1
GRAM-NEGATIVE COCCI
GENUS: NEISSERIA
Objectives: upon completion of this lecture, student will
Describe the morphology & physiology for genus Neisseria.
Determine the virulence factors for genus Neisseria.
Analyze the diseases & pathogenicity for genus Neisseria.
Demonstrate the epidemiology/transmission for genus Neisseria.
Outline the laboratory diagnosis for genus Neisseria.
State the drug of choice and prophylaxis where regularly used.
Lec.4
Dr.Sarmad Zeiny
2014-2015
2
GRAM-NEGATIVE COCCI
GENUS: NEISSERIA
Introduction:
The family Neisseriaceae includes the many genera, important one is genus Neisseria. The
neisseriae are gram-negative cocci that usually occur in pairs. Neisseria gonorrhoeae
(gonococci) and Neisseria meningitidis (meningococci) are pathogenic for humans and
typically are found associated with or inside polymorphonuclear cells. Other neisseriae are
normal inhabitants of the human respiratory tract, rarely if ever cause disease, and occur
extracellularly. So we can divide this genus into:
Pathogenic Neisseria include:
1. N. meningitidis (meningococci) meningitis.
2. N. gonorrhoea (gonococci, G.C) gonorrhea (one of sexually transmitted diseases (STD)).
Non - pathogenic (commensal) Neisseria include:
1. N. catarrhalis (Moraxella or Branhamella catarrhalis).
2. N. sicca, N. subflava, N. lactamica, N. mucosa.
These are normal inhabitants of human respiratory tract.
Common or general characteristics of Neisseria:
1) G –ve diplococci, kidney shape, with flat or concave opposing edge.
2) Oxidase positive.
3) Pathogenic to human only.
4) Ferment carbohydrates acid only
5) Pyogenic
produce pus.
6) Non -hemolytic, non- motile, non-spore forming.
7) Pathological spp. are intracellular while non-pathogenic are
extracellular.
8) Needs 48h of culturing time.
9) They are rapidly killed by drying, sunlight and many disinfectants.
10)
The non-pathogenic species can grow on simple media while the pathogenic species need
enriched media e.g. blood and chocolate agar.
11)
Gonococci and meningococci are closely related with 70% DNA homology and are
differentiated by few LAB tests and specific characteristics
.
Kidney or coffee bean
shape diplococci
3
Neisseria gonorrhoeae (gonococcus)
Reservoir
:
human genital tract
Transmission
• Sexual contact, birth
• Sensitive to drying and cold
Disease: gonorrhea (clap)
a) Localized infection.
b) Systemic infection.
A) Localized infection:
1) Genital infection: which differ in male than in female?
- In MALE it causes urethritis associated with yellowish mucopurulent discharge from
anterior urethra and dysuria the infection can extend to the epididymis leading to
epididymitis and if not treated it will be complicated by fibrosis and urethral stricture.
- In FEMALE the first site of infection is the cervix causing cervicitis the infection is
going to spread from cervix to the vagina causing vaginitis and presented by vaginal
discharge which is mucopurulent in nature, if not treated it will spread upward to involve
fallopian tube resulting in salpingitis & PID
(pelvic inflammatory disease)
which leads to
fibrosis with tube stricture leading to infertility due to tubal damage.
2) Rectal involvement: proctitis, the patient presenting symptoms is purulent discharge
from anus with tensmus.
3) Eye infection (infection of the conjunctival sac): occur in new born babies during
their passage through infected birth canal causing a condition called (ophthalmia
neonatorum) which is a very serious condition and if untreated it will lead to blindness.
Rx
: using antimicrobial agent as silver nitrate and erythromycin.
4) Throat infection (Gonococcal pharyngitis) it’s common in oral sex.
B)
Systemic infection:
Disseminated via the blood stream to the distant organs.(skin, bone, joints):
- Arthritis.
- Meningitis.
- Endocarditis.
- Vasculitis.
4
Diagnostic LAB tests:
a. Specimens:
Pus and secretion are taken from the urethra, cervix, rectum, conjunctiva, throat or synovial
fluid for culture and smear.
