Lect. 13
Regulation (control) of the arterial blood pressure:
Objectives:
1. Draw a "box and arrow" diagram illustrating the arterial
baroreceptor reflex.
2. Describe the changes in blood pressure while going from lying to
standing position.
3. Draw a diagram illustrating the mechanism that control the arterial
BP by adjusting the body fluids and blood volume through
modifying the excretion of water and salt by the kidneys.
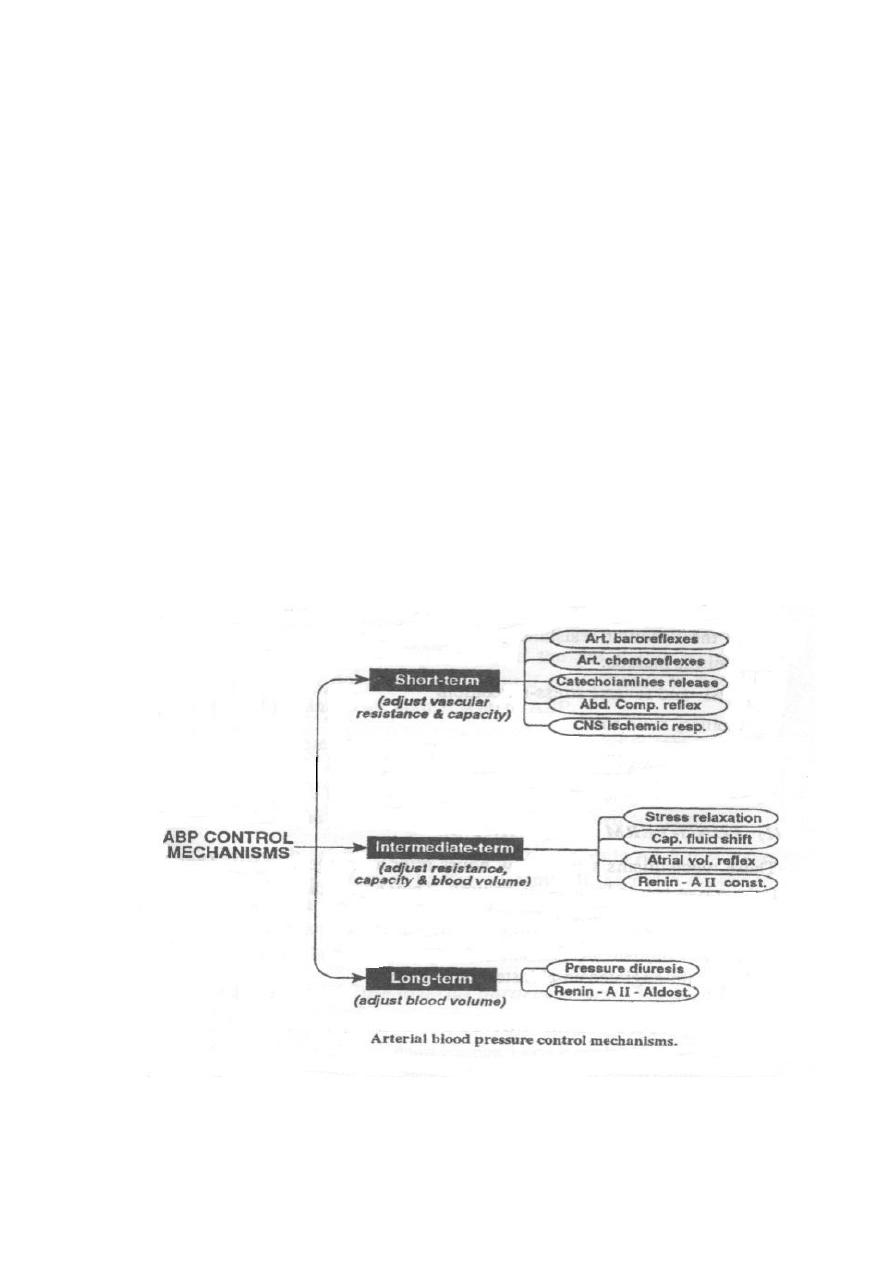
Whenever the arterial BP is altered, the following 3 mechanisms
respectively restore it to the normal level.
