
G
G
e
e
n
n
u
u
s
s
N
N
e
e
i
i
s
s
s
s
e
e
r
r
i
i
a
a
De p a rt m e n t o f Mi c r o b i o l o g y
Co l l e g e o f Me d i c i n e
Ba g h d a d U n i v e rs i t y
Le c . 4 , 2 0 14 - 2 0 15
Dr. S a r m a d M.H. Ze i n y
Objectives:
• De s c ri be t he
m o r p h o l o g y & p h y s i o l o g y
f o r g e n us
Ne i s s e ri a .
• De t e rmi ne t he
v i rul e n c e f a c t o rs
f o r g e n us
Ne i s s e ri a .
• An a l y ze t he
d i s e a s e s &p a t h o g e n i c i t y
f o r g e n us
Ne i s s e ri a .
• De mo n s t ra t e t he
e p i d e m i o l o g y / t ra n s m i s s i o n
f o r
g e n us Ne i s s e ri a .
• Out l i n e t h e
l a b o ra t o ry d i a g n o s i s
f o r g e n us
Ne i s s e ri a .
• S t a t e t h e
d rug o f c h o i c e a n d p r o p h y l a xi s
wh e r e
r e g ul a rl y us e d .
Genus neisseria
•
P
P
A
A
T
T
H
H
O
O
G
G
E
E
N
N
I
I
C
C
:
:
•
N
N
O
O
N
N
-
-
P
P
A
A
T
T
H
H
O
O
G
G
E
E
N
N
I
I
C
C
:
:
ž
N. gonorrhoeae
(gonococci, G.C).
ž
N. meningitidis
(meningococci).
ž
N. catarrhalis.
ž
N. sicca,
others
General characteristics
ž
G
G
–
–
v
v
e
e
d
d
i
i
p
p
l
l
o
o
c
c
o
o
c
c
c
c
i
i
,
,
k
k
i
i
d
d
n
n
e
e
y
y
(
(
c
c
o
o
f
f
f
f
e
e
e
e
b
b
e
e
a
a
n
n
)
)
s
s
h
h
a
a
p
p
e
e
,
,
w
w
i
i
t
t
h
h
f
f
l
l
a
a
t
t
o
o
p
p
p
p
o
o
s
s
i
i
n
n
g
g
e
e
d
d
g
g
e
e
.
.
ž
A
A
l
l
l
l
m
m
e
e
m
m
b
b
e
e
r
r
s
s
a
a
r
r
e
e
O
O
x
x
i
i
d
d
a
a
s
s
e
e
p
p
o
o
s
s
i
i
t
t
i
i
v
v
e
e
.
.
ž
P
P
a
a
t
t
h
h
o
o
g
g
e
e
n
n
i
i
c
c
t
t
o
o
h
h
u
u
m
m
a
a
n
n
o
o
n
n
l
l
y
y
.
.
ž
F
F
e
e
r
r
m
m
e
e
n
n
t
t
c
c
a
a
r
r
b
b
o
o
h
h
y
y
d
d
r
r
a
a
t
t
e
e
s
s
a
a
c
c
i
i
d
d
o
o
n
n
l
l
y
y
.
.
ž
P
P
y
y
o
o
g
g
e
e
n
n
i
i
c
c
:
:
p
p
r
r
o
o
d
d
u
u
c
c
e
e
p
p
u
u
s
s
.
.
ž
N
N
o
o
n
n
–
–
h
h
a
a
e
e
m
m
o
o
l
l
y
y
t
t
i
i
c
c
s
s
.
.
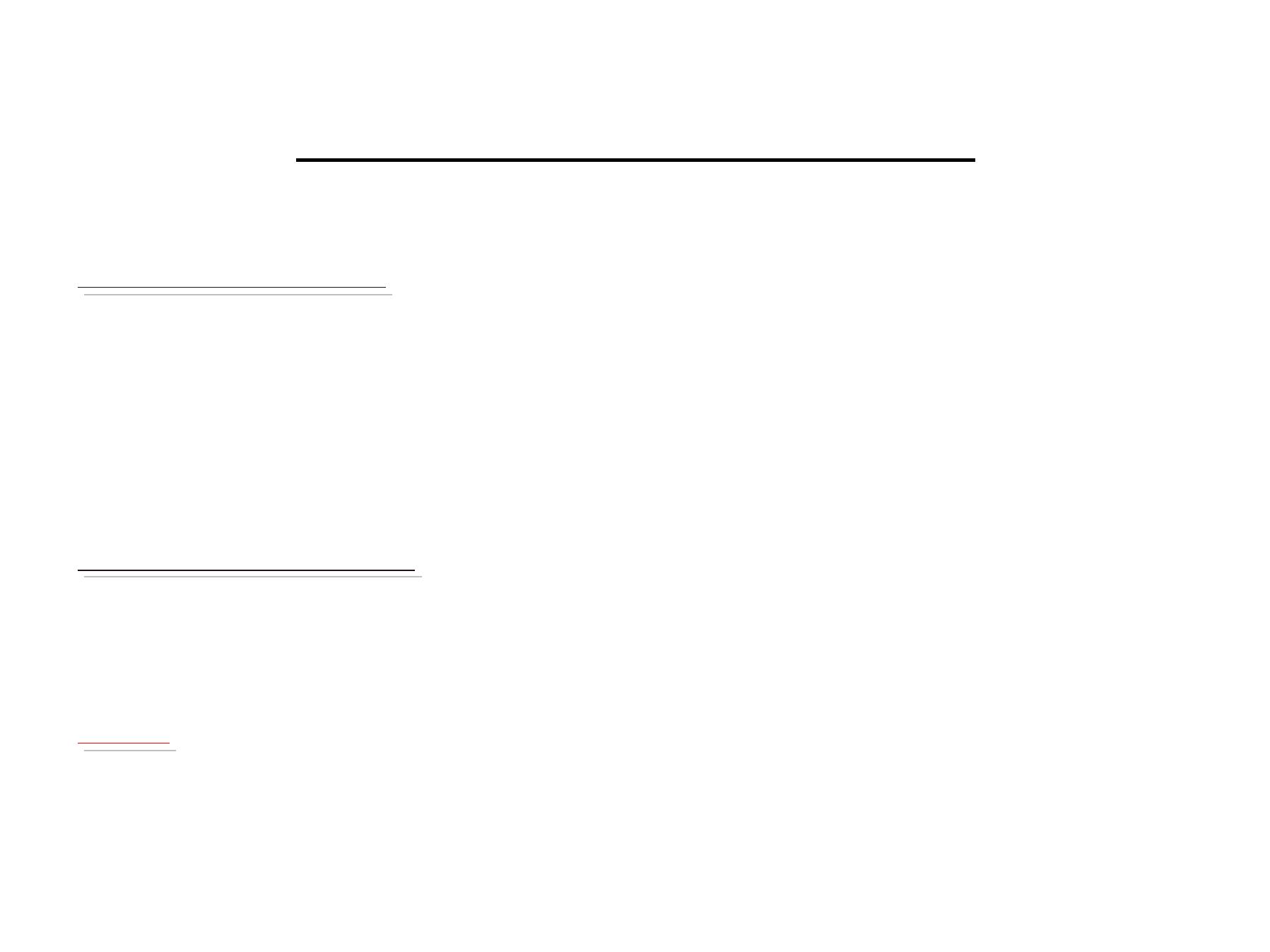
Continuation of general
characteristics
•Intracellular &/ or extracellular.
•Needs 48h of culturing time.
•They are rapidly killed by drying, sunlight and
many disinfectants.
•70%DNA homology and are differentiated by
few LAB tests.
