WOUND
HEALING
Phases of wound healing
Wound healing occurs in 3 phases
1.
Inflammatory phase
2.
Proliferative phase
3.
Remodeling phase
I. Inflammatory phase
A.
Immediate to 2-5 days
B.
Hemostasis
1.
Vasoconstriction
– damaged blood vessels
constrict
2.
Platelet aggregation
– primary hemostasis
3.
Coagulation
– fibrin – secondary hemostasis
(clot
– platelets + fibrin)
C.
Inflammation
A.
Vasodilation
B.
Phagocytosis
II. Proliferative phase
A.
2 days to 3 weeks
B.
Granulation
I.
Fibroblasts lay a bed of collagen to fill the defect
C.
Angiogenesis
D.
Contraction
I.
Wound edges pull together to reduce the defect
E.
Epithelialization
I.
Epithelial cells migrate across the new tissue to
form a barrier between the wound and the
environment
III. Remodeling phase
A.
3 weeks to 2 years
B.
New collagen forms which increases the
tensile strength of the wound
C.
Strength increases and becomes maximum
but not as strong as original tissue
D.
Scar tissue is only 80% of the strength of the
original tissue
Wound healing
Wound healing is accomplished in one of the
following two ways:
1.
Healing by first intention (primary union)
2.
Healing by second intention (secondary
union)
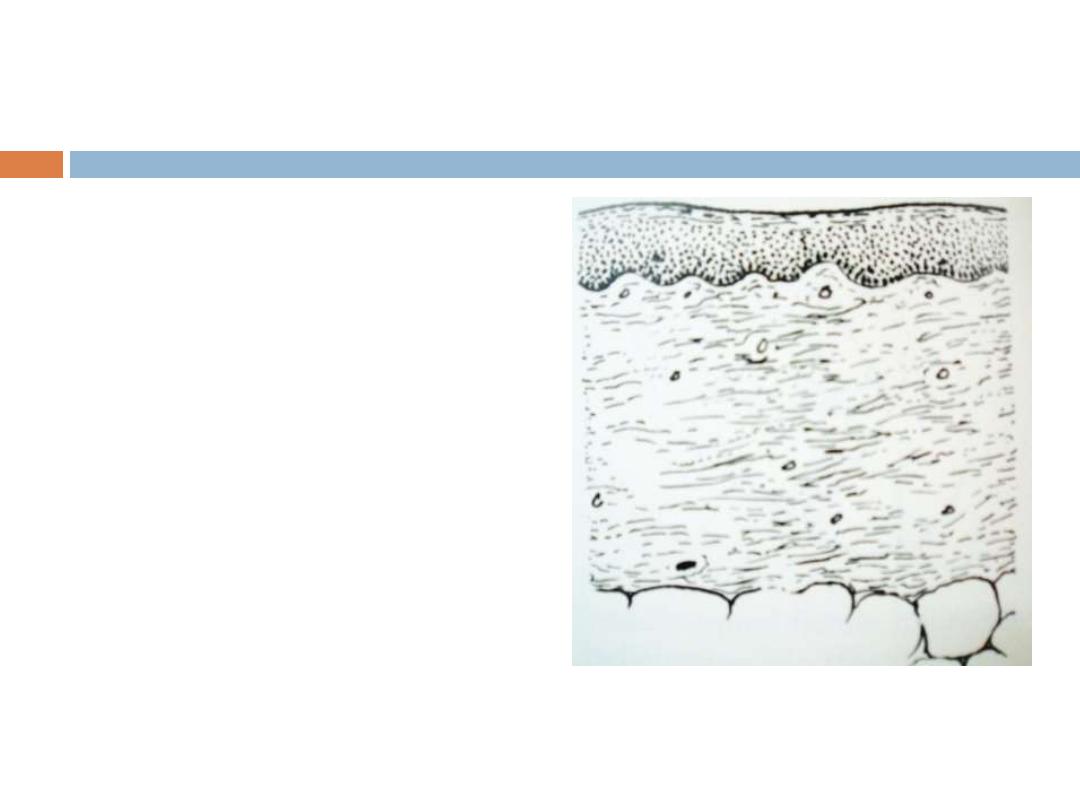
Healing of skin wounds is a classical example
Healing by first intention (primary
union)
Occurs in clean, incised wounds with good
apposition of the edges
– particularly planned
surgical incisions
(clean wounds
– no infections or foreign bodies)
The incision causes only focal disruption of
epithelial basement membrane continuity and
death of a relatively few epithelial and
connective tissue cells.