Short-term mechanisms.
Intermediate-term mechanisms.
Long-term mechanisms.
Short-term mechanisms
These are potent mechanisms, they act within a few seconds after
alteration of the BP and their action lasts for several hours. They are

mostly nervous reflexes that adjust the vascular capacity and resistance as
well as the cardiac pump.
(1) Arterial baroreceptor reflex:
It is a neural reflex that maintains normal arterial pressure. This reflex
is initiated by stretch receptors, which are located in the carotid sinus
and aortic arch.
Signals from the carotid arteries are transmitted through the
glossopharyngeal nerves while signals from the aortic arch are
transmitted through the vagus nerves into; the medullary
cardiovascular centers. They are stretch receptors that discharge when
the arterial BP increases, in which case they discharge signals leading
to stimulation of the CIC (resulting in reflex bradycardia) and VDC
(resulting in generalized vasodilation) and inhibition of the VCC.
Therefore, an increase in the arterial pressure increased the discharge
rate of the baroreceptors, which reflexly decreases the arterial
pressure because of both a decrease in peripheral resistance
(vasodilation) and a decrease in cardiac output (CO).
In other word, when the arterial pressure decreases e.g. on sudden
standing after prolonged recumbency or in case of hemorrhage, the
discharge rate of the barorecrptors to the medullary cardiovascular
center is decreased. This induces:
Increased heart rate because of increased sympathetic and
decreased parasympathetic activities to the heart.
Increased
ventricular
