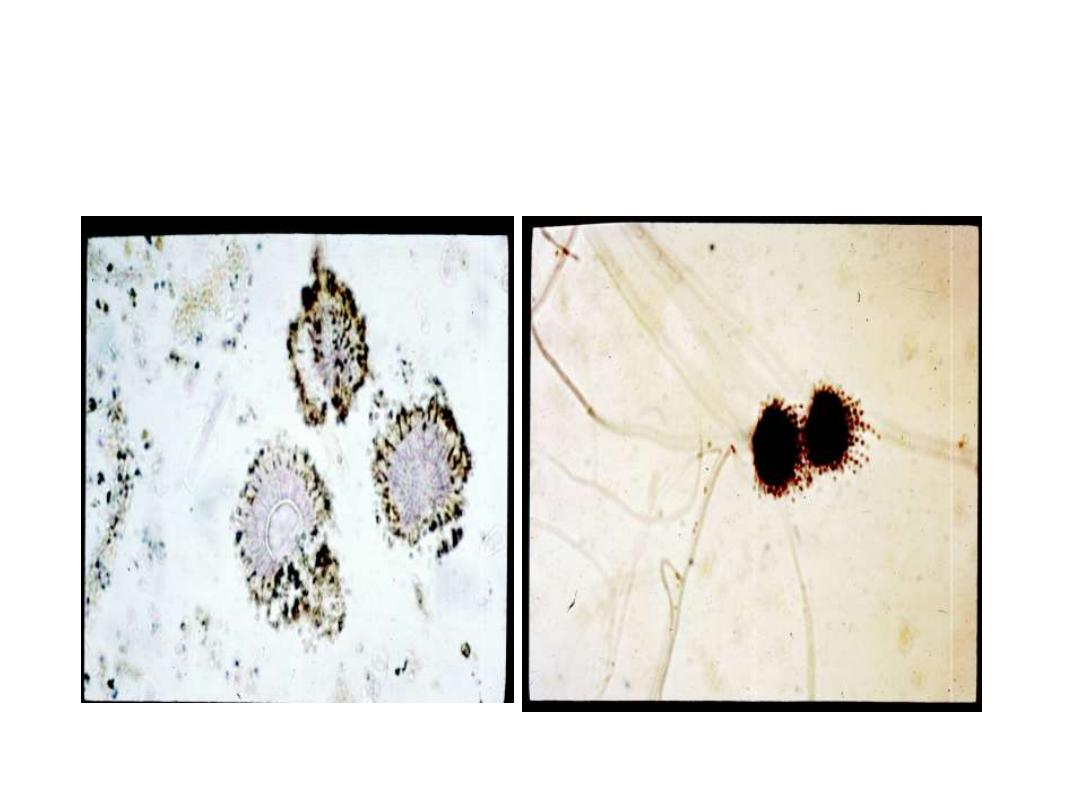
SPOROTRICHOSIS
Primarily a disease of the cutaneous
tissue and lymph nodes. Recently,
pulmonary disease.

