Dr. Ayad Abbas
Lec. 1
FLUID & ELECTROLYTE
Tues. 23 / 9 / 2014
Published by : Ali Kareem
مكتب اشور لالستنساخ
5102
-
5102
1
Surgery
FLUID & ELECTROLYTE
Lec 1:
23/9/2014
د.اياد عباس
Total body fluid and its distribution
Water represents 60% of the mean body mass
The body fluid contained in two compartments which are separated by
cell membrane and these are:
1. Intracellular compartment ICC form 2/3 of TBF.
2. Extracellular compartment ECC form 1/3 of TBF.
Furthermore the ECC is subdivided into:
a.Intravascular 1/4 These 2 spaces are separated from each other by
b.Interstitial 3/4 endothelium of capillary wall.
These spaces are not rigid units, but they are in constant exchange
between them to be in balance.
Transcellular fluid: fluid in CSF, aqueus of eye, vitreous of eye and GIT
secretion.
These are ECF, but in special compartments and have rather different
function from the main mass of the body fluid and they are usually
considered separately.
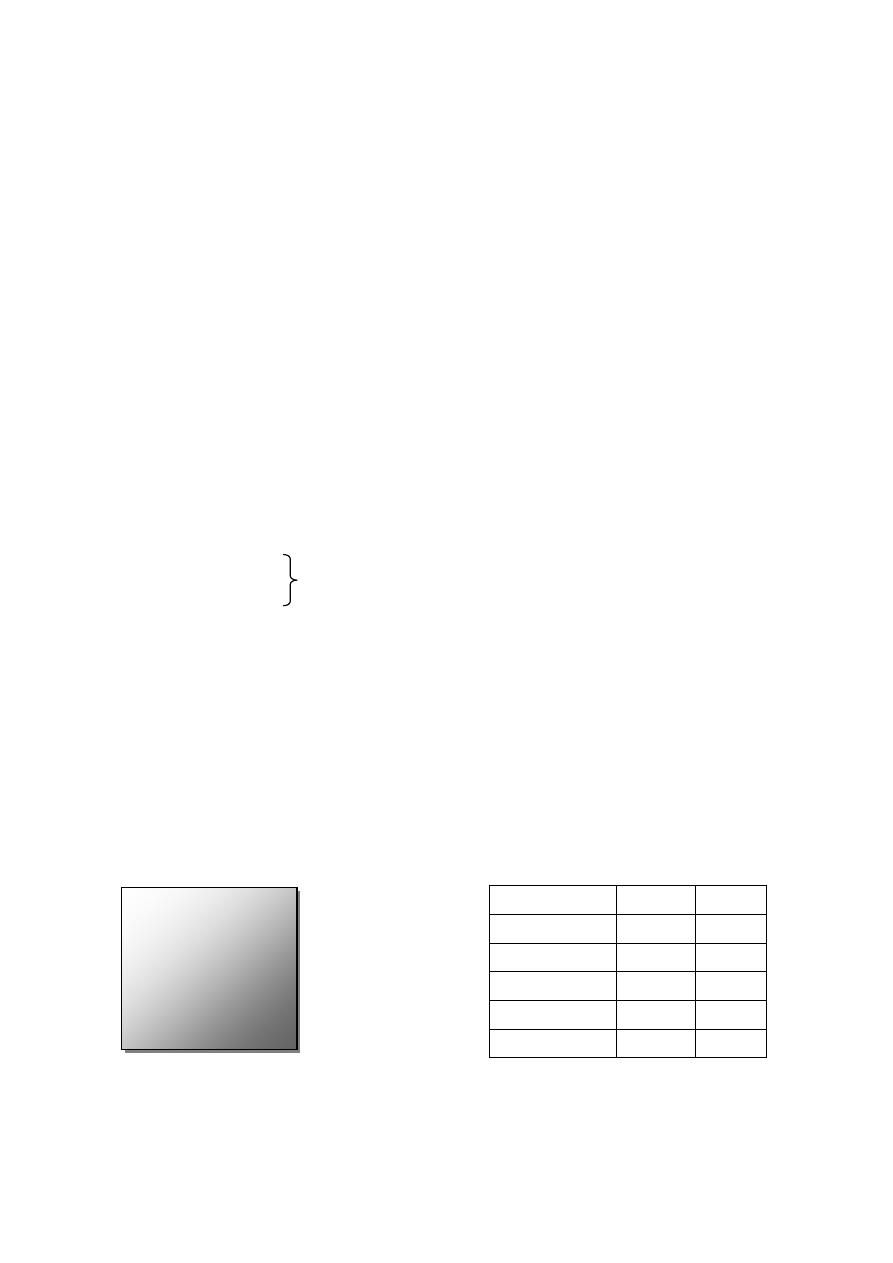
* For adult 70 kg body weight.
