
Lect. 12
Arterial blood pressure
Objectives:
1. Define the terms systemic arterial pressure, systolic pressure,
diastolic pressure, pulse pressure, and mean arterial pressure.
2. Describe the principles and application of sphygmomanometry for
the measurement of systemic arterial pressure.
3. State the influence of decreased aortic distensibility, increase in
heart rate, and increase or decrease in peripheral resistance on
systolic and diastolic systemic arterial pressures.
Arterial blood pressure is the pressure exerted by the blood on the arterial
walls (BP). It normally fluctuates during the cardiac cycle between a
maximum called the systolic blood pressure (SBP) and a minimum
called the diastolic blood pressure (DBP).
The systolic BP normally averages 120 mmHg in young adult males
(range 90 -140 mmHg), and is produced by ejection of blood into the
aorta during left ventricular systole (>140 represents systolic
hypertension). The diastolic BP normally averages 80 mmHg (range 60 -
90 mmHg), and is produced as a result of the elastic recoil of the aorta
during ventricular diastole (> 90 mmHg represents diastolic
hypertension).
The arterial blood pressure (ABP) is often reported as the systolic over
the diastolic pressure (e.g. 120/80). BP value less than normal lower limit
called hypotension (e.g. SBP < 90 mmHg).
Pulse pressure: The difference between both the systolic and diastolic
BP and it normally averages 40 mmHg.
Pulse pressure = systolic BP – diastolic BP =120 – 80 = 40 mmHg.
The mean arterial blood pressure:
Mean BP = Diastolic BP + 1/3 pulse pressure = 80 + 13 = 93 mmHg.
Importance (function) of the arterial blood pressure:
1- It maintains tissue perfusion (i.e. blood flow) throughout various
tissues, including those lying above the heart level (in spite of the
force of gravity).
2- It produces the capillary hydrostatic pressure, which is the main
force concerned with tissue fluid formation (interstitial fluid).
The diastolic blood pressure performs the following functions:
a- It maintains blood flow to the tissues during ventricular diastole
(thus the blood flow to the tissues becomes continuous, not

intermittent).
b- It is essential for the normal coronary blood flow.
c- It prevents blood stasis in the arteries during ventricular diastole.
Measurement of the arterial blood pressure:
This is performed by the sphygmomanometer apparatus, which consists
of an inflatable rubber cuff connected to a mercury manometer. The cuff
can be air inflated by a small hand pump (bulb), and deflated by opening
the attached air-control valve. This apparatus can measure the arterial BP
by 2 methods:
1-Palpatory method
This is an inaccurate method that measures the systolic pressure only.
The cuff is wrapped around the arm so that it surrounds the brachial
artery. The radial pulse is then palpated by the middle 3 fingers of one
hand, and then the cuff is inflated by the other hand till the pulse
disappears (indicating complete obstruction of the brachial artery). The
cuff is then slowly deflated by opening the air-control valve while the
radial pulse is still palpated, till it first becomes palpable. At this
moment, the level of the column of mercury represents the systolic
blood pressure which is equal to the cuff pressure. Diastolic BP can not
measured by this method.
2-Auscultatory method
This is an accurate method that measures both the systolic and diastolic
blood pressures. The cuff is wrapped around the arm and the
stethoscope is placed just below it on the brachial artery at the medial
side of the biceps tendon in the anticubital fossa. The cuff is inflated;
elevating the column of mercury to a level higher (20-30 mmHg), till
the radial pulse become impalpable indicating obstruction of the
brachial artery, and then it is slowly deflated. As the cuff pressure falls,
certain sounds called korotkow's (Korotkoff's) sounds are heard along
with the heart beats. These sounds are produced as a result of turbulent
blood flow in the brachial artery and their quality changes in 5 steps:
1- When the cuff pressure becomes just below the systolic pressure, a
spurt of blood passes through the narrowed brachial artery producing
intermittent turbulence; heard as tapping sounds (1
st
korotkow's
sound). The height of mercury column when the first sound is heard
represents the arterial systolic blood pressure.
2- As the cuff pressure is lowered, the sounds become murmur-like.
3- With further lowering of the cuff pressure, the sounds become louder.
4- When the cuff pressure approaches the diastolic pressure, the turbulent
flow becomes continuous (because the vessel is still constricted), and
the sounds become dull and muffled (4
th
korotkow's sound). The
height of mercury column when the muffled sound is heard represents
the arterial diastolic blood pressure.

