
D
R
. H
UDA
A
BO
-A
LEES
2014-2015
Gram-neg ative r ods
Proteus & Pseudomonas
Objectives:
v
Describe the morphology & physiology for Proteus &
Pseudomonas.
v
Determine the virulence factors of proteus and
pseudomonas.
v
Analyze the diseases & pathogenicity for proteus and
pseudomonas.
v
Over view about the epidemiology.
v
Outline the laboratory diagnosis.
v
Describe the treatment for each.
P
ROTEUS
-P
ROVIDENCIA
-M
ORGANELLA
G
ENERA
¢
According to recent genetic studies many species of
proteus genus have been transferred to genus providencia
and morganella. Such as:
Proteus morganii = Morganella morganii and
Proteus rettgeri = Providencia rettgeri.
¢
That’
s leaves only two species in proteus genus these are:
Proteus vulgaris
and
Proteus mirabilis.
G
ENERAL CHARACTERISTICS
v
Gram-negative rods that are distinguished from other
members of the Enterobacteriaceae by their ability to
produce the enzyme phenylalanine deaminase.
v
Produce the enzyme urease, which cleave urea to form
NH3 and C02.
v
Certain species are very motile and produce a striking
swarming effect on blood agar, characterized by
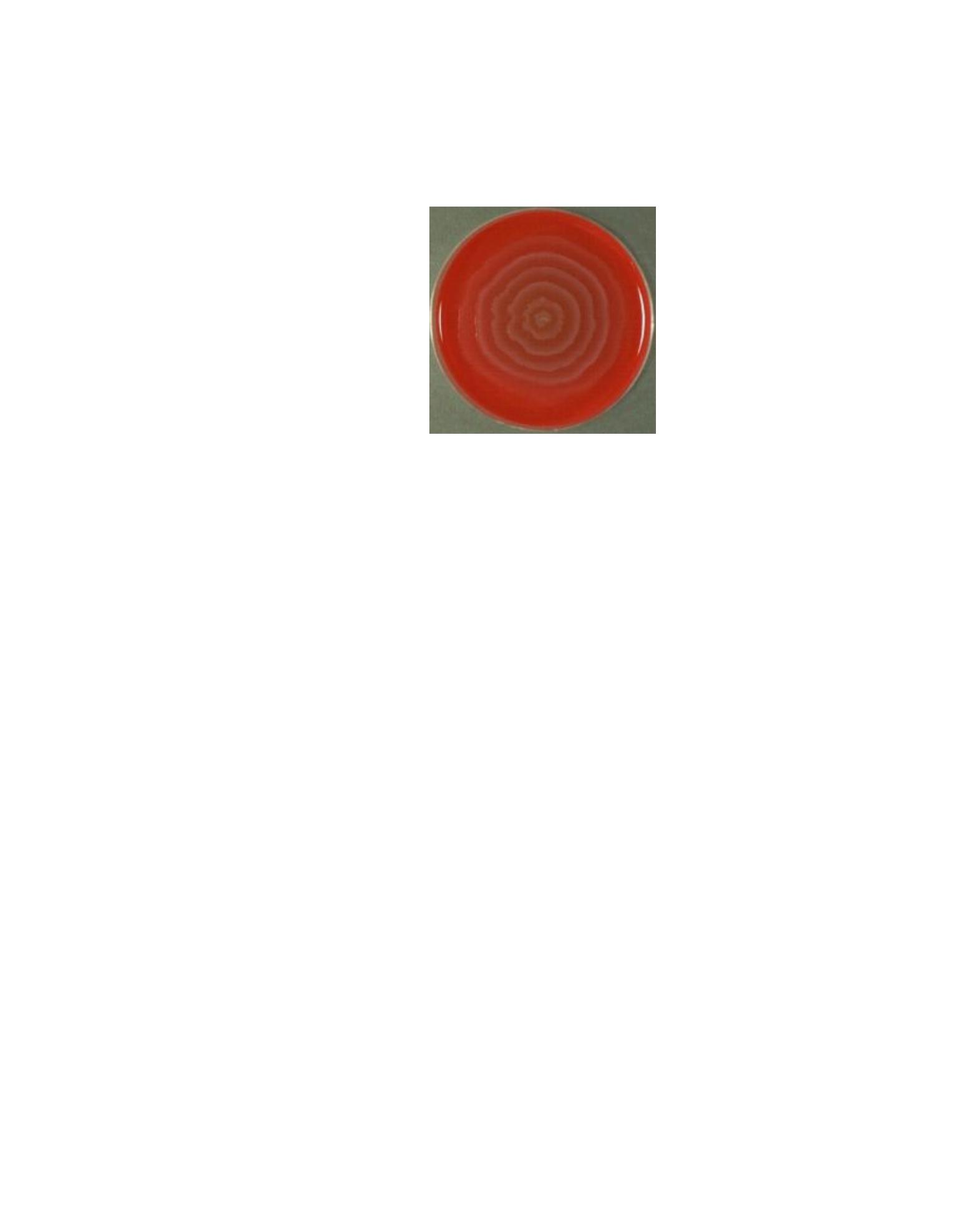
expanding rings (waves) of organisms over the surface
of the agar.(
Swarming Phenomenon
).
v
The cell wall O antigens of certain strains of Proteus,
such as OX-19, OX-K and OX-2, cross-react with
antigens of several species of Rickettsiae (which cause
typhus
fever). These Proteus antigens can be used in
laboratory test to detect the presence of antibodies against
certain rickettsiae in patient's serum. This test, called the
Weil-Felix
. When treated serum of person infected with
typhus fever with Proteus Ag from spp (OX-19, OX-K and
OX-2) will give +ve reaction, means that the patient has
typhus fever
.
H
ABITAT AND
T
RANSMISSION
¢
The organisms are present in the human colon (normal flora)
as well as in soil and water.
¢
Transmission usually endogenous, to urinary tract by
ascending spared of fecal flora.
¢
Proteus. mirabilis is the species that cause most community
and hospital-acquired infections
.
P
ATHOGENESIS AND VIRULENCE FACTORS

