Dr. Aqeel Shakir
Lec. 2
LOWER GI BLEEDING
Tues. 28 / 4 / 2015
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2014 – 2015
LOWER GI BLEEDING Dr. Aqeel Shakir
28-4-2015
2
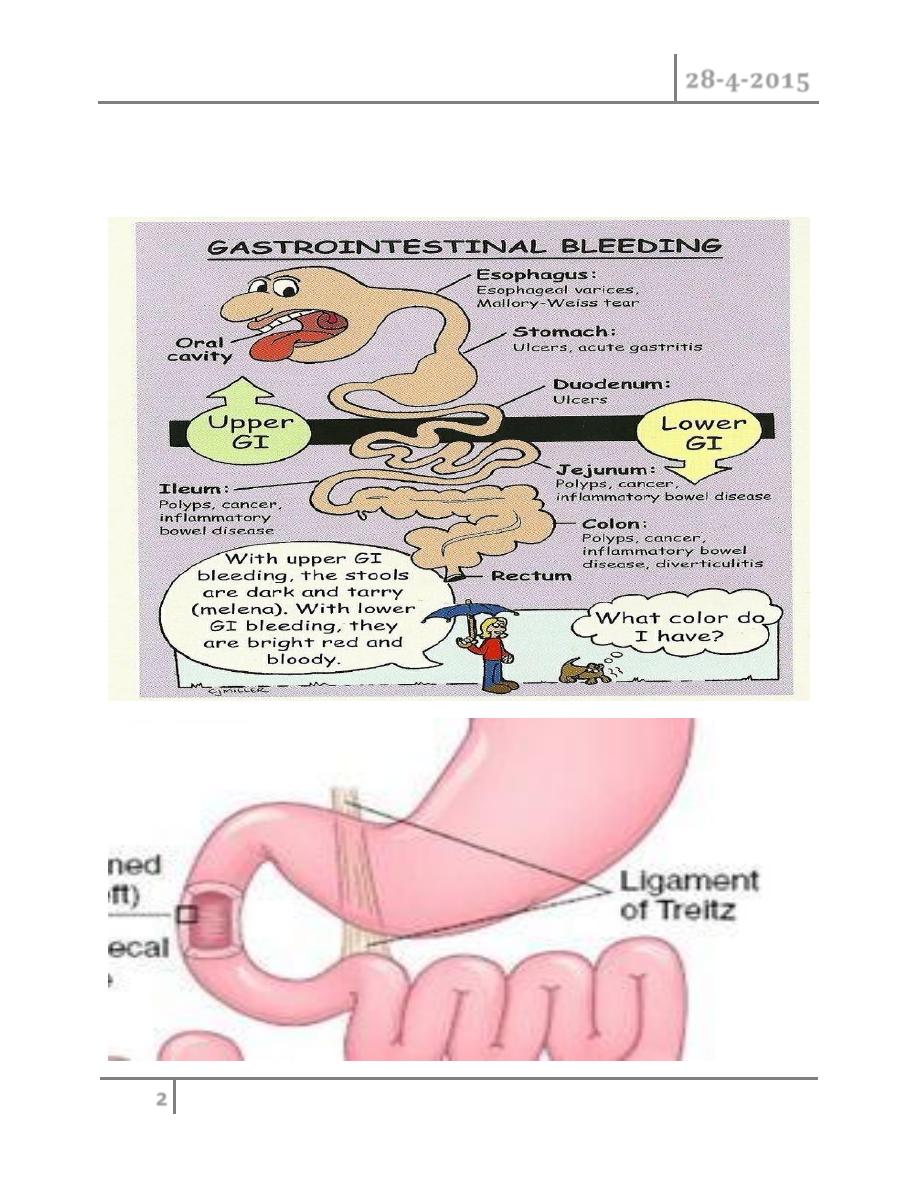
Lower Gastrointestinal Bleeding
LOWER GI BLEEDING Dr. Aqeel Shakir
28-4-2015
3
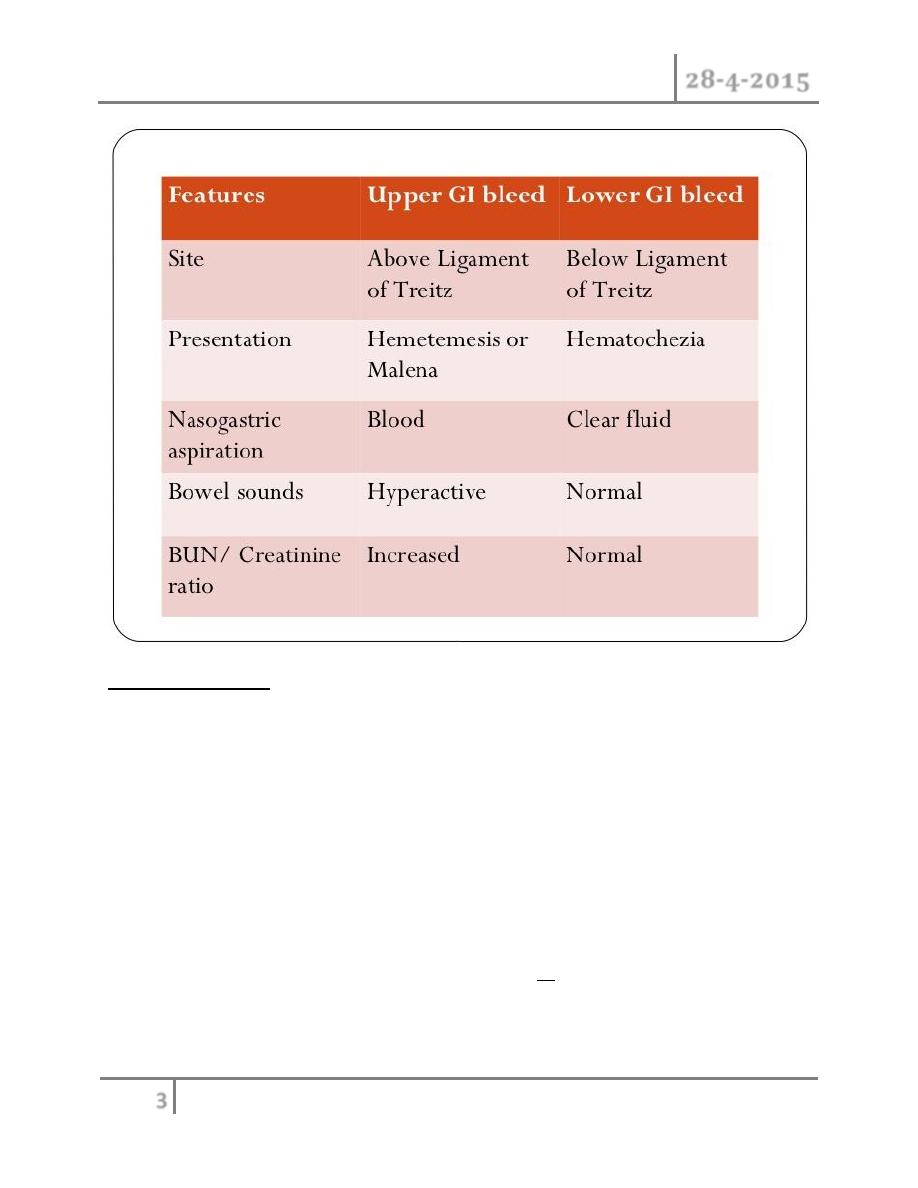
Lower GI bleeding :
Is defined as Bleeding distal to the ligament of Treitz.
It can range in severity from trivial to massive.
LGIB accounts for approximately 20% of all major GI bleeds.
More commonly bleeding is from a colonic rather than a small bowel
source.
Annual incidence 21 cases per 100,000.
Increased in males and in older patients (mean age at presentation of 63 to
77 years).
80-90% of cases will stop bleeding spontaneously.
