Dr. Abdul Ameer M.
Hussein
Lec. 4
Chronic Peripheral
Vascular Disease
Tues. 23 / 12 / 2014
Published by : Ali Kareem
مكتب اشور لالستنساخ
2014 – 2015
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
2
Chronic peripheral vascular disease
(Ischaemia(
Peripheral
vascular disease (PVD), also known as
peripheral arterial disease
(PAD) or peripheral artery occlusive disease
(PAOD)
Types of PVD
There are two main types of PVD :
Organic PVD: This involves changes in blood vessel structure. This type of
PVD causes inflammation, tissue damage, and blockages
Functional PVD: This does not involve physical problems in the blood
vessels. It causes incidental or short-term symptoms. These are usually
spasms that occur erratically
Organic PVD Causes
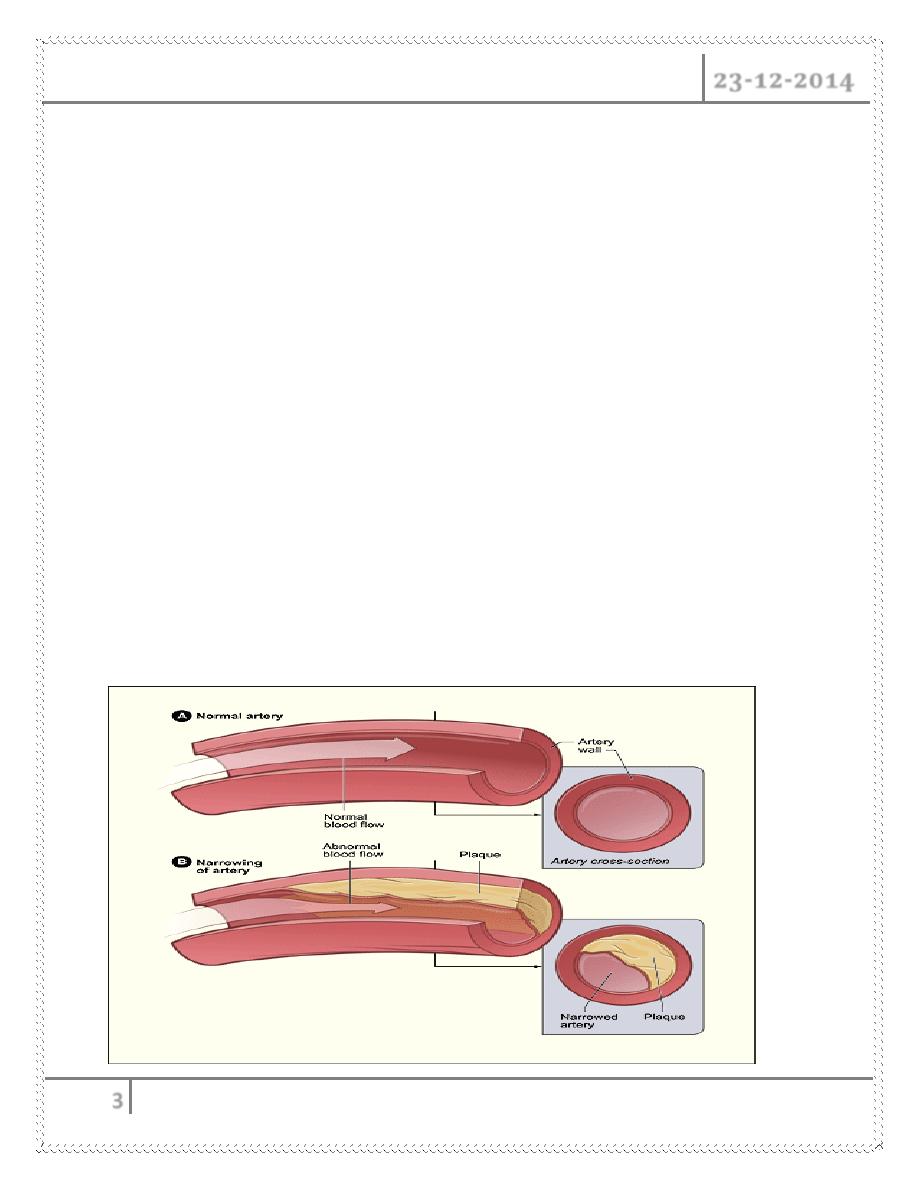
Peripheral artery disease is often caused by atherosclerosis.
