
Lect. 14
The microcirculation and the lymphatic system
Objectives:
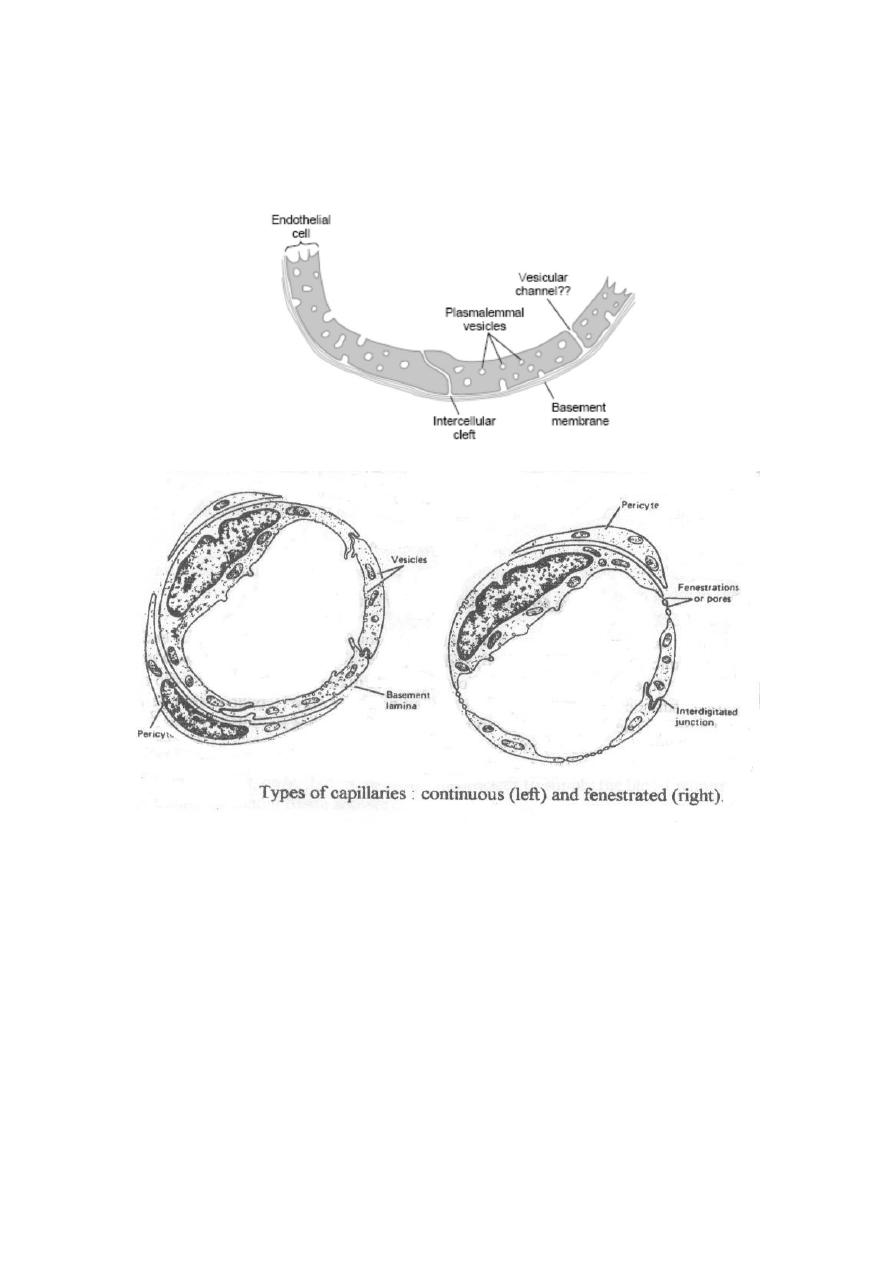
1. State (with the aid of diagram) the basic structure of a precapillary
sphincter and a capillary.
2. Define the term oncotic (colloid osmotic) pressure and state how it
is conferred to plasma.
3. State and explain briefly the effects on tissue fluid formation in a
vascular bed of: altered capillary hydrostatic pressure, decreased
plasma protein concentration, elevated central venous pressure,
increased capillary permeability, and obstruction of lymph
drainage.