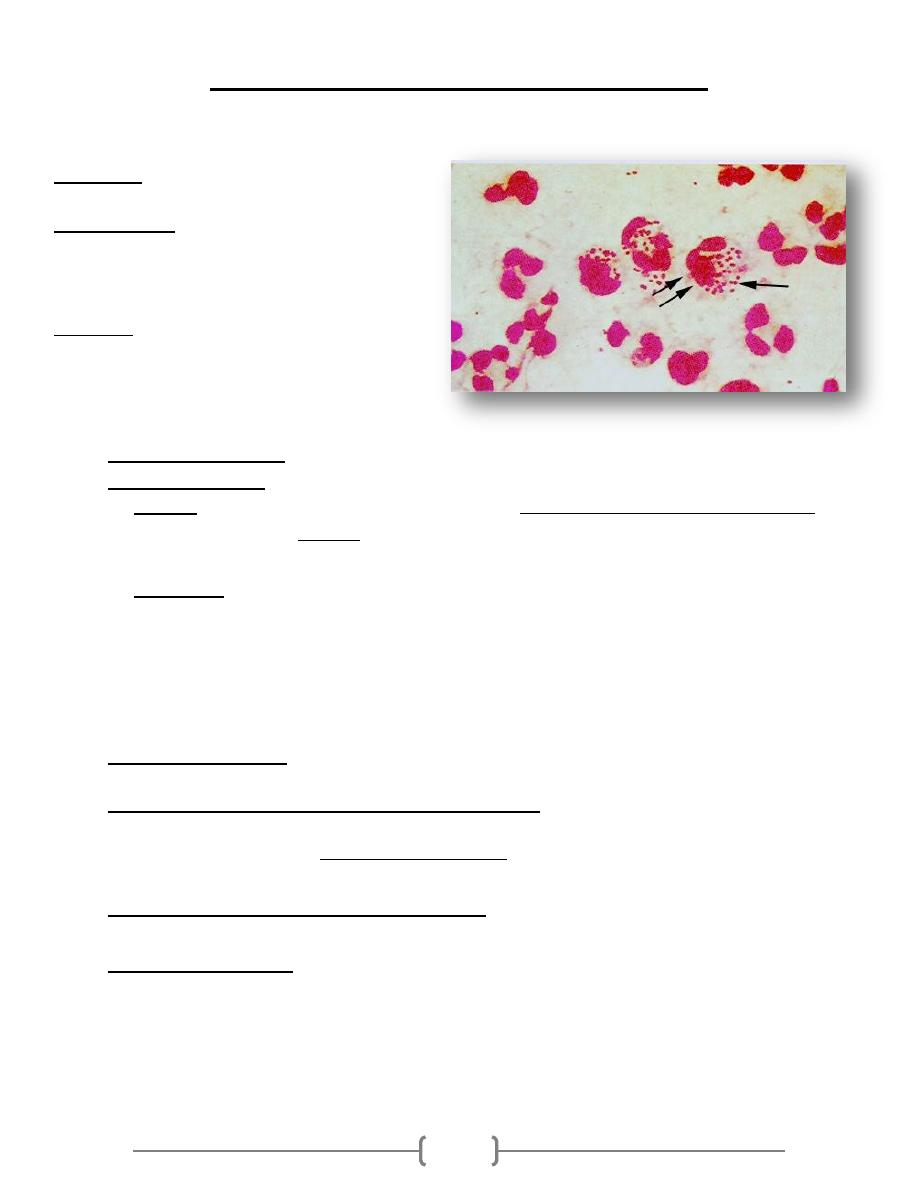
b. Smears:
Gram stained smears of urethral or endocervical exudate reveal many diplococci
within pus cells.
In MALE, the finding of numerous neutrophils containing gram
negative diplococci in a smear of urethral exudate permits a provisional diagnosis of
gonococcal infection and indicates that the individual should be treated. In contrast, a
positive culture is needed to diagnose gonococcal infection in FEMALE.
