
Physiology of
The Blood
hemostasis
By prof. Israa f. jaafar

Learning objectives
•
Understand the Platelet structure and function
•
Explane the Platelet production
•
Understand the phases of hemostasis:
–
vascular
–
platelet
–
Coagulation (clotting and anticlotting mechanism)

Platelets
•
Cell fragments involved in clotting system
•
Formed from megakaryocyte.
•
Circulates for 9–12 days
•
Are removed by spleen
•
2/3 are reserved for emergencies

KEY CONCEPT-Platelets
•
Platelets are involved in coordination of
hemostasis (blood clotting)
•
Platelets, activated by abnormal changes in
local environment, release clotting factors
and other chemicals
•
Hemostasis is a complex cascade that builds
a fibrous patch that can be remodeled and
removed as the damaged area is repaired

Platelet Counts
•
150,000 to 500,000 per microliter
•
Thrombocytopenia
:
–
abnormally low platelet count
•
Thrombocytosis
:
–
abnormally high platelet count
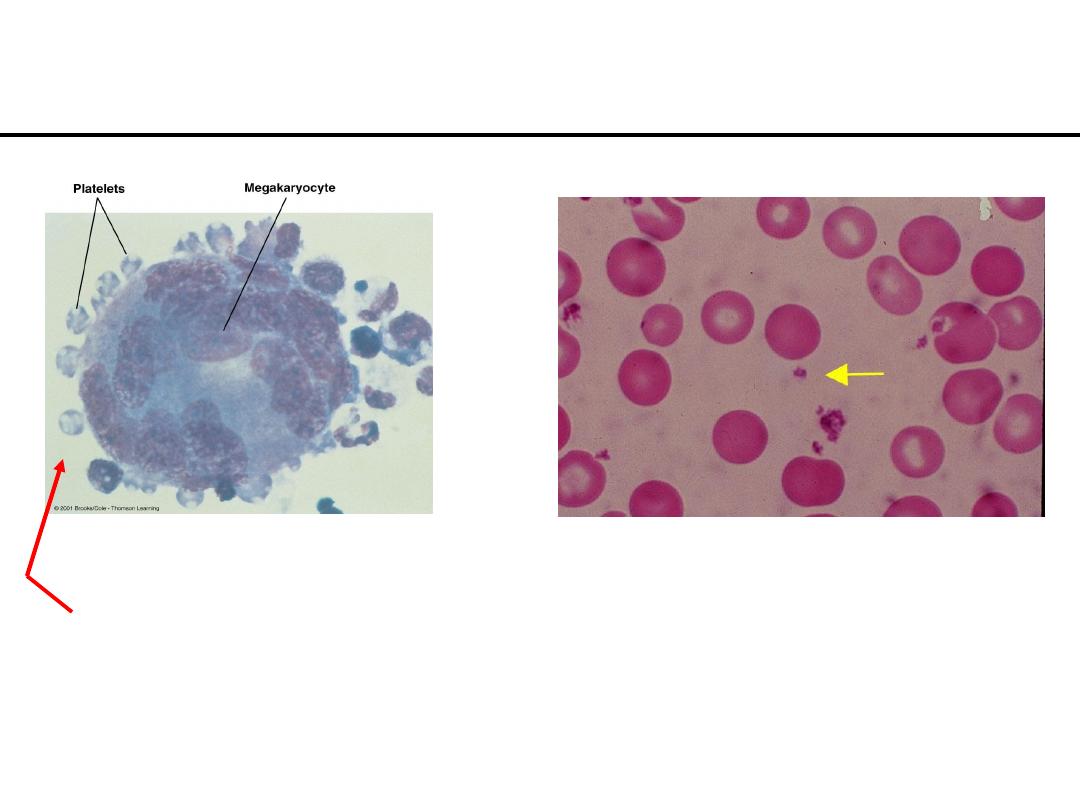
Platelets (Thrombocytes)
* Cell fragments bound to megakaryocytes
* “Bud Off” and are released into the blood
Function of Platelets
.1
Release important clotting chemicals
.2
Temporarily patch damaged vessel walls
.3
Actively contract tissue after clot formation