In atherosclerosis, fatty deposits (plaques) build up in the artery walls and
reduce blood flow
Less commonly, the cause of peripheral artery disease may be
Blood vessel inflammation.
Injury to the limbs.
Unusual anatomy of the ligaments or muscles.
Radiation exposure
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
3
Functional PVD Causes
The body responds to certain external stimuli by restricting blood flow to the
peripheral vessels. The most common causes of functional PVDs are:
Emotional stress
Smoking
Cold temperatures
Operating vibrating machinery or tools
ATHEROSCLEROSIS
Atherosclerosis is a chronic inflammatory response of the arterial wall
initiated by injury to the endothelium
Atherosclerosis is a slow, complex disease in which fatty substances,
cholesterol, cellular waste products, calcium, and other substances build up
– called plaque - in the inner lining of an artery
Atherosclerosis is a slow, complex disease in which fatty substances,
cholesterol, cellular waste products, calcium, and other substances build up
– called plaque - in the inner lining of an artery
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
4
Risk Factors For Atherosclerosis
Major Risk factor
Constitutional
o Age
o Sex
o Genetic
o Familial
Acquired
o Hyperlipidemia
o Hypertension
o Cigarette smoking
o Diabetes mellitus
Minor Risk factors
o Environmental influence
o Obesity
o Hormone estrogen def Physical inactivity
o Stress
o Infection(C. pneumonia CMV)
o Homocystin urea
o Alcohol
Complications of atherosclerosis
1- Narrowing of vascular lumen … chronic ischemia
2- Superimposed thrombosis … acute ischemia
3- Ulceration with liberation of fatty core … acute ischemia, fat emboli, DIC
4- Pressure atrophy of the media with fibrosis….weakening of the wall ….
Aneurysmal dilatation
5- Dystrophic calcification
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
5
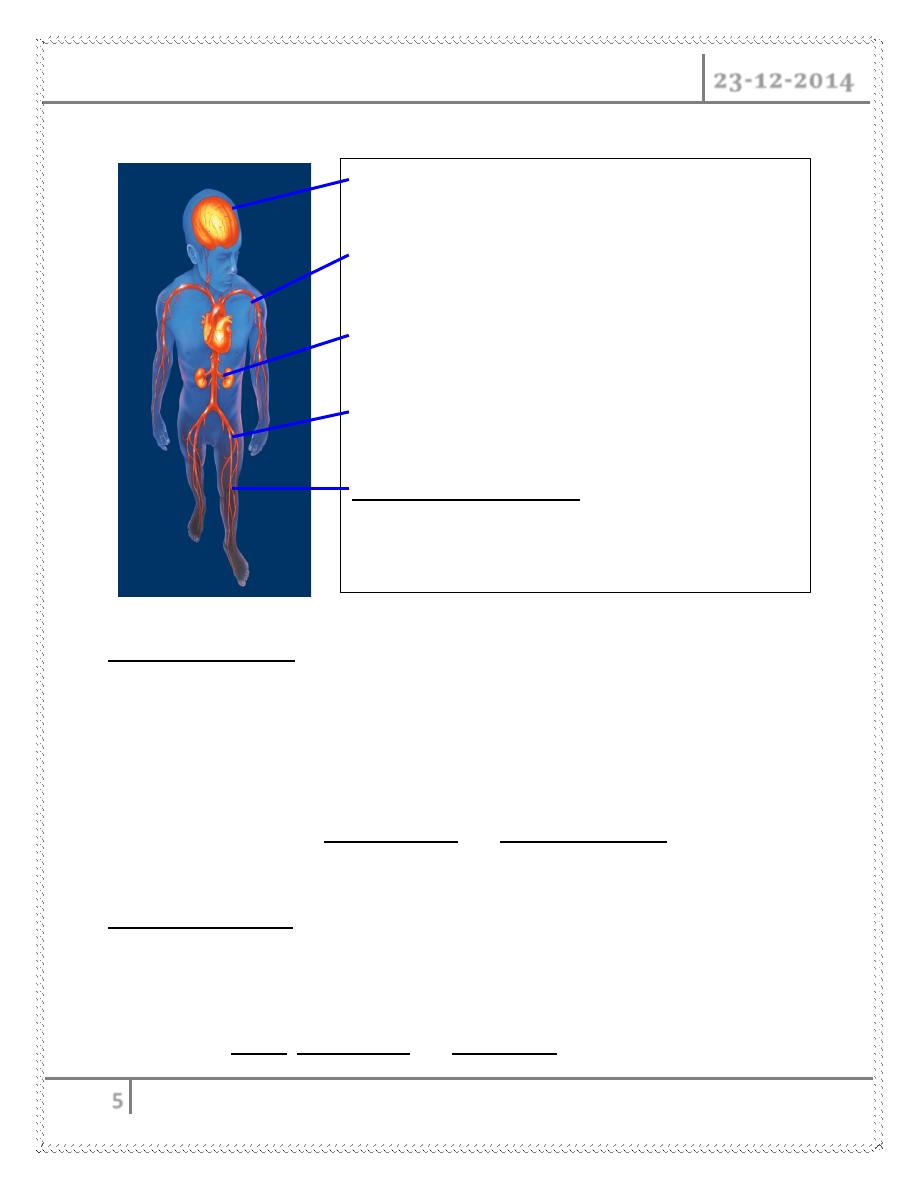
Major manifestations of atherothrombosis include
Arterial Insufficiency
There is a deceased blood flow toward the tissues, producing ischemia
Pulses one usually diminished or absent