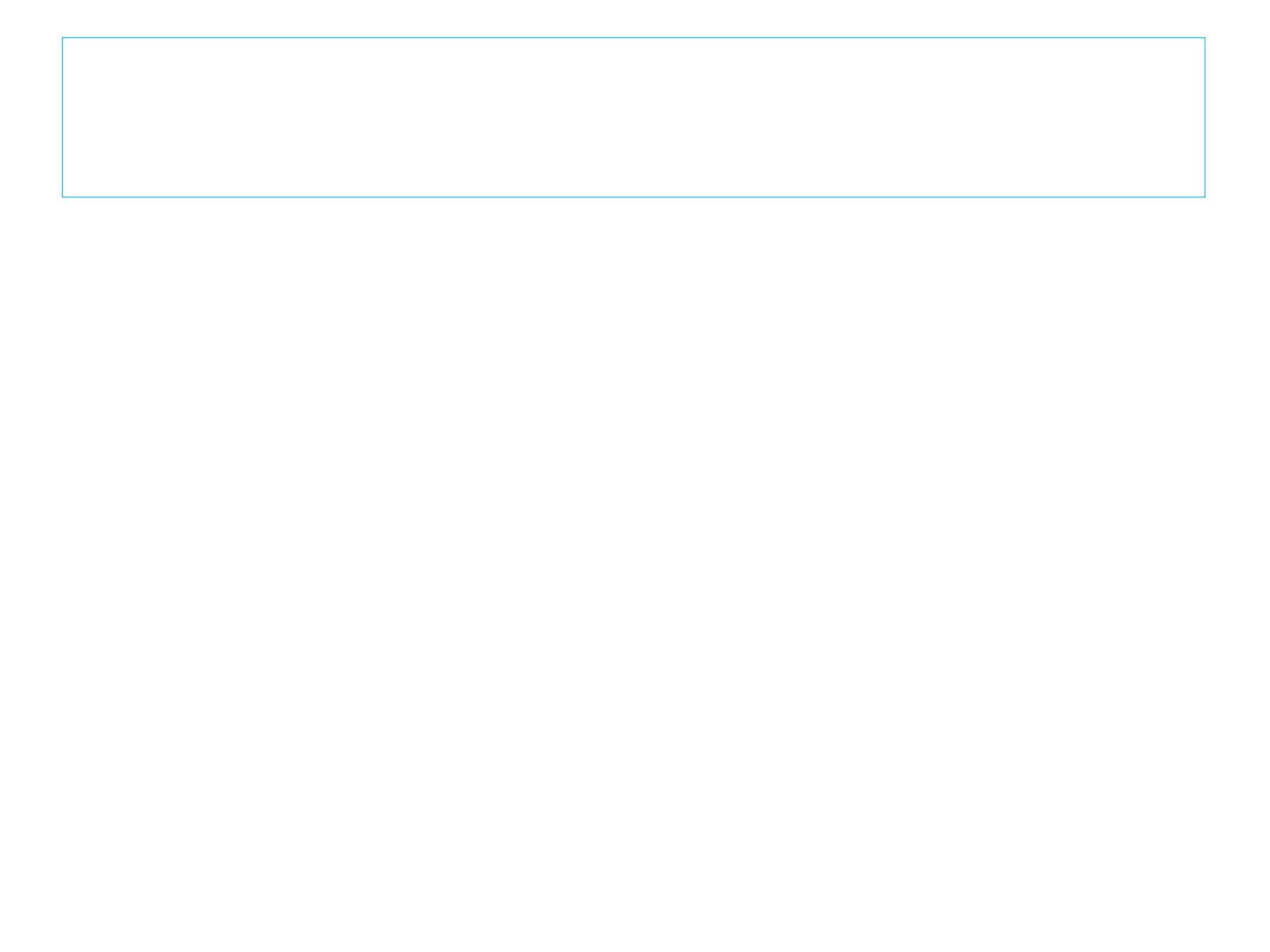
Gram’
s negative
Diplo cocci
K
K
i
i
d
d
n
n
e
e
y
y
(
(
c
c
o
o
f
f
f
f
e
e
e
e
b
b
e
e
a
a
n
n
)
)
s
s
h
h
a
a
p
p
e
e
w
w
i
i
t
t
h
h
f
f
l
l
a
a
t
t
o
o
p
p
p
p
o
o
s
s
i
i
n
n
g
g
e
e
d
d
g
g
e
e
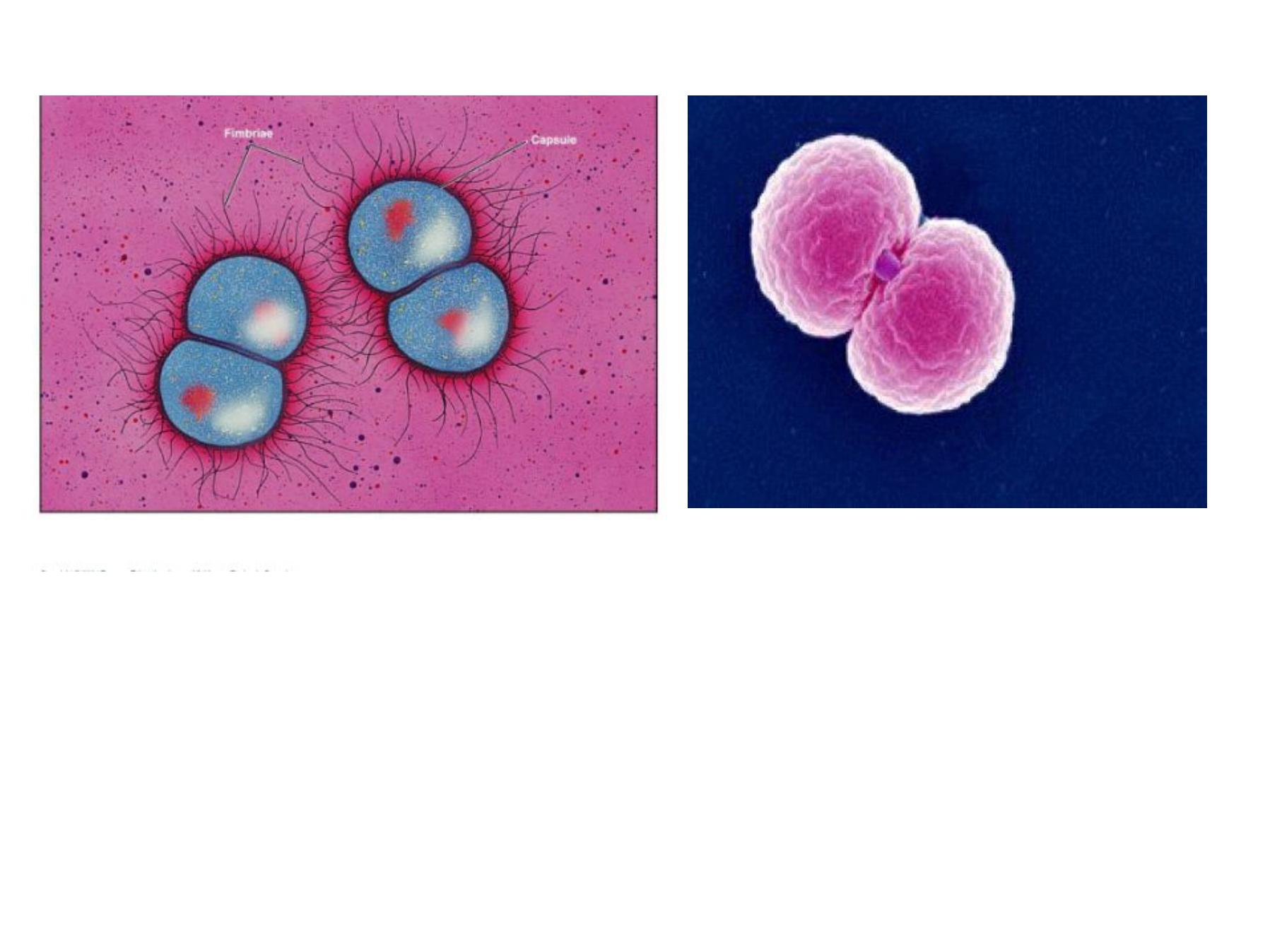
Neisseria
Neisseria attached to lymphocyte
By Electronic Microscopy
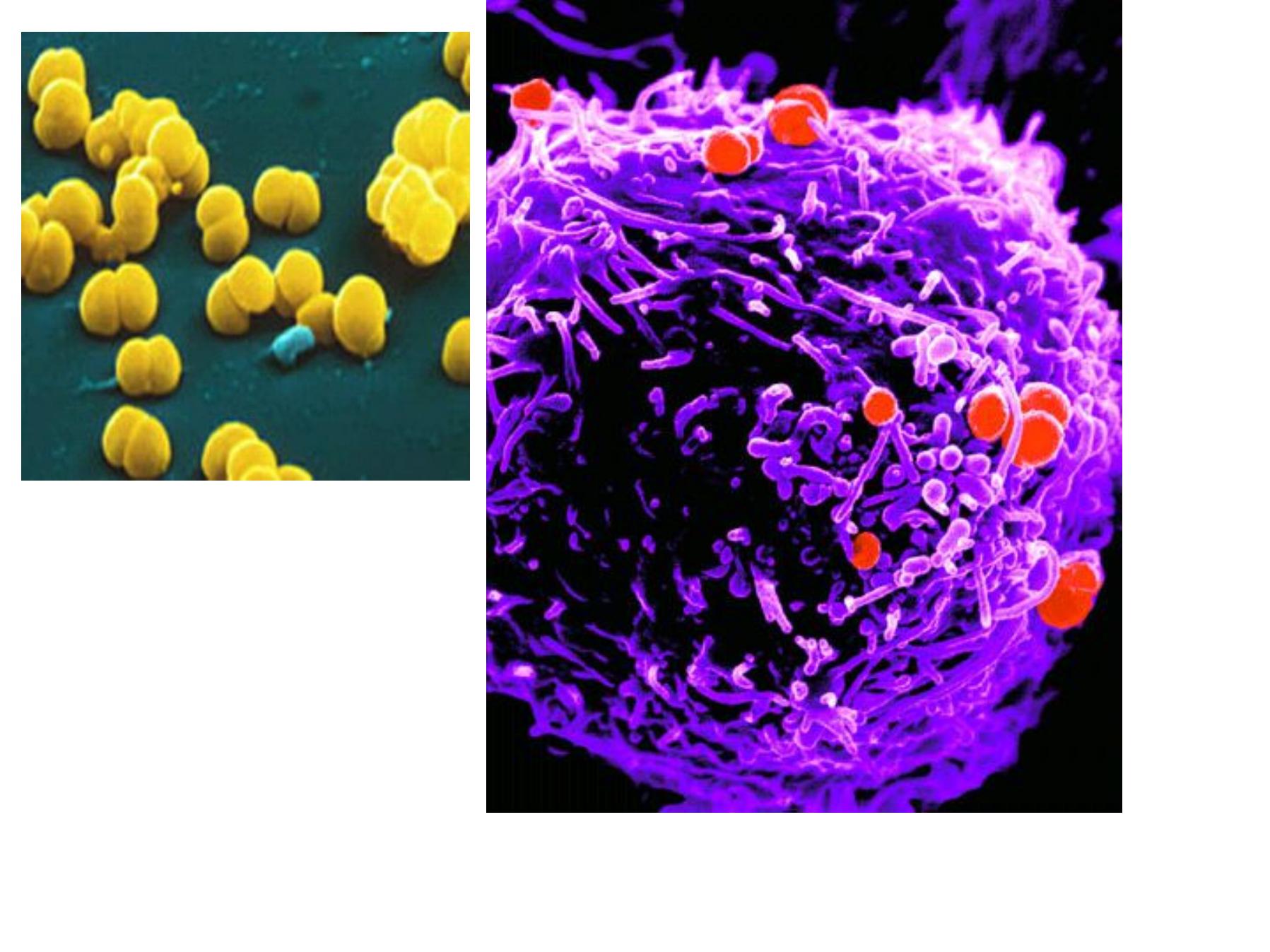
Direct Gram’
s staining slide from urethral swab
Neisseria gonorrhoeae (gonococcus)
Reservoir: human genitaltract
•
Transmission
• Sexualcontact, birth
• Sensitive to drying and cold
•
Disease: à gonorrhea (STD)
• Localized infection.
• Systemic infection.
Gonorrhea
Local
Urethritis
Cervicitis
Vaginitis
salpingitis
&
PID
Proctitis
ophthalmia
neonatorum
Gonorrhea
Systemi
c
Arthritis
meningitis
Endocarditi
s
vasculitis

Ophthalmia neonatorum
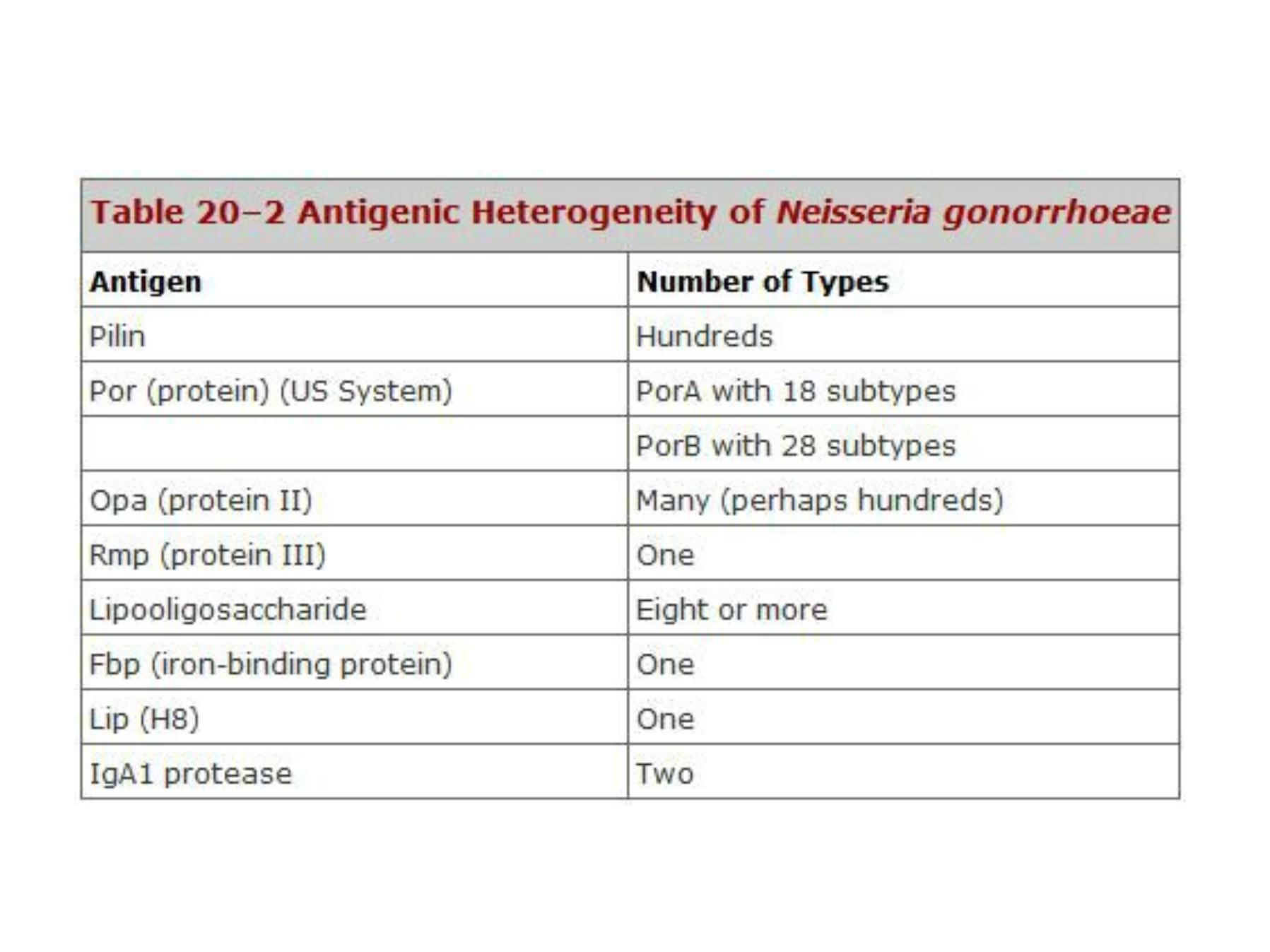
Antigenic & Virulence structures:
1)
Pilli:
• Attachment to mucosalsurfaces.
• Inhibit phagocytic uptake.
• Antigenic (immunogenic) variation:> 1million variants
2) Porin (por) protein (protein I):
3) Opacity (Opa) proteins (protein II): Attachment
4) RMP (protein III):
• It is associated with (Opa) protein in the formation of
pores.
5) Lipooligosaccharide (LOS): endotoxic effect.
6) IgA protease.
7) Other proteins: L ip ( H8), Fbp (ferric binding protein)
Porin (por) protein:
• Extends through the gonococcal cell membrane.
• Por proteins may impact intracellular killing of gonococci
within neutrophils
by preventing phagosome-lysosome
fusion.
• In addition, variable resistance of gonococci to killing by
normal human serum depends upon whether Por protein
selectively
binds to complement components C3b and
C4b
.
• Each strain of gonococcus expresses only one of two
types of Por, but the Por of different strains is antigenically
different.
• Serologic typing of Por by agglutination reactions with
monoclonal antibodies has distinguished
18 serovars of
PorA and 28 serovars of PorB.
Lipooligosaccharide:
• It has endotoxic effect and it is responsible for
toxicity of gonococci.
• Gonococci can express
more than one
antigenically different lipooligosaccharide
(LOS)
chain simultaneously.
• In a form of molecular mimicry, gonococci make
L OS molecules that structurally resemble human
cell membrane glycosphingolipids
.
• The presence on the gonococcal surface of the
same surface structures as human cells helps
gonococci evade immune recognition.