4. Define the term edema.
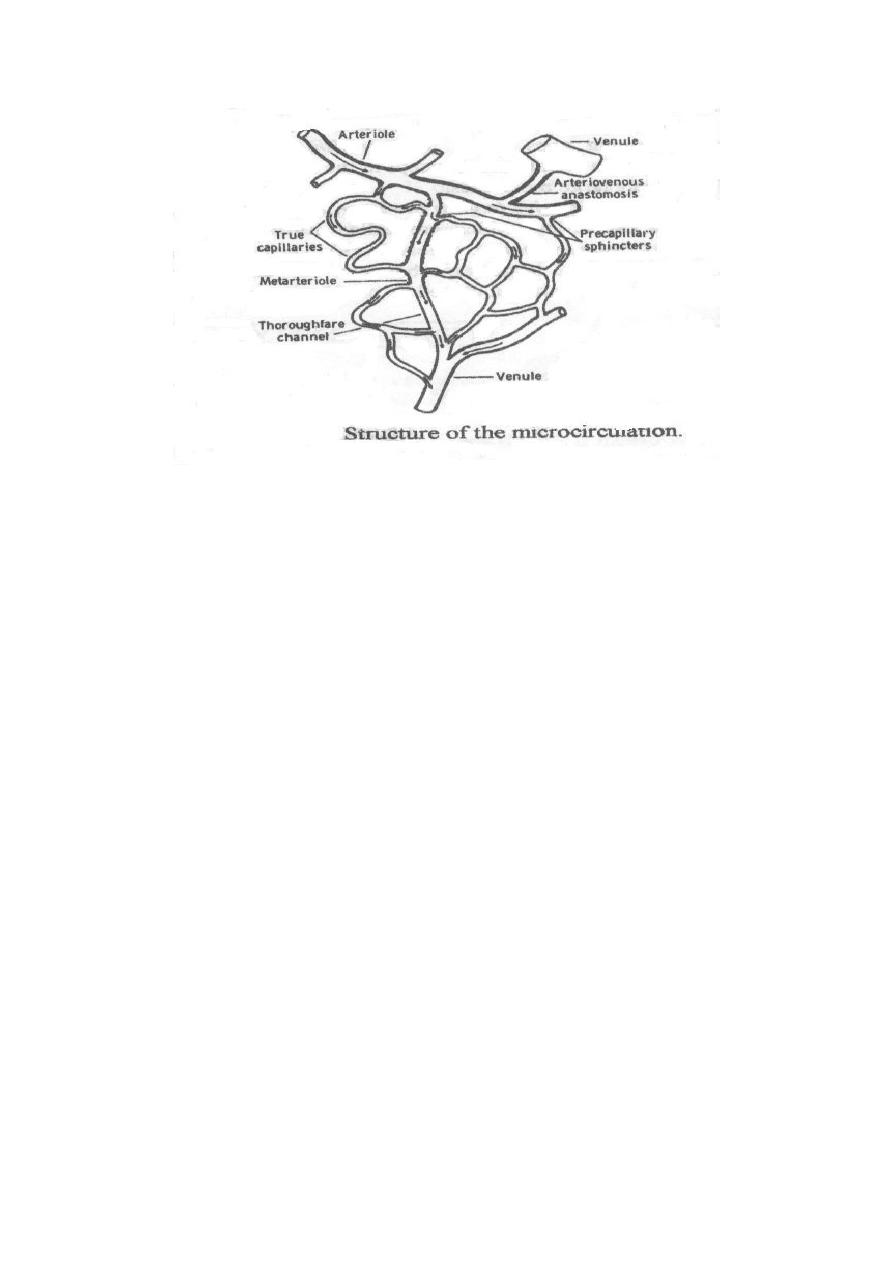
Structure of the microcirculation:
The arterioles divide into smaller vessels called metarterioles and true
capillaries arise from both the arterioles and metarterioles. The openings
of the true capillaries are surrounded by minute smooth muscles called
precapillary sphincters which respond well to various stimuli.
Capillaries are generally made up of a single layer of endothelial cells
surrounded by a basement membrane and special cells called pericytes,
which are contractile cells and also release many vasoactive agents.
Capillaries are divided into 3 main types:
1-Continuous capillaries (in all muscles and the brain):
In this type, the edges of the endothelial cells interdigitate forming
intercellular
clefts (slit pores) between the cells. These pores generally permit
passage of molecules. However, their size varies widely in different
regions e.g. they are much smaller in the brain than in skeletal muscles;
helps the development of a blood brain barrier.
2-Fenestrated capillaries (in the kidneys, intestinal villi and most
endocrine glands):
In this type, the cytoplasm of the endothelial cells itself is interrupted,
forming gaps called fenestrations that are closed by thin membranes
(except in the renal glomeruli) and permit passage of relatively large
molecules.