Sharp, stabbing pain occurs because of the ischemia,
Particularly with activity
There is interference with nutrients and 0
2
arriving to the
Tissues, leading to ischemic ulcers and changes in the skin
Venous Insufficiency
There is deceased return of blood from the tissues to the heart
Leads to venous congestion and stasis of blood
Pulses are present
Lead to edema, skin changes and stasis ulcers
Cerebrovascular disease
Coronary artery disease
Renal artery stenosis
Visceral arterial disease
Peripheral arterial disease
–
Intermittent claudication
–
Critical limb ischemia
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
6
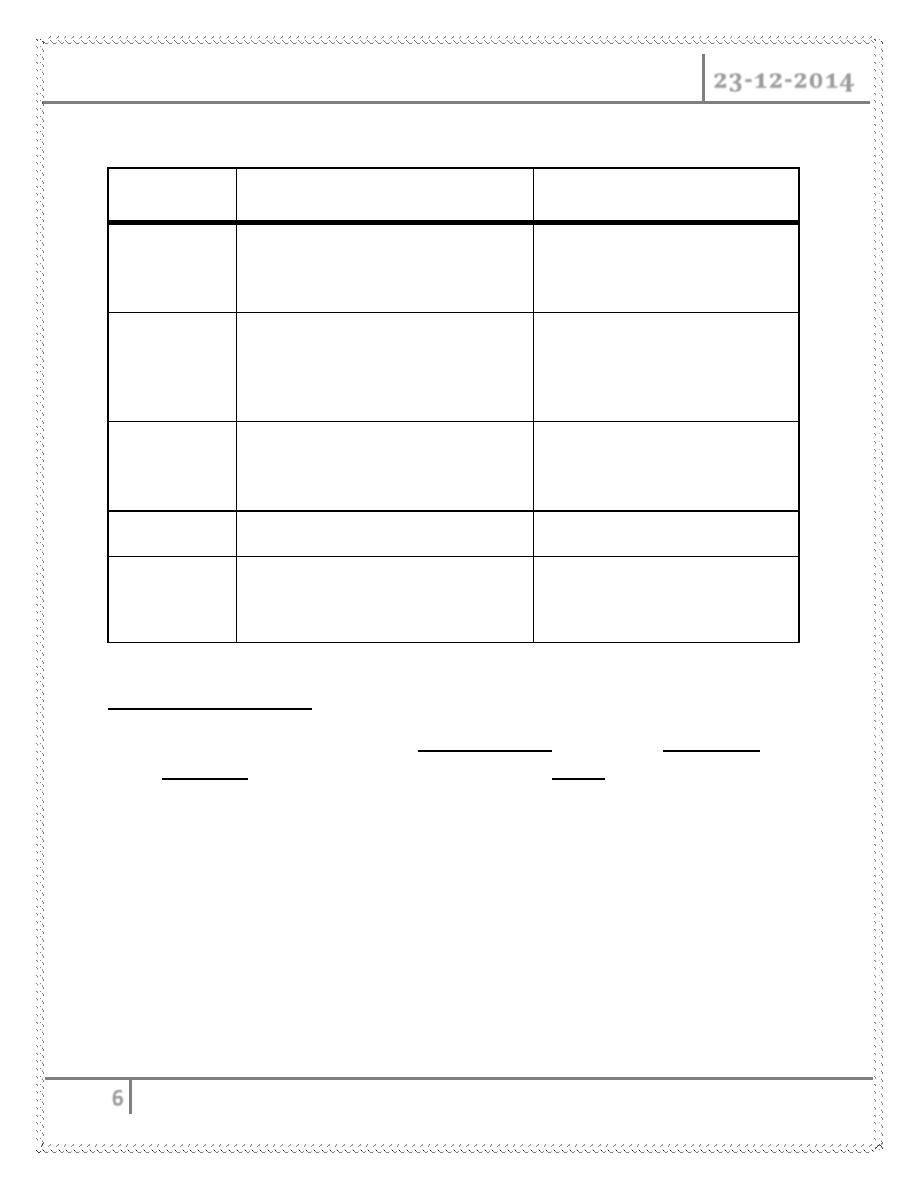
Comparison of characteristics of Arterial & Venous Disorders
Arterial Disease
Venous Disease
Skin
cool or cold, hairless, dry,
shiny, pallor on elevation,
rubor on dangling
warm, tough, thickened,
mottled, pigmented areas
Pain
sharp, stabbing, worsens w/
activity and walking, lowering
feet may relieve pain
aching, cramping, activity
and walking sometimes
help, elevating the feet
relieves pain
Ulcers
severely painful, pale, gray
base, found on heel, toes,
dorsum of foot
moderately painful, pink
base, found on medial
aspect of the ankle
Pulse
often absent or diminished
usually present
Edema
infrequent
frequent, esp. at the end of
the day and in areas of
ulceration
Associations with PVD
Many
PVD patients also have
angina pectoris
or have had
myocardial
infarction
.
There is also an increased risk for
stroke
The
moderate consumption of alcohol has been found to be associated with
a
reduction of the risk of PVD by almost one-third compared to those who
do not
drink alcohol
Clinical Presentation
Patients have a decreased quality of life due to a reduction in walking
distance and speed leading to immobility
Ranges in severity from intermittent claudication to limb ischemia
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
7
Can present with buttock, thigh, calf or foot claudication singly or in
combination
Diminished pulses with occasional bruits over stenotic lesions