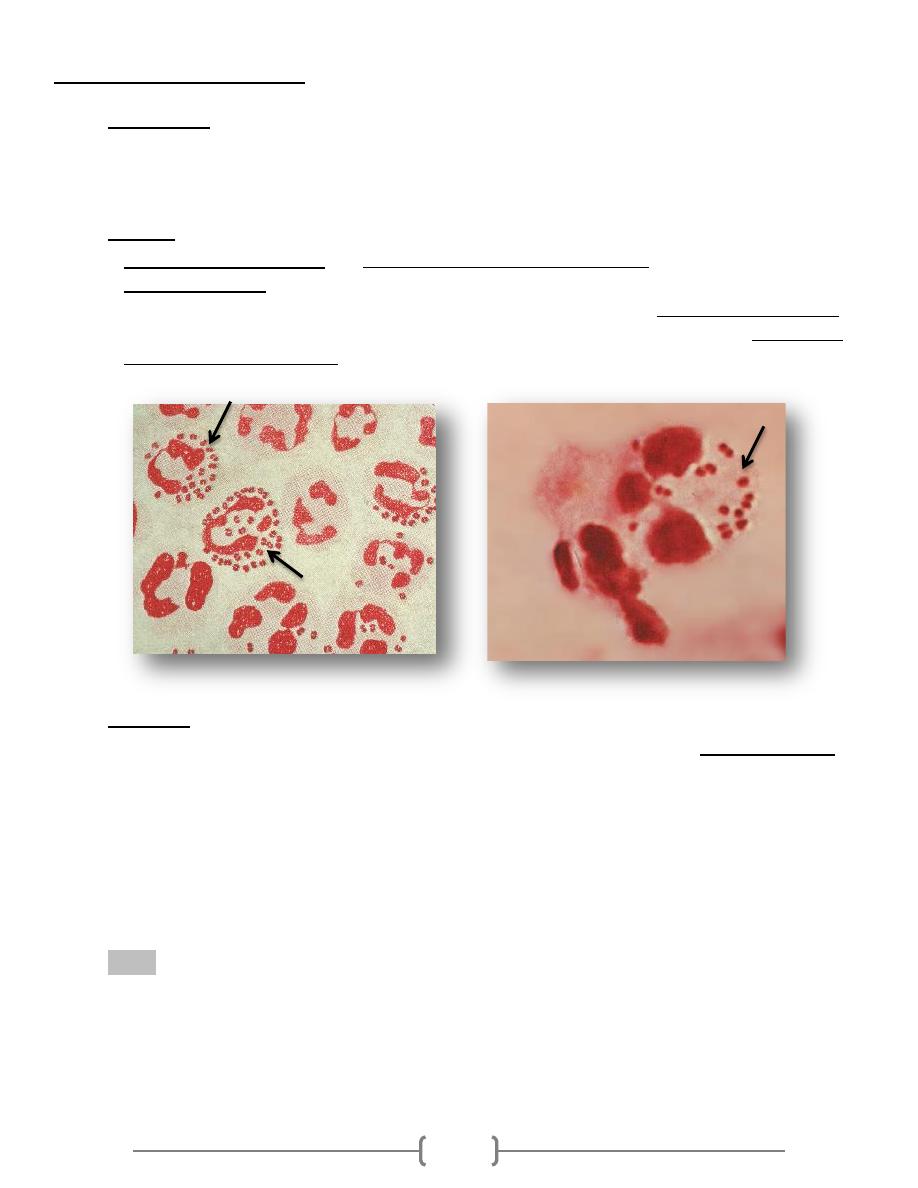
c. Culture:
Immediately after collection of pus or mucous is streaked on enriched selective media:
A. Thayer Martin (TM): Chocolate agar + Enrichment element +Antibiotics: Colistin
(against G
– ve rods)
; Vancomycin
(against G + ve)
; Nystatin
(against fungi)
.
B. Modified Thayer Martin: same as TM + Trimethoprim (inhibit proteus).
C. Martin – Lewis (ML).
D. New York City (NYC).
It needs 5 – 7% CO
2
(candle jar, CO
2
generating kit); Humid atmosphere; 35 – 37 C
◦
,
72hrs
5
d. Biochemical test.
