1
NERVOUS SYSTEM Dr.Firdous
It is the most complex systems in the body histologically and physiologically and is
formed by a network of many billion nerve cells, where it provides rapid communications
between different areas of the body through the neurons and nerve fibers.
Nerve tissue is distributed throughout the body.
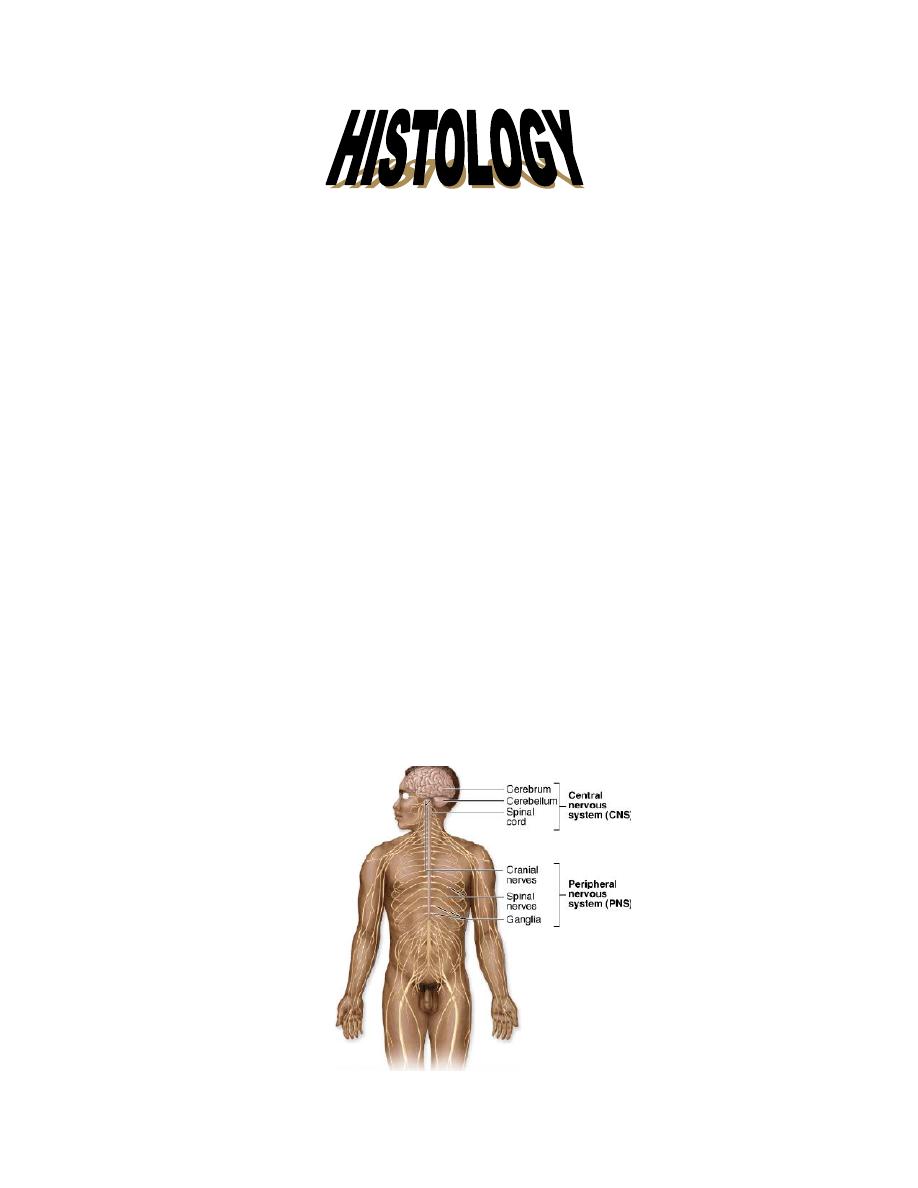
Anatomically, the N.S. is divided into:
1- Central N.S.(C.N.S.), includes : brain, and spinal cord.
2- Peripheral N.S. (P.N.S.), includes: nerve fibers, and ganglia.
Neurons are the anatomical and functional unit of the N.S. their functions are:
1- Gather information from sensory receptors.
2- Process information and provide memory.
3- Generate appropriate signal to the effector cells.