PORTALS OF ENTRY
• Inhalation
• Inoculation


ECOLOGICAL
ASSOCIATIONS
• Rose thorns
• Sphagnum moss
• Timbers
• Soil
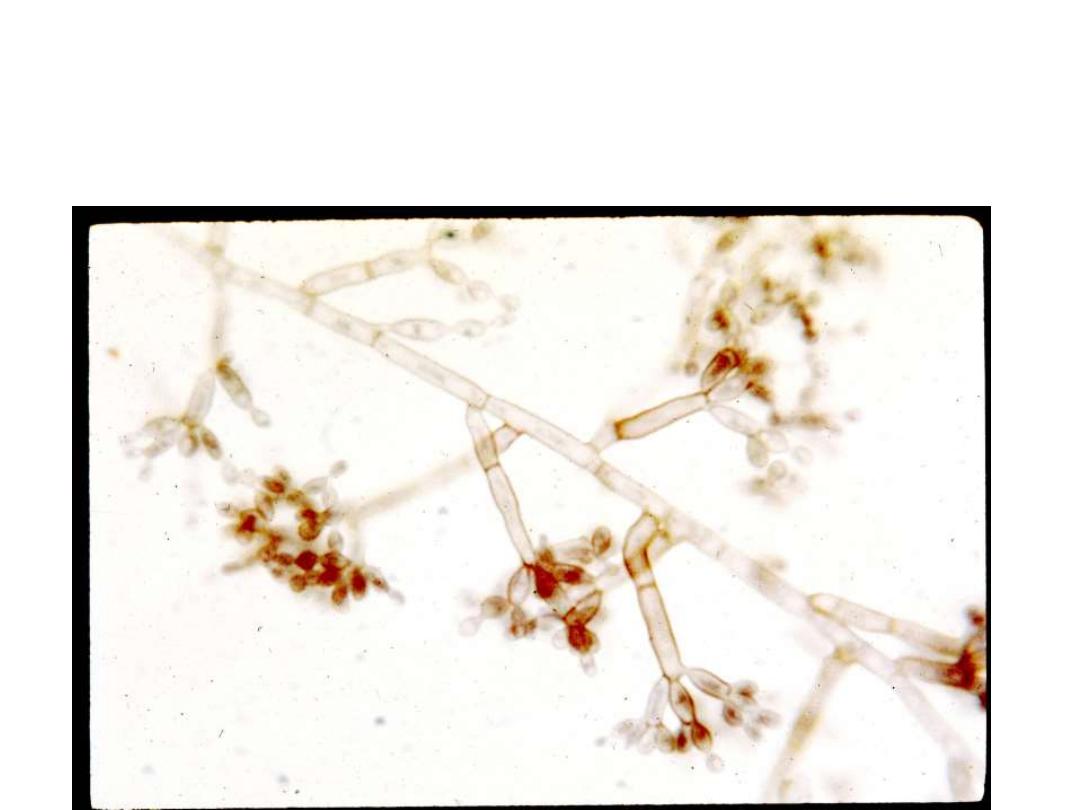
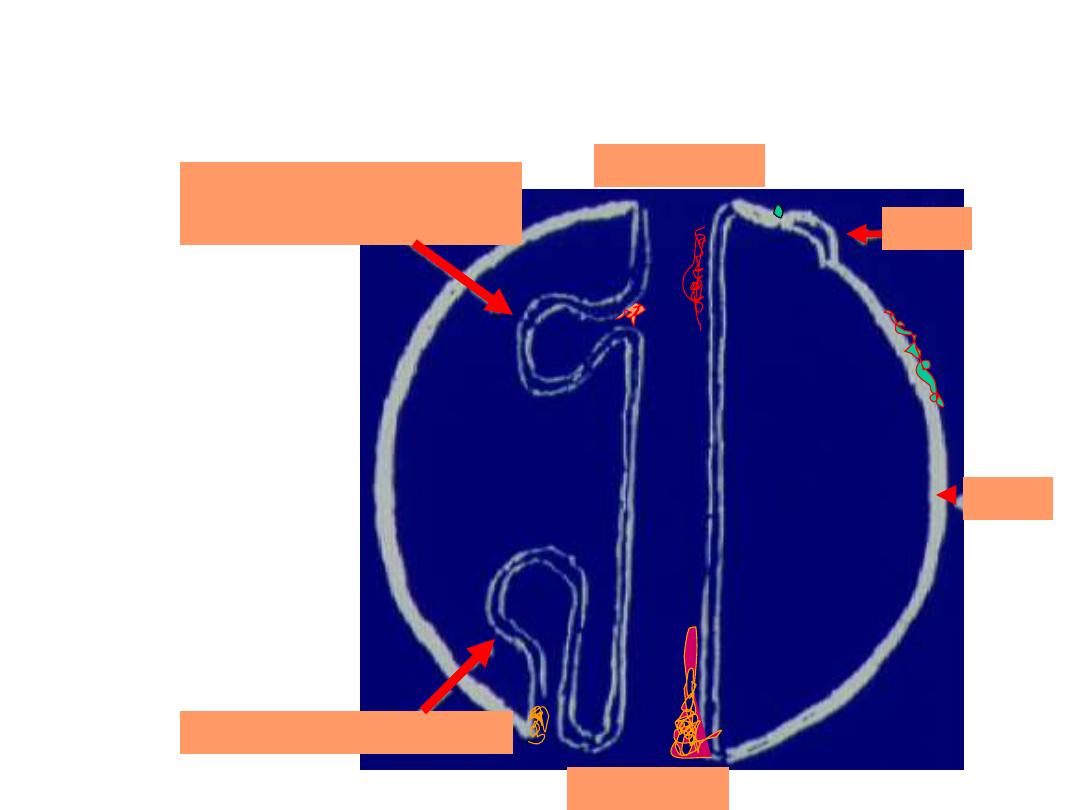
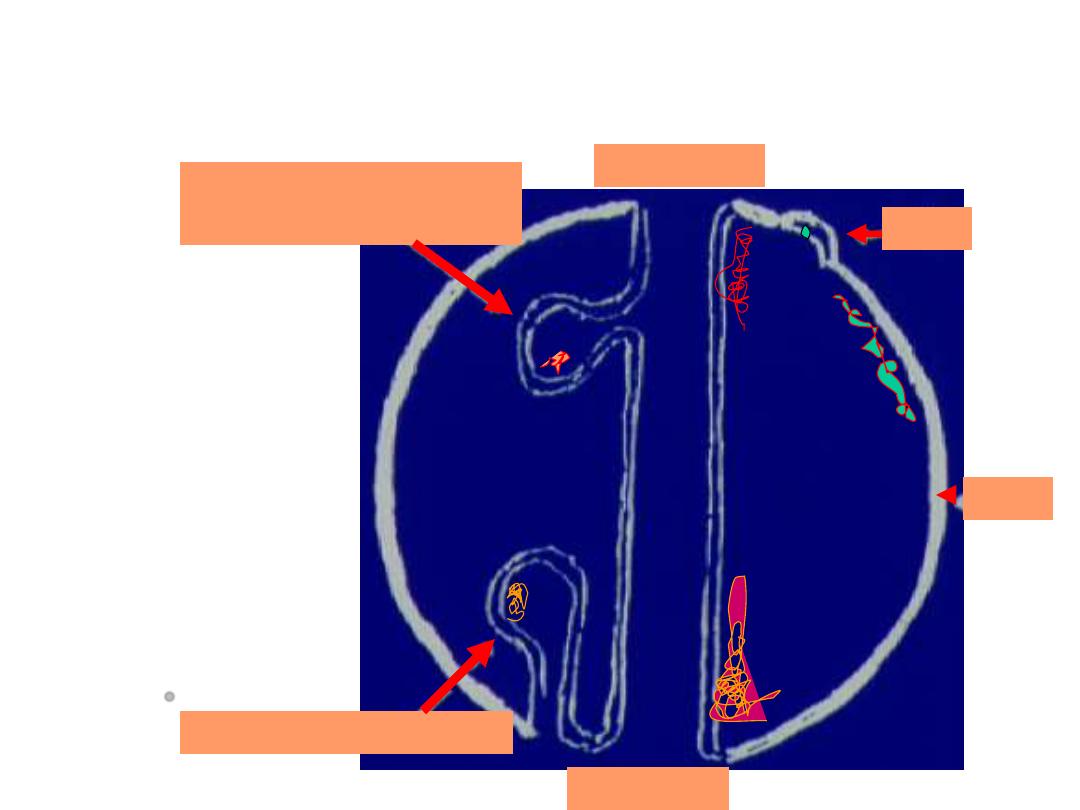
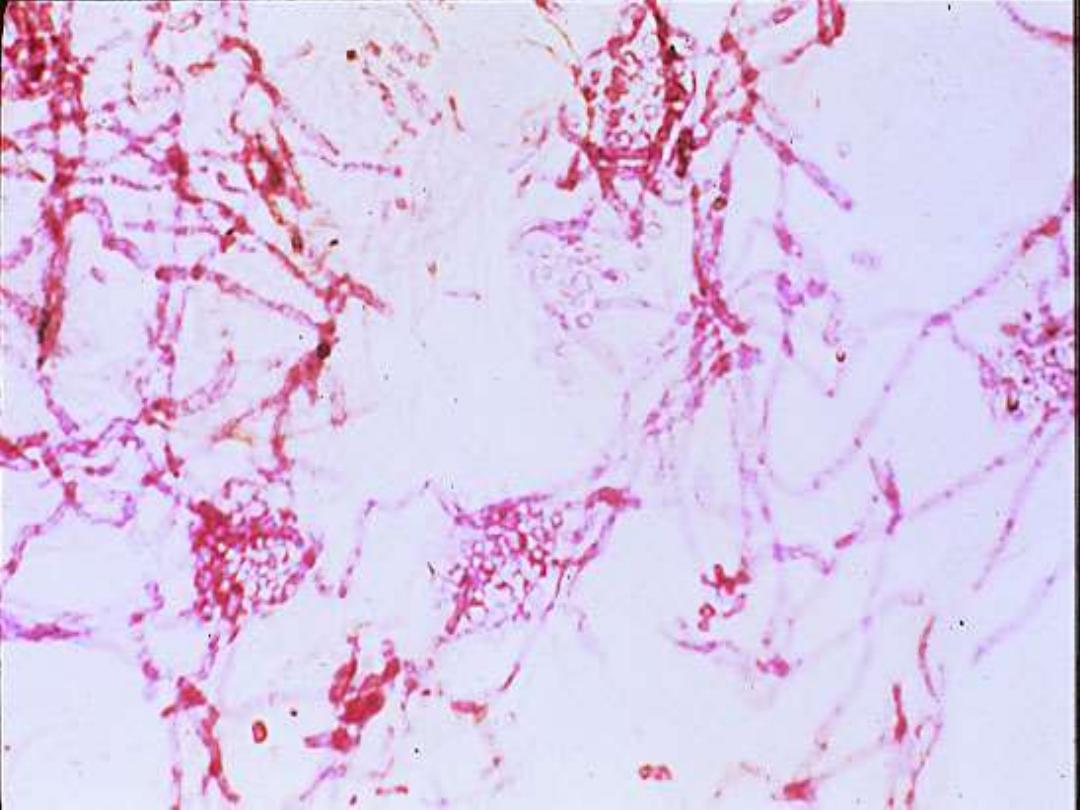
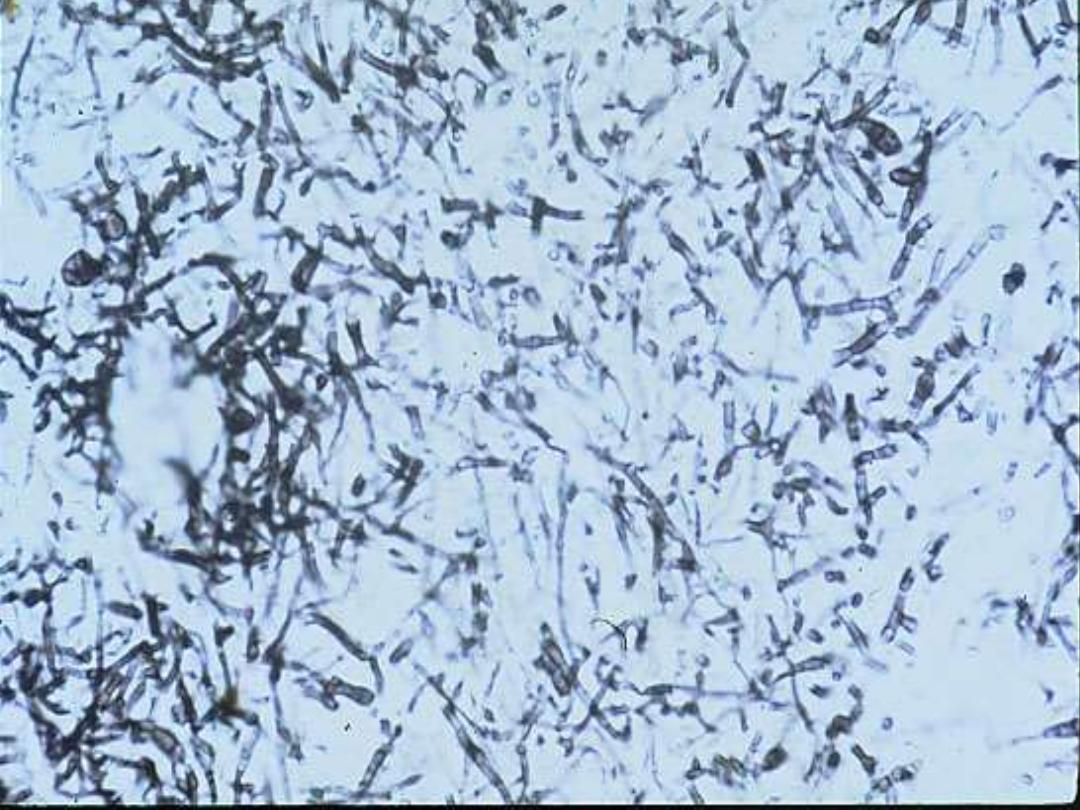
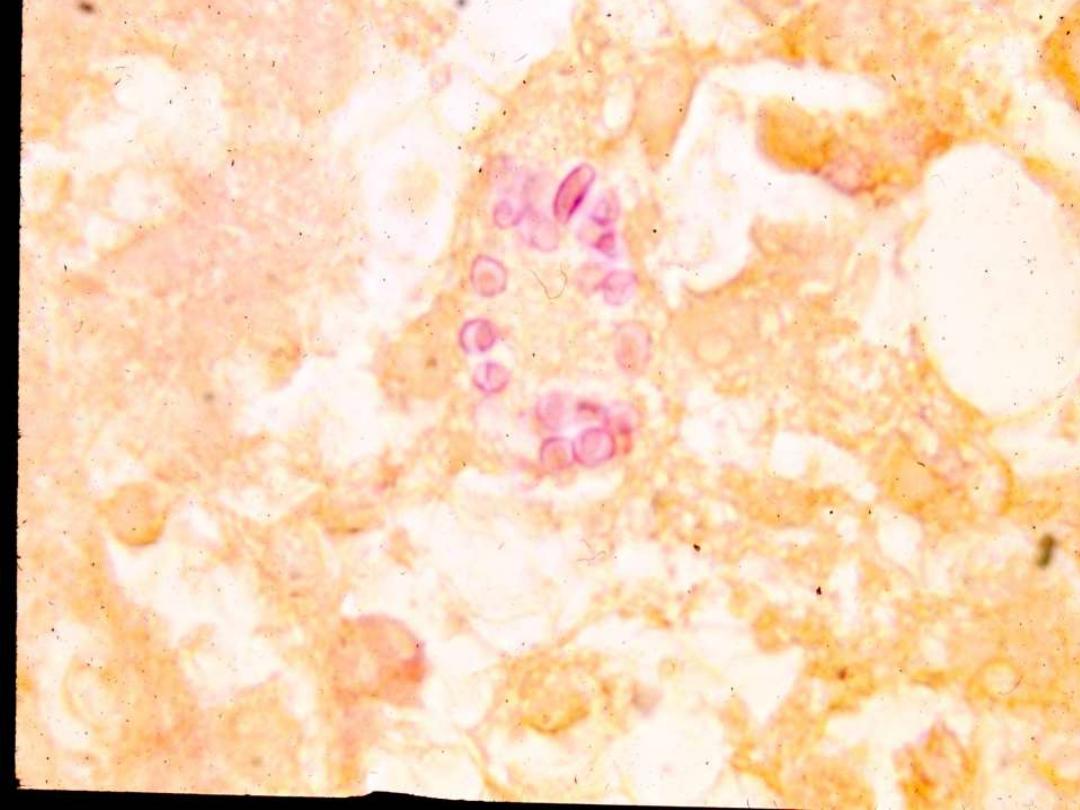
Sporotricosis in wet mount