1) Oxidase test: + ve for all Neisseria spp.
Special reagent (oxidase reagent) is colorless, when get contact with oxidase enzyme
purple in color i.e. positive oxidase test.
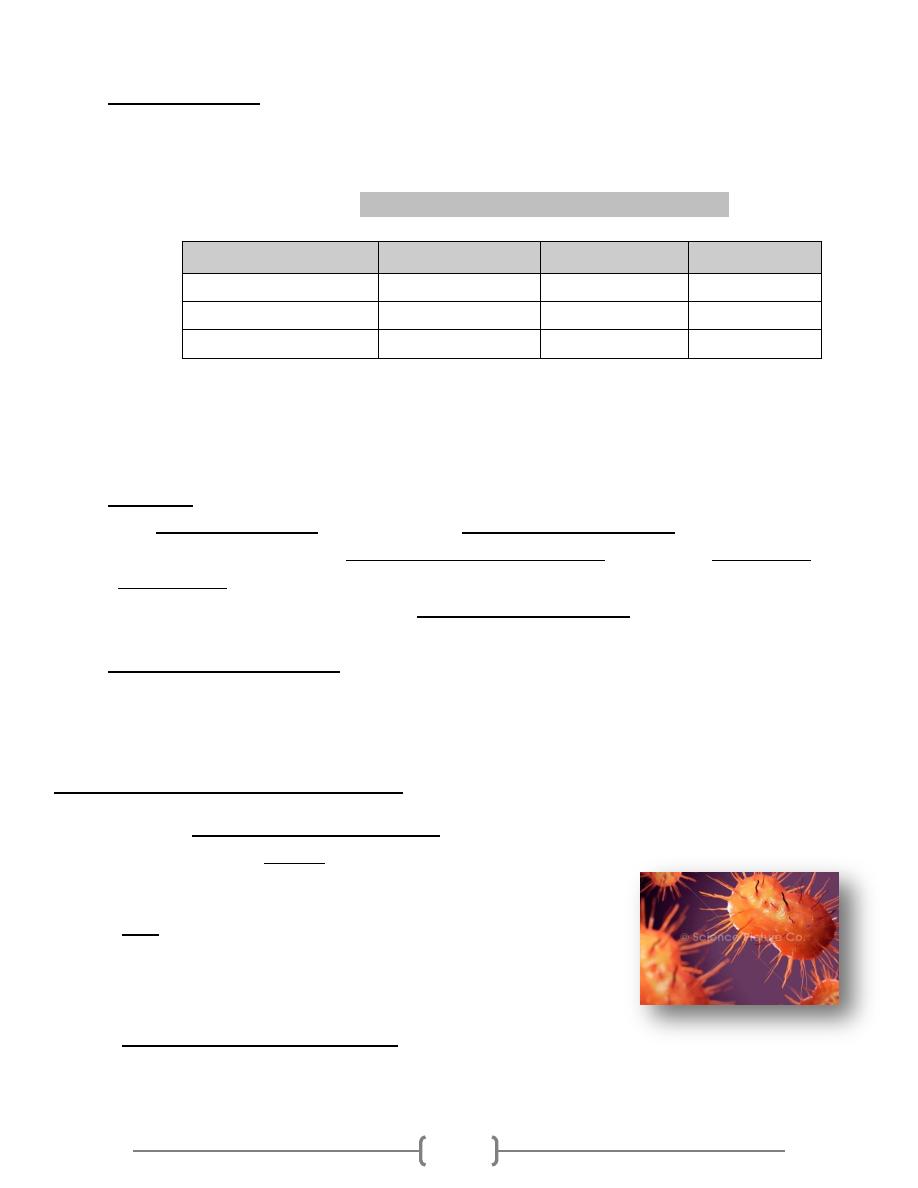
2) Sugar fermentation test:
(important in differentiation between Neisseria spp.)
Sucrose
Maltose
Glucose
N. spp.
ـــ
+
+
N. meningitidis
ـــ
ـــ
+
N. gonorrhoea
ـــ
ـــ
ـــ
M. catarrhalis
3) DNAse test:
+ ve Moraxella catarrhalis.