Platelet production- called
thrombocytopoiesis
:it occurs in bone marrow
•
Stop bleeding from a damaged vessel
Hemostasis
•
Hemostasis
involved in
Three Steps
1. Vascular Spasm
2. Formation of a platelet plug
3. Blood coagulation (clotting)
Steps in Hemostasis
•
Immediate constriction of blood vessel
•
Vessel walls pressed together – become
“sticky”/adherent to each other
•
Minimize blood loss
*DAMAGE TO BLOOD VESSEL
LEADS TO:
1. Vascular Spasm:
Steps in Hemostasis
a. PLATELETS attach to exposed collagen
b.
Aggregation of platelets causes release of
chemical mediators (ADP, Thromboxane A
2
)
c.
ADP attracts more platelets
d.
Thromboxane A
2
(powerful vasoconstrictor)
* promotes aggregation & more ADP
2. Platelet Plug formation: (figure 11-10)
Leads to formation of platelet plug !
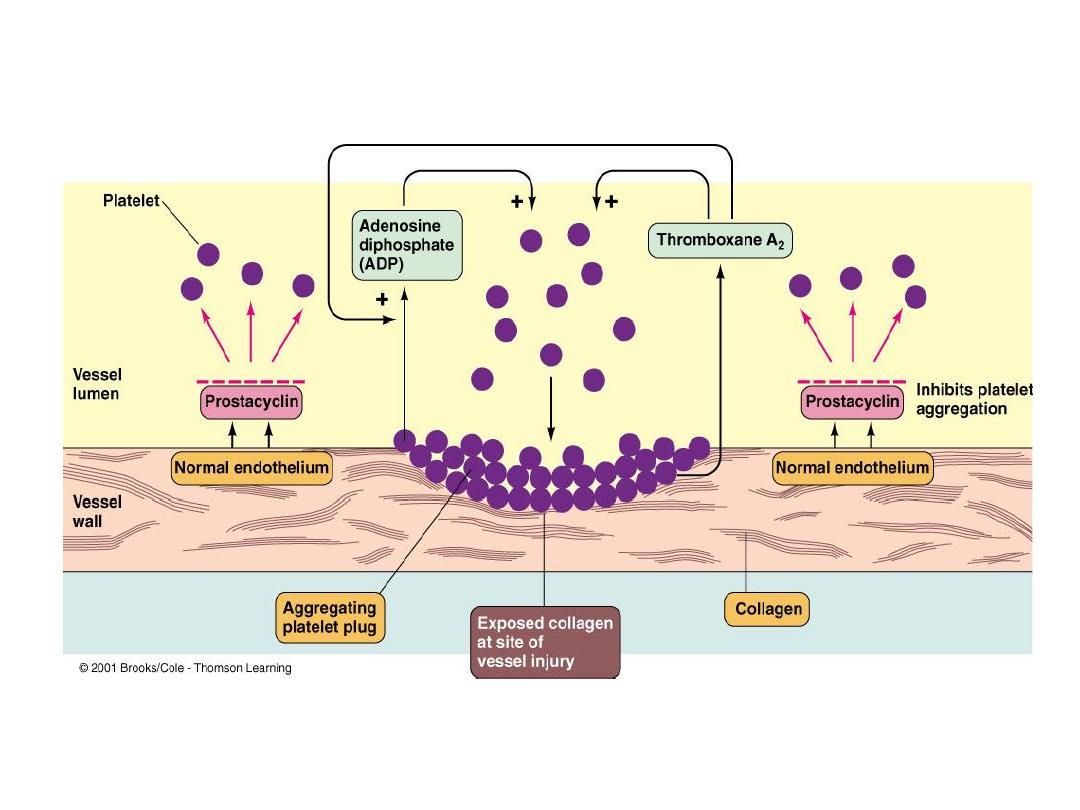
Figure 11-10
(+)
Feedback promotes formation of platelet Plug !
Final Step in Hemostasis
.a
Transformation of blood from liquid to solid
.b
Clot reinforces the plug
.c
Multiple cascade steps in clot formation
.d
Fibrinogen (plasma protein)
Fibri
n
Thrombin
3. Blood Coagulation (clot formation):
“Clotting Cascade”
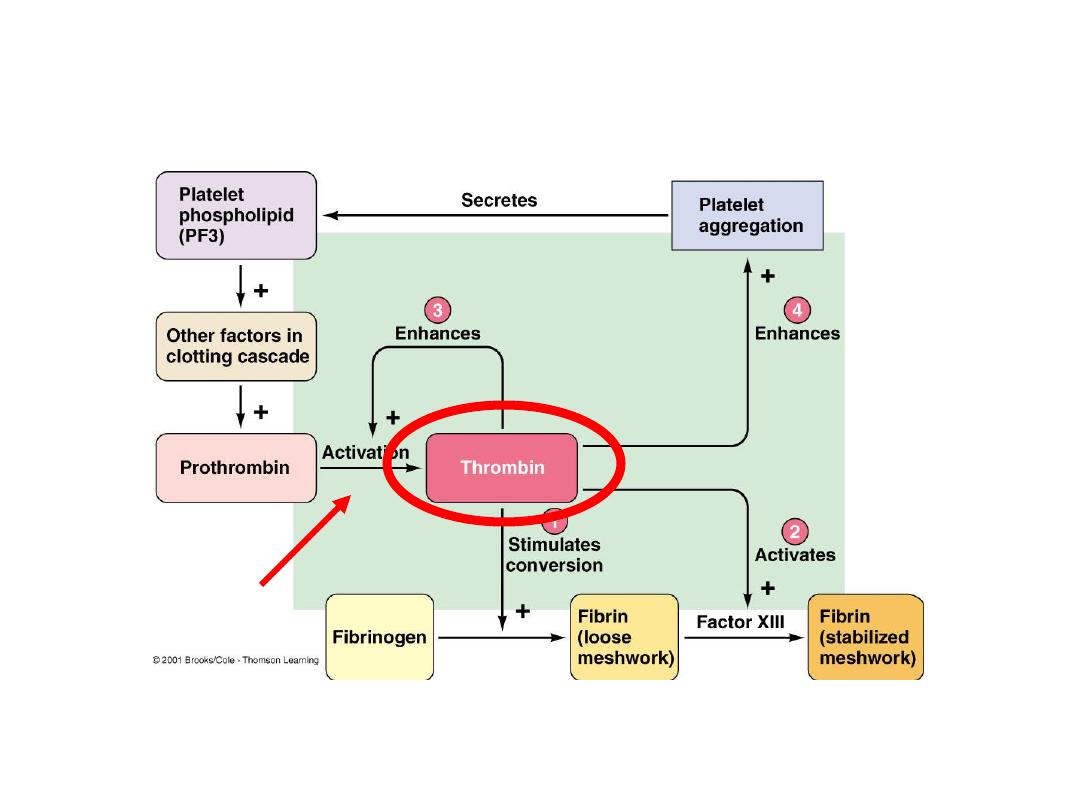
Figure 11-11
Thrombin in Hemostasis
Factor X