As a result, epithelial regeneration
predominates over fibrosis
Healing by first
intention:
Sequence of events
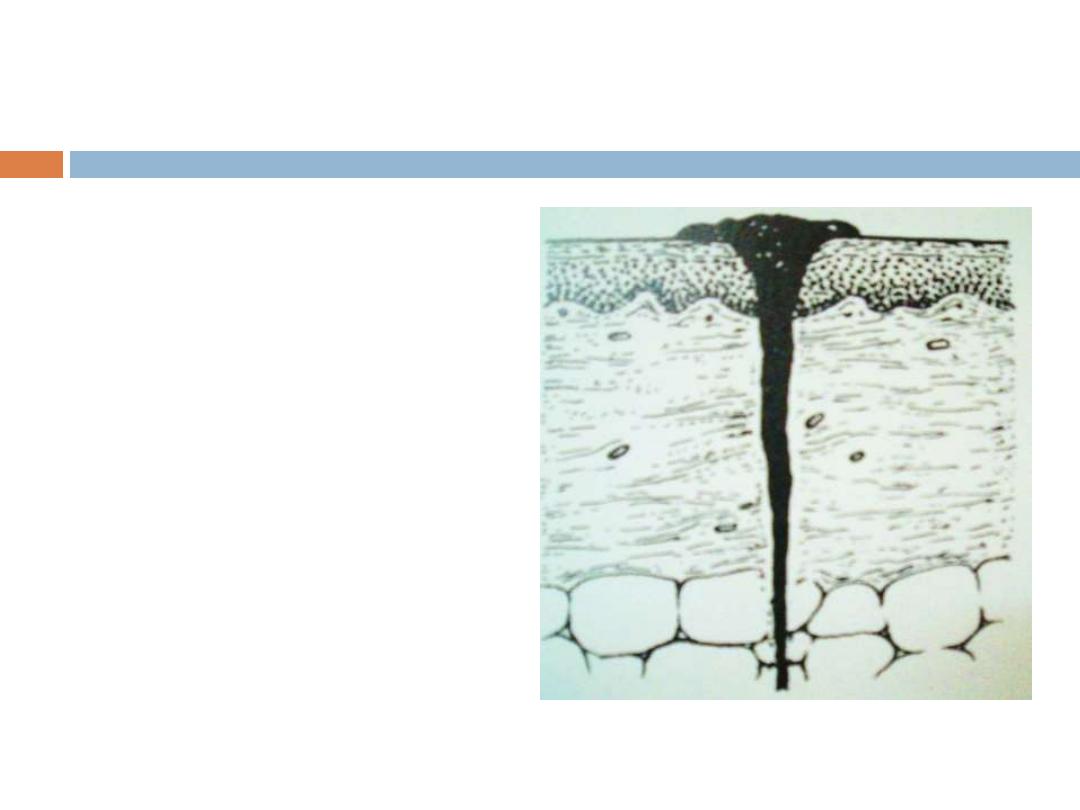
Immediate
The narrow
incisional space
rapidly fills with
fibrin clotted blood
Dehydration at the
surface produces a
scab to cover and
protect the healing
repair site
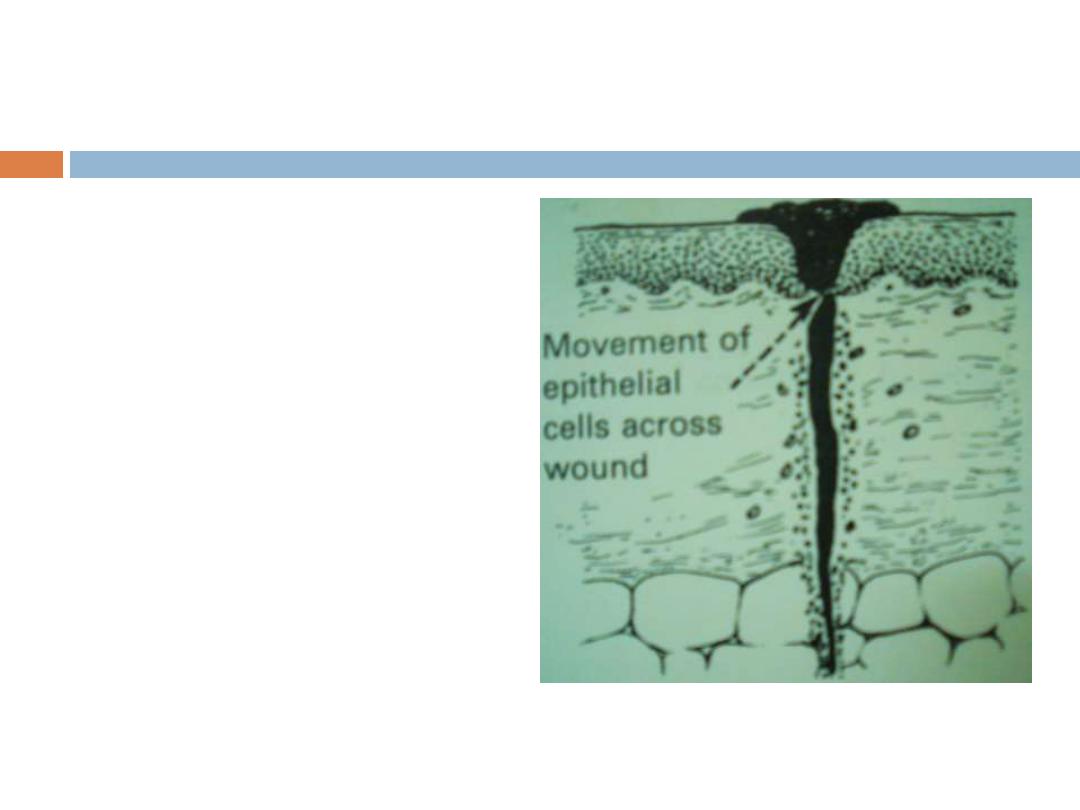
Within 24 hrs
Movement and
proliferation of
epithelial cells across
the wound resulting
in a thin, but
continuous epithelial
layer
Early inflammation
close to the edges
(neutrophils)
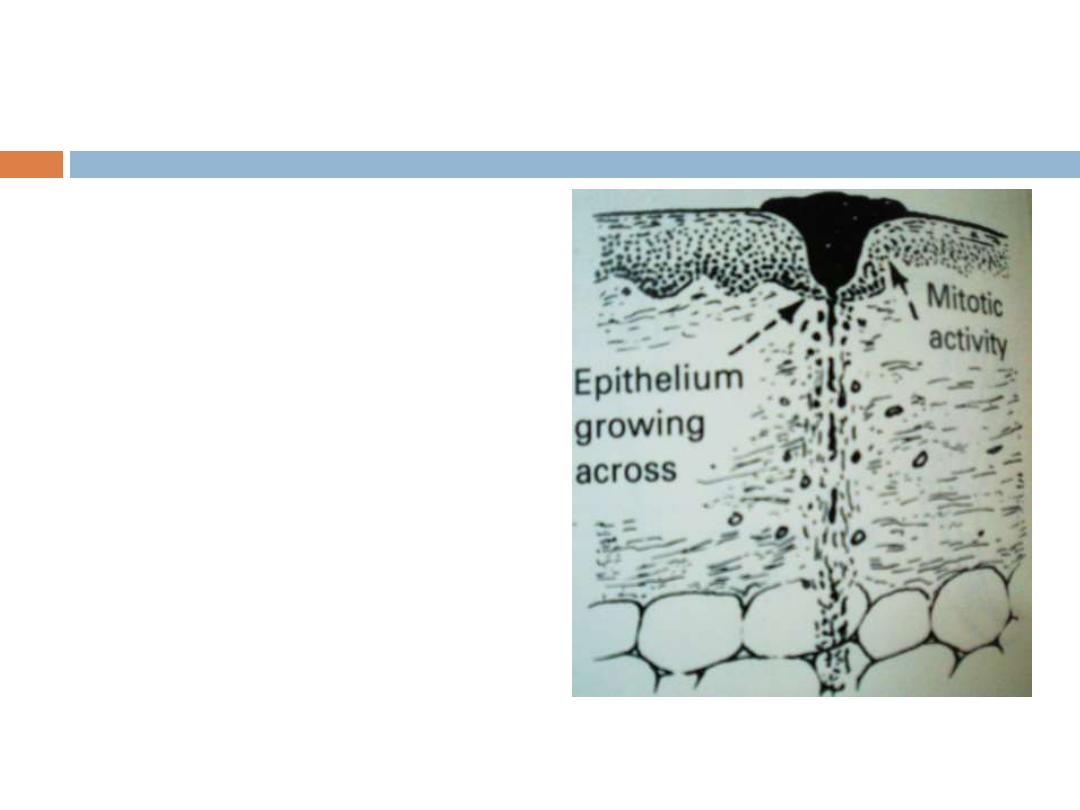
2-3 days
Neutrophils replaced
by macrophages
Macrophages
remove the blood
clot
Proliferation of
epithelial cells
Fibroblastic activity
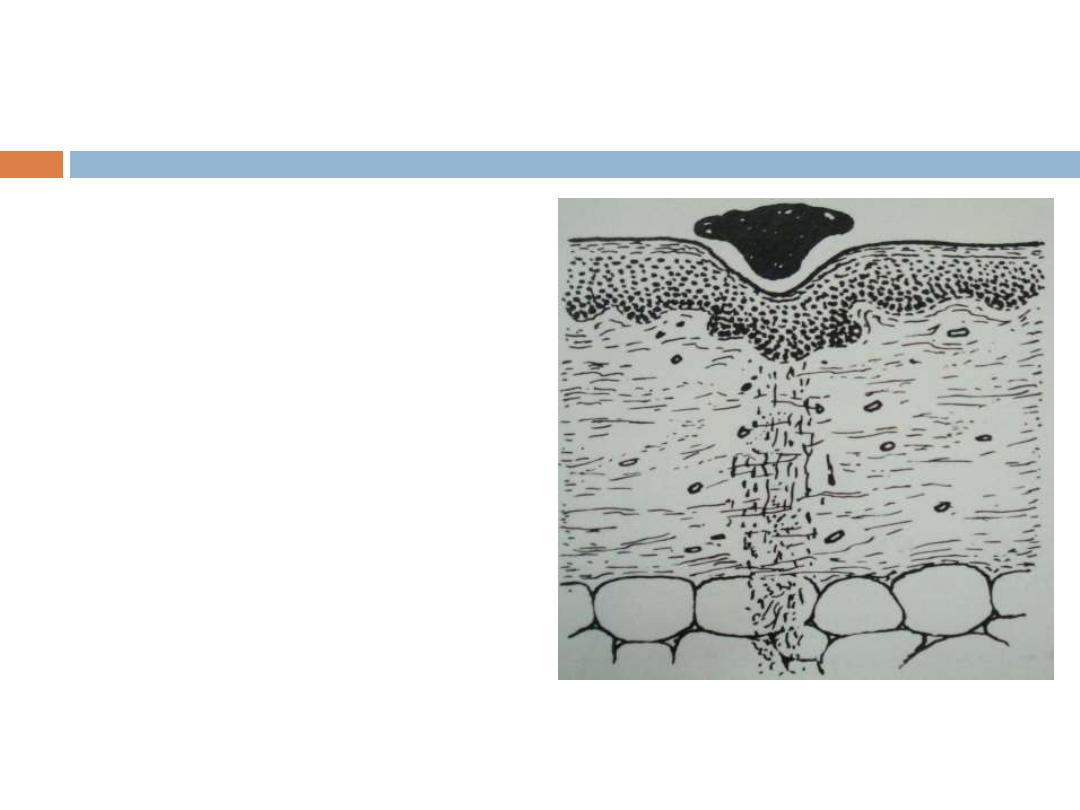
10-14 days
Scab loose
(aka dry clot)
Epithelial covering
complete