5- When the cuff pressure becomes lower than the diastolic pressure, the
sounds disappear because the blood flow becomes continuous but not
turbulent (silent, laminar flow; 5
th
korotkow's sound).
The systolic pressures obtained by the palpatory method are usually 2-5
mmHg lower than those measured by the auscultatory method because:
The finger's sensitivity cannot determine exactly when the first beat
is felt.
As the blood travels the distance from the cuff to the wrist, the cuff
pressure is further decreased, thus recording a lower systolic
pressure.
The silent gap:
During measuring the arterial BP by the auscultatory method, sometimes
(especially in hypertension) the korotkow's sounds disappear (after 2
nd
korotkow's sound) for a variable gap at pressures well above the
diastolic pressure then reappear again (3
rd
korotkow's sound). This
occurs due to unknown causes and may lead to recording of false low
systolic pressure values (3
rd
korotkow's sound) if the sounds above the
gap are missed and only those below the gap are heard. However, this is
avoided by:
(a) Palpating the radial pulse while inflating the cuff till it disappears (in
this case, the cuff pressure is certainly above the systolic pressure)
(b) Determining the systolic pressure first by the palpatory method, then
raising the cuff pressure above the recorded value.
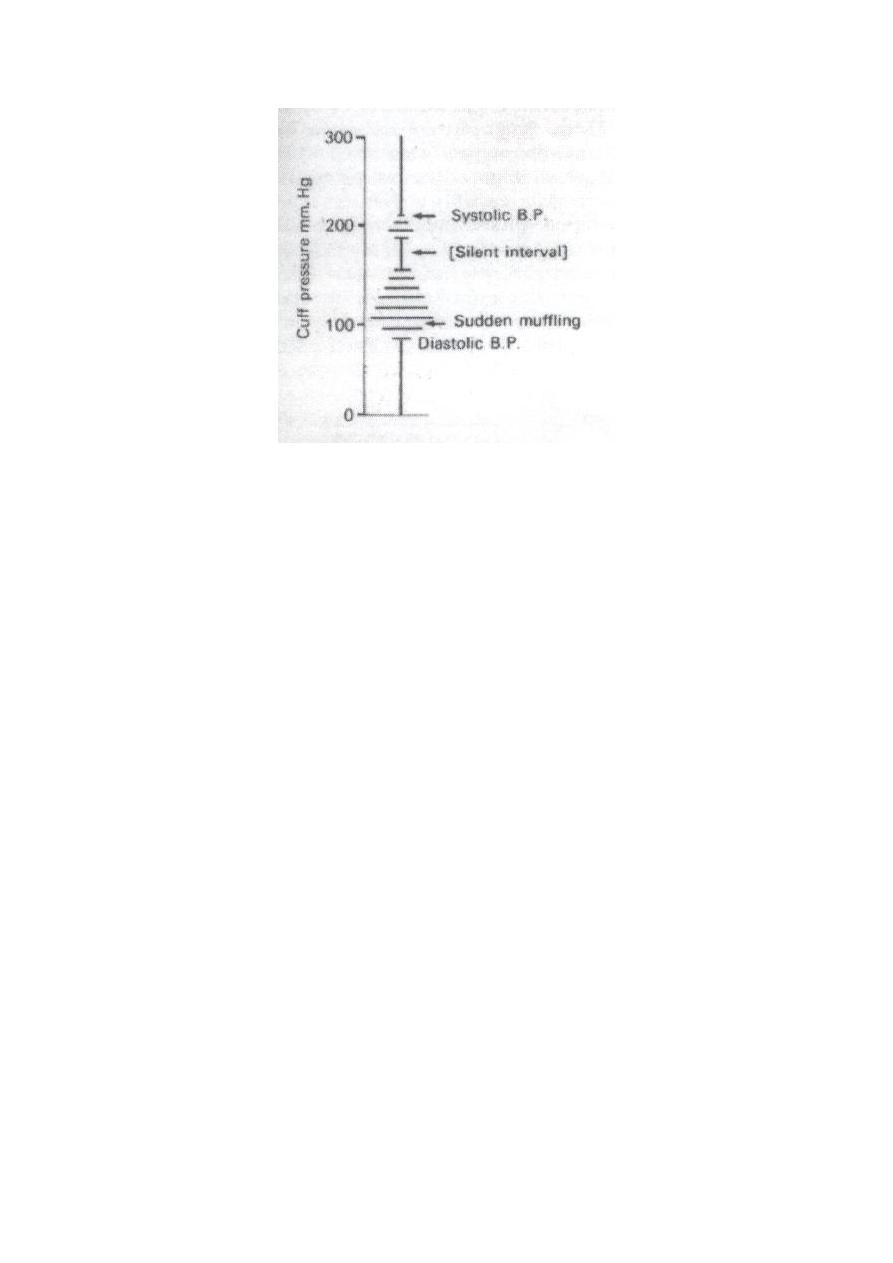
Figure: Silent interval in severe hypertension, it is not normally present.
Physiological factors that affect the arterial blood pressure:
Age: The arterial BP is very low at birth (about 70-80/40-50
mmHg) then it rises progressively till about 120/80 mmHg at the
age of 20 years. Its rise continues gradually after that age, but its
rate increases markedly after the age of 40 years due to the normal
gradual loss of arterial elasticity, so that it becomes normally about
I50/90 mmHg after the age of 60years.
Sex: The arterial BP is generally slightly higher in adult males than
in females. However, it becomes slightly higher in females after the
menopause.
Body region: The arterial BP is normally higher in the lower limbs
than in the upper limbs.
Body built: The arterial BP is usually high in obese persons.
Race: The arterial BP is often high in western countries (probably
due to genetic factors, but stress, environmental or dietary factors
may contribute).
Diurnal variation: The arterial BP is normally lowest in the early
morning and highest in the afternoon.
Meals: The arterial BP increases slightly after meals (especially the
systolic) due to vasodilatation (VD) in the splanchnic area, which
increases both the venous return (VR) and cardiac output (CO).
Exercise: The arterial BP markedly increases during exercise,
especially the systolic (the diastolic pressure is often not changed or