3-Sinusoidal capillaries (in the liver, spleen and bone marrow): In this
type, the capillaries (which are called sinusoids) have very wide
lumens and are extremely porous because;
Their endothelium is discontinuous.
There are large gaps between the endothelial cells that are not
closed by membranes.
.
Trans-capillary exchange mechanisms:
The transport of fluids across the capillary walls occurs by the following
mechanisms
Diffusion:
This is the process by which a substance in solution expands to fill all of
the available volume. It occurs down a concentration gradient i.e.
substances diffuse from areas of high to areas of low concentration.
Water and water-soluble substances (e.g. glucose, urea, Na
+
, Cl
-
& K
+
)
diffuse only through the slit pores and fenestrae and their rates of
diffusion are inversely proportionate to their molecular sizes. On the
other hand, fat-soluble substances diffuse across the whole capillary wall
i.e. through the pores as well as the cytoplasm of the capillary endothelial
cells (since they dissolve in the phospholipid bilayer of the endothelial
cell membranes), thus the diffusion of fat-soluble substances and gases
(e.g. O
2
and CO
2
) is normally greater and faster than water-soluble
substances.
Filtration:
This is the process by which fluid and dissolved solutes are forced
through the pores in the capillary membrane due to a difference in
hydrostatic pressure on the two sides, and the amount of fluid filtered per
unit time is proportionate to:
(a) The difference in pressure.
(b) The capillary surface area and permeability.

The force of filtration is opposed by the force of osmosis, and both forces
are concerned with the bulk flow of fluids and solutes across the capillary
walls through formation and drainage of the interstitial fluid.
Transcytosis:
This is the mechanism of transport of large molecules across the capillary
membrane. These molecules are transported through the capillaries by
endocytosis into their lining endothelial cells followed by exocytosis at
the interstitial side of these cells. Small amounts of protein leave blood
stream to interstitial fluid by this mechanism.
Diapedesis:
This is the mechanism of transport of a whole cell across the capillary
membrane e.g. leukocytes leave the bloodstream toward areas of
inflammation by this mechanism.
Formation and drainage of the interstitial fluid:
The spaces between the tissue cells are called the interstitium It consists
of thick bundles of collagen fibres and thin filaments formed of
hyaluronic acid and protein, as well as a fluid known as the tissue or
interstitial fluid (IF). The IF is continuously formed and drained by the
capillaries, and it contains almost the same constituents of the plasma
except the plasma proteins.
Factors that affect tissue fluid formation and drainage:
The Starling's forces (the hydrostatic and osmotic forces that act
across the capillary walls)
The capillary permeability.
The Starling's forces:
1-The hydrostatic capillary pressure (hcp):
This forces fluid outwards through the capillary membranes into the
interstitial spaces, and it normally averages 35 mmHg at the arteriolar
ends of capillaries and 12 mmHg at their venular ends.
2-The interstitial fluid pressure (ifp):
This forces fluid inwards through the capillary membranes, and it
normally averages 1 mmHg.
3-The plasma colloid osmotic pressure or oncotic pressure (pop):
This is produced mainly by plasma albumin. It averages 25 mmHg and
it
causes osmosis of fluid inwards through the capillary membranes.