Fibrous union of
edges
Wound still weak
vascularization
By the end of the first month
Scar comprises of a
cellular connective tissue
devoid of inflammatory
infiltrate, covered by intact
epidermis
Dermal appendages
destroyed in the line of
incision are permanently
lost
Tensile strength of the
wound increases and
reaches maximum
Healing by second intention
(secondary union)
This occurs in open wounds, particularly when
there has been significant loss of tissue,
necrosis or large wounds with irregular margins
Regeneration of parenchymal cells cannot
completely reconstitute the original architecture
Abundant granulation tissue grows in from the
margin to complete the repair
Granulation tissues consists of:
ECM fibroblasts
Macrophages, neutrophils
New blood vessels
Healing by second
intention
(secondary union)
sequence of events
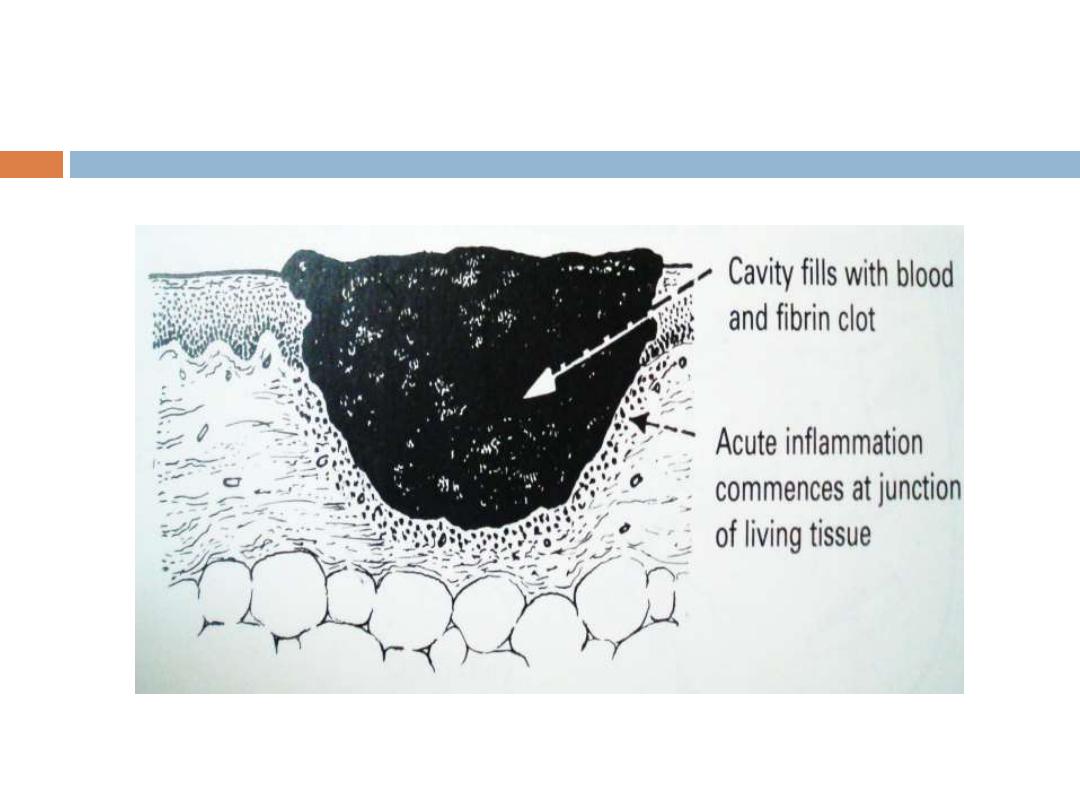
Early
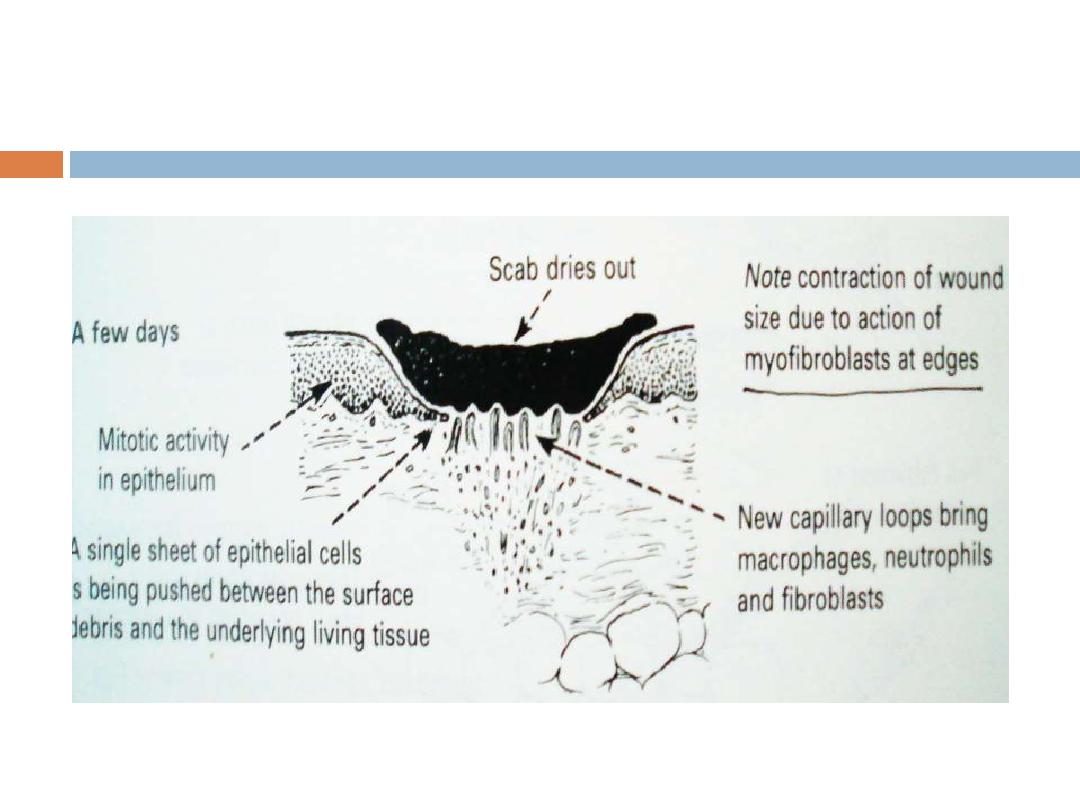
A few days
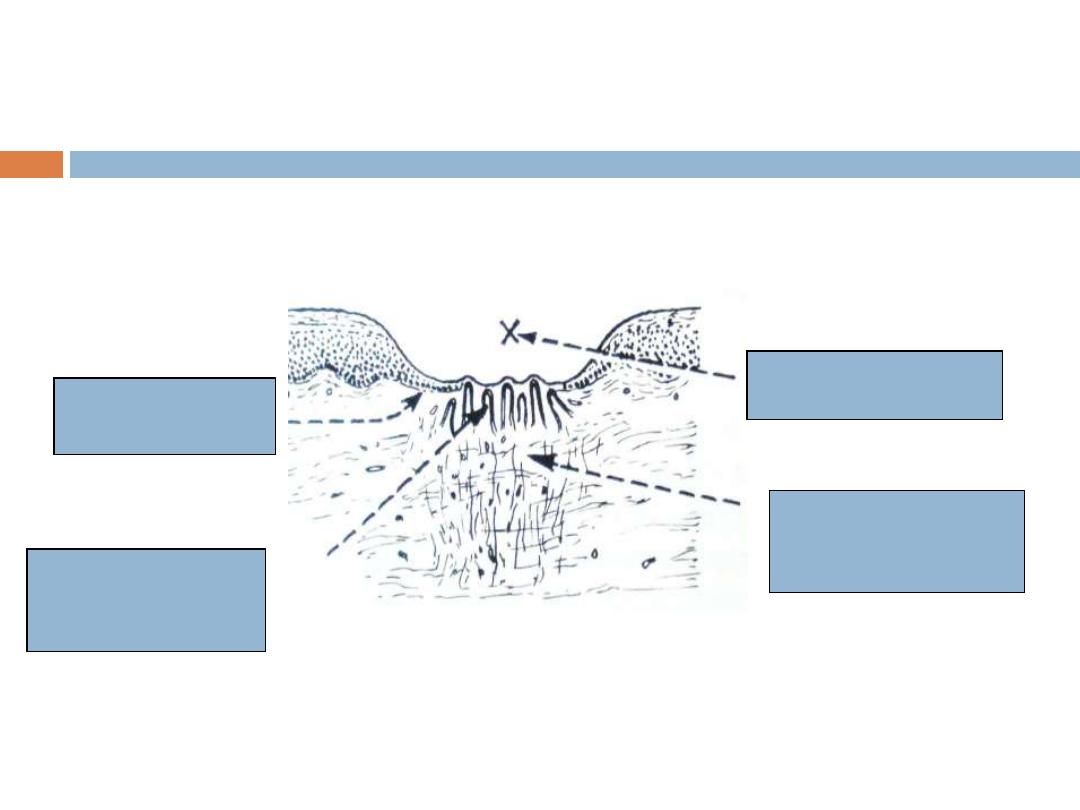
1 week
Epithelial
proliferation
Capillary loops
(granulations)
Scab shed
Loose connective
Tissue formed by
fibroblasts
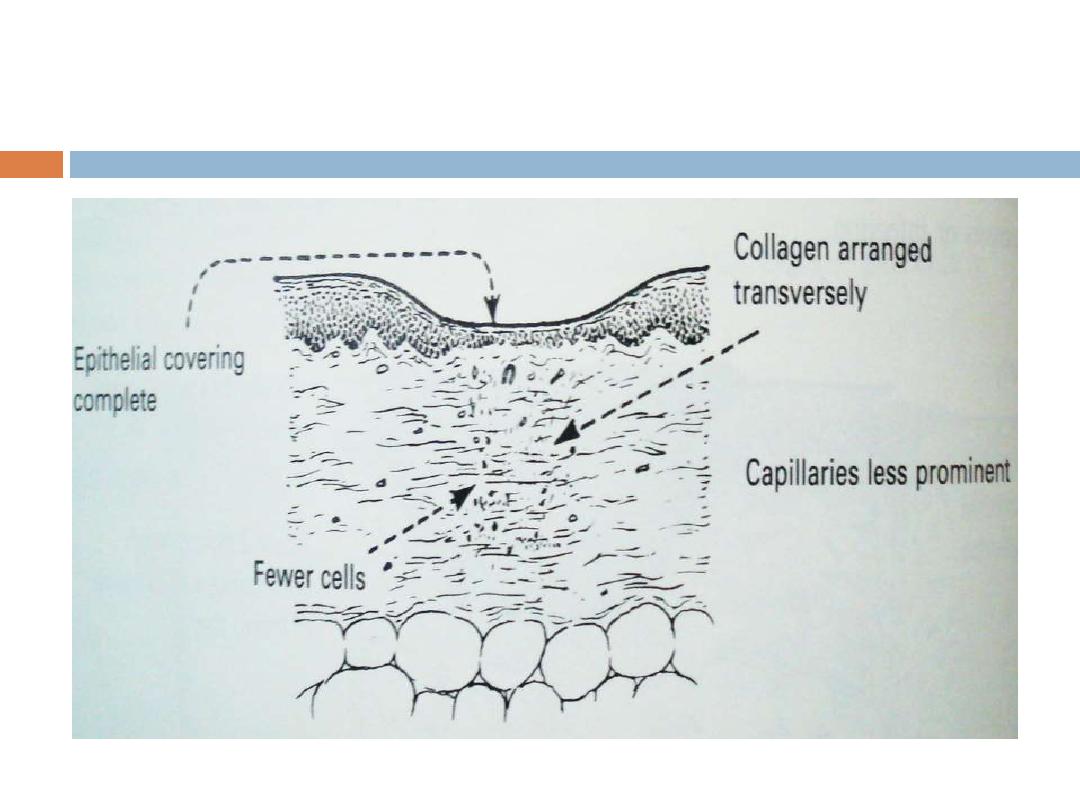
2 weeks onwards
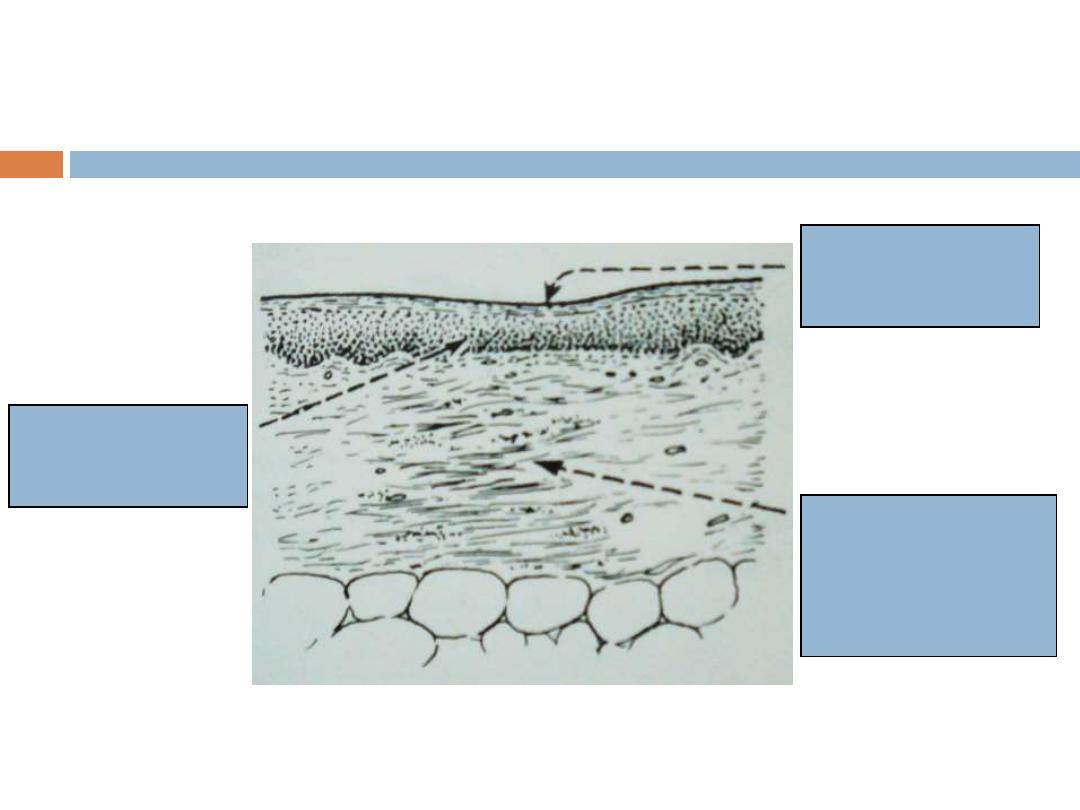
Months
Full thickness of
Epithelium restored
Varying depth of
Surface depression
Thick collagenous
Scar tissue becoming
Less vascular
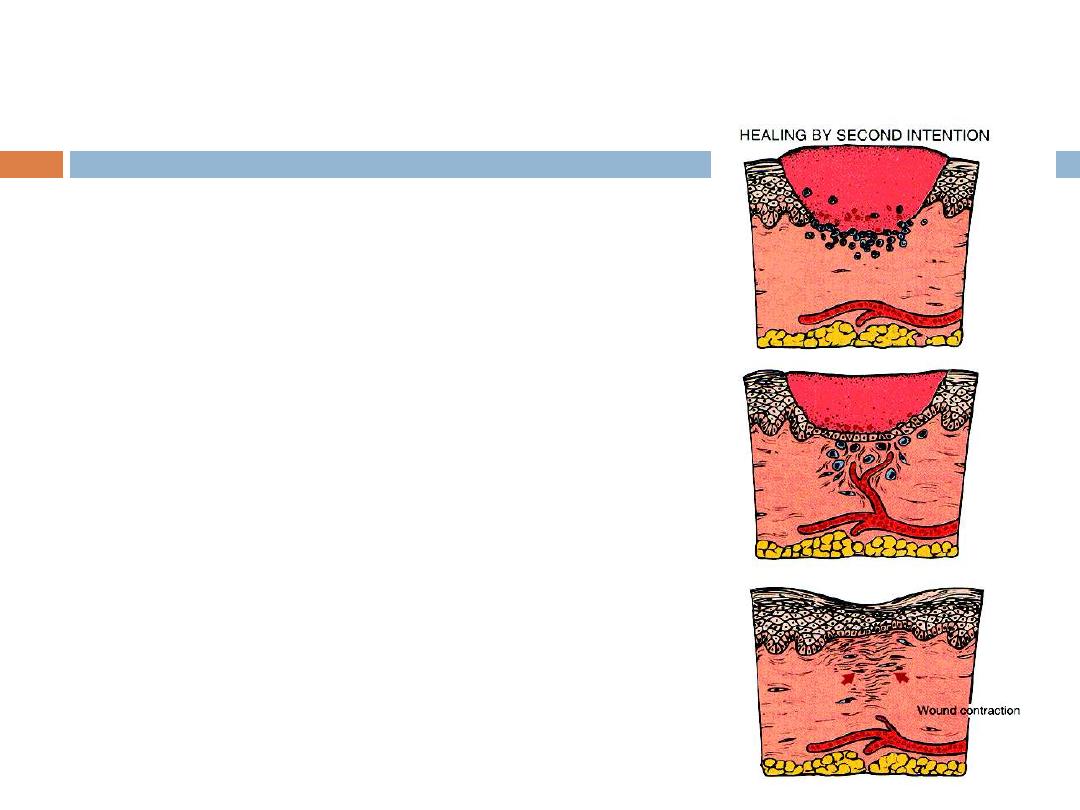
Secondary union differs from
primary union in several
respects
1.
inflammatory reaction is
more intense
2.
larger amounts of
granulation tissue formation
3.
larger scar
4.
***wound contraction
Myofibroblasts: modified
fibroblasts with feature of
SMC
defect significantly