even decreases).
Emotions: The arterial BP increases considerably in most emotions
especially the systolic (due to increased sympathetic stimulation).
Intercourse: The systolic BP often increases during intercourse.
Sleep: The arterial BP is often slightly decreased during quiet sleep
(due to decrease of the sympathetic activity) but it may increase
during nightmares.
Environmental temperature: In hot environments, the systolic
pressure may increase slightly due to tachycardia, but the diastolic
pressure often fells due to cutaneous VD. On the other hand,
exposure to cold increases both the systolic and diastolic pressures
due to cutaneous vasoconstriction (VC).
Gravity: On standing, the force of gravity increases the mean
arterial pressure and the venous pressure below a reference point in
the heart (in the right atriurn) and decreases them above that point
by about 0.77 mmHg.
Respiration: The arterial BP shows rhythmic fluctuations during the
respiratory cycle. It is decreased during inspiration (although the
systemic VR and right ventricular CO are increased) because the
lung vascular capacity is increased and accommodates most of the
right ventricular CO, so the pulmonary VR is decreased resulting in
reduction of both the left ventricular CO and the arterial BP. It is
then increased during expiration due to squeeze of the pulmonary
vascular bed (which increases the pulmonary VR and left
ventricular CO).
Factors that determine and maintain the blood pressure:
1- Cardiac output (CO).
2- Total peripheral resistance (PR).
3- Elasticity of the aorta and large arteries.
4- Blood volume and circulatory capacity.
The cardiac output and the total peripheral resistance are the most
important factors affecting blood pressure. In other words, the blood
pressure is determined by the cardiac output multiplied by the peripheral
resistance.
BP = CO X PR

1-Cardiac output:
The arterial BP is directly proportionate to the CO, which equals the
product of the stroke volume (SV) multiplied by the heart rate (HR).
CO = SV X HR
A- Effect of changes in the stroke volume on the blood pressure:
With a constant HR, an increase in the SV raises systolic pressure with
no significant change in diastolic pressure. The opposite occurs when
the SV is decreased.
B- Effect of changes in the heart rate on the blood pressure:
With a constant venous return, an increase in the HR raises mainly the
diastolic pressure with no significant change in the systolic pressure.
The rise of the diastolic pressure is due to shortening of the diastolic
periods (which leads to blood accumulation in the arteries, thus
preventing fall of the diastolic pressure to the normal level). On the
other hand, the constant systolic pressure is due to the decreased
ventricular filling which decreases the SV. The opposite occurs when
the HR is decreased.
2- Total peripheral resistance:
It is the sum of all the vascular resistances within the systemic
circulation.
The PR is essential for maintenance of the arterial B.P. particularly the
diastolic pressure. It is produced mainly in the arterioles and is
determined by 3 factors:
(a) The radius (or diameter) of the vessel.
(b) Blood viscosity.
(c) The length of the vessel.
Normally the total peripheral resistance can only be determined by the
arteriolar diameter, because the other 2 factors are normally kept
constant.
3- Elasticity of the aorta and large arteries:
Part of the pumping energy of the heart is expended in distension of the
aorta & large arteries. This energy is released during cardiac diastole
causing elastic recoil of the walls of these vessels. Such effect is essential
for production and maintenance of a relatively high diastolic BP. In
addition to maintenance of a high diastolic pressure, the elasticity of the

aorta and large arteries also prevent excessive rise of the systolic BP. This
is clear when there is rise in the systolic pressure in severe arteriosclerosis
in which the elasticity of the aorta and large arteries is lost and the blood
flow to the tissues becomes rather intermittent i.e. mainly during systole.
4- Blood volume and circulatory capacity:
These parameters are major factors in maintenance of the arterial BP
especially the systolic BP as follows: When the blood volume increases
(e.g. in diseases associated with excessive salt and water retention), the
venous return is also increased leading to an increase of both the EDV
and SV, thus the systolic pressure rises. Conversely, when the blood
volume decreases (e.g. after a severe haemorrhage), the venous return,
EDV and SV are also decreased, thus the systolic BP falls.
>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>
>>>>>>>>