Litres*
%
compartment
45
100%
TBF
30
66%
ICF
15
33%
ECF
12
25.5%
ISF
4
7.5%
IVF
Fat 15%
Protein 18%
Mineral 7%
ICF 40%
Interstitial 15%
Intravascular 5%

2
Fluid intake
Fluid intake is derived from two sources:
(1) exogenous; and (2) endogenous.
Exogenous water is either drunk or ingested in solid food.
The quantities vary within wide limits, but average 2—3 litres per 24 hours,
Taking into consideration their body weight, the water requirements
of infants and children are relatively greater than those of adults because of:
(1) the larger surface area per unit of body weight;
(2) the greater metabolic activity due to growth; and
(3) the comparatively poor concentrating ability of the immature
kidney.
Endogenous water is released during the oxidation of ingested food;
the amount is normally less than 500 ml 24 hours.
1 gm of fat → 1 ml of fluid,
1 gm of protein → 0.4 ml of fluid,
1 gm of CHO → 0.6 ml of fluid
However, during starvation, this amount is supplemented by water released
from the breakdown of body tissues.
Fluid output
Water is lost from the body by four routes.
1 • By the lungs. About 400 ml of water is lost in expired air each 24 hours. In
a dry atmosphere, and when the respiratory rate is increased, the loss is
correspondingly greater (this also applies to the patient who has their trachea
intubated).
2•By the skin. When the body becomes overheated, there is visible
perspiration, but throughout life invisible perspiration is always occurring. The
cutaneous fluid loss varies within wide limits in accordance with the
atmospheric temperature and humidity, muscular activity and body
temperature. In a temperate climate the average loss is between 600 and 1000
m1124 hours.
3
3• Faeces. Between 60 and 150 ml of water are lost by this route daily. In
diarrhoea this amount is greatly multiplied.
4• Urine. The output of urine is under the control of multiple influences, such
as blood volume, hormonal and nervous influences, among which the
antidiuretic hormone plays a major role controlling tonicity of the body fluids,
a function that it performs by stimulating the reabsorption of water from the
renal tubules, thus varying the amount excreted after the requirements of the
first three routes have been met. The normal urinary output is approximately
1500 ml124 hours, and provided that the kidneys are healthy, the specific
gravity of the urine bears a direct relationship to the volume. A minimum
urinary output of approximately 400 m1124 hours is required to excrete the end