decreases in size as wound
heals.
Wound Strength
Skin wounds
1 week old; 10% of unwounded skin
rapid increase in tensile strength as scar
tissue accumulates over 2 months
Completely healed; 70-80% of unwounded skin
Scar tissue is never as strong as the original
tissue !!
Factors that influence healing
Classified as
A.
Systemic
and
B.
Local
Systemic Factors
that Delay/Retard
Wound Healing
Nutrition
Protein deficiency, Vitamin C deficiency
inhibit collagen synthesis
Zn deficiency (cofactor in type III collagenase)
Metabolic status
diabetes mellitus:
Susceptibility to infection caused by impaired
circulation and increased glucose.
Circulatory status
inadequate blood supply
atherosclerosis, vascular defects
Hormones
glucocorticoids inhibit collagen synthesis, decrease
inflammation
Local Factors
that Delay/Retard
Wound Healing
Infection
most important cause of delayed wound healing
Persistent injury and inflammation
Mechanical factors
motion early in healing
Foreign material - like suture material and foreign bodies
Size, location & type of wound
wounds in ↑ vascularized areas (face) heal faster than
in poorly vasc areas (tendon, feet)
small wounds heal faster than larger
incisions faster than blunt trauma (contusions)
Complications of wound healing
1.
Deficient scar formation
( most important)
2.
Excessive formation of repair
components
3.
Exaggerated contraction
Deficient scar formation
Can lead to two types of complications:
A. Wound Dehiscence (rupture of wound)
most common after abdominal
surgery
coughing, vomiting,
B. Ulceration - defect in the continuity

Wound Dehiscence
Excessive formation of repair
components
1.