As many as 25% will re-bleed either during or after their hospital
admission.
While most patients have a self-limited illness, the reported mortality
ranges from 2-4%.
LOWER GI BLEEDING Dr. Aqeel Shakir
28-4-2015
4
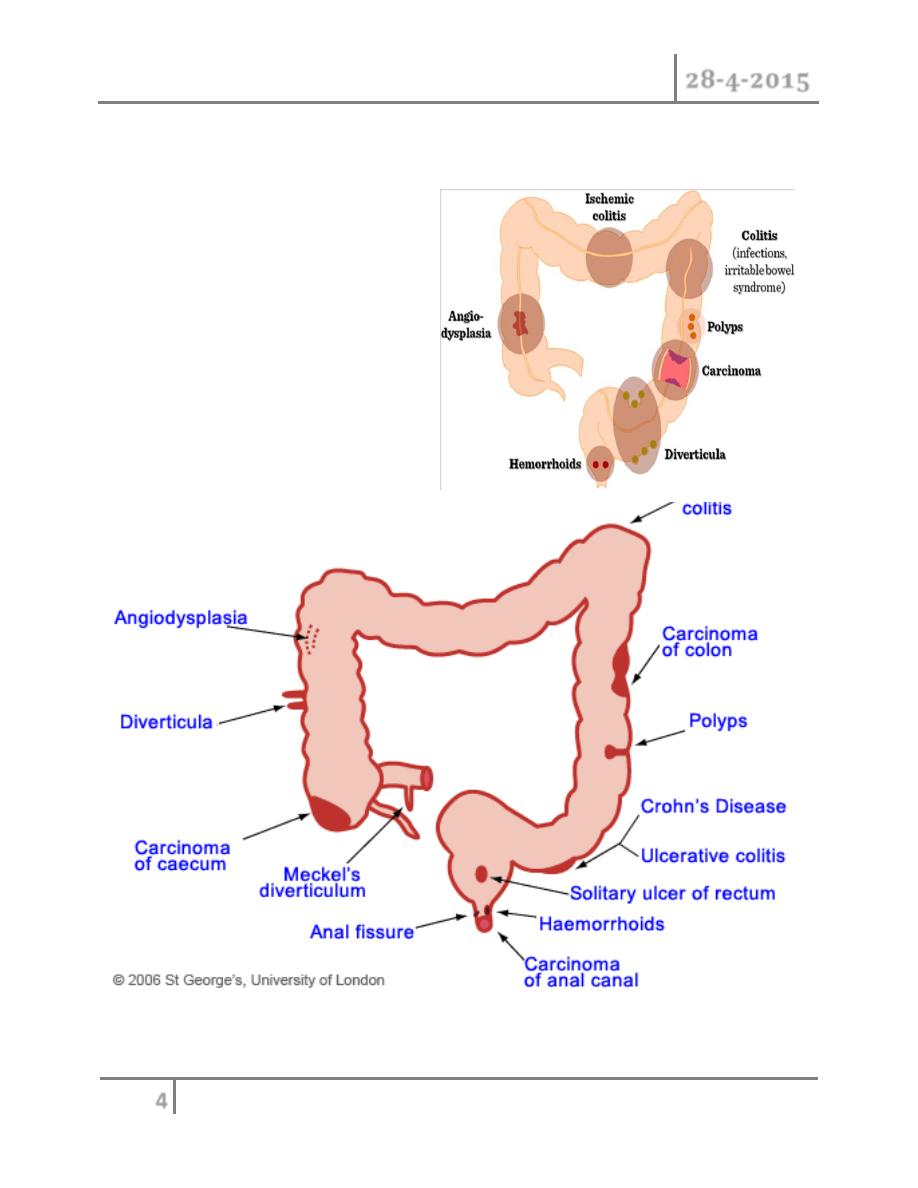
Among all patients presenting with lower GI bleeding, diverticular disease
is the most common cause, followed by, vascular anomalies or ischemic
colitis.