SPOROTRICHOSIS
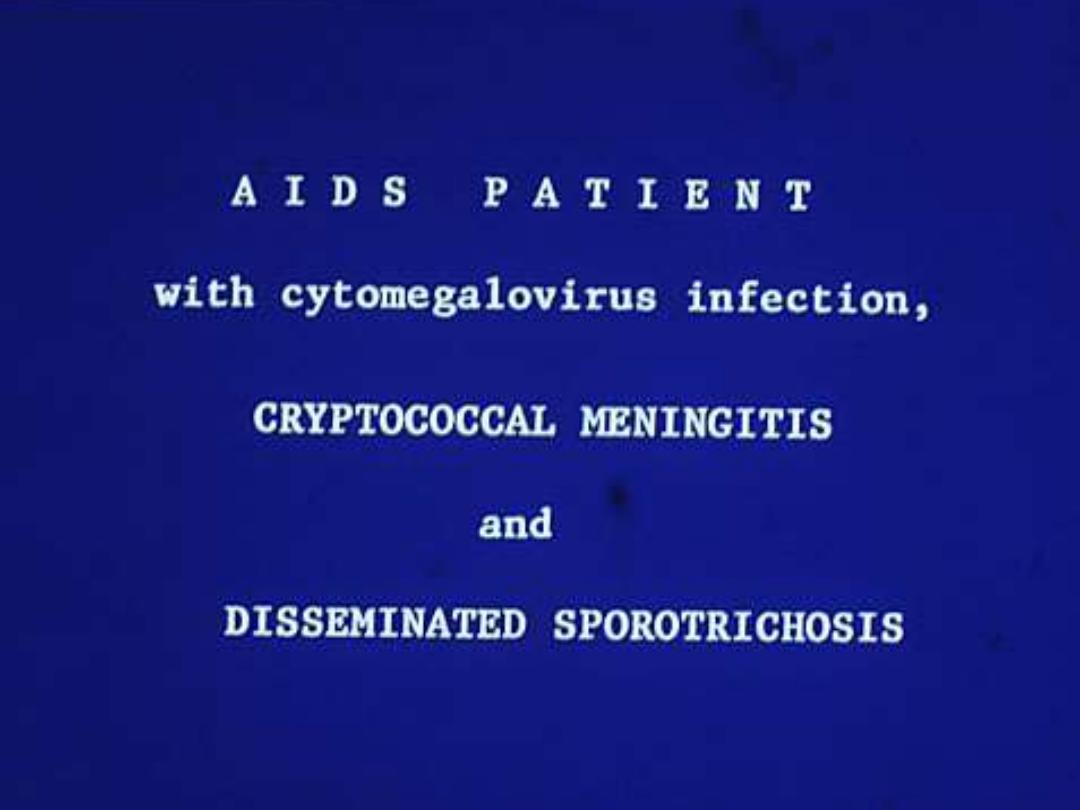
• One report
• 16 Patients
• 10 localized disease
– 7-lung, 2-skin, 1 CNS
• 6 Disseminated
– 5/6 – CNS
All did poorly

