
BACTERIOLOGY
د
.
هيفاء الحديثي
Chlamydiae
- Are obligate intracellular organisms
↓
Grow only within cells
Including
1. Chlamydia trachomatis
eye, respiratory and genital
tract infections.
2. Chlamydia pneumoniae
atypical pneumonia
3. Chlamydia psittaci
psittacosis
Important properties
- They lack the ability to produce sufficient energy to grow
independently.
- They have a rigid cell wall (but not a typical
peptidoglycan layer)
- Have a replicative cycle different from that of all bacteria
begin when extra cellular, metabolically inert (elementary body)
enter the cell
↓
Reorganize into larger metabolically active (reticulate body)
↓
release daughter repeated binary fission
elementary bodies
appear as inclusions
useful in diagnosis
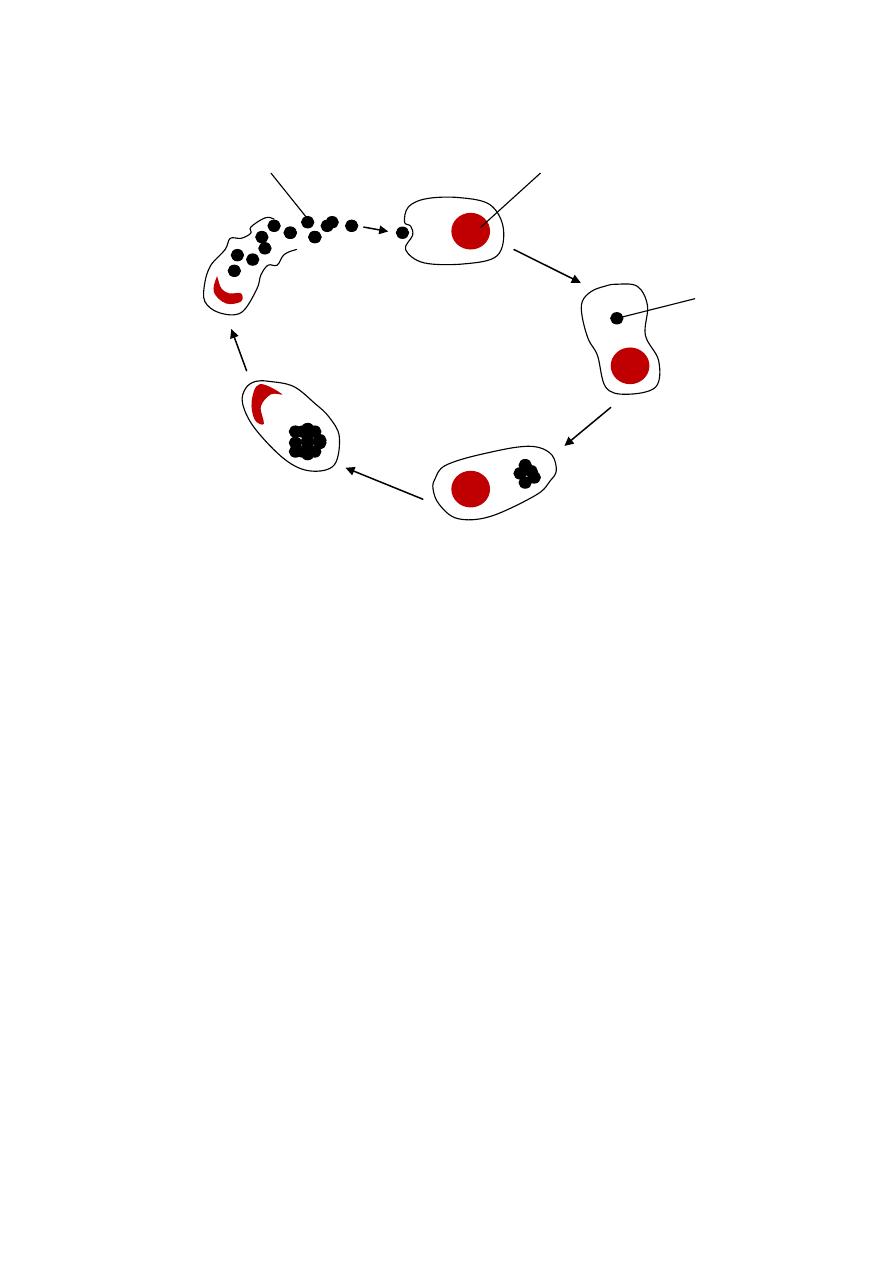
Life cycle of Chlamydia
- All chlamydiae share a group-specific lipopolysacharide
antigen (detected by CFT)
- They also possess species-specific and immunotype-
specific antigens (proteins) (detected by IF)
- C.psittaci and C.pneumoniae each have 1 immunotype,
where as C.trachomatic has at least 15.
Transmission & Epidemiology
- C.trachomatis infects only humans and transmitted by
close personal contact (sexually or by passage through the
birth canal)
- Individuals with asymptomatic genital tract infections are
important reservoir.
Elementary body
Cell nucleus
Formation of
reticulate body