Etiology
Anorectal causes
Colonic causes
Small bowel causes
Vascular anamolies

LOWER GI BLEEDING Dr. Aqeel Shakir
28-4-2015
5
Anorectal causes :
• Include hemorrhoids -anal fissure and rectal ulcer.
• Bleeding from hemorrhoids and fissure is uncommonly associated
with hemodynamic instability or large volume of blood loss.
• While rectal ulcer can cause severe hemorrhage and hemodynamic
instability
• Possible causes of rectal ulcer are :
o Radiation.
o Sexual transmitted disease.
o NSAIDs.
o Liver disease.
o Trauma.
Diverticular disease:
• Contributes 20-60% of the cases of LGIB.
• In 75% of patients bleeding will stop spontaneously.
• Rebleeding rate after first episode 25% and increase to 50% after two
episodes.
• Diverticular bleeding is distributed equally between the right and left
sides of the colon.
• Observation alone is generally recommended following the first
episode of diverticular haemorrhage. However, following a second
episode, the risk of subsequent episodes appears to approximate 50%,
and thus elective resection has been recommended.
LOWER GI BLEEDING Dr. Aqeel Shakir
28-4-2015
6
Angiodysplasia:
• Only about 15% of patients with vascular ectasia will develop
gastrointestinal hemorrhage.
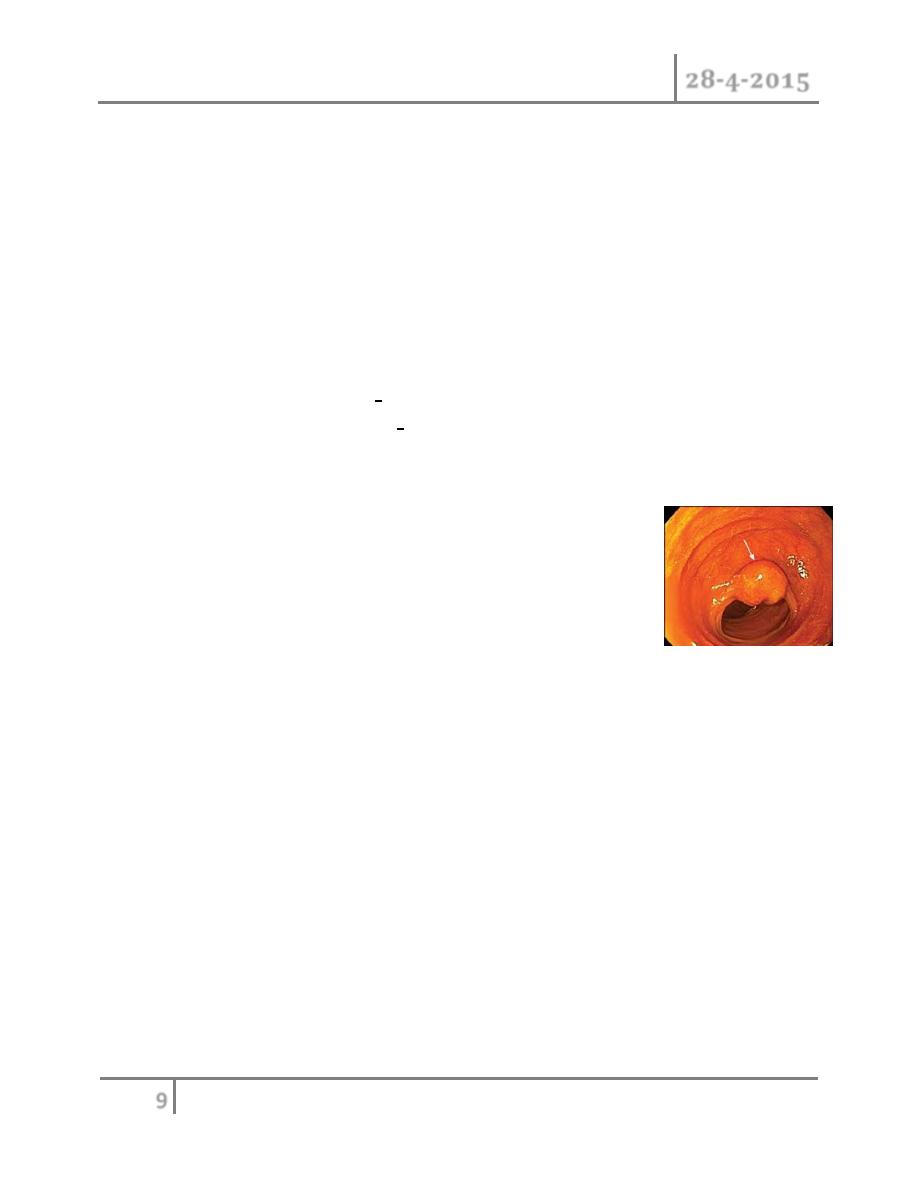
Colorectal neoplasm
• Although colorectal cancer is most commonly associated with occult
blood loss rather than overt bleeding, patients with rectosigmoid
lesions may present with hematochezia.