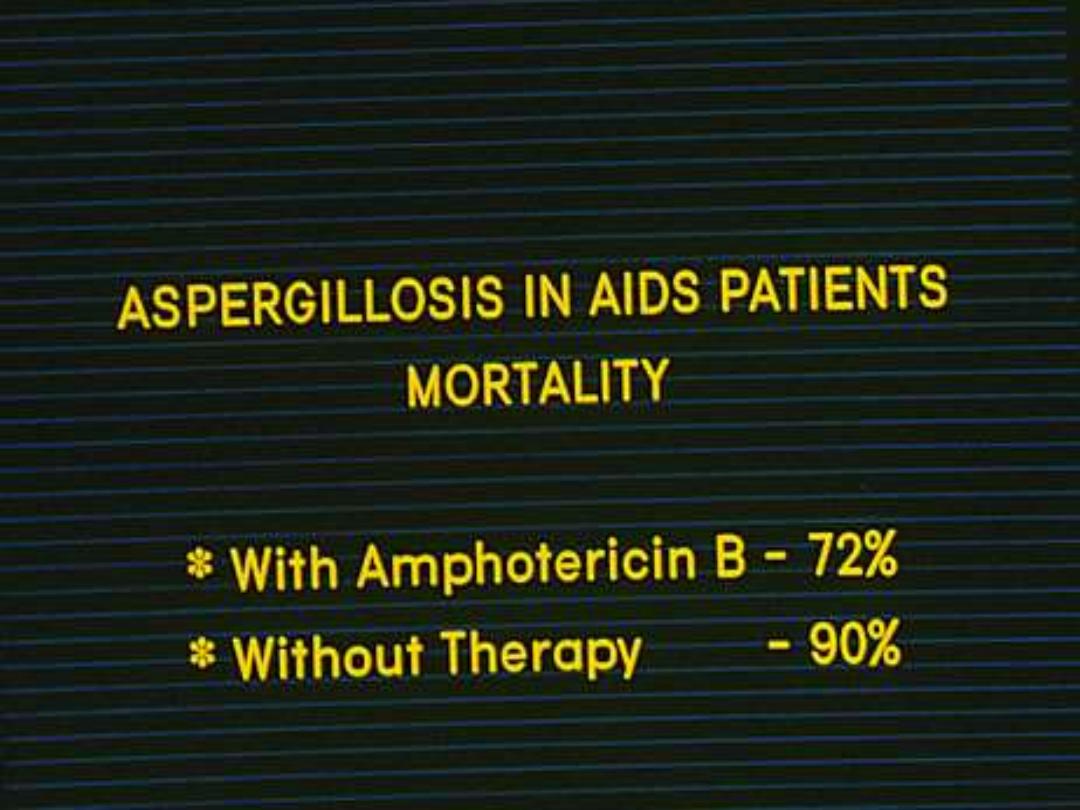
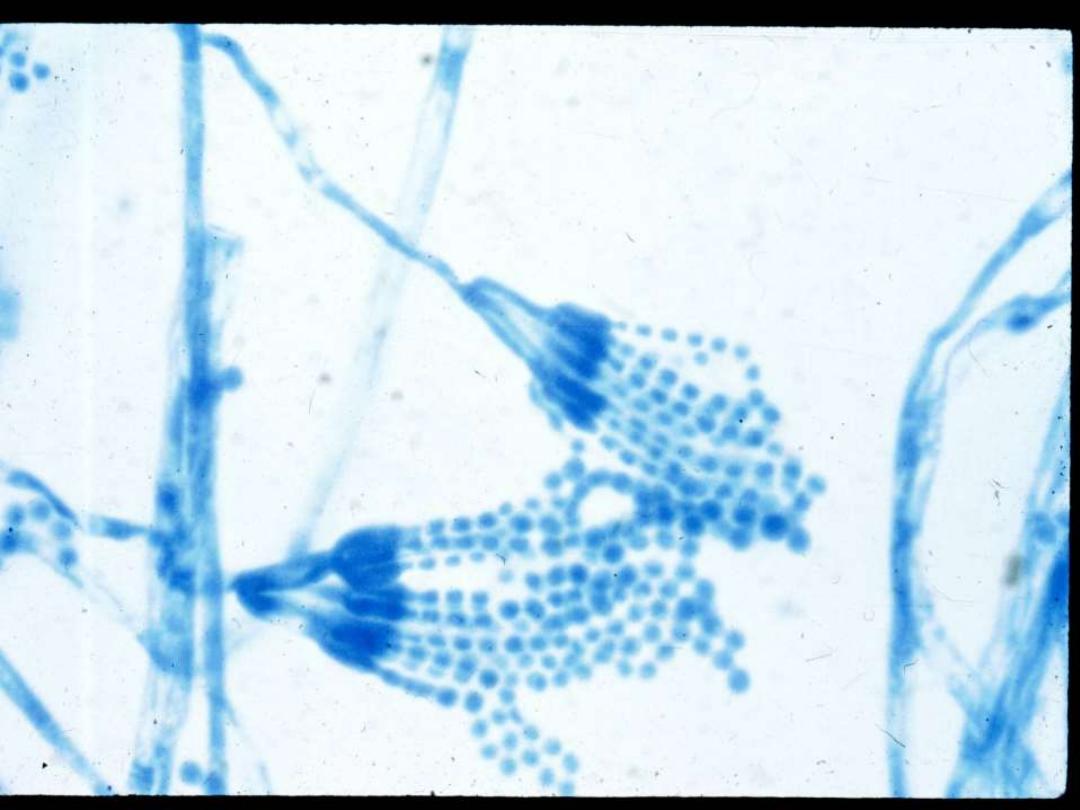
Aspergillus species
HIGH NUMBER X LOW VIRULENCE =
NO DISEASE
NORMAL HOST

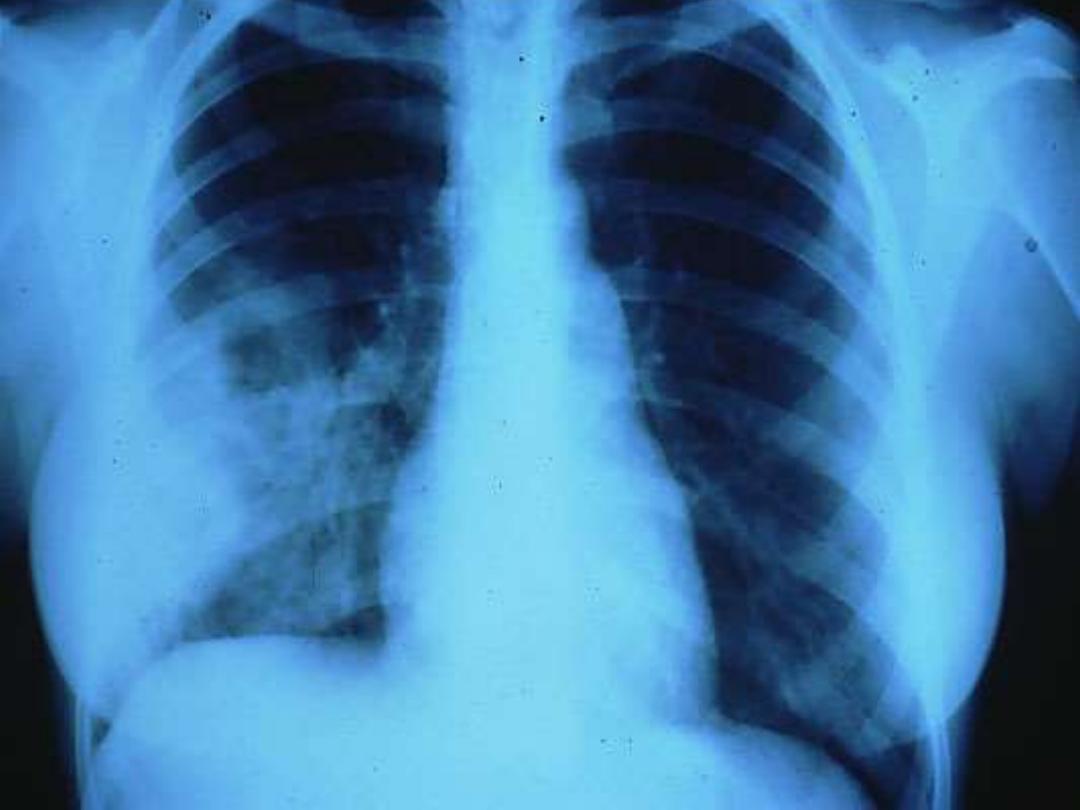
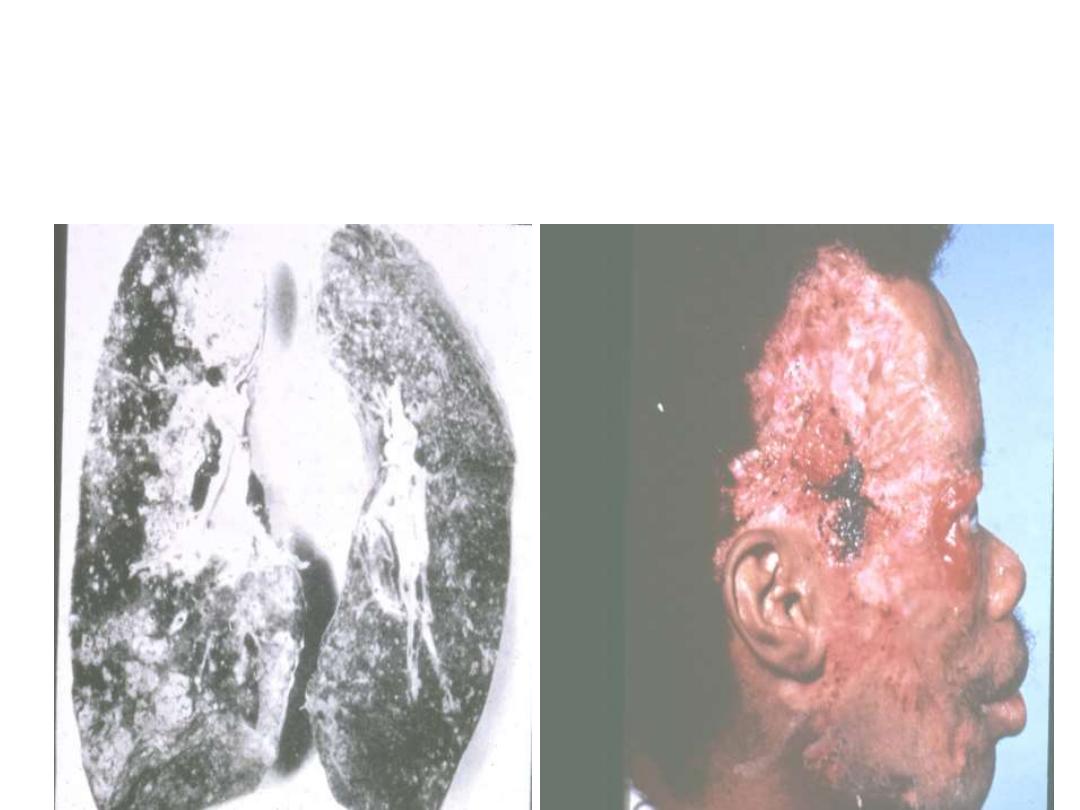
ASPERGILLOSIS
• A variety of diseases:
• pulmonary
1. ALLERGIC
2. FUNGUS BALL
3. INVASIVE
• , external ears, eyes, meninges, sinuses or
blood stream