Treatment
• More than 20 percent of current isolates of N. gonorrhoeae are
resistant to penicillin, tetracycline, cefoxitin, and/or spectinomycin.
Penicillin-resistant organisms are called PPNG—penicillinase
producing N. gonorrhoeae. These strains contain plasmids that carry
the gene for β-lactamase.
• However, most organisms still respond to treatment with third-
generation cephalosporins; for example, a single intramuscular dose
of ceftriaxone is the recommended therapy for uncomplicated
gonococcal infections.
• Intramuscular spectinomycin is indicated in patients who are allergic
to cephalosporins.
• Additional therapy with azithromycin 1g orally in a single dose or
with doxycycline 100 mg orally twice a day for 7 days is
recommended for the possible concomitant chlamydial infection.
Azithromycin has been found to be safe and effective in pregnant
women, but doxycycline is contraindicated.
Prevention of gonorrhea :
• The infectivity of the organism is such that the chance of
acquiring infection from a single exposure to an infected sexual
partner is 20–
30% for men and even greater for women.
• Avoiding multiple sexual partners.
• Rapidly eradicating gonococci from infected individuals by
means of early diagnosis and treatment, and finding cases and
contacts through education and screening of populations at
high risk.
• Mechanical prophylaxis (condoms) provides partial protection.
• Chemoprophylaxis is of limited value because of the rise in
antibiotic resistance of the gonococcus.
• Gonococcal ophthalmia neonatorum is prevented by local
application of 0.5% erythromycin ophthalmic ointment or 1%
tetracycline ointment to the conjunctiva of newborns.
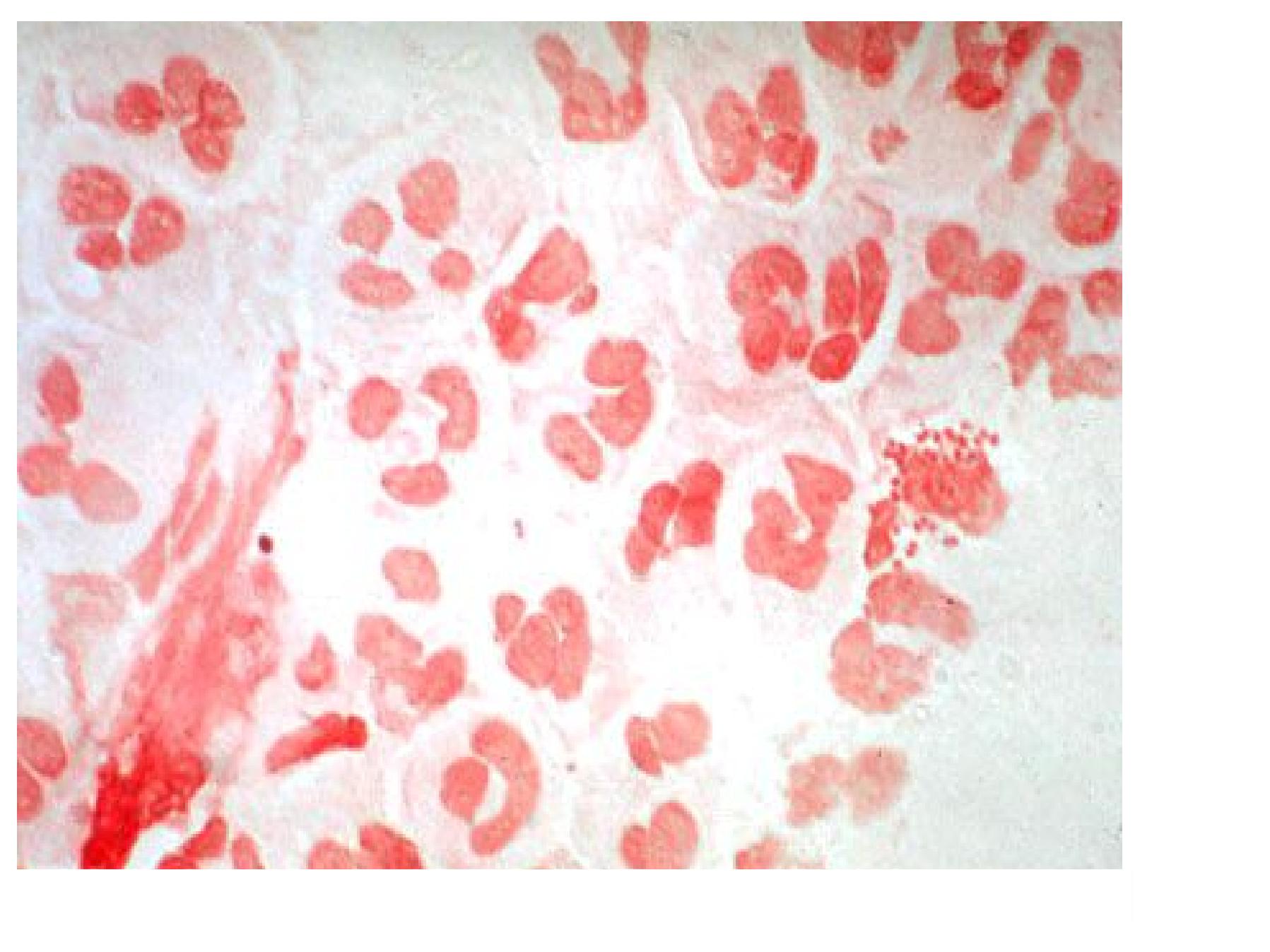
Neisseria meningitidis
(meningococcus)
Distinguishing Features
• Gram- negative, kidney coffee bean- shaped diplococci.
• Large capsule, Antigenic.
• Grows on chocolate (not blood) agar in 5 % C0 2
atmosphere.
• Ferments maltose in contrast to gonococci.
Reservoir
: human nasopharynx (5 - 10 % carriers).
Transmission:
• Respiratory droplets; oropharyngealcoloniz ation,
spreads to the meninges via the bloodstream
Antigenic & Virulence structures:
1) Capsule
: At least 13 serogroups most
important serogroups are A,B,C,Y, W135 .
2) Outer membrane protein (OMP):
about 20
antigenic types, used for serotyping.
3) Pilli:
attachment
4) IgA protease
: cleaves IgA
5) Opa protein
: attachment
6) Lipooligopolysaccharide (Endotoxin
) : fever,
septic shock in meningococcemia.
Q
Q
)
)
A
A
n
n
s
s
w
w
e
e
r
r
w
w
i
i
t
t
h
h
t
t
r
r
u
u
e
e
o
o
r
r
f
f
a
a
l
l
s
s
e
e
:
:
T
T
h
h
e
e
i
i
m
m
p
p
o
o
r
r
t
t
a
a
n
n
t
t
C
C
r
r
i
i
t
t
e
e
r
r
i
i
a
a
f
f
o
o
r
r
g
g
e
e
n
n
u
u
s
s
N
N
e
e
i
i
s
s
s
s
e
e
r
r
i
i
a
a
a
a
r
r
e
e
:
:
a. Gram –
ve diplococci.
b. Kidney shaped diplococci.
c. Oxidase positive.
The answer: all above are true.