4- Release of neurotransmitters.
By creating, analyzing, identifying, and integrating information, the nervous system
generates two great classes:
Intrinsic conditions (eg; blood pressure, O 2 and CO 2 content, pH, blood glucose
levels, and hormone levels)
Behavioral patterns (eg; feeding, reproduction, defense, interaction with other living
creatures).

2
Neurons are variable in size, ranging from 4-5 µm in diameter(granule cells of the
cerebellar cortex), up to 150 µm in diameter (pseudounipolar neuron).
They also have variable shapes :
a- Multipolar neurons: star shaped , with single axon and multiple dendrites. They are
usually large and of the motor type.
b- Bipolar neurons: generally small in size, with single dendrite. They are of the
interneuron type, providing local communications among other neurons within the
C.N.S., as in the retina, olfactory mucosa, and ganglia.
c- Pseudounipolar neurons: They have single process that form a T shape; one branch
act as dendrite, and the other as an axon. Stimuli will travel directly without passing
through the cell body. These cells are of the sensory type as in the cerebrospinal
ganglia.
NEURON
Nerve cells, or neurons, are responsible for the reception, transmission, and
processing of stimuli; and the release of neurotransmitters and other informational
molecules.
Each neuron consists of three main structures:
І- Perikarion (cell body): it represents the trophic center for the whole nerve cell, and
act also as a receptive area for stimuli. It contains the following organells:
3
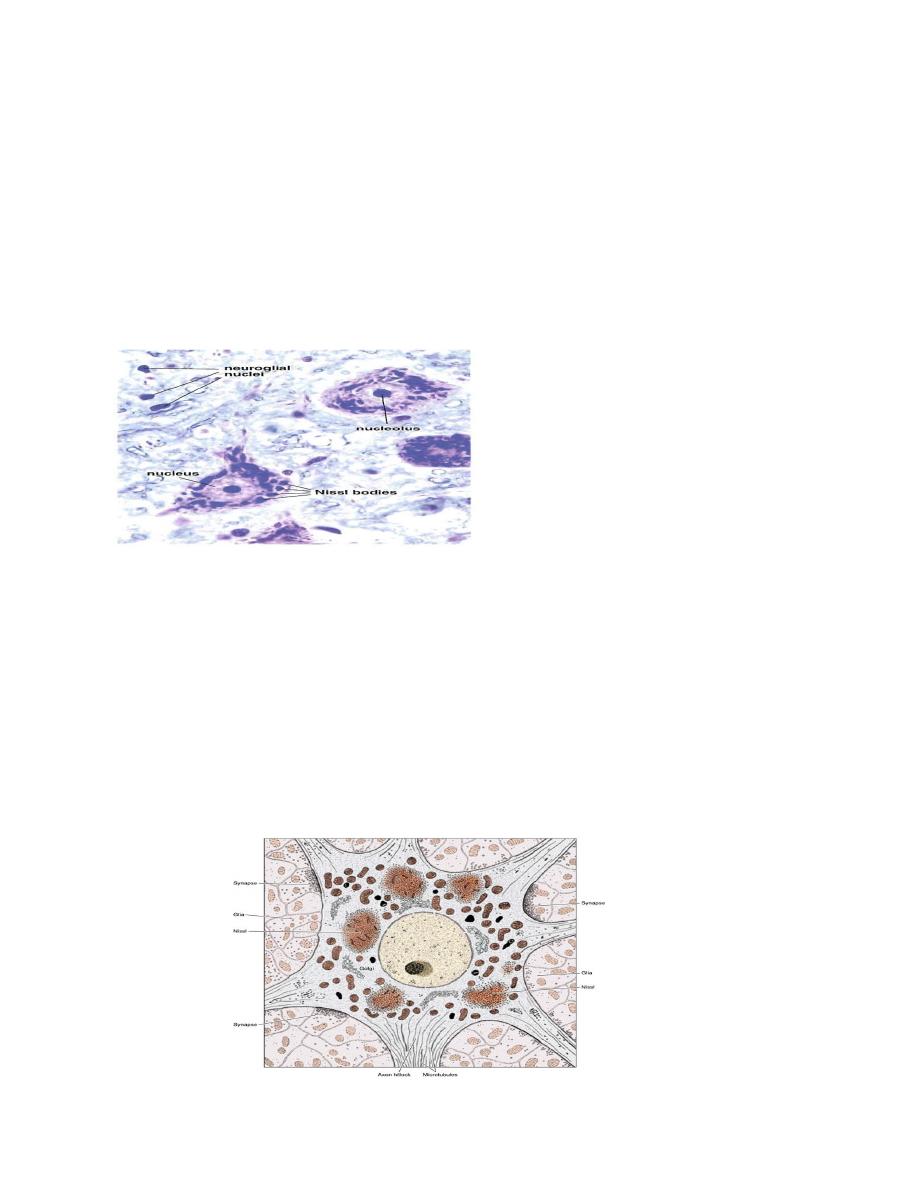
1- Nucleus: usually it is large, spherical, euchromatic(pale staining), with prominent
nucleolus. It is usually centrally located, except in the nerve cell of Clark
,
s column of
spinal cord, and the neuron of sympathetic ganglia, where it is eccentric. The
chromatin is dispersed.