Clotting Cascade
•
Participation of 12 different clotting factors
(plasma glycoproteins)
•
Factors are designated by a roman numeral
•
Cascade of proteolytic reactions
•
Intrinsic pathway
/ Extrinsic pathway
•
Common Pathway
leading to the formation
of a
fibrin clot !
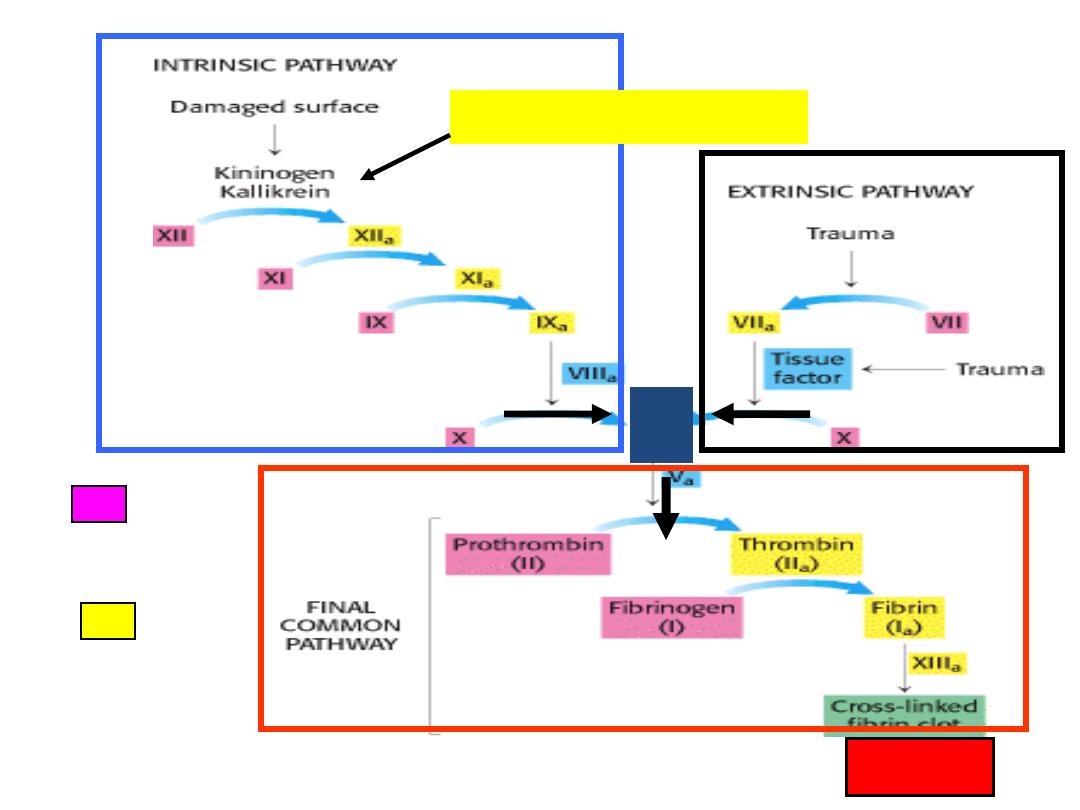
inactive
active
Hageman factor (XII)
CLOT
!
X
Clotting Cascade
•
Intrinsic Pathway
:
–
Stops bleeding within
(internal)
a cut vessel
–
Foreign Substance (ie: in contact with test
tube)
–
Factor XII (Hageman Factor)
•
Extrinsic pathway:
–
Clots blood that has escaped into tissues
–
Requires tissue factors external to blood
–
Factor III (Tissue Thromboplastin)
Clotting Cascade
•
Fibrin :
–
Threadlike molecule-forms the meshwork of the clot
–
Entraps cellular elements of the blood forms CLOT
–
Contraction of platelets pulls the damaged vessel
close together:
•
Fluid squeezes out as the clot contracts
(Serum)