products of protein metabolism.
Fluid Balance
Defined as a ratio between water input (through all routs) and water output
(through all routs and it is normally equal to one).
Fluid balance = fluid input/fluid output = 1
◊ If the ratio > 1→ +ve fluid balance (input > output).
◊ If the ratio < 1→ -ve fluid balance (input < output). Electrolyte distribution
in the body
Electrolyte distributed in the body compartment in different
concentration.
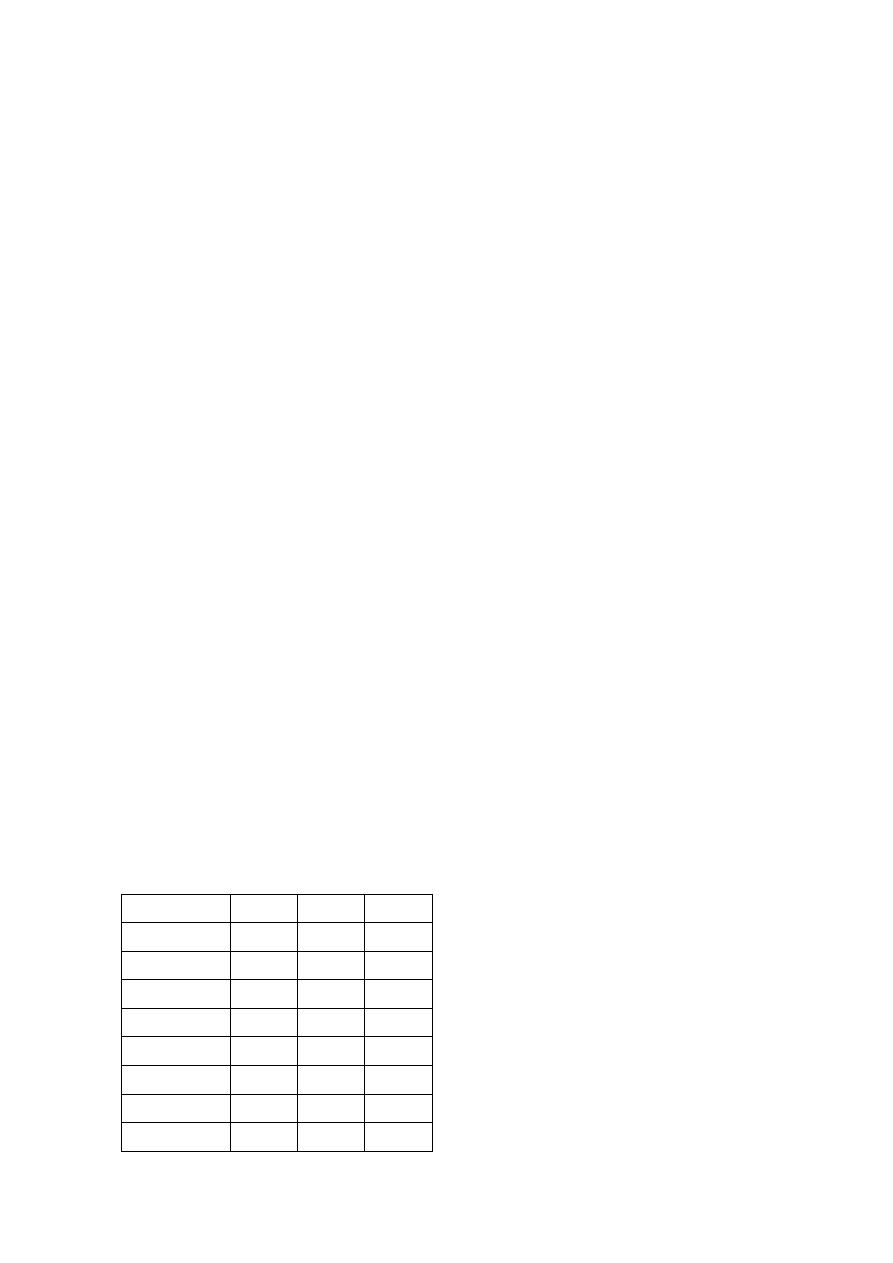
IS
IV
IC
Electrolyte
142
145
10
Na
+
4
4
140
K
+
3
3
< 1
Ca
+2
2
2
50
Mg
+2
110
105
4
Cl
-
28
24
10
HCO
3
-
28
2
75
HPO
4
-2
2
7
16
Protein
4
◊ The daily requirement of Na
+
= 1-2 mmol/day.
◊ The daily requirement of K
+
= 0.5-1 mmol/day.
Osmolarity: is a number of osmoles per liter of solution and plasma
osmolarity .
Osmolarity = 280-300
osmolarity
= 2 [Na
+
] + 0.055 [Glc] + 0.36 [BUN
**
]
=2 X 140 + 0.055 X 120 + 0.36 X 40 =300
*The 2 is for Na
+
+ Cl
-
**Blood Urea Nitrogen
◊ Movement of fluid between IC & EC depends on the tonicity
(OSMOLARITY) of ECF.
◊ ↑ tonicity of ECF → fluid shift from ICC to ECC → shrinkage of cell.
◊ ↓ tonicity of ECF → fluid shift from ECC to ICC → swelling of cell.
Shrinkage is a dangerous effect, it have neurological, respiratory and
cardiovascular effect. It can cause Drowsiness, Confusion, Convulsion,
Coma, Shallow Breathing, Apnea, Tachycardia and Finally Stand Still.
Swelling (Edema) also has a dangerous effect, ex: incase of CEREBRAL
EDEMA ,this edema may cause CVA (cerebro-spinal accident) which
occur due to the compression on the vessel that carry the O
2
and
Nutrients to the Cerebral hemisphere.
◊ As Intravascular compartment is separated from Interstitial compartment by
semi permeable membrane (permeable to electrolyte, water and glucose and
impermeable to large molecule e.g. protein).Then The movement between i.v
& i.s governed by OSMOSIS and ONCOTIC PRESSUER.
In case of Liver Cirrhosis and Nephrotic Syndrome , there will be loss
of Proteins that will lead to Decreasing the ONCOTIC PRESSUER.
5
Osmosis: Diffusion of solvent molecule from a region of low concentration of
solute to a region of high concentration of solute through a membrane
impermeable to that solute.
Osmotic pressure: The pressure of solution that is necessary to prevent
solvent diffusion.
Oncotic pressure: The pressure of plasma that is necessary to prevent
movement of fluid from I.V to I.S compartment. It reflect the presence of
proteins in I.V compartment.