1.
Radiography not specific (except fungus ball)
2.
Clinical symptoms are not specific
3.
Blood cultures seldom positive
4.
Serology seldom positive (early)
5.
Need invasive procedures for early detection
causative agents
A. FUMIGATUS
A. NIGER
A. FLAVUS

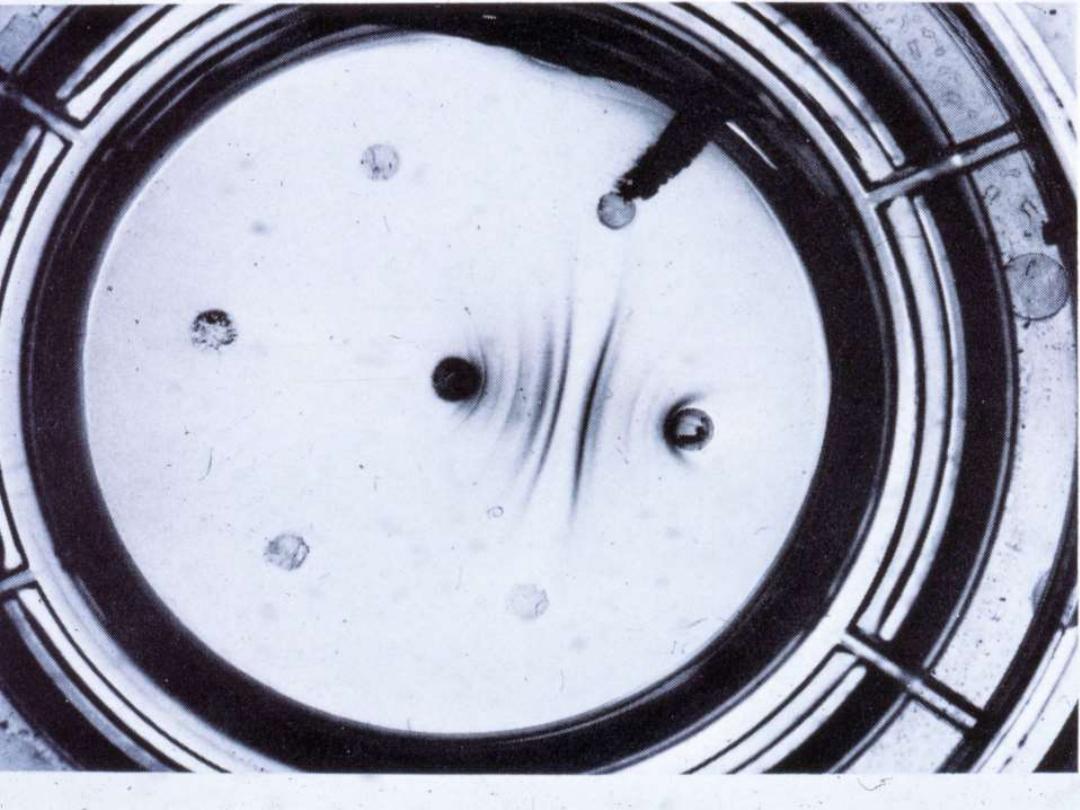
SEROLOGIC TESTS
1. IMMUNODIFFUSION
(antibody)
2.
EIA - GALACTOMANNAN
(antigen
)
Aspergillus species
LOW NUMBER X LOW VIRULENCE = INFECTION
COMPROMISED HOST


CLINICAL PRESENTATION
1. Atypical Signs and Symptoms
2. Unusual Organ Affinity
3. Outside Endemic Area
4. Unusual histopathology
5. Unusual Pathogens