- ve Other Neisseria spp.
e. Serology:
- It is not of great value in the diagnosis to detect ANTIBODIES against this
bacterium? Because of the antigen diversity of Gonococci and there is delay in the
development of these antibodies.
- So it is more important to detect gonococcal ANTIGENS using a technique called
(ELISA) or using radioimmunoassay (RIA).
f. PCR (molecular method): Detection of gonococcal nucleic acid using DNA probe
which can detect nucleic acid of the m.o.
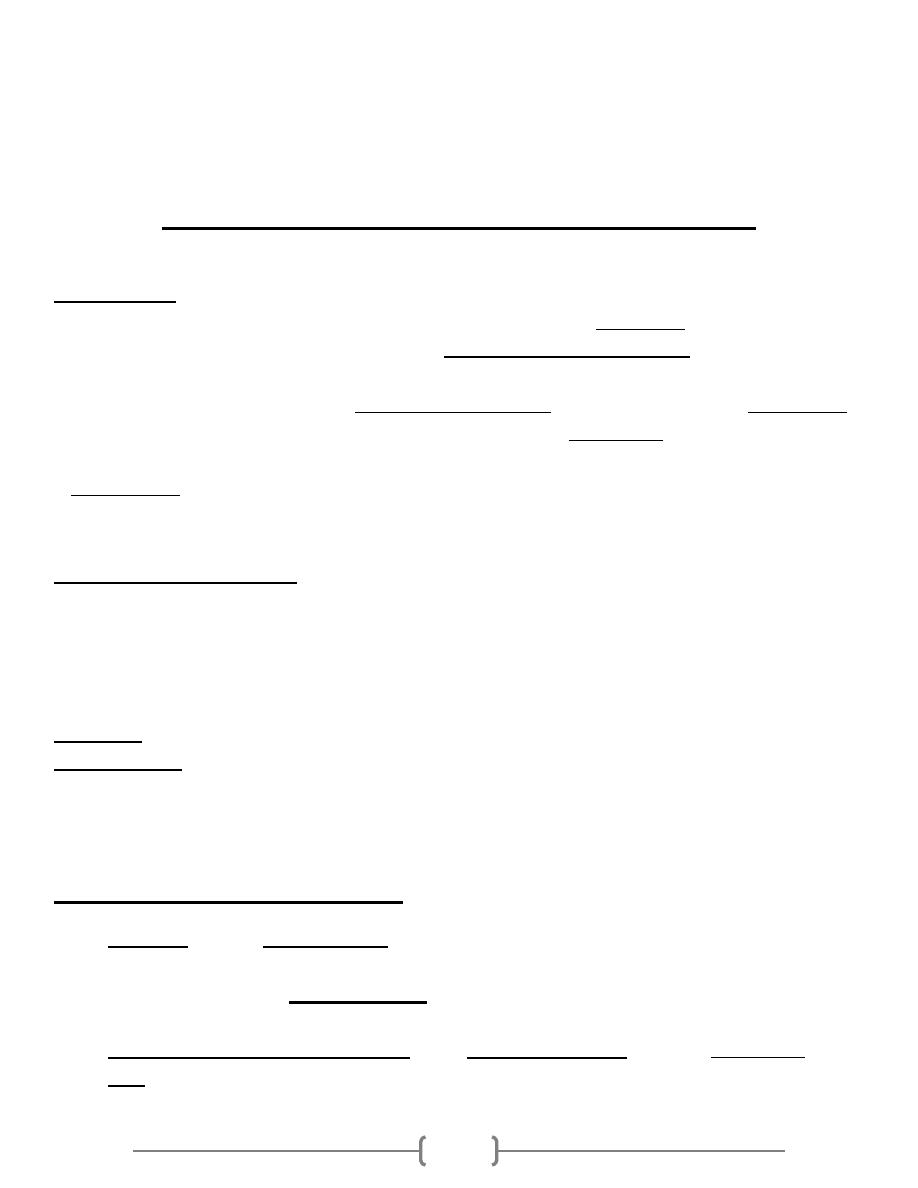
Antigenic & Virulence structures:
Gonococci are antigenically heterogeneous both in vivo and in vitro. These antigenic
changes help the m.o. to escape from the immune system, these
include:
1) Pili:
- Attachment to mucosal surfaces.