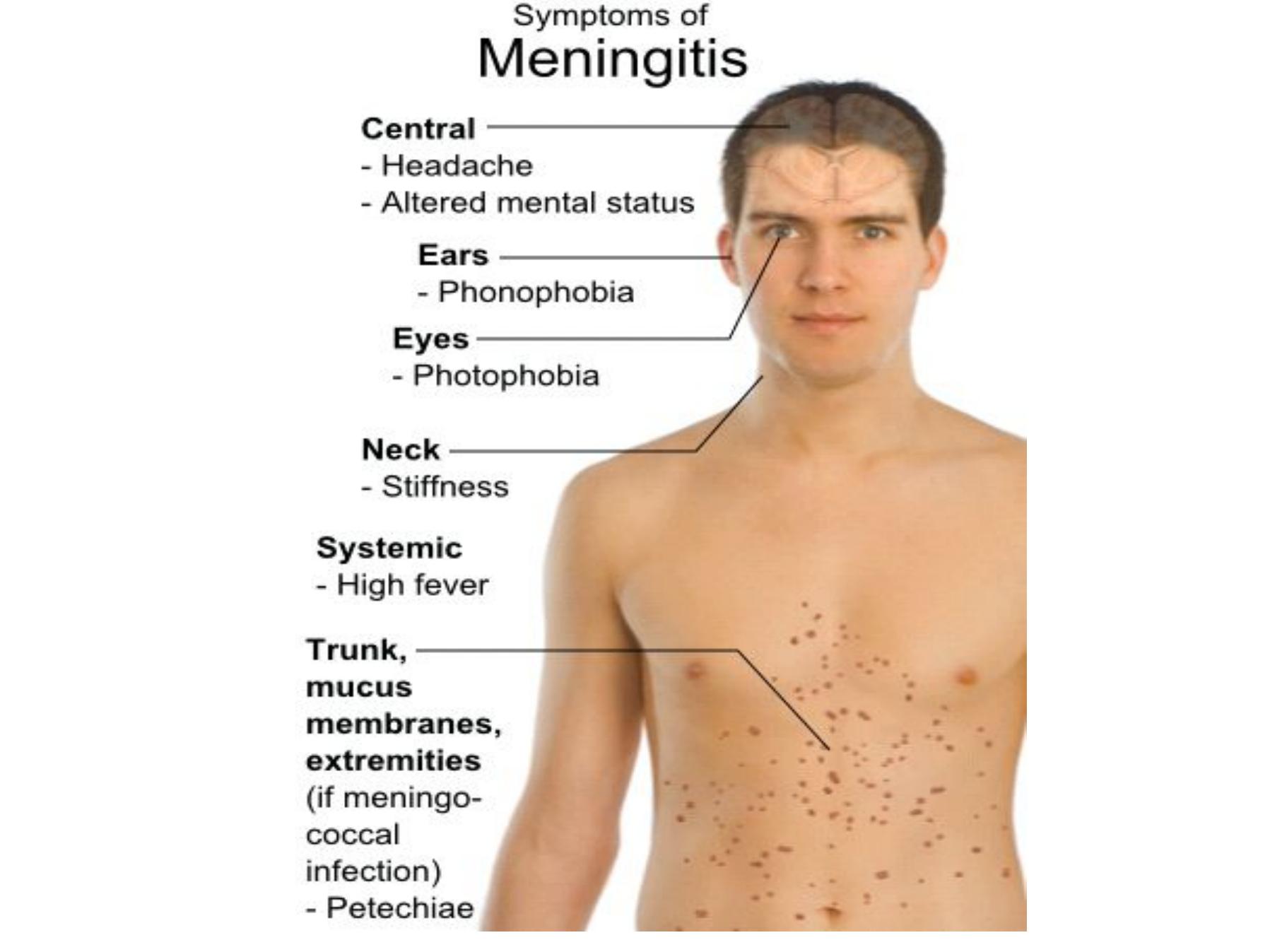
Diseases & Pathogenicity
• The source of the infection is either the patient
or the carriers.
• The route of entry is through the nasopharynx
by droplet.
•Attach to the epithelia then spread through the
blood stream:
a. Meningitis:
mainly in adult ages 11to 55 years.
b. Fulminating meningococcemia.

Fulminating meningococcemia
Risk factors :
1) Recent viral or mycoplasma upper
respiratory tract infection,
2) Active or passive smoking, and
3) Complement deficiency (C5-C8).
Treatment:
•Medical emergency.
•Penicillin Gis the drug of choice.
•Chloramphenicol and cefotaxime (or
ceftriaxone) can be used.
Prevention
Ø Irradiation of the carrier states (major source).
Ø Isolation of the patient.
Ø Chemoprophylaxis for contact people.
Ø
Vaccination
:
A conjugate meningococcal vaccine
(MCV4) used in adolescents and adults ages 11
to 55 years. Against A, C, W-135, and Y
conjugated to diphtheria toxoid.
Vaccination
Vaccination is recommended for persons 11–
55 years
of age who are among the following
a
a
t
t
-
-
r
r
i
i
s
s
k
k
g
g
r
r
o
o
u
u
p
p
s
s
:
:
• Persons with functional or surgical asplenia;
• persons with complement deficiencies;
• travelers to highly endemic areas (eg, sub-Saharan
Africa);
• “
Closed populations" such as military and for
• Clinical laboratory workers (microbiologists).
M
M
o
o
r
r
a
a
x
x
e
e
l
l
l
l
a
a
c
c
a
a
t
t
a
a
r
r
r
r
h
h
a
a
l
l
i
i
s
s
•N eisseria catarrhalis, B ranhamella and now they
are a separated genus “M oraxella”.
•Normally found in upper respiratory tract
especially among school children. (5 0 % of
school children carry this microorganism)
•M ay cause pneumonia, otitis media, sinusitis and
other infections.
•Oxidase positive.
•Non fastidious organisms à can grow on nutrient
agar.
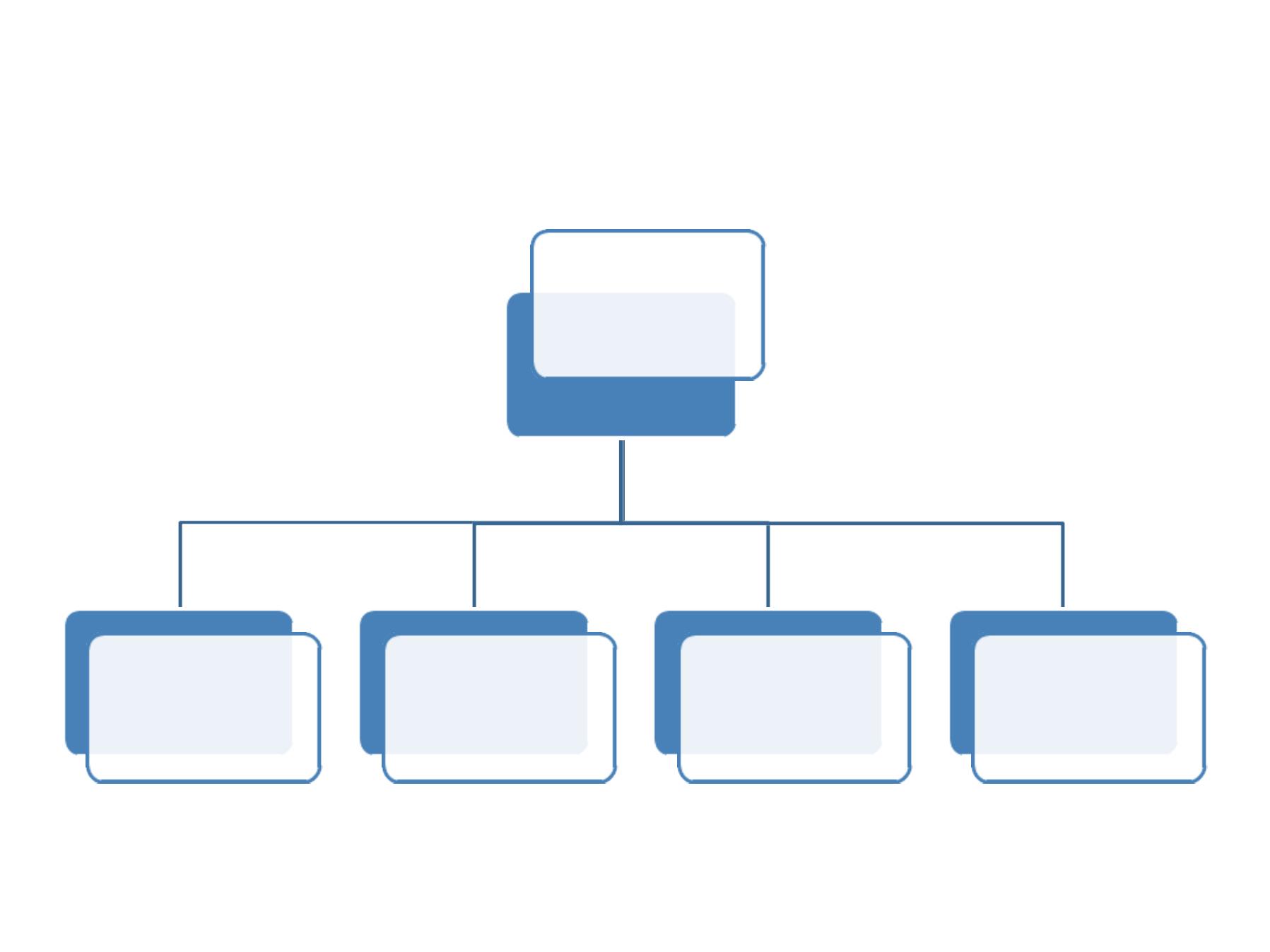
Specimens
Direct Gram’
s
Slide
Culture
Biochemical
Serology
Antibiotics
sensitivity
L
L
a
a
b
b
o
o
r
r
a
a
t
t
o
o
r
r
y
y
D
D
i
i
a
a
g
g
n
n
o
o
s
s
i
i
s
s
s
s
t
t
e
e
p
p
s
s
Laboratory Diagnosis:
1
1
)
)
S
S
p
p
e
e
c
c
i
i
m
m
e
e
n
n
s
s
:
:
•
C
C
S
S
F
F
,
,
B
B
l
l
o
o
o
o
d
d
,
,
t
t
h
h
r
r
o
o
a
a
t
t
s
s
w
w
a
a
b
b
à
à
m
m
e
e
n
n
i
i
n
n
g
g
o
o
c
c
o
o
c
c
c
c
a
a
l
l
i
i
n
n
f
f
.