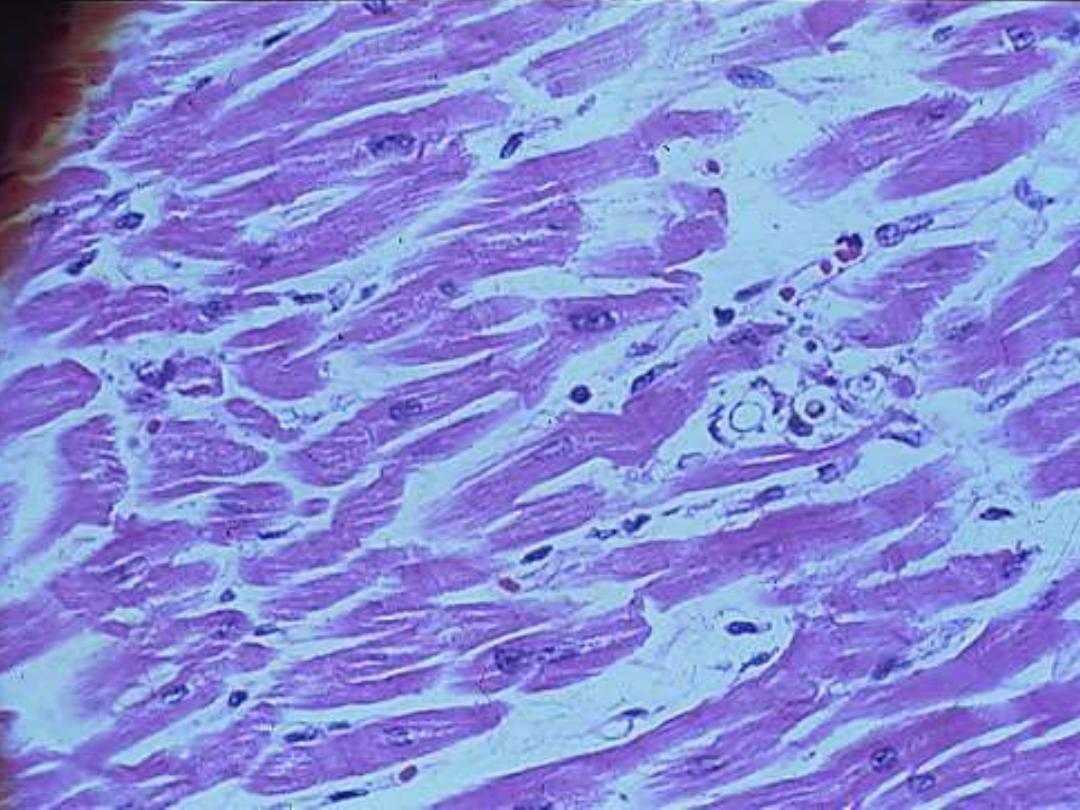
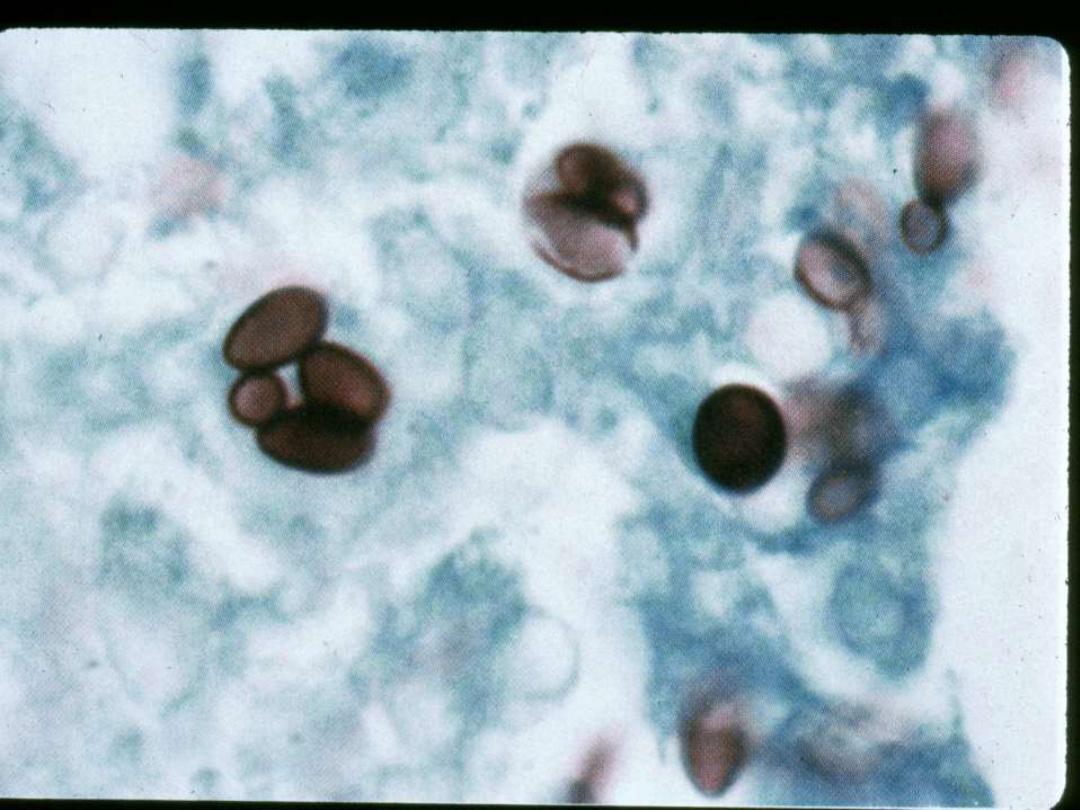
Blastomycosis in
immunocompramized patients
1.
A CHRONIC SUPPURATIVE AND
GRANULOMATOUS DISEASE OF ANY TISSUE
WITH A PREDILECTION FOR LUNGS, SKIN,
PROSTATE AND BONE
2.
SYSTEMIC
USUALLY PULMONARY
2.
CUTANEOUS
PRIMARY
SECONDARY