4-The interstitial fluid colloid osmotic pressure (ifop):
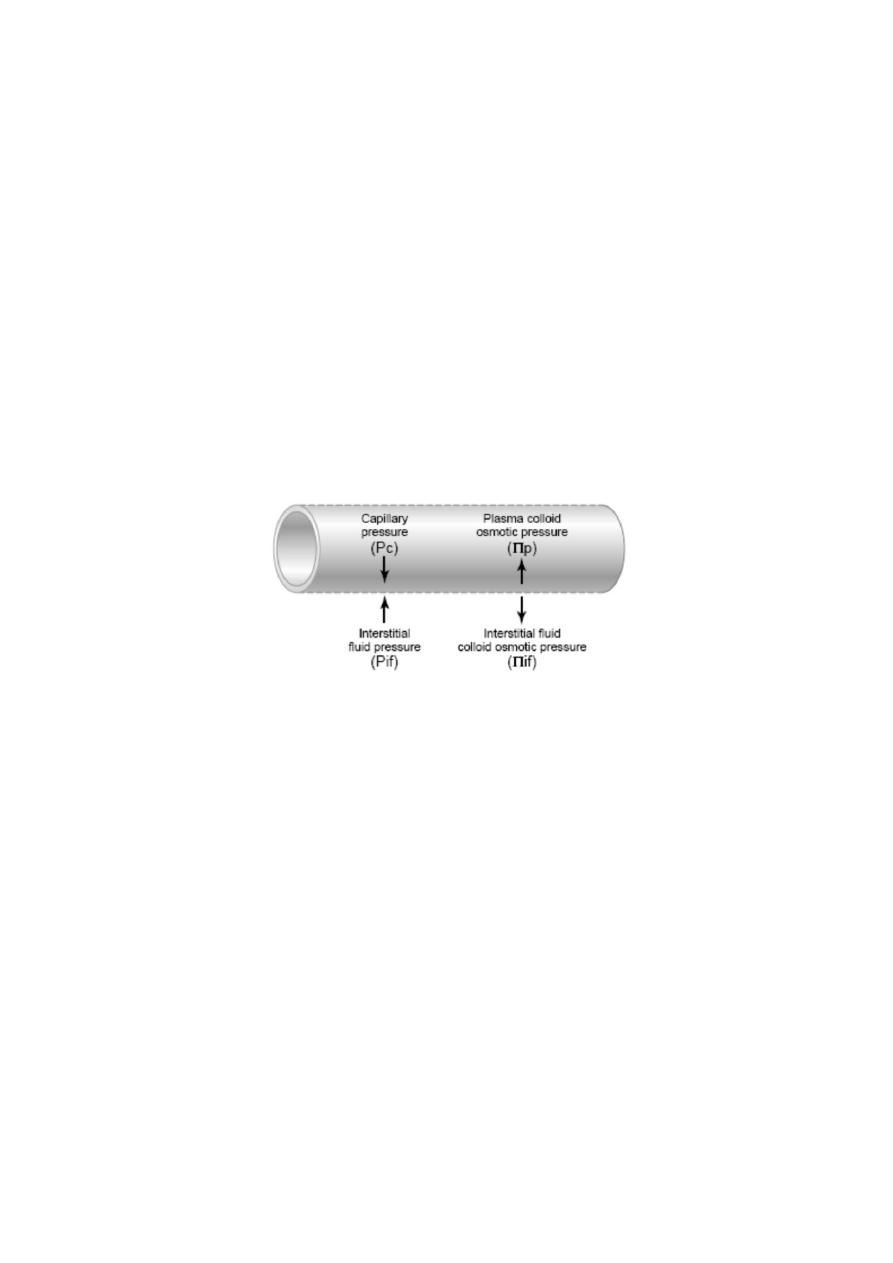
This causes osmosis of fluid outwards through the capillary
membranes into the interstitial spaces, and it normally averages 3
mmHg.
The (hcp) and (ifop) favour fluid filtration from the capillaries while the
(pop) and (ifp) favour fluid reabsorption into the capillaries. Considering
the balance of the Starling's forces at both ends of the capillaries, it is
clear that at their arteriolar ends, the filtering forces exceed the
reabsorbing forces by about 12 mmHg [(35 + 3) - (25 + 1)] resulting in
fluid filtration, while at their venular ends, the reabsorbing forces exceed
the filtering forces by about 11 mmHg [(25 + 1) - (12 + 3)] resulting in
fluid reabsorption.
It was proved that the interstitial fluid pressure (ifp) is negative in certain
areas e.g. the subcutaneous tissues (-2 to -3 mmHg), and in this case, it
favours fluid filtration rather than reabsorption.
Figure: Fluid pressure and colloid osmotic pressure forces operate at the
capillary membrane, tending to move fluid either outward or inward
through the membrane pores.
THE LYMPH CIRCULATION
This circulation is concerned with return of the excess tissue fluid that is
not reabsorbed at the capillaries back to the bloodstream. This fluid is
called lymph, and it is similar to the plasma (being an isotonic colourless
transparent fluid having a pH of 7.4) but it contains less protein and Ca
+2
and has a higher A/G ratio (Albumin/Globulin ratio) since albumin is
more easily filtered. Its average protein content is 3 gm %, but it varies

in different organs and it clots (as it contains fibrinogen and prothrombin)
and is rich in lymphocytes.
Lymph circulates in non-innervated vessels that form a lymphatic system.