2- 2- Rough endoplasmic reticulum(RER): It is well developed, organized in parallel
cisternae with numerous polyribosomes in between. They synthesize protein. When
the neuron is stained by basophilic stain, RER and free ribosomes will appear as
basophilic granules known as Nissl bodies. They present more in motor neurons, and
absent in axon hillock .
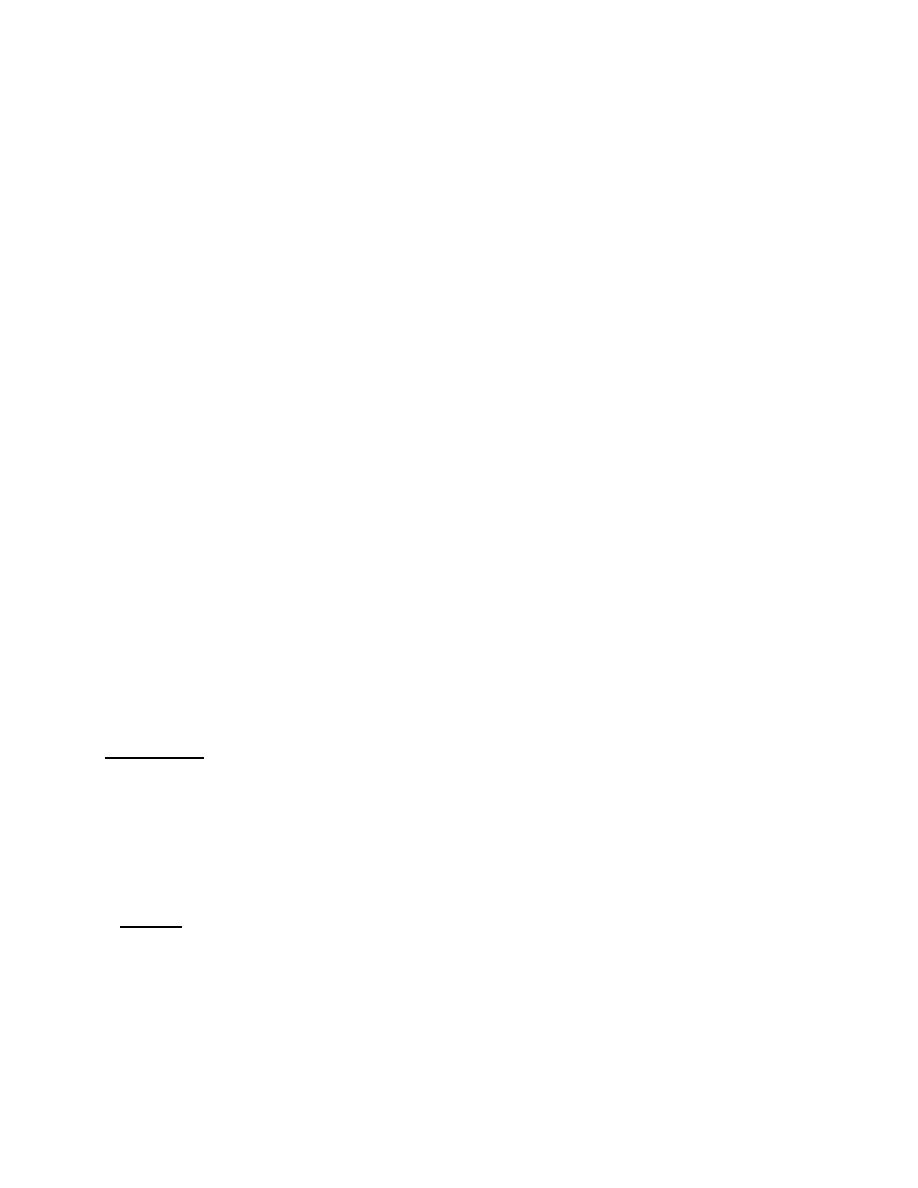
3- Golgi complex: consists of parallel multiple smooth cisternae around the nucleus.