• CR-cancers are source of LGIB in 9-13% of patients.
Ischemic colitis
• Occurs in 9-18% of patients.
• Results from a sudden and often temporary reduction in mesenteric
blood flow, typically caused by hypoperfusion, vasospasm, or
occlusion.
• The usual areas affected are the “watershed” areas of the colon: the
splenic flexure and the rectosigmoid junction.
• Patients tend to be elderly, often with significant atherosclerosis or
cardiac disease.
Other colonic etiologies:
• Inflammatory bowel disease:
o Acute hemorrhage occurs 0.9-6% in CD and 1.4-4% in UC.
o Bleeding occurred in both young and old patients and not
related to disease duration.
LOWER GI BLEEDING Dr. Aqeel Shakir
28-4-2015
7
o Malignant lesion must be considered in patient with long
standing history of IBD and LGIB.
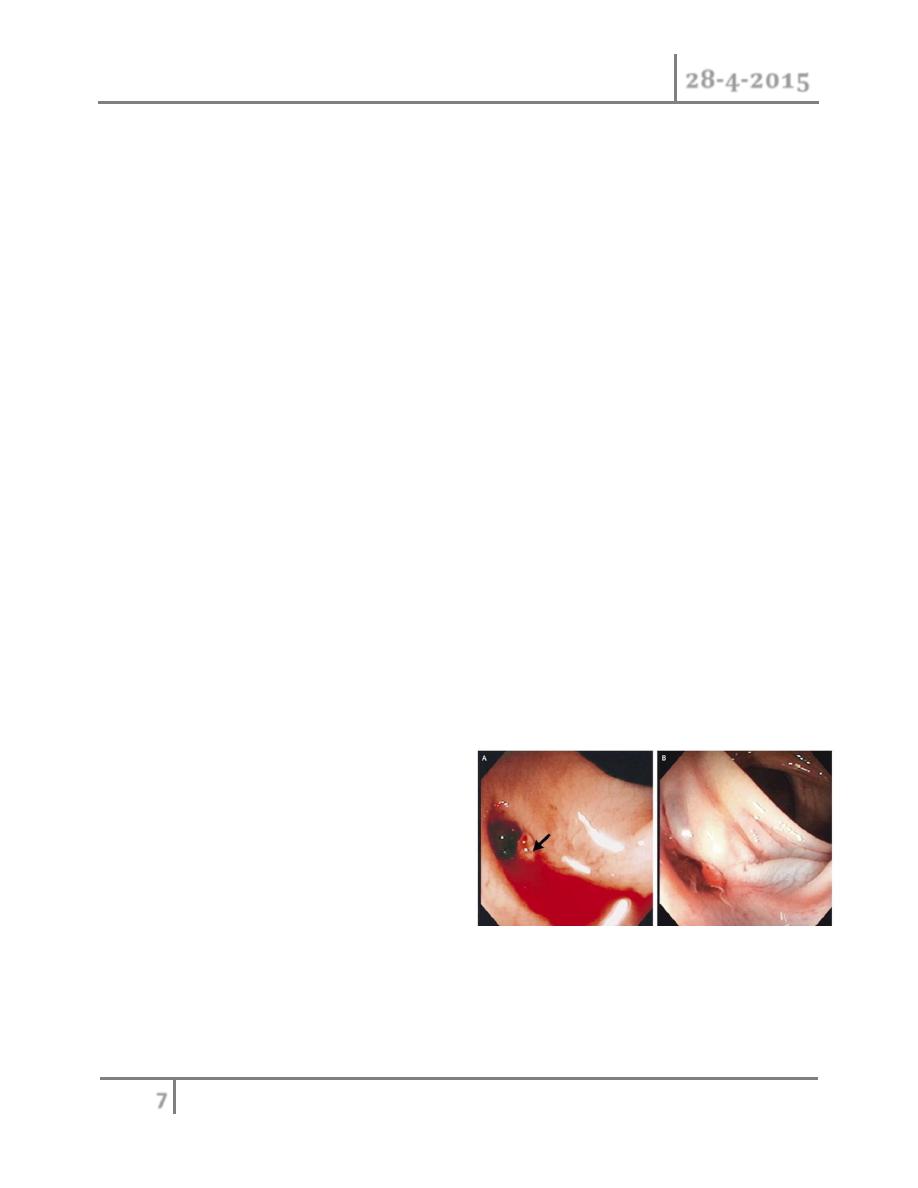
• Infectious colitis or enteritis :
• Radiation colitis/proctitis.
• Trauma, hematologic disorders and NSAIDs.
• Post polypectomy (occurs in 0.3% to 6.1% of polypectomies).
• Bleeding from CR-anastomosis (o.5-1.8%).
Small bowel sources account for 3-5% of all cases of LGIB :
o Angiodysplasia is most common cause of small bowel hemorrhage
(70-80%).
o small bowel diverticula,
o
Meckel’s diverticula,
o neoplasia,