contractility
because
of
increased
sympathetic activity to the ventricular myocardium.
Vasoconstriction (arteriolar and venous) because of increased
sympathetic activity to the arterioles and veins.
The net result is an increased cardiac output (increased heart rate and
stroke volume), increased total peripheral resistance (arteriolar
constriction), and a return of blood pressure toward normal.
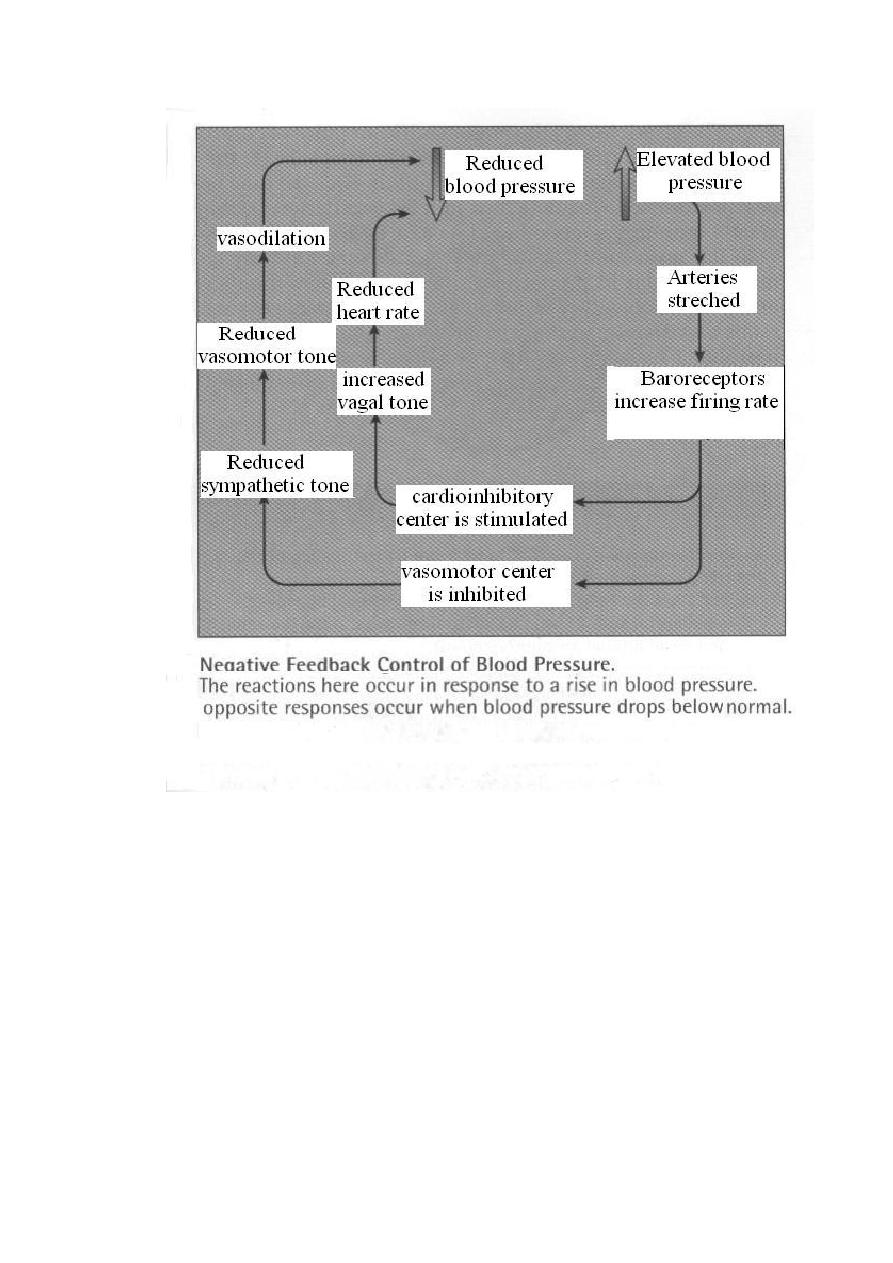
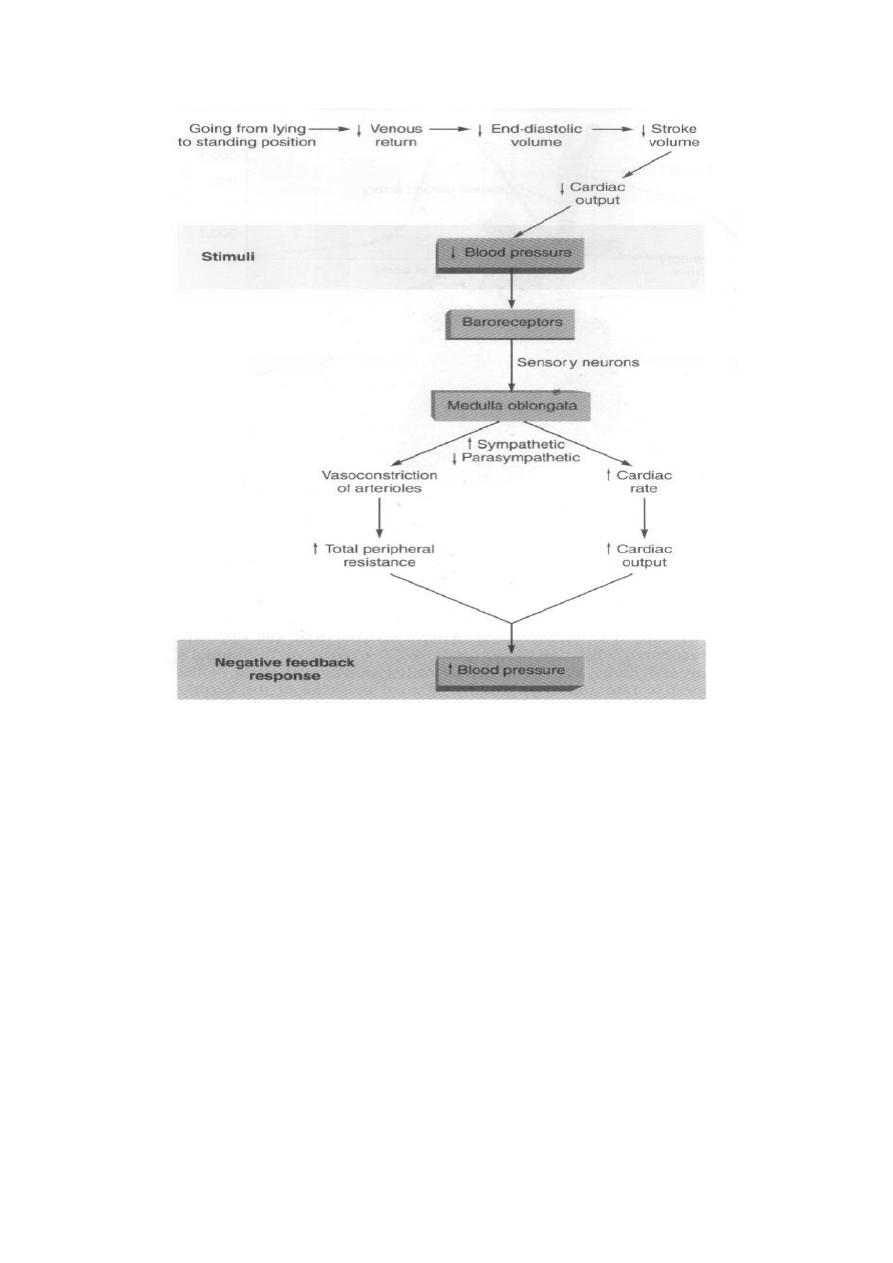
Figure: Baroreceptor reflex that help to maintain an adequate blood
pressure upon standing (- ve feedback control of BP).
(2) Arterial chemoreflexes:
The receptors of these reflexes are located in the carotid and aortic
bodies, and they are stimulated when the arterial BP is reduced below
60 mmHg (mainly as a result of local ischemia and hypoxia), in
which case they discharge signals leading to stimulation of the VCC
and inhibition of the CIC and VDC. This causes elevation of the
arterial BP by increasing:
The cardiac pumping power and CO (by the resulting tachycardia).
The peripheral resistance (by the generalized Vasoconstriction
(VC)).
Catecholamine secretion from the adrenal medullae.
(3) Release of adrenal medullary catecholamines:
Hypotension stimulates the release of adrenaline and noradrenaline
from the adrenal medulla. Adrenaline improves the cardiac pumping
by stimulating the myocardial contractility and rhythmicity. In high

doses, adrenaline produces general vasoconstriction and increase the
peripheral resistance. Noradrenaline is a strong vasoconstrictor. The
two catecholamines act to raise a low blood pressure back toward