This system originates as minute lymphatic capillaries in the tissues
(which are highly-permeable blind vessels lined by a single layer of
endothelial cells) that drain the excess tissue fluid. These capillaries unite
forming larger lymphatic vessels, which drain in the thoracic and right
lymph ducts that open in the subclavian veins at the base of the neck.
The lymph nodes are located along the course of the lymphatic vessels,
and such vessels have smooth muscle in their walls and contain valves
that allow unidirectional flow toward their central end.
EDEMA
This is fluid accumulation in tissues, which is either intra or extra-
cellular.
Intracellular edema:
This is a non-pitting edema that is produced as a result of either:
Depression of the cell membrane metabolic activity e.g. due to
ischemia. In this case, the lack of O
2
and nutrients depress the Na
+
pump
mechanism
and the excess Na
+
inside the cells causes osmosis of water into the
cells.
Inflammation: This increases the cell membrane permeability,
allowing Na
+
and other ions to diffuse into the cells with
subsequent water osmosis.
Extracellular edema:
This is a pitting edema (i.e. pressing the skin by the finger produces a pit)
except in cases of chronic lymphedema. It is due to accumulation of
excessive amounts of interstitial fluid (mostly in the dependent parts of
the body by the effect of gravity), and this has 2 main causes:
1- Excessive leakage of fluid from the capillaries.
This is produced by an increase of fluid filtration or a decrease of fluid
reabsorption at the capillaries or both, which often occur due to either:
An increase of the capillary hydrostatic pressure: This occurs due
to either elevation of the venous pressure (e.g. due to heart failure,
venous obstruction) or arteriolar V.D. (e.g. by vasodilator drugs).
Hypoproteinaemia: This decreases the plasma colloid osmotic
pressure
which reduces tissue fluid reabsorption. It occurs due to either a
decrease
of
synthesis of plasma proteins (e.g. in severe liver disease and
undernutrition)
or excessive loss of plasma proteins (commonly in the urine in

cases
of
the
nephrotic syndrome, or from damaged skin areas in cases of severe
burns).
An increase of capillary permeability: This increases filtration of
both tissue fluid and proteins (the latter farther increases filtration
by increasing the osmotic pressure of the interstitial fluid). It
occurs due to either inflammation, bacterial infections, allergic
reactions (due to release of histamine), prolonged ischemia and
certain toxins, vitamin deficiency (especially vitamin C) and
excessive heat or cold.
Excessive retention of salt in the body: This is an important factor
in the production of renal and cardiac edema.
2- Inadequate lymph drainage.
This occurs due to blockage of the lymph vessels, which leads to
accumulation of both fluid and protein in the tissue spaces (the latter
also increases fluid filtration by increasing the osmotic pressure of the
interstitial fluid). The condition is called lymphedema, and if it
persists, it causes a chronic inflammatory condition that leads to
fibrosis of the interstitial tissue, and the edema becomes non-pitting.
It often occurs in cancer, after certain surgical operations (e.g. radical
mastectomy) and by infection with filaria worms. The latter obstruct
the lymphatics, causing massive swelling of the affected organ
(commonly the legs or scrotum), a condition known as
elephantiasis.
Safety factors against production of edema:
Normally, the following 3 factors prevent occurrence of edema:
(1) Low compliance of the subcutaneous interstitium.
The negative interstitial fluid hydrostatic pressure in subcutaneous
tissues holds these tissues together and makes compliance (their
distensibility) to be low. Accordingly, small increases in tissue fluid
volume cause large increases in hydrostatic pressure of the interstitial
fluid, which opposes further fluid filtration and also increases the
lymph flow; both effects prevent development of edema.
(2) Increasing the lymph flow.
The lymph flow can increase 10 - 50 folds when fluid begins to
accumulate in the tissue spaces. This removes large amounts of the
interstitial fluid and maintains the low compliance state of the
subcutaneous interstitium, and both effects prevent development of
edema.
(3) Washdown of interstitial fluid protein.

The increased lymph flow often results in reduction of the protein
concentration in the interstitial fluid because the amount removed is
usually greater than that filtered by the blood capillaries.
Accordingly, the osmotic pressure of the interstitial fluid is decreased,
which lowers the net filtration force across the capillaries and tends to
prevent further accumulation of fluid.
The efficiency of the 3 edema safety factors is estimated by finding how
much can the average capillary hydrostatic pressure increase above nor-
mal before edema occurs. Normally, it is about 17 mmHg (i.e. the
capillary hydrostatic pressure can raise by 17 mmHg before significant
edema occurs).
>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>
>>>>>>>