1.
Endotoxin
causes fever and shock associated with sepsis.
2.
The vigorous motility
of Proteus organism may contribute to
their ability to invade the UT.
3.
The Production of Urease enzyme
urease is an important
feature of the pathogenesis of UTI by Proteus. Urease
hydrolyzes the urea in urine to form ammonia, which raises
the PH resulting to alkaline urine. This encourages the
formation of stones (calculi) (
struvite
) composed of
magnesium ammonium phosphate. Stones in the UT
obstruct urine flow, damage urinary epithelium, and serve as
a nidus for recurrent infection by trapping bacteria within
the stone. Because alkaline urine also favors growth of
the organisms and more extensive renal damage,
treatment involves keeping the urine at a low pH.
P
REDISPOSING FACTORS FOR
UTI
¢
Some conditions enhance the chances of getting UTI:
1.
The colonization of the vagina.
2.
Urinary catheters.
3.
Abnormalities of the urinary tract such as strictures, valves,
and stones
.
C
LINICAL FINDINGS AND DISEASES
¢
Urinary tract infection.
¢
Pneumonia.
¢
Wound infection.
¢
Septicemia.
L
ABORATORY
D
IAGNOSIS
1.
Staining by Gram stain : Gram –
ve rods.
2.
.
Culture:
a. On MacConkey and EBM ager produce non-lactose
fermenter (colorless) colony.
b. On blood ager produce characteristic
Swarming
phenomena
which considered as diagnostic feature for
Proteus however, can cause misdiagnosis for other bacteria as
it can cover other colonies and cannot obtain pure culture.
How it can be prevented.
3.
P. vulagaris and p. mirabilis produce H2S which blacken the
butt of TSI agar.
4.
P. mirabilis is indole negative, while others are indole positive.
5.
Ferment glucose producing acid and gas.
6.
Urea agar (urease test) =: Pink (+ ); Yellow (-).
T
REATMENT
¢
It is best to do antibiotics sensitivity test antibiotics
before using antibiotics to reduce drug resistance.
¢
Trimethoprim-sulfamethoxazole or ampicillin is often
used for uncomplicated UIT.
¢
Third generation cephalosporin should be used for
serious infections.
P
SEUDOMONAS
Many important species:
¢
Pseudomonas aeruginosa