normal.
(4) The CNS ischemic response:
In cases of reduction of the arterial BP below 60 mmHg, brain
ischemia occurs. The resulting local hypoxia (and to a little extent
also hypercapnia and acidosis) stimulate the VCC, resulting in
generalized VC which elevates the arterial BP and maintains the
cerebral blood flow.
(5) The abdominal compression reflex:
Whenever the VCC is stimulated the medullary reticular formation is
simultaneously excited and sends signals in the somatic nerves to
skeletal muscles, specially the abdominal muscles, leading to an
increase of their tone. This is an important mechanism to raise the
arterial BP since it increases the intraabdominal pressure, which
compresses the abdominal veins resulting in an increase of the venous
return and consequently, the CO (which helps elevation of the arterial
BP).
Intermediate-term mechanisms
These mechanisms control the arterial BP by adjusting the vascular
capacity and resistance as well as the blood volume. They act within a
few minutes after alteration of the BP and their action lasts for several
days. During this time, the nervous, rapid short-term mechanisms usually
fatigue and become less effective. They include the following:
(1) Capillary fluid shift mechanism:
This mechanism occurs especially when the arterial BP is altered as a
result of changes in the blood volume. An increase in the blood
volume increases the capillary hydrostatic pressure, and this helps
fluid filtration into the tissue spaces, thus the blood volume is
decreased leading to reduction of the arterial BP toward the normal
level.