4- Mitochondria: scattered throughout the cytoplasm, and increase in number at the
axon terminal. They supply energy.
5- Lysosomes: present in large number.
6- Neurofillaments: abundant in both cell body and processes, usually of the
intermediate type(10 nm). They provide cytoskeleton to maintain the shape of the cell.
When the neuron is stained by silver stain, neurofillaments will appear as brown threads
known as neurofibrills, when seen by L.M.
7- Microtubules: Well organized net work, important for the transport of substances and
organells through axon.
4
Axonal (axoplasmic) transport has two main components:
A slow stream: travels a few millimeters each day, carrying cytosolic and cytoskeletal
proteins (primarily enzymes, actin, and myosin) along the axon and maintaining the axon
terminals.
A fast stream : it is about 100 times faster than slow stream, (400 mm per day), carries
axoplasmic vesicles in the anterograde direction. The vesicles supply the various
constituents needed by the axon terminals for replacing macromolecules expended during
neurotransmission, including the enzymes, proteins, and phospholipids involved in local
synaptic vesicle production.
Anterograde movement: where macromolecules and organells such as mitochondria
and synaptic vesicles are transported from cell body, where they are synthesized, into the
axon terminal. Substantial evidence indicates that the anterograde motor protein
responsible for fast axonal transport is kinesin. Attached to the cytosolic surface of
axoplasmic vesicles, this microtubule-activated ATPase drives the vesicles along the
microtubule in the direction of its distal end.
Retrograde flow : in the opposite direction transports several molecules, including
endocytosed particles (including viruses and toxins), to the cell body. The retrograde
motor protein driving of mitochondria is more intermittent and it occurs at an
intermediate speed. About half as rapid as the fast anterograde stream, it returns unused
or recycled constituents.
Motor proteins related to retrograde axon flow include dynein, a protein with ATPase
activity present in microtubules.
Dendritic transport appears to have the same characteristics and to serve the same
functions for the dendrite as axonal transport does for the axon.
8- Lipofuscin: which is a residue of undigested material by lysosomes.
ІІ-Dendrites: they are multiple, short, branching like a tree, to increase the receptive area
of the neuron ( up to 200000 axonal termination). The diameter of the dendrite becomes
thinner as it divides. Their cytoplasm have no Golgi complex. Bipolar neurons, with only
one dendrite, are uncommon. Cytoplasmic composition of the dendrite base, close to the
neuron body, is similar to that of the perikaryon. synapses impinging on neurons are
located in dendrite spines, which are usually mushroom-shaped structures.
ІІІ- Axon: Single, cylindrical process that conduct nerve impulse from the cell body to
another cell or effector organ. It has a variable length, reaching up to 100 cm.,as the axon
of Golgi typeІ neuron, or could be very short as the axon of typeІІ neuron. The origin of
the axon from cell body is conical in shape and called axon hillock. In myelinated nerve
fibers, the portion of axon between axon hillock and the beginning of myelin is called
initial segment, which is rich in ion channels important in action potential. Sometimes,
collateral branches arise from the axon that returns to the cell body. The cytoplasm of the
5
axon (axoplasm) contains mitochondria, microfilaments, microtubules, S.E.R., but no
Nissl bodies.
Recent studies provide evidence of local synthesis of axonal proteins in some large
nerve terminals. Some vertebral axon terminals (i.e., from the retina) contain
polyribosomes with complete translational machinery for protein synthesis. These
discrete areas within the axon terminals, called periaxoplasmic plaques, possess
biochemical and molecular characteristics of active protein synthesis. Protein synthesis
within the periaxoplasmic plaques is modulated by neuronal activity. These proteins may
be involved in the processes of neuronal cell memory.