So movement of fluid between i.v and i.s depends on 3 factors:
1.Hydrostatic pressure of i.v
2.Hydrostatic pressure of i.s
3.Oncotic pressure of i.v
= HP (vessels) - [HP (i.s) + OP (vessels)]
◊ In artery = 37- (1+25) = +11→ shift to interstitial
◊ In veins = 17 - (1+25) = -9 → shift to vein
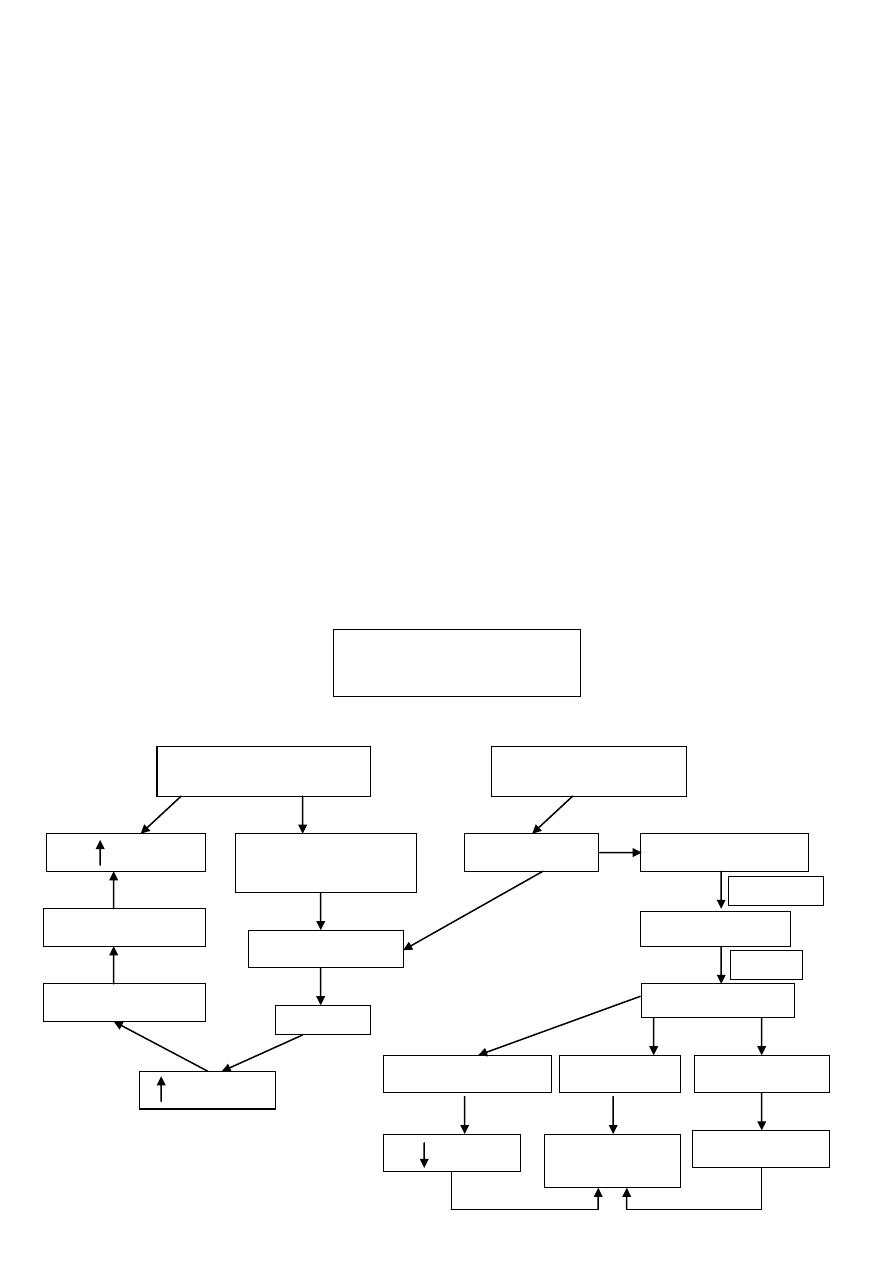
Dilution of ECF
HyperOsmolarity
HypoVolaemia
Angiotensinogen
ADH
Baroreceptor
H
2
O retention
Angiotensin I
Angiotensin II
Osmoreceptor
In Ant.Hypothalamu
s
Hypothalamus
RBF
H2O
Retention
Na retention
Vasoconstriction
ADH
Aldosterone
Thirst
H
2
O Intake
ACE
Renin
Control of body
fluids and electrolytes
6
SUMMARY
1.Defence of tonicity:
● Hyperosmolarity thirst
fluid retension
↑ADH
● Hypoosmolarity: vice versa.