(2) Stress relaxation mechanism:
A rise of the arterial BP stretches the arteries and increases the
tension in their walls. However, after sometime (varying from a few
minutes to a few hours) the arteries relax and the tension in their walls
decreases. This is called stress relaxation of the arteries, and it helps
lowering of the arterial BP.
(3) Renin-angiotensin vasoconstriction mechanism:
A fall of the arterial BP leads to renal ischemia. This stimulates
secretion of a hormone called renin from the juxtaglomerular cells of
the kidney, which acts on a plasma ά
2
globulin called angiotensinogen
(a polypeptide synthesized by the liver) forming angiotensin I. An

enzyme called ACE (angiotensin-converting enzyme) converts
angiotensin 1 into angiotensin II (especially in the lungs), which has
a potent vasoconstrictor effect that helps elevation of the arterial BP
(4) Right atrial mechanism:
This occurs especially when the arterial BP is altered as a result of
changes in the blood volume. An increase in the blood volume
stimulates the volume receptors in the right atrium resulting in the
following effects:
Generalized VD (which decreases the peripheral resistance and
increases
the venous capacity) including VD of the afferent renal arterioles
(which
increases the glomerular filtration, leading to more water and salt
excretion).
Reflex inhibition of secretion of the antidiuretic hormone (ADH).
This
helps
water excretion by the kidney.
The secretion of ANP (atrial natriuretic peptide), this also helps salt
and water excretion by the kidney. All these effects help lowering
of the arterial BP, and opposite effects (elevation of BP) occur
when the blood volume is decreased.
Long-term mechanisms
These mechanisms control the arterial BP by adjusting the body fluids
and blood volume through modifying the excretion of water and salt by
the kidneys. This occurs by variations in: (a) Glomerular filtration. (b)
Secretion of the aldosterone hormone.
A fall of the arterial BP reduces glomerular filtration, so the renal
excretion of water and salt is decreased. At the same time, renin is
secreted and angiotensin II is formed, which in addition to producing VC,
it also stimulates aldosterone secretion from the adrenal cortex, which