Keloid / hypertrophic scar
(excess collagen)
2.
Exuberant granulation or proud flesh
(excessive granulation tissue that protrudes
above the level of the surrounding skin and
impairs the growth of epithelium)
Keloid / hypertrophic scar
Raised scars due to accumulation of excess
amounts of collagen ( type III
– type I)
Hypertrophic scars do not grow beyond the
boundaries of the original wound
Keloids grow beyond the boundaries of the original
wound (more serious)
Can result from a surgery, an accident, body piercing or
can be spontaneous
Genetic predisposition
More common in African
– Americans
Commonly seen over face, shoulders and chest
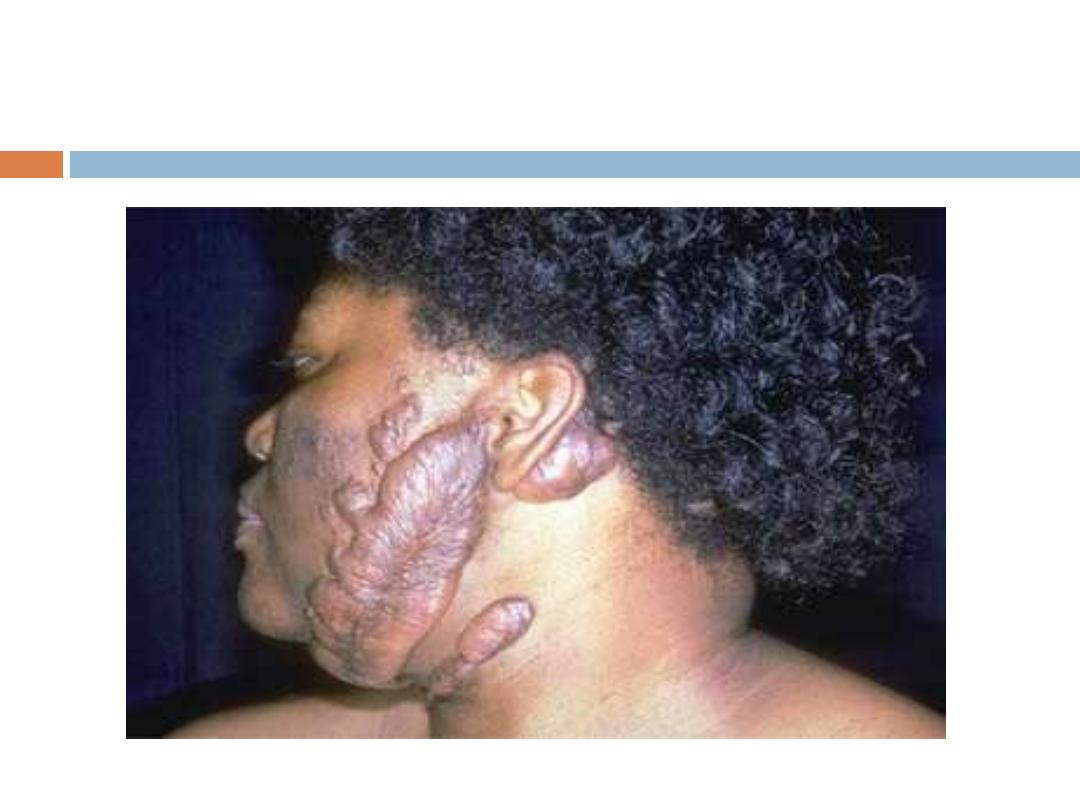
Keloid

Exuberant granulation
(proud
flesh)
Excessive granulation
tissue
Protrudes above
surrounding skin
Prevents re -
epithelialization