.
•
H
H
i
i
g
g
h
h
v
v
a
a
g
g
i
i
n
n
a
a
l
l
s
s
w
w
a
a
b
b
,
,
u
u
r
r
e
e
t
t
h
h
r
r
a
a
l
l
d
d
i
i
s
s
c
c
h
h
a
a
r
r
g
g
e
e
a
a
n
n
d
d
u
u
r
r
i
i
n
n
e
e
d
d
e
e
p
p
o
o
s
s
i
i
t
t
à
à
G
G
.
.
C
C
.
.
i
i
n
n
f
f
.
.
2
2
)
)
G
G
r
r
a
a
m
m
'
'
s
s
s
s
t
t
a
a
i
i
n
n
:
:
•
G
G
–
–
v
v
e
e
,
,
d
d
i
i
p
p
l
l
o
o
c
c
o
o
c
c
c
c
i
i
•
I
I
n
n
t
t
r
r
a
a
c
c
e
e
l
l
l
l
u
u
l
l
a
a
r
r
&
&
/
/
o
o
r
r
e
e
x
x
t
t
r
r
a
a
c
c
e
e
l
l
l
l
u
u
l
l
a
a
r
r
.
.
N
N
o
o
t
t
e
e
:
:
U
U
r
r
e
e
t
t
h
h
r
r
a
a
l
l
s
s
w
w
a
a
b
b
f
f
o
o
r
r
m
m
a
a
l
l
e
e
i
i
s
s
d
d
i
i
a
a
g
g
n
n
o
o
s
s
t
t
i
i
c
c
,
,
b
b
u
u
t
t
H
H
i
i
g
g
h
h
v
v
a
a
g
g
i
i
n
n
a
a
l
l
s
s
w
w
a
a
b
b
f
f
o
o
r
r
f
f
e
e
m
m
a
a
l
l
e
e
n
n
e
e
e
e
d
d
c
c
o
o
n
n
f
f
i
i
r
r
m
m
a
a
t
t
i
i
o
o
n
n
,
,
w
w
h
h
y
y
?
?
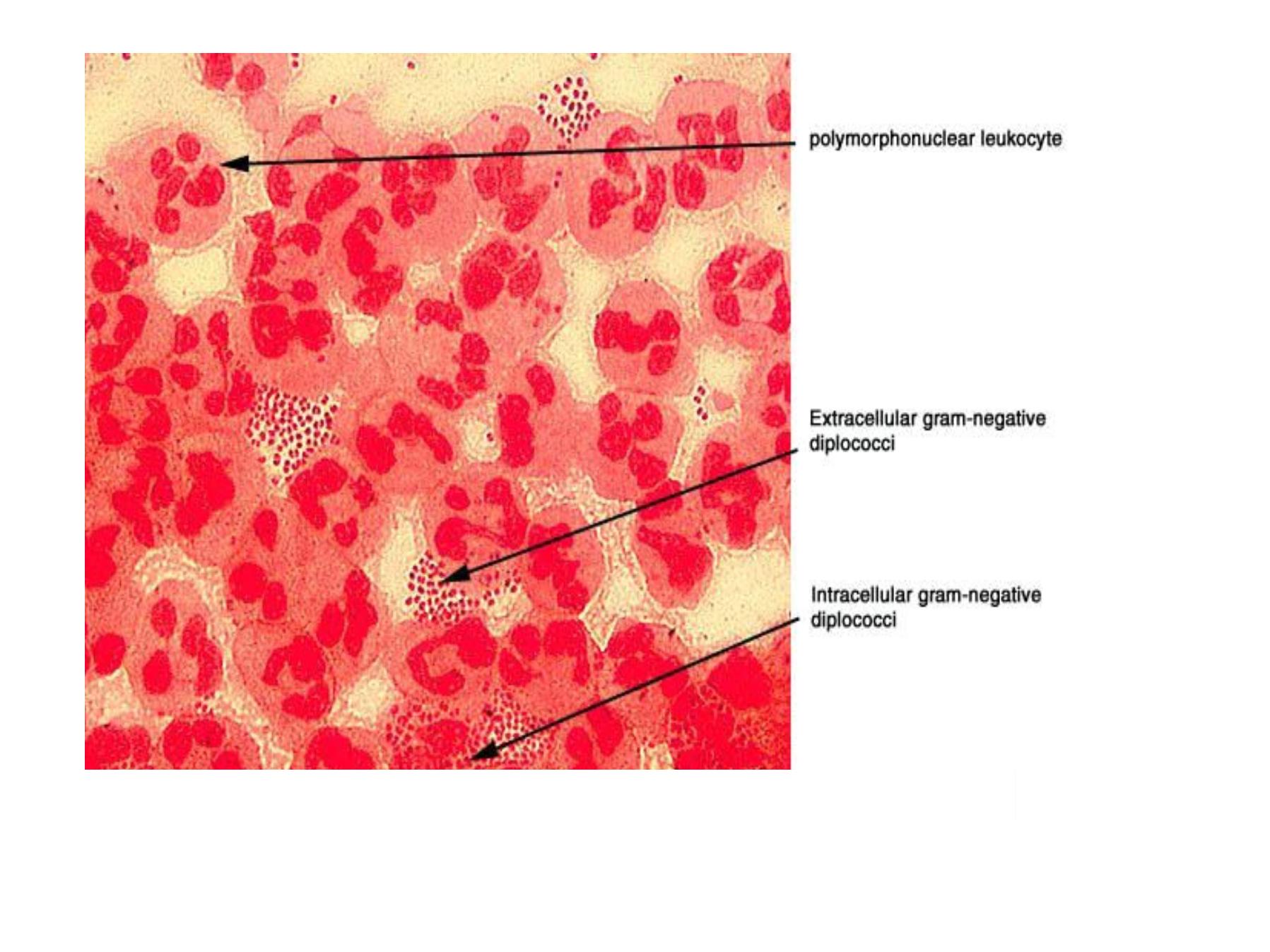
Direct Gram’
s staining slide from urethral swab
Gram’
s staining slide for urethral discharge

3
3
)
)
C
C
U
U
L
L
T
T
U
U
R
R
E
E
:
:
•Pathogenic fastidious need
chocolate agar, selective media.
•Non –pathogenic non fastidious
can grow on nutrient media.