Poor wound healing, unilateral cool extremity, shiny skin, hair loss, and nail
changes
Only 1 in 10 patients with PAD has classical symptoms of intermittent
claudication (IC)
1 in 5 people over 65 has PAD
†
Claudication
literally 'limping' (Latin), is a medical term usually referring to impairment in
walking, or pain, discomfort or tiredness in the lower limb that occurs during
walking and is relieved by rest
Foot
o Occlusive disease of the tibial and peroneal vessels
Calf
o Cramping in upper 2/3 usually due to SFA stenosis
Thigh
o Usually occlusion of the common femoral artery
Buttock and Hip
o
Aortoiliac occlusive disease (Lariche’s syndrome)
Classification
I.
Mild pain on walking
"(
claudication)
II.
Severe
pain on walking relatively shorter distances (intermittent
claudication)
III.
Rest pain
IV.
Tissue
loss (gangrene)
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
8
Natural History of PAD
Associated with significant mortality because of association with coronary
and cerebrovascular events including death, MI, and stroke
6x more likely to die within 10 yrs than patients without PAD
5 yr mortality rate in pts with claudication is about 30%
Continued use of smoking results in a two fold risk of mortality
Diagnosis
Ankle
brachial pressure index
(
ABPI
/
ABI
)
which is a measure of the fall in
blood
pressure in the arteries supplying the legs. A reduced ABPI (less than
0.9
)
is consistent with PVD. Values of ABPI below
0.8
indicate moderate
disease and below
0.5
severe disease
Doppler
ultrasound
Angiography
Computerized tomography (CT) scanners provide
direct imaging of the
arterial system as an alternative to angiography
TREATMENT
Dependent on the severity of the
disease, the following
steps can be taken
Conservative
measures
Anti-platelet agents
Diabetic control
Smoking cessation
Anti- hypertensive
Statin therapy
Weight reduction
Exercise rehabilitation
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
9
Intervention
therapy
Angioplasty (PTA or percutaneous
transluminal angioplasty) can be done
on solitary lesions in large arteries
,
such as the femoral artery
.