- In trachoma, the microorganisms is transmitted by finger-
to eye contact.
- C.pneumoniae
human
by aerosol
- C.psittaci
birds
dry feces of bird
humans
Pathogenesis & clinical finding
- Chlamydiae infect primarily epithelial cell & rarely
invasive
- C.psittaci infect lungs primarily
asymptomatic
↓
or produce high fever & pneumonia
- C.pneumoniae causes upper & lower respiratory tract
infections (bronchitis & pneumonia, in young adults)
- C. trachomatis, types A, B and C
trachoma and chronic
conjunctivitis and may lead to blindness.
Types D-K
genital tract infections
In men
non gonococcal urethritis
epididymitis or proctitis.
In women
cervicitis
salpingitis
infertility
Infants born to infected mothers
mucopurulent eye
infections 7-12 days after labour.
or develop (chlamydial pneumonitis) 2-12 weeks
Patient with genital tract infection may develop
autoimmune disease caused by antibodies against
C.trachomatis
cross reacting with antigens on cells of

the urethra, joints and uveal tract, this so called (Reiter's
syndrome).
Chlamydia trachomatis L1-L3 immunotypes cause
lymphogranuloma venereum
a sexually transmitted
disease with lesions on genitalia and in lymph nodes.
Laboratory diagnosis
- Cytoplasmic inclusion seen with Giemsa's stain or by
immunofluorescence.
- Organisms can be identified in exudates by fluorescent
antibody staining, ELISA, or by use of DNA probe
(hybridyzation).
- Chlamydiae can be grown in cell culture or embryonated
egg
- Chlamydial antigens can be detected by ELISA.
- Serologic tests reliable in diagnosis of chlamydial
infection but not for C.trachomatis because the frequency
of infection is so high that many people already have
antibodies.
Treatment
- All Chlamydia are susceptible to tetracycline and
erythromycin.
- C.psittaci & C.pneumoniae
tetracycline
- C.trachomatis
sexual infection
azithromycin
- There is no vaccine available against any chlamydial
disease.

Rickettsiae
They are the agents of:
Typhus
R.prowazekii
R.typhi
R.tsutsugamoshi
Rocky Mountain spotted fever
R.rickettsii
Q fever
Coxiella burnetii
Important properties
- Are very short rods, their cell wall resemble that of Gram's
negative but stained poorly.
- Are obligate intracellular parasites
- Rickettsiae devide by binary fission inside host cell but by
a distinctive intracellular cycle.
- Several rickettsiae (R.prowazekii, tsutsugamoshi &
richettsii) posses antigens that cross-react with antigens of
the OX strains of Proteus vulgaris
The Weil-Felix test
anti-richettsial antibodies in
serum will agglutinate Proteus vulgaris.
Pathogenesis
- The life cycle of rickettsiae maintained in nature in certain
arthropods (ticks, fleas and lice)
transmitted to human
by bite of arthropod, except C.burnetti which is
transmitted by aerosol.
- All rickettsial infections are zoonotic only for epidemic
typhus which occur only in humans.
- The typical lesion caused by rickettsiae is a vasculitis
particularly in the endothelial lining.
- Damage of vessels of skin
characteristic rash, edema
and hemorrhage.
- Endotoxin is involved in pathogenesis but no exotoxin or
cytolytic enzymes.
-Typhus begins with the sudden onset of chills, fever, headache
and other influenza like symptoms 1-3 weeks after the louse
bite. A maculopapular rash appear on the trunk 5
th
-9
th
days of
the onset. Signs of sever meningo-encephalitis. In untreated
cases death may occurs from peripheral vascular collapse or
from bacterial pneumonia.
Epidemic typhus
R.prowazekii (louse transmit infection
from person to person)
Endemic typhus
R.typhi (by flea).
Laboratory diagnosis
- Based on serologic analysis rather than isolation of the
organism
- Rickettsiae can be grown in cell culture or embryonated
egg but hazardous.
- CFT provides more specific data.
- Weil-Felix reaction (microagglutination test) based on
cross reaction of antigens in rickittsial disease and with O
antigen (polysaccharide) found in Proteus vulgaris strains
OX-2, O-19 & OX-k. but the test is of limited value.

Yersinia
- Short pleomorphic Gram's negative rods, can exhibit
bipolar staining.
- Mainly microaerophilic, catalase positive and oxidase
negative.
- All are animal pathogens but some can cause bacterial
zoonoses and human infected accidently mainly through
vectors.
Yersinia pestis
Is the cause of plaque (black death)
Antigenic structure & virulence factors
1. Lipopolysaccharide capsule or envelope protein (fraction
1, F-1) with endotoxic activity and antiphagocytosis, loss
of capsule is accompanied by a loss of virulence.
2. V-W antigens-2 proteins encoded by genes on plasmid.
3. Exotoxins that are lethal to animal but with unknown role
in humans.
Two additional correlates of virulence are the formation of
pigmented colonies on certain media and the ability to
synthesize purines.
Pathogenesis & Epidemiology
The zoonotic cycle consist of transmission among wild rodents
by fleas, most rodents are asymptomatic, humans are accidental
hosts. This cycle predominate during time of poor sanitation.