Selective media for Neisseria
A. Thayer Martin (TM).
B. Modified Thayer Martin.
C. Martin –Lewis (ML).
D. New York City (NYC).
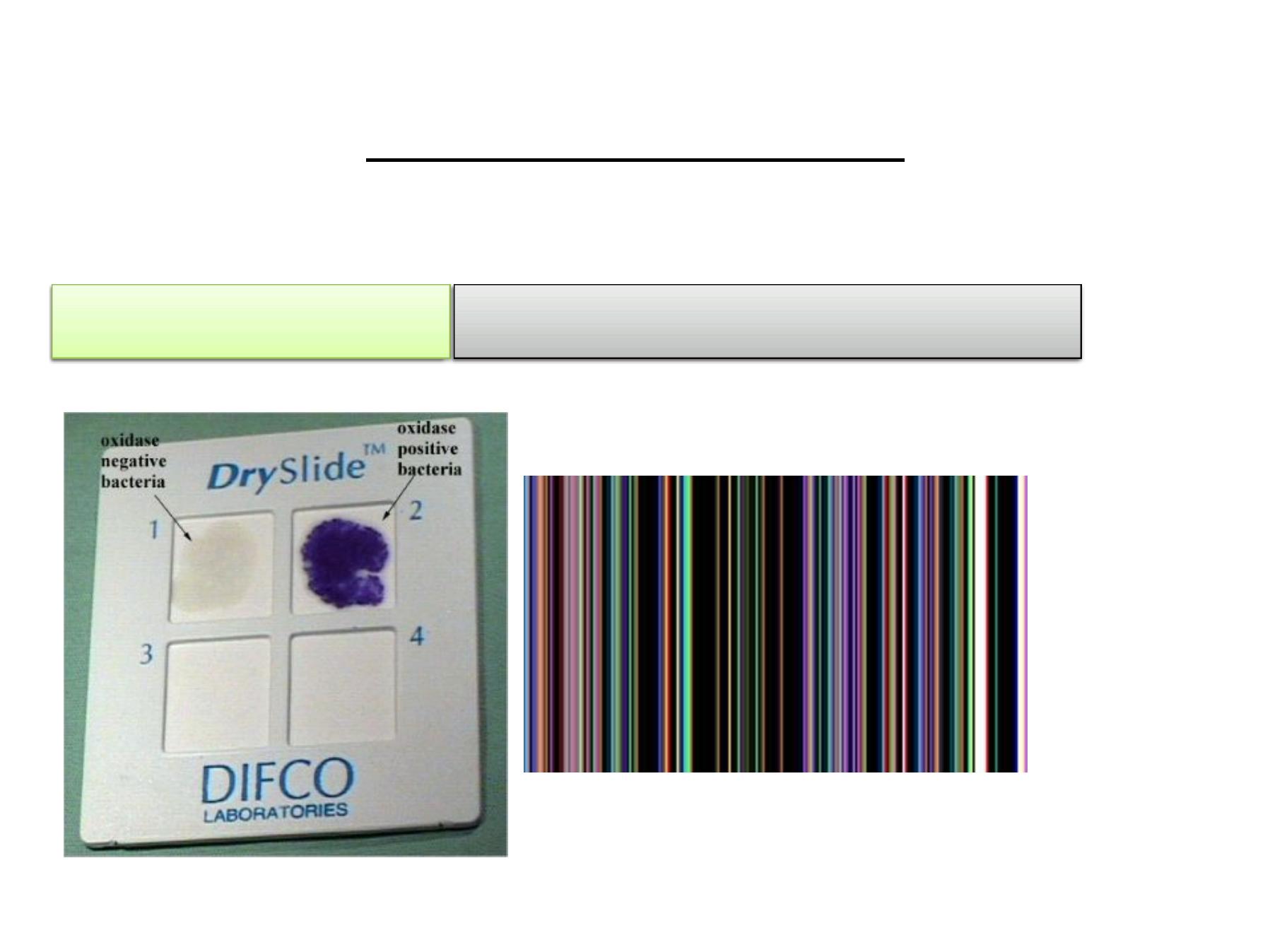
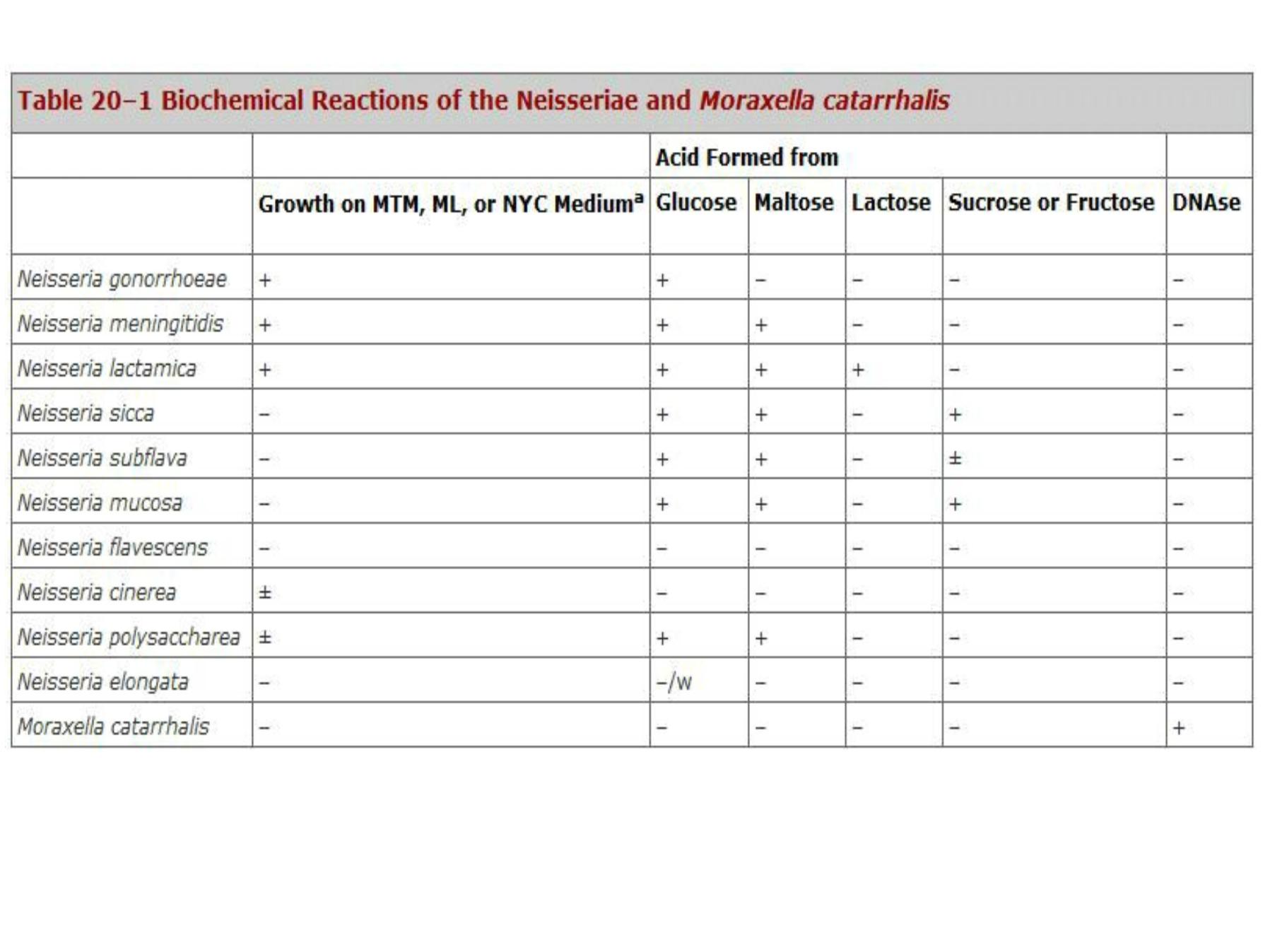
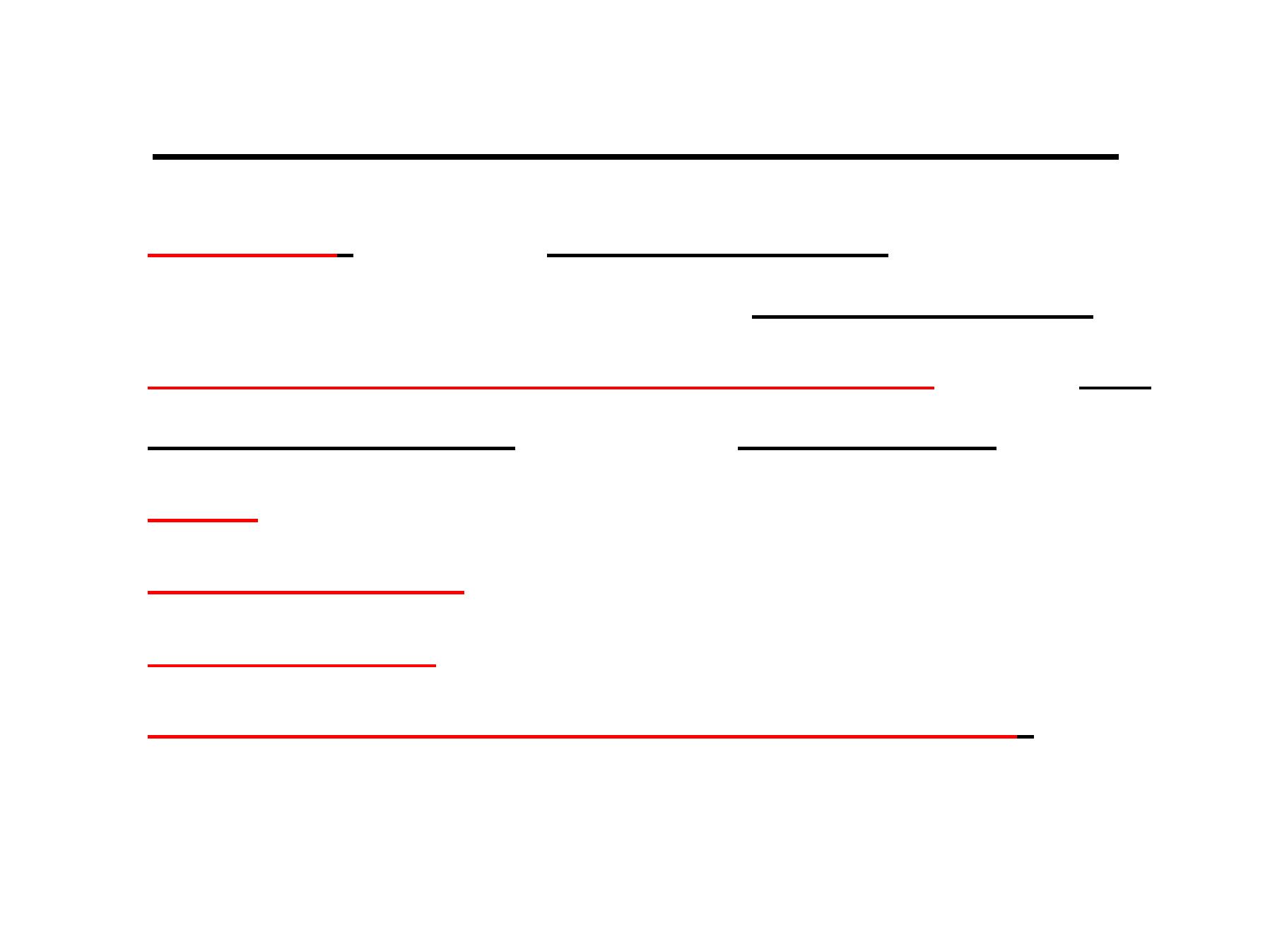
Biochemical tests
1
1
)
)
O
O
x
x
i
i
d
d
a
a
s
s
e
e
t
t
e
e
s
s
t
t
+
+
v
v
e
e
f
f
o
o
r
r
a
a
l
l
l
l
N
N
e
e
i
i
s
s
s
s
e
e
r
r
i
i
a
a
s
s
p
p
p
p
.