Stenting
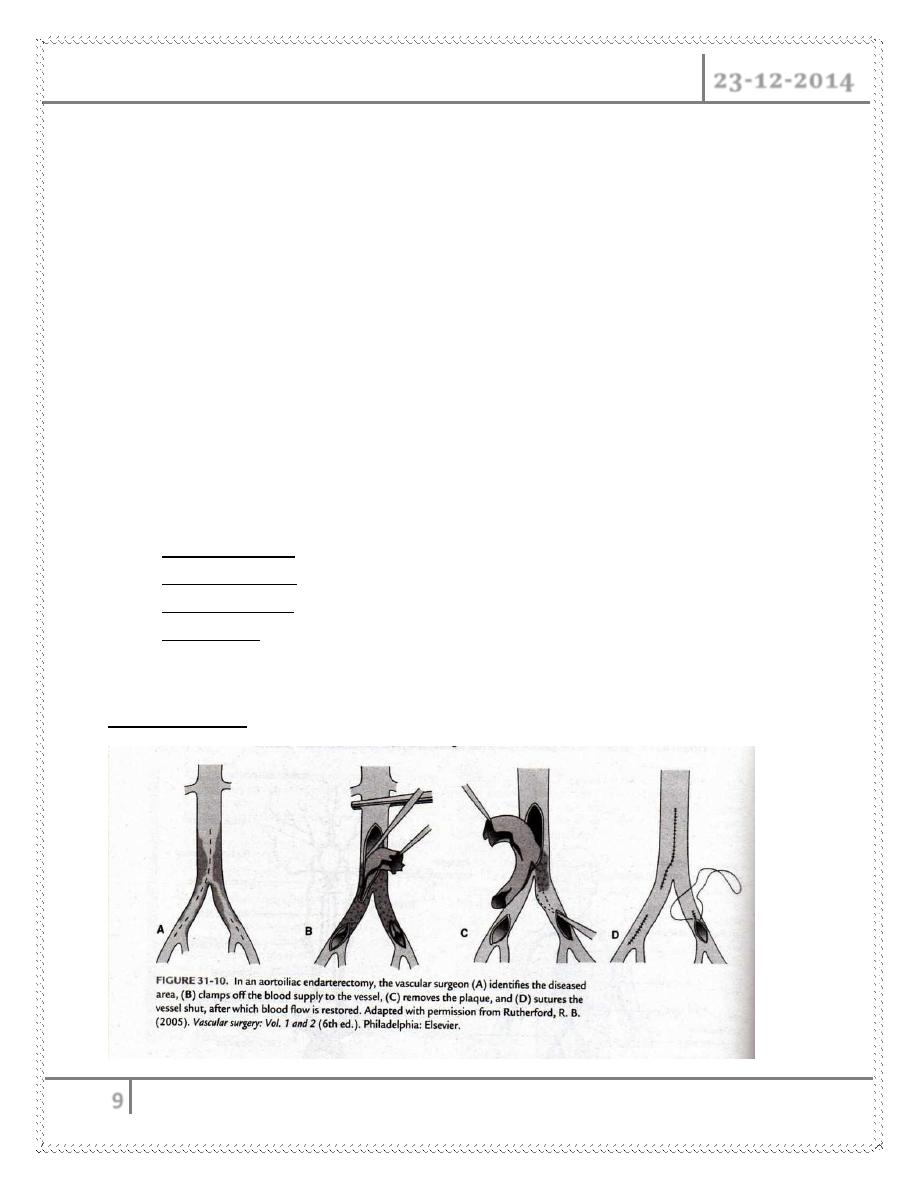
Surgical therapy
Lesions might be better treated surgically if :
Long segments
Multi focal stenosis
Eccentric, calcified lesions
We may do
Bypass grafting
.
Endarterectomy
Sympathectomy
.