Functions of Thrombin
•
Stimulates formation of tissue factor
–
stimulates release of PF-3:
–
forms positive feedback loop (intrinsic and
extrinsic):
•
accelerates clotting
Bleeding Time
•
Normally, a small puncture wound stops
bleeding in 1–4 minutes

Other Factors
•
Calcium ions
(Ca
2+
) and
vitamin K
are both
essential to the clotting process
Clot dissolution
•
Clot is slowly dissolved by the “fibrin splitting”
enzyme called
Plasmin
•
that is
cursor
-
inactive pre
is the
Plasminogen
activated by Factor XII (Hageman Factor)
(simultaneous to clot formation)
•
Plasmin gets trapped in clot and slowly dissolves
it by breaking down the fibrin meshwork

Clotting: Area Restriction
.1
Anticoagulants
(plasma proteins):
–
antithrombin-III
–
alpha-2-macroglobulin
.2
Heparin
.3
Protein C
(activated by
thrombomodulin
)
.4
Prostacyclin

Clot formation:
Too much or too little
•
Too much:
–
Inappropriate clot formation is a thrombus (free-
floating clots are emboli)
–
An enlarging thrombus narrows and can occlude
vessels
•
Too little:
–
Hemophilia- too little clotting- can lead to life-
threatening hemorrhage (caused from lack of one of
the clotting factors)
–
Thrombocyte deficiency (low platelets) can also lead to
diffuse hemorrhages