Identification
1. Microscopic observation
2. Conversion
3. DNA Probe
4-IMMUNODIFFUSION
5-COMPLEMENT FIXATION
6-EIA
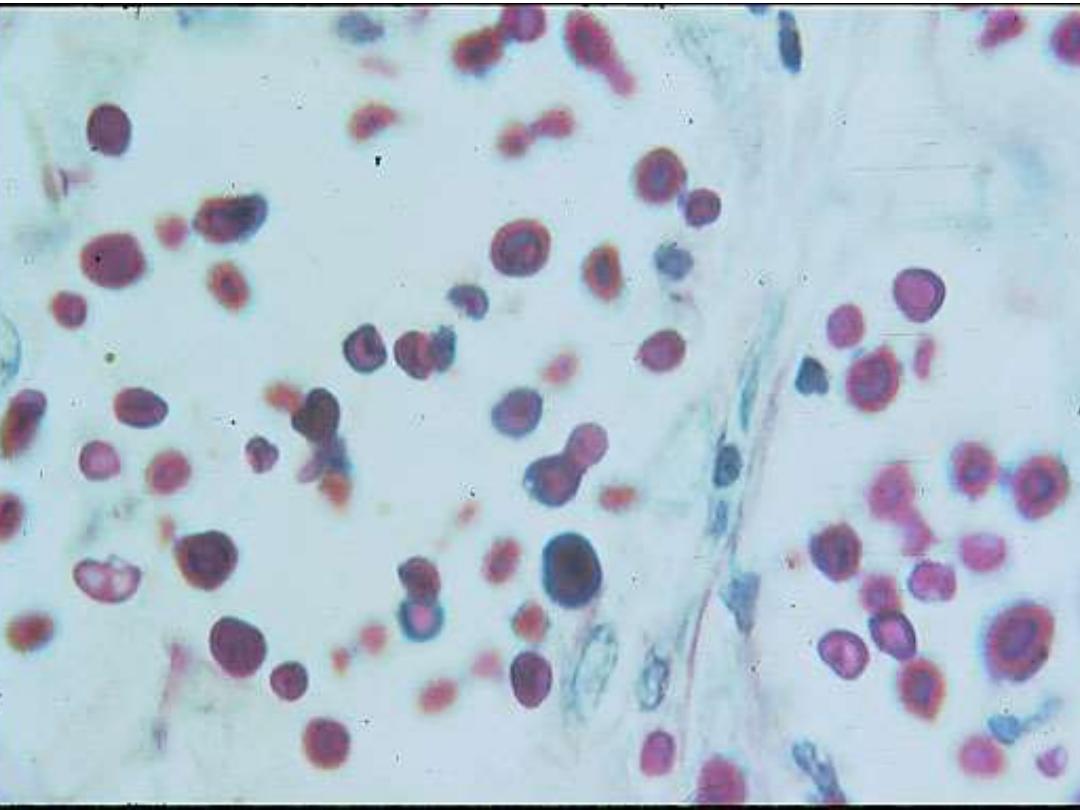
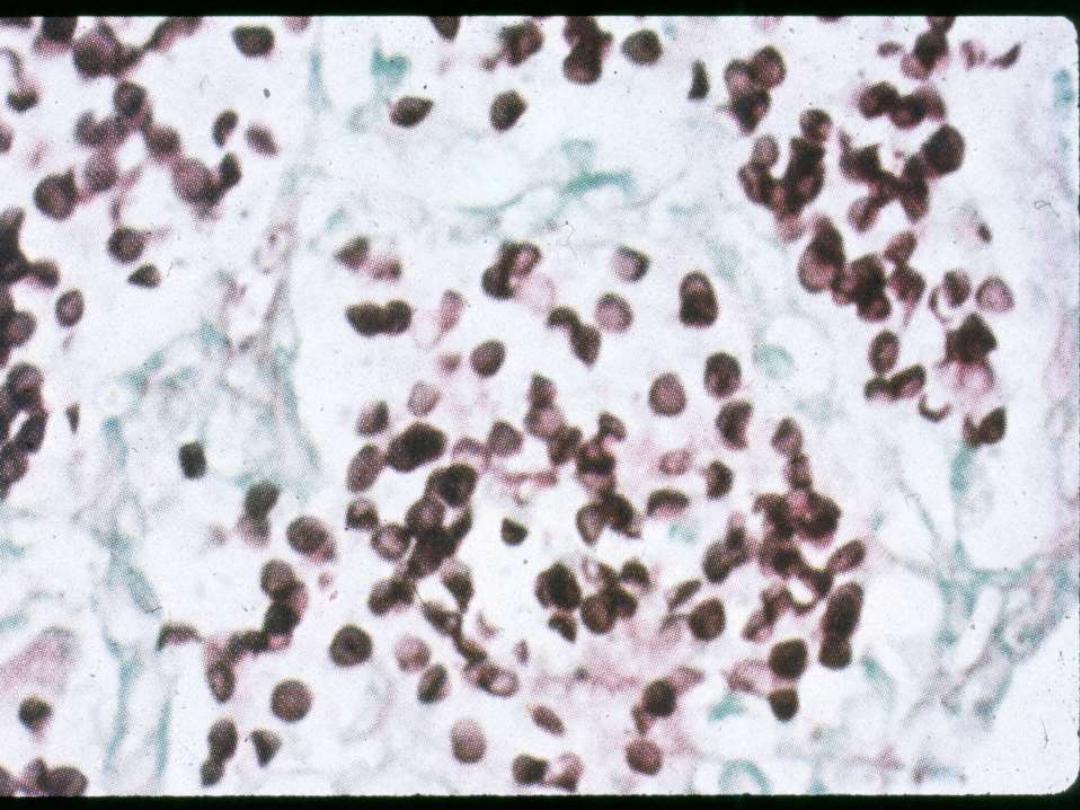
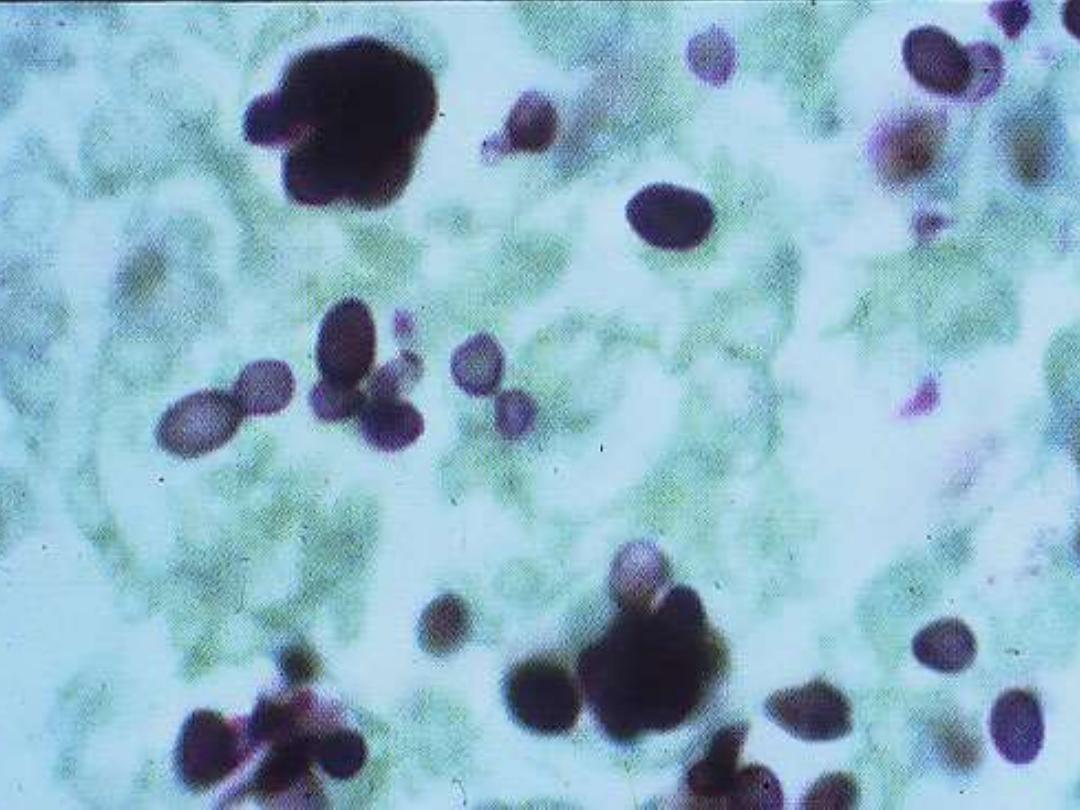
HISTOPLASMOSIS
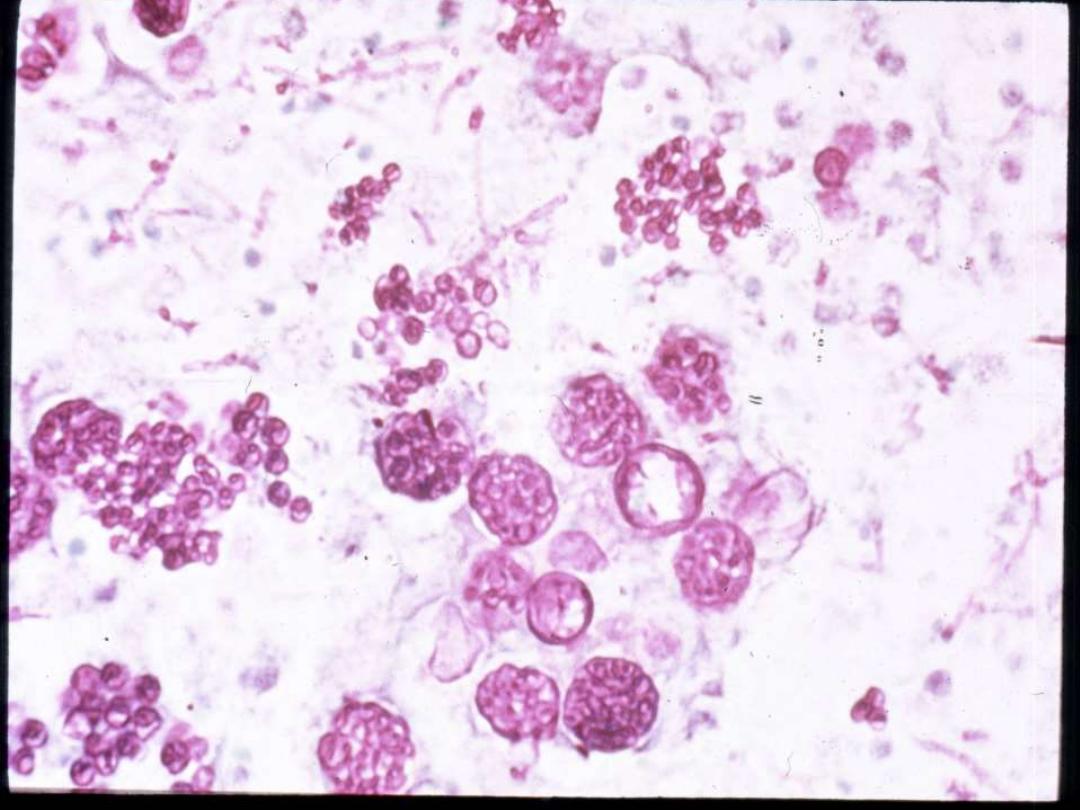
Spherules

HISTOPLASMOSIS IN I.C PATIENTS
• ALL CASES ARE DISSEMINATED
• RELAPSES ARE GREATER THAN 50 %
• RAPIDLY FATAL IN 10 %

CLINICAL PRESENTATION
1. Atypical Signs and Symptoms
2. Unusual Organ Affinity
3. Outside Endemic Area
4. Unusual Histopathology
5. Unusual Pathogens