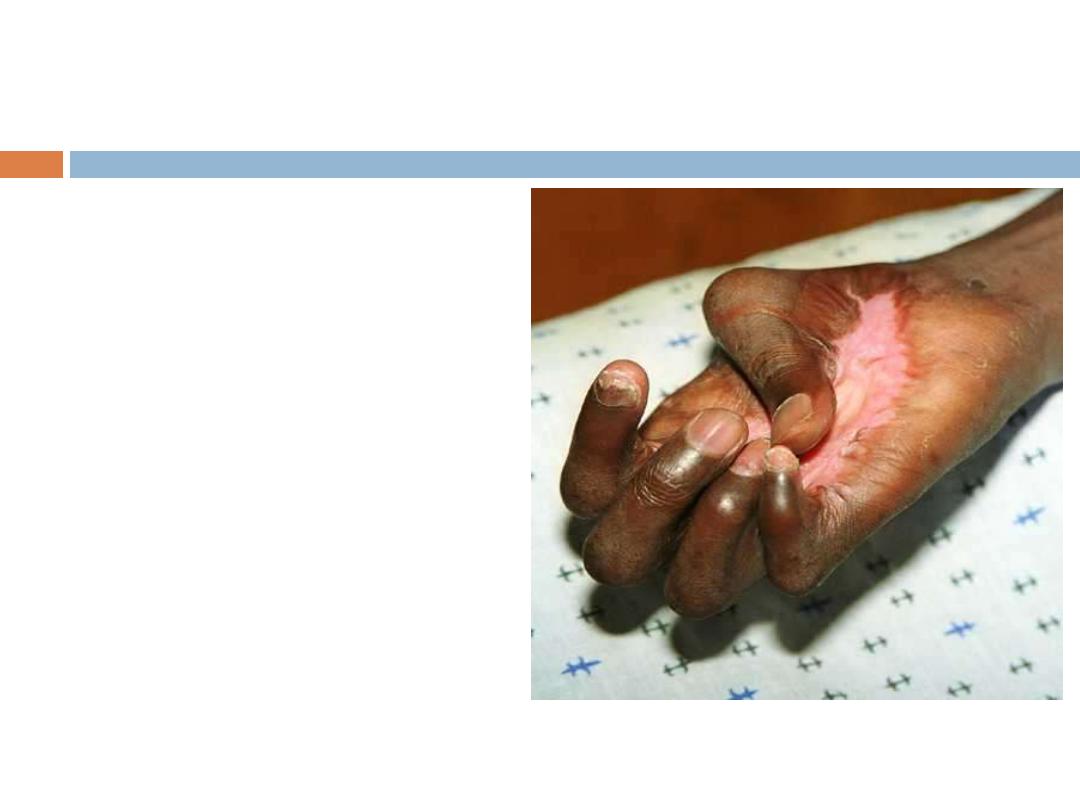
Exaggerated contraction
deformation of
surrounding tissue or
wound
Can compromise the
movement of joints.
most common on
palms, soles, anterior
thorax following
severe burns
Important Growth factors
responsible for wound healing
Platelet derived growth factor:
Promotes migration and proliferation of fibroblasts
Is chemotactic for monocytes
Epidermal growth factor
Promotes growth of endothelial, epithelial cells
and fibroblasts
Growth factors in wound
healing
Fibroblast growth factor:
Promotes synthesis of ECM proteins including
fibronectin.
Chemotactic for fibroblasts and endothelial cells
Promotes angiogenesis
Vascular Endothelial Growth Factor (VEGF)
Angiogenesis
Macrophage derived growth factors
IL-1 and TNF
Promote proliferation of fibroblasts and endothelial cells.