2.Defence of volume:
Volume (body fluid) determined by total amount of osmoticaly active solute in
ECF → ; therefore the mechanism to defense the volume is the same
mechanism to defense the Na
+
.
Water depletion
-Pure water depletion is usually due to diminished intake. This may be due to:
lack of availability,
-difficulty or inability to swallow because of painful conditions of the mouth
and pharynx,
-or obstruction in the oesophagus.
-Exhaustion and paresis of the pharyngeal muscles will produce a similar
picture.
-Pure water depletion may also follow the increased loss from the lungs after
tracheostomy. This loss may be as much as 500 ml in excess of the normal
insensible loss. After tracheostomy, humidification of the inspired air is an
important preventive measure.
Clinical features
The main symptoms are weakness and intense thirst.
The urinary output is diminished and its specific gravity increas-ed.
The increased serum osmotic pressure causes water to leave the cells
(intracellular dehydration), and thus delays the onset of overt compensated
hypovolaemia (see below).

7
Water intoxication
This can occur when excessive amounts of water, low sodium or
hypotonic solutions are taken or given by any route. The commonest cause on
surgical wards is the overprescribing of intravenous 5per cent glucose solutions
to postoperative patients. Colorectal washouts with plain water, instead of
saline, have caused water intoxication during total bowel wash-through prior to
colonic surgery. A major component of the TURP (transurethral resection of
the prostate) syndrome is the water intoxication caused by excessive uptake of
water (and glycine) from irrigation fluid.
Similarly, water intoxication can occur if the body retains water in
excess to plasma solutes. This can be seen in the syndrome of inappropriate
antidiuretic hormone (SIADH) secretion which is most commonly associated
with lung conditions such as lobar pneumonia, empyema and oat-cell
carcinoma of bronchus, as well as head injury.
Clinical features
These include drowsiness, weakness, sometimes convulsions and
coma. Nausea and vomiting of clear fluid are common, and, with the notable
exception of the SIADH, usually the patient passes a considerable amount of
dilute urine. Laboratory investigations may show a falling haematocrit, serum
sodium and other electrolyte concentrations.
Treatment
The intake of water having been stopped, the best course is water
restriction. If the patient fails to improve, transfer to an intensive care or high
dependency unit will be necessary for more invasive monitoring and controlled
manipulation of fluids and electrolytes. The administration of diuretics or
hypertonic saline should not be undertaken lightly as rapid changes in serum
sodium concentration may result in neuronal demyelination and a fatal
outcome.
Types of fluids used for mangment:
1- Crystaloid: (Isotonic – Isoosmolar):

8
a- Normal Saline contain NaCl 0.9 ٪
b- Glucose Water cntain glucose 5 ٪(inside the body glucose enter cell and
the I.V become hypoosmolar).
c- Glucose Saline conatin NaCl and glucose and according to the ٪of NaCl
called ½ , 1/3 and 1/5.
d- Ringer solution and ringer lactate contain NaCl, K
+
, Ca
+2
, HCO
3
and
lactate.
2- Colloid Fluids: (Hyperosmolar):
Contain large particles that cannot pass through the semi-permeable
membrane that separate the I.V compartment from I.S compartment.
Dextran 40, Dextran 70, Hemacel, Jel Fusion, Albumin.
These fluids should not be given for more than 1 L.
Complication of these Fluids:
1- Diluted Thrombocytopnea.
2-Interferce with Cross Match.
3- Anaphylactic reaction.
the 2
nd
and 3
rd
complications are especially of Dextrans.
Suggested Routin Postoperative Fluid Regime,
taking in account the
body response to Trauma “SURGERY”:
1- In the 1
st
24 hours after surgery (zero day of operation): the patient requires
no salts and less water than normal requirement , so 2 liters of 5 ٪dextrose
is enough.
2- In the 1
st
and 2
nd
Post-Operative Day: the metabolic response to surgery
diminishes and the patient requires 2 liters of 5 ٪dextrose and 1 liter of 0.9 ٪
normal saline.
3- In the 3
rd
Post-Operative day and thereafter 0.5-1 mmol/kg of KCl is add to
fluid per 24 hours.
Printed by :
Ali Malik

9
Special greetings to: Marwan Zuhair, Mohamed Esam, Sabah Nasir,
Yasir Kasim and to Zaid Fareed