.
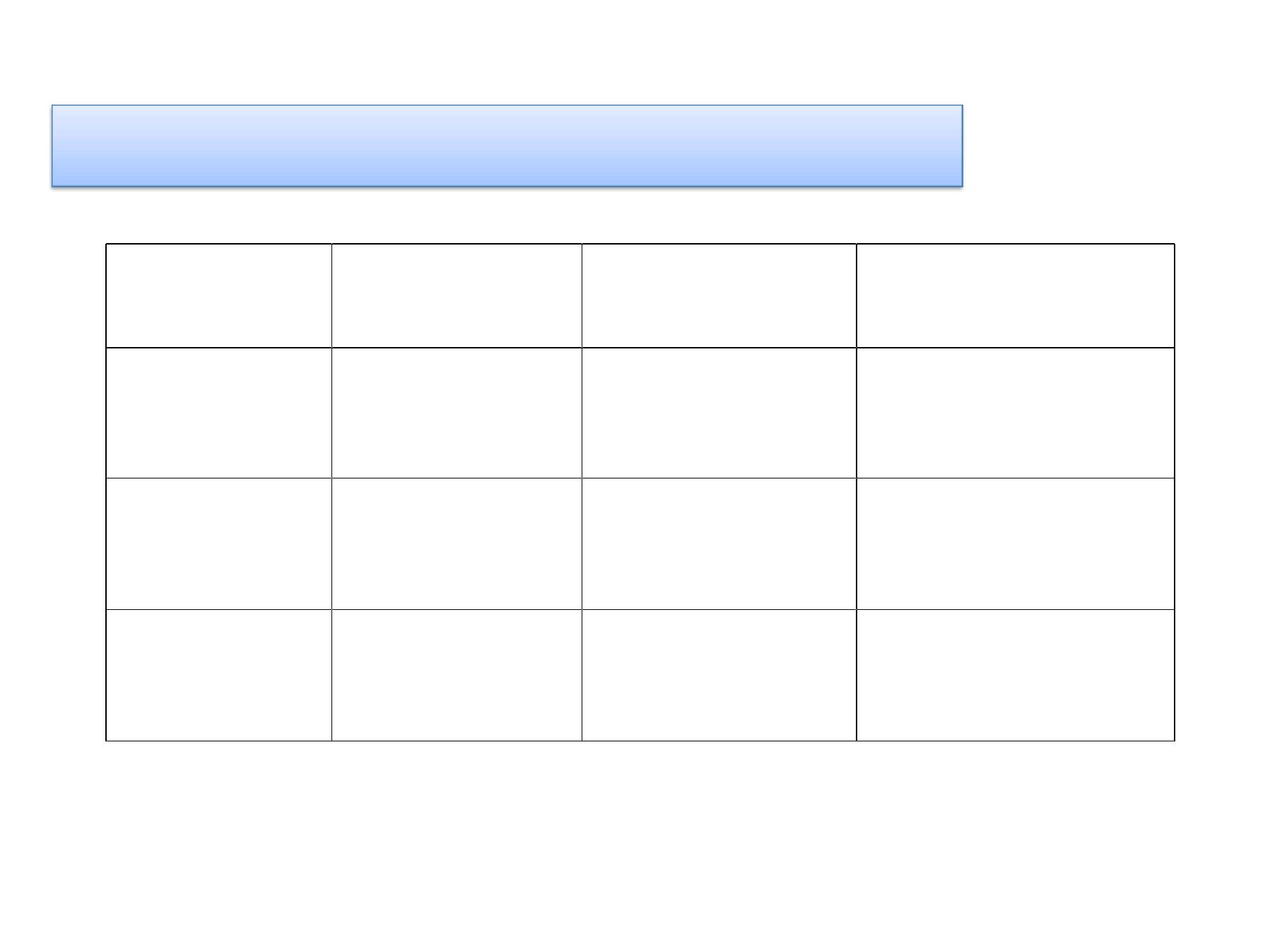
2
2
)
)
S
S
u
u
g
g
a
a
r
r
f
f
e
e
r
r
m
m
e
e
n
n
t
t
a
a
t
t
i
i
o
o
n
n
t
t
e
e
s
s
t
t
S
S
u
u
c
c
r
r
o
o
s
s
e
e
M
M
a
a
l
l
t
t
o
o
s
s
e
e
G
G
l
l
u
u
c
c
o
o
s
s
e
e
N
N
.
.
s
s
p
p
p
p
.
.
ـــ
ـــ
+
+
+
+
N
N
.
.
m
m
e
e
n
n
i
i
n
n
g
g
i
i
t
t
i
i
d
d
i
i
s
s
ـــ
ـــ
ـــ
ـــ
+
+
N
N
.
.
g
g
o
o
n
n
o
o
r
r
r
r
h
h
o
o
e
e
a
a
ـــ
ـــ
ـــ
ـــ
ـــ
ـــ
N
N
.
.
c
c
a
a
t
t
a
a
r
r
r
r
h
h
a
a
l
l
i
i
s
s
3) DNAse test:
+
+
v
v
e
e
ðà
ðà
M
M
o
o
r
r
a
a
x
x
e
e
l
l
l
l
a
a
c
c
a
a
t
t
a
a
r
r
r
r
h
h
a
a
l
l
i
i
s
s
.
.
-
-
v
v
e
e
ðà
ðà
O
O
t
t
h
h
e
e
r
r
N
N
e
e
i
i
s
s
s
s
e
e
r
r
i
i
a
a
s
s
p
p
p
p

HOW DIFFERENTIATE BETWEEN PATHOGENIC AND NON
PATHOGENIC Neisseria?
1) Sugar fermentation test.
2) DN Ase test.
3) PCR.
Serology
Serology for G.C:
•It is not of great value in the diagnosis to
detect ANTIBODIES ?
• So it is more important to detect
gonococcal ANTIGENS using a technique
called (ELISA) or using radioimmunoassay
(RIA).
Rapid detection methods (detect Ag)
vN. meningitidis ðàC.S.F ðàLatex agglutination test.
vN. gonorrhoea ðàurethral discharge ðàELISA, DNA
probe (molecular assay) e.g. PCR.
Serogrouping for N. meningitidis.
Latex agglutination test ðà
specific antisera for each 13
serogroups. (The most prevalent serogroups are A, B,
C, W135, and Y)

Summary/ conclusions:
• Neisseria are G- ve diplococci.
• Neisseria are oxidase positive bacteria.
• Pathogenic and non- pathogenic species can be
differentiated by sugar fermentation, nitrate reduction
and PCR.
• Gonococci is highly antigenic variable due to pilli
antigenic variation.
• Meningococci is capsulated with 13 serogroups of that
capsule.
• Neisseria species are sensitive to pencillins and
cephalosporins.
• Vaccine against most virulent strain of meningococci
are given to high risk groups.
T
T
H
H
A
A
N
N
K
K
Y
Y
O
O
U
U