- Inhibit phagocytic uptake.
- Antigenic (immunogenic) variation:> 1 million variants
2) Porin (por) protein (protein I):
- Extends through the gonococcal cell membrane, each strain of gonococcus expresses
only one type of por.
6
3) Opacity (Opa) proteins (protein II):
- Attachment to mucosal surfaces.
4) RMP (protein III):
- It is associated with (Opa) protein in the formation of pores.
5) Lipooligosaccharide (LOS):
- It has endotoxic effect and it is responsible for toxicity of gonococci.
6) IgA protease:
- Split IgA making it in non-functioning form, so IgA protease is a virulent factor that
enhances colonization of bacteria.
7) Other proteins: Lip (H8), Fbp (ferric binding protein).
Treatment & prevention:
More than 20 percent of current isolates of N. gonorrhoeae are resistant to penicillin.
A single intramuscular dose of ceftriaxone is the recommended therapy for
uncomplicated gonococcal infections.
Intramuscular spectinomycin is indicated in patients who are allergic to cephalosporins.
Many patients with gonorrhea have coexisting chlamydial infections. Therefore,
doxycycline is effective against Chlamydia.
Prevention of gonorrhea involves:
- Evaluation and management of sexual contacts.
- Antibiotic prophylactically in an exposed individual even in the absence of symptoms.
7
- The use of barrier methods is also a preventive measure against gonorrhea as is the case
for all sexually transmitted infections.
- No vaccine is available for gonorrhea.
Neisseria meningitidis (meningococcus)
Introduction:
N. meningitidis is one of the most frequent causes of meningitis. Infection with N.
meningitidis can also take the form of a fulminant meningococcemia, with intravascular
coagulation, circulatory collapse, and potentially fatal shock, but without meningitis. In each
case, symptoms can occur with extremely rapid onset and great intensity. Outbreaks of
meningitis, most common in winter and early spring, are favored by close contact between
individuals, such as occurs in schools, institutions, and military barracks. N. meningitidis tends
to strike young, previously well individuals and can progress over a matter of hours to death.
Distinguishing Features
• Gram-negative, kidney coffee bean-shaped diplococci.
• Large capsule, Antigenic.
• Grows on chocolate (not blood) agar in 5% C02 atmosphere.
• Ferments maltose in contrast to gonococci.
Reservoir: human nasopharynx (5-10% carriers).
Transmission:
• Respiratory droplets; oropharyngeal colonization, spreads to the meninges via the bloodstream
• Disease occurs in only small percentage of colonized individuals.
Antigenic & Virulence structures:
a) Capsule: At least 13 serogroups of meningococci have been identified by immunologic
specificity and capsular polyscaccharides the most important serogroups associated with
disease in human are A,B,C,Y, W135 ,they are associated with fulminant sepsis with or
without meningitis, which is used for the preparation of vaccines.
b) Outer membrane protein (OMP): about 20 antigenic types, used for serotyping.
c) Pili:
Pili and outer membrane proteins important in ability to colonize and invade.
8
d) IgA protease: cleaves IgA allows oropharynx colonization.
e) Opa protein: attachment
f) Lipooligopolysaccharide (Endotoxin) : fever, septic shock in meningococcemia.
Epidemiology
Transmission occurs through inhalation of respiratory droplets from a carrier or a patient in the
early stages of the disease. In addition to contact with a carrier, risk factors for disease include:
- Recent viral or mycoplasma upper respiratory tract infection,
- Active or passive smoking, and
- Complement deficiency (C5-C8).
In susceptible persons, pathogenic strains may invade the bloodstream and cause systemic
illness after an incubation period of 2 to 10 days. An incidence peak among adolescents and
young adults led the Centers for Disease Control (CDC) to recently recommend vaccination of
this at-risk group. Humans are the only natural host.