Amputation
Endarterectomy
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
10
BURGER’S DISEASE
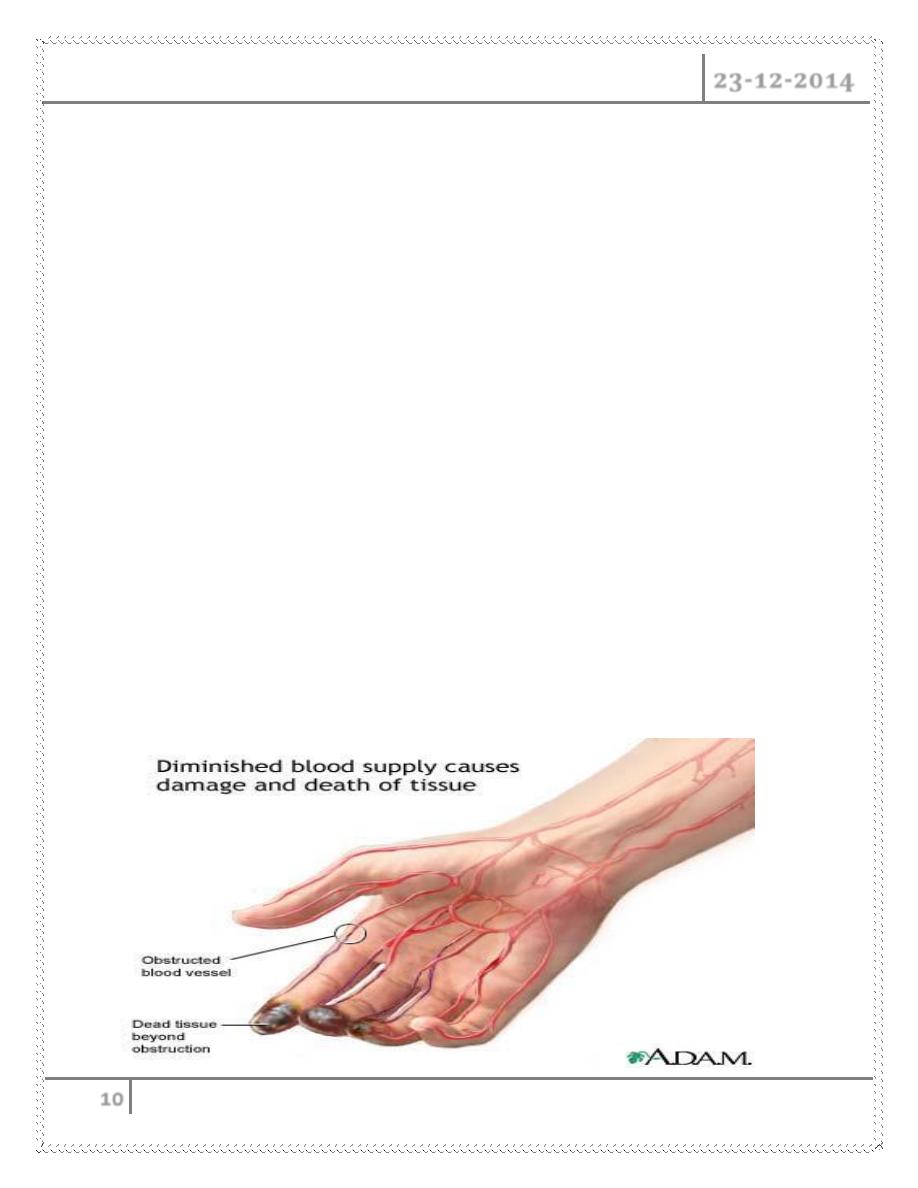
It is called Thrombo angitis oblitrans because histologically was characterized by
thrombosis in both arteries and veins, and were associated with marked
inflammatory response which may lead to complete obstruction it affect medium
and small vessel , usually femoral and brachial arteries are not involved
Clinical features
It begins in young adult life between 20 -35 years
Associated with smoking especially early smoking
Exacerbation with smoking
Remission with stop smoking
Cold sensitivity
Intermittent claudication
Rest pain
Pale & cold
Numbness and Paraesthesia
Diminish pulses
May be gangrene
Thromboangitis Obliterans
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
11
TREATMENT
Conservative treatment
Surgical treatment
Sympathectomy
Amputation when gangrene develop
RAYNAUD’S DISEASE
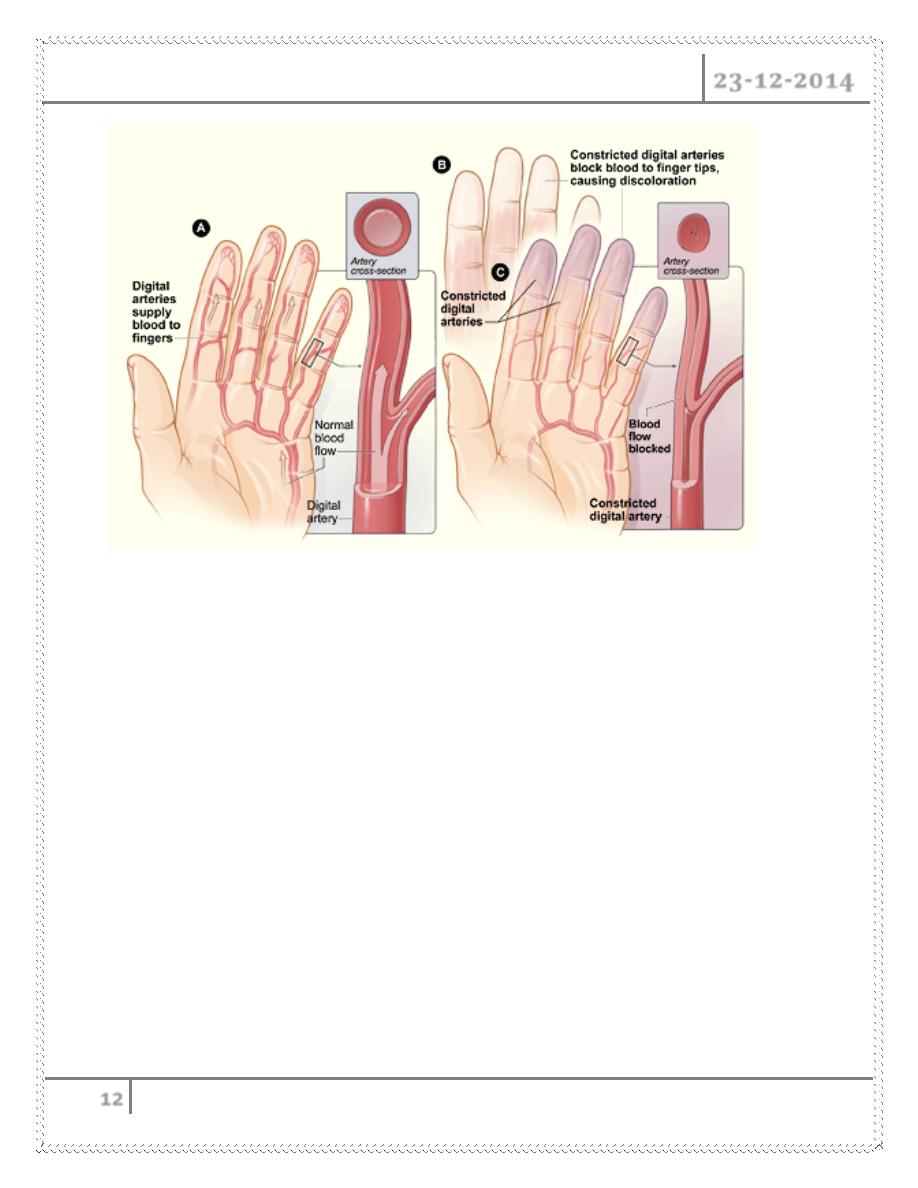
Is a disease characterized by episodic attacks of vasospasm causing closure of the
small sized arteries and arteriole of the distal part of the extremity in response to
cold exposure or emotional stimuli, it usually affect upper limb arteries
Pathology
- The condition is attributed to abnormal sensitivity in the direct response
of the artery to cold
- When cooled these vessels go into spasm and as a result the part become
pale, then the decrease in theblood flow lead to accumulation of
metabolite in the capillaries so the capillaries dilated and become filled
with deoxygenated blood so the part become swollen and dusky
- As the attack passes off the arteries relax, oxygenated blood returns into
the capillaries so hands become red with burning pain
- Later oblitrative changes occur leading to ischemic changes of the tips
of the fingers
Chronic PVD Dr. Abdul Ameer M. Hussein
23-12-2014
12
Clinical Features
Burning pain in the fingers.
Color changes ( pallor, cyanosis and redness).
Normal peripheral pulses.
Later ulceration and gangrenous changes
TREATMENT
Avoid the causative factors
Operative treatment – Dorsal sympathectomy
Done By
Ali Kareem