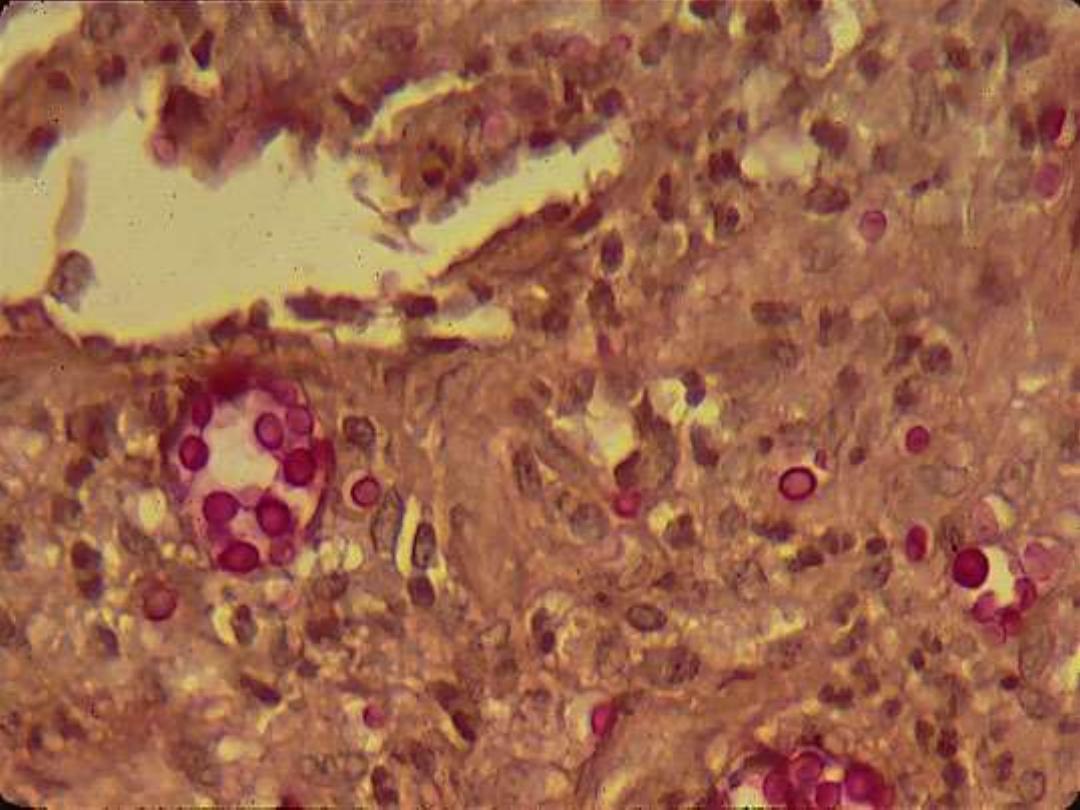
INFLAMMATORY REACTION
• NORMAL HOST
– PYOGENIC
– GRANULOMATOUS
• IMMUNODEFICIENT HOST
– NECROTIC

CLINICAL PRESENTATION
1. Atypical Signs and Symptoms
2. Unusual Organ Affinity
3. Outside Endemic Area
4. Unusual histopathology
5. Unusual Pathogens
Opportunistic Fungi
Include many species from:
A (Aspergillus)
To
Z (Zygomyces)

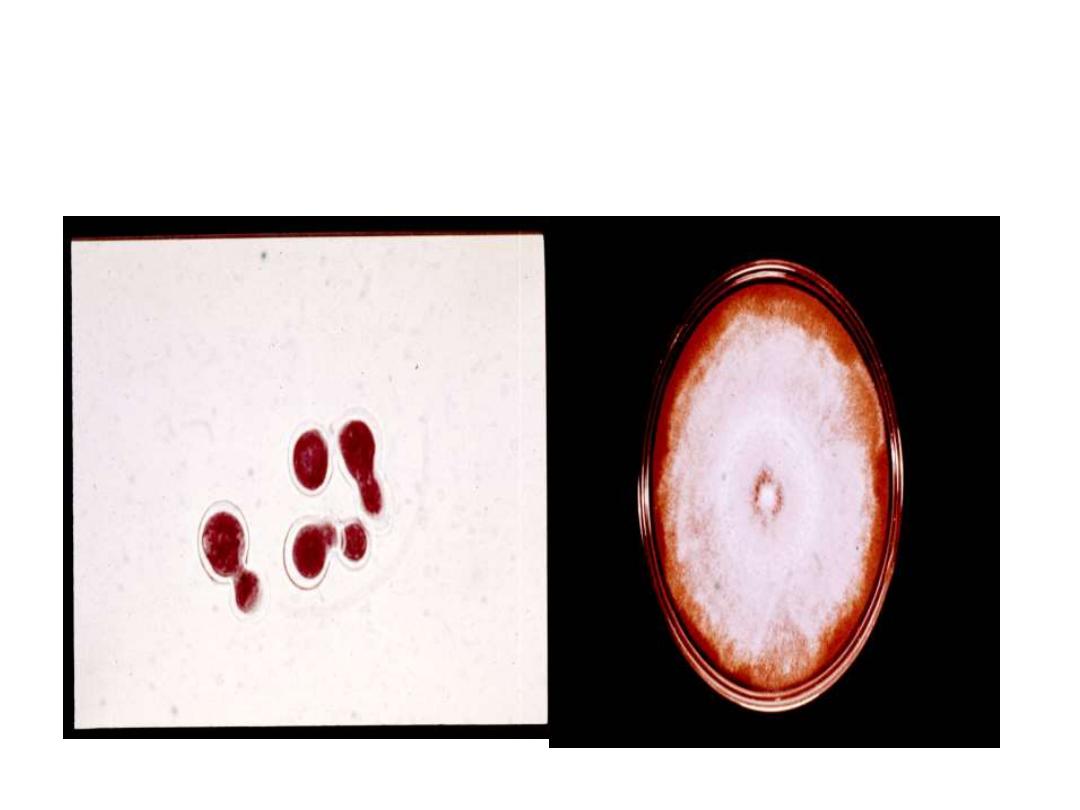
Penicillium marneffei
1. Usually not a pathogen
2. The only dimorphic penicillium
3. Produces a red pigment
4. Endemic in the Far East


Pneumocystis jiroveci
Recently confirmed as a member of
Kingdom Fungi. Formerly thought to
be a protozoan.
Cryptococcus neoformans
• Diabetes mellitus
• Tuberculosis
• Lymphoma
• Hodgkin’s disease
• Corticosteroid therapy
• Immunosuppression
Candida albicans
• Prolonged antibiotic therapy
• Prolonged intravenous therapy
• Prolonged urinary catheters
• Corticosteroid therapy
• Diabetes mellitus
• Hyperalimentation
• Immunosuppression
Torulopsis (Candida) glabrata
• Cytotoxic drugs
• Immunosuppression
• Diabetes mellitus
• Hyperalimentation
• Intravenous catheters
Mucormycetes
• Diabetes mellitus
• Leukemias
• Corticosteroid therapy
• Intravenous therapy
• Severe burns
Aspergillus species
• Leukemias
• Corticosteroid therapy
• Tuberculosis
• Immunosuppression
• Intravenous drug abuse
IMPROVING TREATMENT
1. New Drugs
2. New therapeutic regimen
3. Aggressive therapy
4. Conjunctive therapy
IMPROVING TREATMENT
New Drugs
Lipid Amphotericin B
Third generation azoles
(Posaconazole, Voriconazole)
New classes of antifungal agents
(Echinocandins)
IMPROVING TREATMENT
New Therapeutic Regimen
Combination Therapy
1. Simultaneously administering two drugs
2. Sequential Tx with two or more drugs
3. Alternate Administration of two or more
IMPROVING TREATMENT
AGGRESSIVE THERAPY
FOR IMMUNOCOMPROMISED
PATIENTS
1. Prophylactic – Anti-fungal agents at, or
near, the time of chemotherapy.
2. Posaconazole now approved.
IMPROVING TREATMENT
AGGRESSIVE THERAPY
FOR IMMUNOCOMPROMISED
PATIENTS
2. Empirical – Start therapy when patient at
risk, i.e., fever and/or infiltrate without
response to anti-bacterials.
IMPROVING TREATMENT
AGGRESSIVE THERAPY
FOR IMMUNOCOMPROMISED
PATIENTS
3. Pre-emptive –When there is some
additional evidence of fungal infection
(serology, isolate, etc.)
IMPROVING TREATMENT
CONJUNJUNCTIVE THERAPY
Antifungal agent plus a recombinant
monoclonal antibody.
IMPROVING TREATMENT
CONJUNJUNCTIVE THERAPY
FOR IMMUNOCOMPROMISED
PATIENTS
The use of anti-fungal agents with
immunotherapy.
Immunotherapy
• Interferons
• Colony stimulating factors
• Interleukins

“In the field of observation, chance only favors those who
are prepared.”
Louis Pasteur - 1854
From:
Inaugural Address as Professor of
Chemistry and Dean of Faculty of Science,
Lillie, France.
“In the field of observation, chance only favors those who are
prepared.” Louis Pasteur -1854

“Only the prepared mind can help the impaired host”
Libero Ajello, Chief Mycology Division, CDC 1972

MYCOLGISTS have more
FUN
GI