Diseases & Pathogenicity:
The source of the infection is either the patient or the carriers.
The route of entry is through the nasopharynx by droplet.
Meningococci will attach to the epithelial cell by pilli. From the nasopharynx the
meningococci will spread through the blood stream to the target organ causing
bacteremia. So the squeal is either meningitis or suffers from fulminating
meningococcemia.
Meningitis: mainly in adult ages 11 to 55 years, it is usually begin suddenly with
headache, vomiting and stiff neck, this will progress to coma within few hours.
Fulminating meningococcemia is more sever with high fever and hemorrhagic rash;
there may be disseminated intravascular coagulation and circulatory collapse (water-
house- friderichsen syndrome).
Laboratory diagnosis:
a) Specimens: Blood, CSF, Nasopharyngeal swab are taken for carrier surveys.
b) Smears:
- Gram stain smear of CSF show typical Neisseria within polymorphnuclear leukocytes.
c) Culture:
- Chocolate agar and Thayer martin media, incubated at 37c.
d) Serology: Rapid dx. test
to measure Ag or antibodies to meningococcal
polysaccharides:
9
- Latex agglutination test,
to identify N. meningitidis capsular antigens in CSF
.
- Immunoelectrophoresis.
e) PCR: most sensitive and specific method.
Treatment:
- Bacterial meningitis is a medical emergency. Accordingly, antibiotic treatment cannot
await a definitive bacteriologic diagnosis.
- Penicillin G is the drug of choice for treating meningococcal disease. In patient
allergic to penicillin chloramphenicol and cefotaxime (or ceftriaxone) can be used.
Prevention:
1) Irradiation of the carrier states (major source).
2) Isolation of the patient.
3) Chemoprophylaxis for contact people.
4) Vaccination: A conjugate meningococcal vaccine (MCV4) was approved in the United
States in 2005 for use in adolescents and adults ages 11 to 55 years, and has replaced
the unconjugated polysaccharide vaccine. MCV4 is a tetravalent vaccine that contains
capsular polysaccharides from serogroups A, C, W-135, and Y conjugated to diphtheria
toxoid.
Vaccination is recommended for persons 11–55 years of age who are among the following at-
risk groups:
• Persons with functional or surgical asplenia;
• persons with complement deficiencies;
• travelers to highly endemic areas (eg, sub-Saharan Africa);
• “Closed populations" such as military and for
• Clinical laboratory workers (microbiologists).
10
Moraxella catarrhalis:
Previously they are called Neisseria catarrhalis, the name changed to Branhamella and
now they are a separated genus “Moraxella”.
They are normally found in upper respiratory tract especially among school children.
(50% of school children carry this microorganism)
May cause pneumonia, otitis media, sinusitis and other infections.
It is nonmotile, gram-negative coccobacilli that are generally found in pairs.
Moraxella are aerobic.
Oxidase positive.
Non fastidious organisms can grow on nutrient agar.
Does not ferment carbohydrates.
Summary:
Neisseria are G-ve diplococci.
Neisseria are oxidase positive bacteria.
Pathogenic and non-pathogenic species can be differentiated by sugar fermentation,
nitrate reduction and PCR.
Gonococci are highly antigenic variable due to pilli antigenic variation.
Meningococci are capsulated with 13 serogroups of that capsule.
Neisseria species are sensitive to penicillins and cephalosporins.
Vaccine against most virulent strain of meningococci is given to high risk groups.
References:
-
Review of Medical Microbiology and Immunology11th edition 2010.
-
Clinical Microbiology Made Ridiculously Simple, 6
th
ed, 2014.
-
Baily & Scott diagnostic microbiology, 12
th
ed.
-
Lippincotts Illustrated microbiology 3
ed
ed., 2013
Additions to lec2 & Lec3:
Treatment for genus streptococci:
Drug of choice is penicillin G; alternatives are cephalosporins, tetracycline, aminoglycosides,
macrolides (clarithromycin or azithromycin), flouroquinolones.
Resistant cases vancomycin.
END