¢
Burkholderia cepacia
¢
Burkholderia mallei
¢
Burkholderia pseudomallei
G
ENERAL CHARACTERISTICS
¢
Pseudomonades are Gram-negative rods.
¢
Motile.
¢
Strict aerobic means that they drive their energy only by
oxidation of sugar rather than fermentation.
¢
Non-lactose fermenter.
¢
Oxidase-positive.
¢
P. aeruginosa isolated from patients with cystic fibrosis have
prominent slime layer (Glycocalyx) which give their colony
very mucoid appearance.
¢
P. aeruginosa produces two pigments useful in clinical
and laboratory diagnosis:
¢
1- Pyocyanin
, which can color the pus in a wound blue not
produced by other species.
¢
2- Pyoverdin
(fluorescein). It is a greenish yellow pigment
produced by many other species.
E
PIDEMIOLOGYAND TRANSMISSION
¢
P aeruginosa is widely distributed in soil and water.
¢
10% of people carry it as normal flora of the colon.
¢
Opportunistic pathogens, cause infection in patients with
severe burns and chronic respiratory diseases.
¢
Important cause of hospital acquired infection as it have
remarkable ability to withstand disinfectants, also its ability
to grow in simple aqueous solutions resulted in

contamination of respiratory therapy and anesthesia
equipment, intravenous fluid, and even distilled water.
P
ATHOGENESIS AND VIRULENCE FACTORS
Pathogenesis based on multiple virulence factors:
¢
Endotoxin, exotoxins, and enzymes
¢
Endotoxin
cause symptoms of sepsis and septic shock, the
best known exotoxin is
Exotoxin A
which cause tissue
necrosis.
¢
Enzymes
such as elastase and proteases, which are
histotoxic and facilitate invasion of the organism into the
blood stream.
¢
Pyocyanin
damages the cilia and the mucosal cells of the
respiratory tract.
C
LINICAL FINDINGS AND DISEASES
¢
P. aeruginosa can cause infections anywhere in the body.
And it is one of the important cause of gram-negative
nosocomial infection
¢
Urinary tract infection.
¢
Pneumonia the most common cause of gram negative
nosocomial pneumonia, especially in cystic fibrosis patient.
¢
Wound infection especially burns.
¢
Sepsis.
¢
Endocarditis
.
C
LINICAL FINDINGS AND DISEASES

¢
Malignant otitis externa
, which is sever external otitis.
especially in diabetic patients
¢
Corneal infection in contact lens users.
¢
Bone infection as osteochondiritis.
¢
Folliculitis and other skin infections as
ecthyma
gangrenosum .
LABORATORYDIAGNOSIS
1.
Oxidase positive.
2.
Culture:
a. On MacConkey agar: No lactose fermentation give pale
colonies.
b. Nutrient agar: Demonstrate pigment production like
pyocyanin and pyoverdin that diffuse into the agar.
c. blood agar: Spreading flat pigmented, sometime with Beta-
hemolysis mucoid, confluent growth.
T
REATMENT
¢
Pseudomonas .aeruginosa usually resistant to many
antimicrobial agents.
1.
The drugs of choice are B-lactam compounds as
penicillin, pipracillin, ticarcillin.
2.
Aminoglycosides such as gentamycin and tobramycin.
1&2 often given in combination to provide potential
effect and reduce drug resistance.
3.
Ciprofloxacin.
PREVENTION
Prevention is easier than cure.

1.
Patients at risk as patients with severe burns should be kept
in isolated ward to reduce the chance of infection.
2.
Therapeutic substances and medical instrument should be
kept sterile and screened frequently for contamination
especially if they are used for many patients.
R
EFERENCES
¢
.
Jawetz, Melnick and Adelberg's Medical Microbiology
(Brooks, Butel, Morse). 25th ed. Copyright 2010.
¢
Medical microbiology by David Greenwood 17 th ed. 2007.
¢
L evinson W. Review of Medical Microbiology and
Immunology.12 th ed. Copyright 2012, McGraw-Hill.