The flea ingests the bacteria while taking blood from bacteremic
rodent
organisms inoculated with the bite
spread to the
regional lymph nodes
swollen and tender (buboes)
bubonic plaque
high concentration in blood
disseminated
form abscess in many organs.
The endotoxin-related symptoms including
disseminated
intravascular coagulation and cutaneous hemorrhages (black
death).
Primary pneumonic plaque may occur by respiratory droplet
transmission of the organisms from patients with pneumonic
plaque or secondary pneumonic plaque from septic emboli that
can reach the lungs.
Laboratory diagnosis
- Specimens may be stool, blood, pus or material obtained
from bubo. Sputum in pneumonic plaque.
- Staining of smear by Giemsa's stain reveal typical safety
pin appearance also flourescent antibody staining can be
used.
- Culture is the best diagnostic method where they usually
increase the small amount of micro-organisms by cold
enrichment (buffer saline at 4
o
C for 2-4 weeks), then
placed on MacConkey.
- Serology-at or after two weeks
rise of agglutinating
antibodies (against envelope antigens)
can be detected
but cross reaction may confuse the results.

Treatment
- The choice is usually combination of Streptomycin and
tetracycline.
- No significant antibiotic resistance.
- Treatment should not wait for the results of bacteriologic
culture.
Prevention
1. Controlling the spread.
2. Isolation of suspected cases
3. Treatment of contacts with tetracycline.
4. A vaccine of formalin-killed organisms provides partial
protection against bubonic plaque (not pneumonic).
Yersinia enterocolitica
Yersinia pseudotuberculosis
Those are domestic animal pathogens but can cause human
diarrheal disease by accidental ingestion of micro-organisms.

Francisella tularensis
Are animal pathogens, transmissible to humans by arthropods
bites and direct contact with infected animal tissues, inhalation
of aerosols or ingestion of contaminated food or water
Tularemia.
Pasteurella multocida
Causes wound infection associated with cat and dog bites
(organisms are normal flora of mouth of many animals)
rapid
cellulitis.
Osteomylitis
cat sharp teeth implant micro-organisms under
the periosteum.
Cat bite should not be sutured and prophylactic Ampicillin must
be given.
Bacteroids species
- Very important anaerobic Gram's negative bacilli
- Normal flora of the bowel and genital tract.
- Usually associated with intra-abdominal suppuration in
association with anaerobic cocci and bacilli as
Peptostreptococcus and Clostridia.
- Isolated under anaerobic conditions.
- Treated by Clindamycin and Metronidazole.
Mycoplasmas
Are a group of small, wall-less organisms of which Mycoplasma
pneumoniae is the major pathogen.
Mycoplasma pneumoniae
atypical pneumonia
Important properties
- Mycoplasma are the smallest free-living organisms (
0.3/
m)
- Absence of a cell wall
stain poorly with Gram's stain.
And antibiotics that inhibit cell wall synthesis are
ineffective.
- Pleomorphic
a flexible 3-layer cell membrane
- Mycoplasmas can grow on artificial media (including
several lipids)
grow slowly (1week)
visible colony
"fried egg" shape.
Pathogenesis & Epidemiology
- Only human pathogen transmitted by respiratory droplets.
- In the lungs, the organism is rod-shaped with a tapered tip
that contains specific proteins attached to the respiratory
epithelium. The mucosa not invaded but ciliary motion is
inhibited
necrosis of epithelium.
- M.pneumonia has one serotype but immunity is
incomplete, auto-antibodies produced during infection
(cold agglutinins) against red blood cells and brain, lung
and liver cells
extra pulmonary manifestations.

- Infections occur worldwide, increasing in winter effect
mostly young adults, outbreaks occur in groups of close
contact. 10% of infected individuals develop pneumonia.
Clinical findings
Most common cause of atypical pneumonia,
(causative bacterium can not be isolated on routine lab media
and the disease does not resemble pneumococcal pneumonia)
- The onset is gradual, begins with non-productive cough,
sore throat, or earache
then produce whitish, non-
bloody sputum.
- Constitutional symptoms (fever, headache, malaise and
myalgias) are pronounced.
- The disease resolves spontaneously in 10-14 days.
Laboratory Diagnosis
- Culturing sputum sample may take at least 1 week and
need special media.
- Serological test
cold agglutinin titer
1:128
recent
infection
IgM auto antibodies against type O RBC
agglutination at 4
o
C
(Non specific)
false positive
influenza virus
_ adenovirus
- Infection can be confirmed by 4-fold rise in specific
antibody titer in CFT.

Treatment
- Usually erythromycin or tetracycline
Shorten the duration
- Disease resolve by it self
- Penicillins and Cephalosporins are inactive
Other mycoplasmas
M.hominis
infrequent cause of pelvic inflammatory
disease
Ureaplasma urealyticum
one of several causes of non
gonococcal urethritis.