increases Na
+
reabsorption in the renal tubules. These effects increase the
body fluids and blood volume, which elevates the arterial BP to the
normal level. On the other hand, a rise of the arterial BP increases
glomerular filtration, producing pressure diuresis which leads to
excessive loss of water and salt in the urine. At the same time, renin
secretion is inhibited and angiotensin II is not formed, thus aldosterone
secretion is inhibited, leading to loss of Na
+
and water in the urine. These
effects reduce the arterial BP to the normal level.
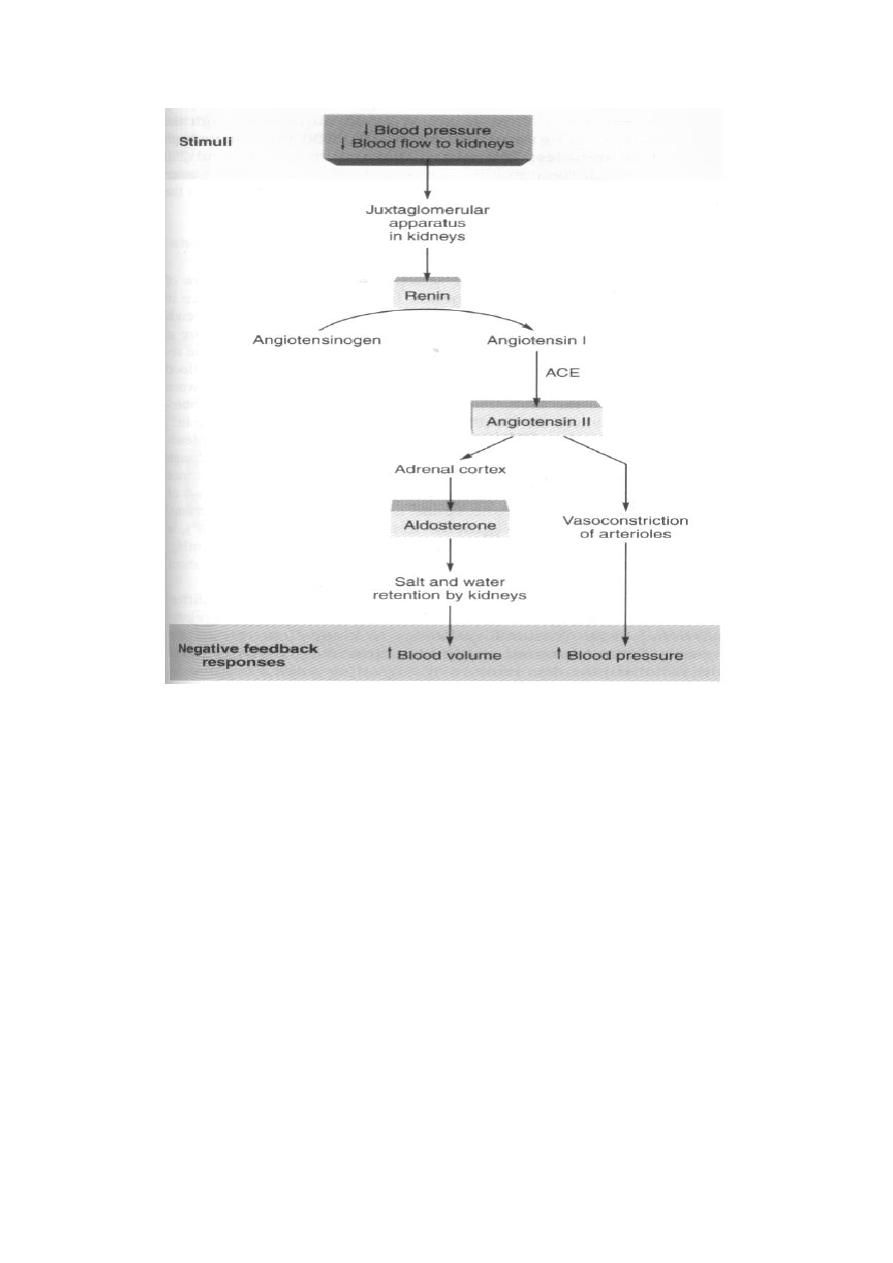
Figure: The renin-angiotensin-aldosterone system.
Importance of Salt (NaCl) in the Arterial blood Pressure Regulation:
An increase in salt intake is more likely to elevate the arterial pressure
than is an increase in water intake. The reason for this is that pure water is
normally excreted by the kidneys almost as rapidly as it is ingested, but
salt is not excreted so easily. When the salt accumulates in the body, it
increases the extracellular fluid volume for two basic reasons:
1. When there is excess salt in the extracellular fluid, the osmolality of
the fluid increases, and this in turn stimulates the thirst center in the
brain, making the person drink extra amounts of water to return the
extracellular salt concentration to normal. This increases the
extracellular fluid volume.
2. The increase in osmolality caused by the excess salt in the extracellular
fluid also stimulates the hypothalamic-posterior pituitary gland
secretory mechanism to secrete increased quantities of antidiuretic
hormone (ADH). ADH then causes the kidneys to reabsorb greatly
increased quantities of water from the renal tubular fluid, thereby
diminishing the excreted volume of urine but increasing the
extracellular fluid volume. Thus, for these important reasons, the

amount of salt that accumulates in the body is the main determinant of
the extracellular fluid volume. Because only small increases in
extracellular fluid and blood volume can often increase the arterial
pressure greatly, accumulation of even a small amount of extra salt in
the body can lead to considerable elevation of arterial pressure.
>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>
>>>>>>>