o Crohn’s disease,
o aorto-enteric fistulas.
Forms of lower GI bleeding
Bright red hematochezia
Dark hematochezia
Bright red blood per rectum
Hematochezia is passage of bright red or maroon stool
LOWER GI BLEEDING Dr. Aqeel Shakir
28-4-2015
8
Presentation
Vital signs – 20-30% with shock
Form of bleeding –
Abdominal pain – Present versus absent, location
LOWER GI BLEEDING Dr. Aqeel Shakir
28-4-2015
9
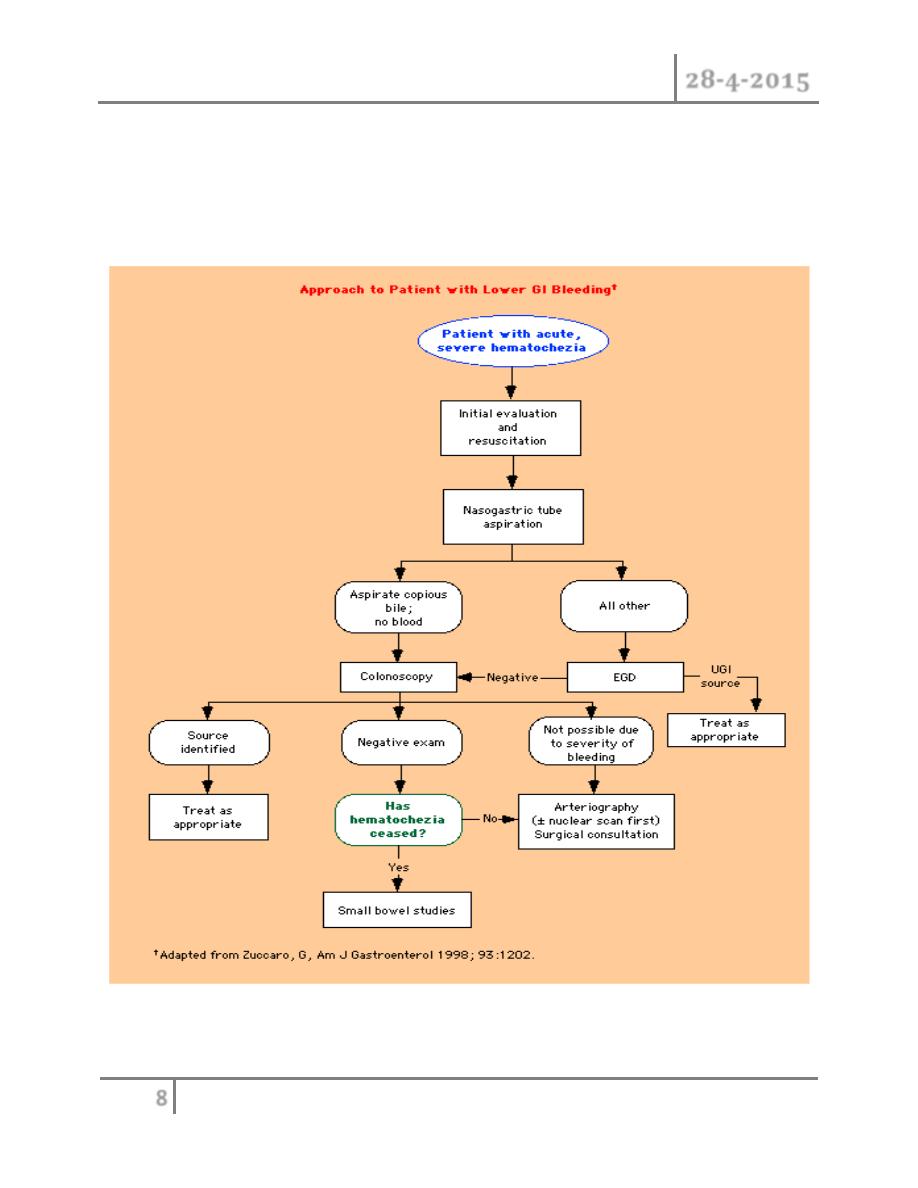
Nasogastric Aspirate
> 90% of those with red, pink or black aspirates have upper GI source
> 60% of those with negative (bilious) aspirate have lower source,
Sigmoidoscopy and colonoscopy
o Patients with bright red hematochezia and minimal blood loss can undergo
initial evaluation with anoscopy and flexible sigmoidoscopy, unless the
patient is age 50 or older(a full colonoscopy is generally recommended to
rule out a colonic neoplasm)
o Those with dark hematochezia or bright red blood per rectum and evidence
for significant blood loss should undergo full colonoscopy
o Active, brisk bleeding and continued hemodynamic
instability despite ongoing resuscitation is an indication
for emergency angiography rather than colonoscopy.
o Since lower GI bleeding can originate anywhere in the
small bowel or colon, angiography is also preferable to laparotomy in the
setting of such bleeding.
o Surgery is generally reserved for patients whose bleeding site is identified
by angiography but who are inappropriate for, or fail, angiographic therapy
MANAGEMENT
Stabilize the patient
Stop the bleeding
Find the source of bleeding
Prevent recurrence of bleeding
LOWER GI BLEEDING Dr. Aqeel Shakir
28-4-2015
10
Surgery - Indications in lower GI bleeding
o The majority of patients with LGIB will stop spontaneously and never
require surgery
o approximately 10-25% of patients will require operative intervention
o The indications for surgery include:
1. Continued or recurrent hemorrhage despite nonoperative attempts.
2. Transfusion requirement >6 units within 24 hours.
3. Hemodynamic instability patients who have massive ongoing bleeding
and are unresponsive to initial resuscitation.
#END
Dear Friends,
This is the last lecture I delivered to you this year, I hope they met your
satisfaction.
I’d like to thank you all for your support this year, you are really
amazing, that’s gave me the ambition to do my best & do help as much as
I can.
Meet you next year with a new hope to pass a new year; together .
Yours with love,
Ali Kareem