.
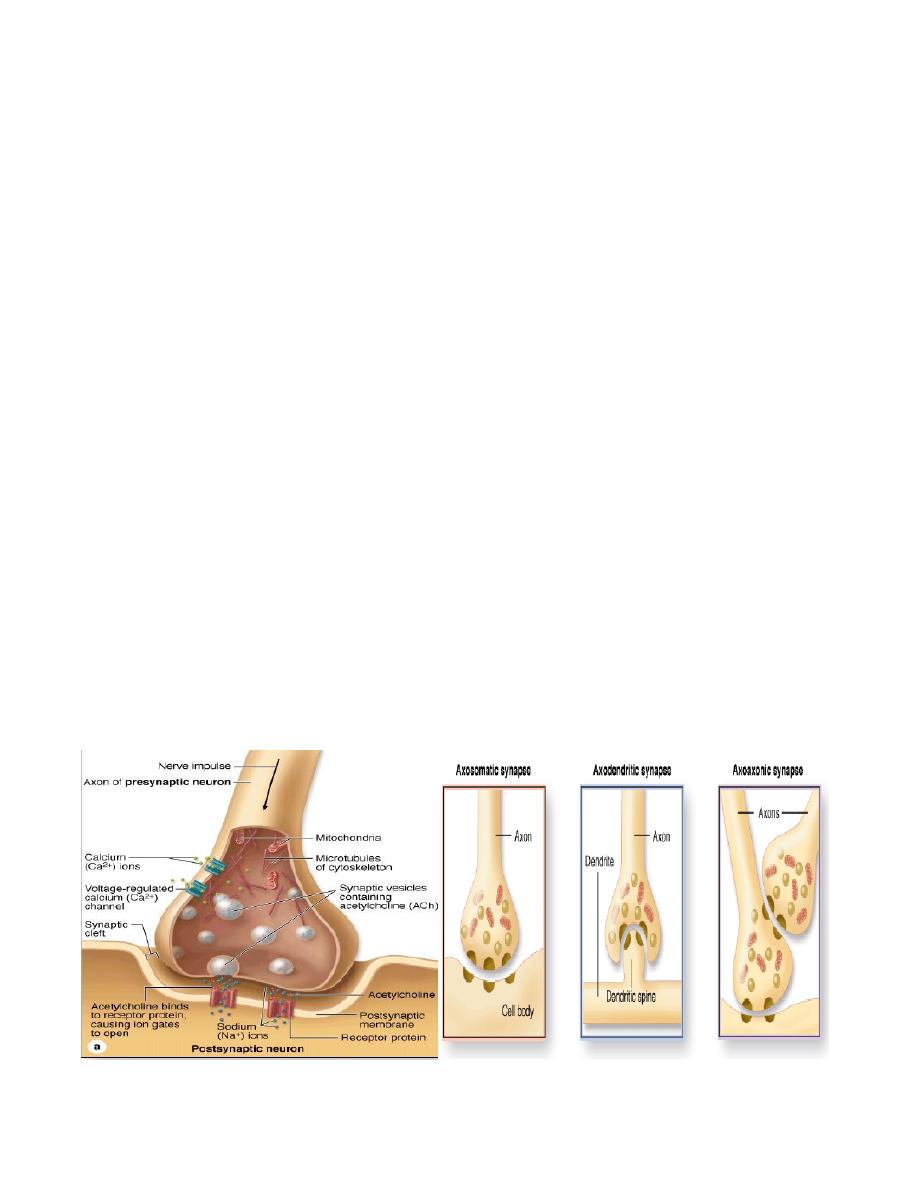
SYNAPSE
It is a unidirectional area of nerve impulse transmission through a contact between
neurons, or between neurons and effector cells ( muscle or gland).
Types of synapse:
1- Axo-somatic.
2- Axo- dendritic.
3- Axo-axonic: Very rare.
4- Chemical synapse: where the transmission of impulse is through a neurotransmitter.
5- Electrical synapse: the transmission of impulse is through gap junctions, where ions
can freely pass, and the impulse is directly conducted.
6- Conjoint synapse: is a combination of the two.
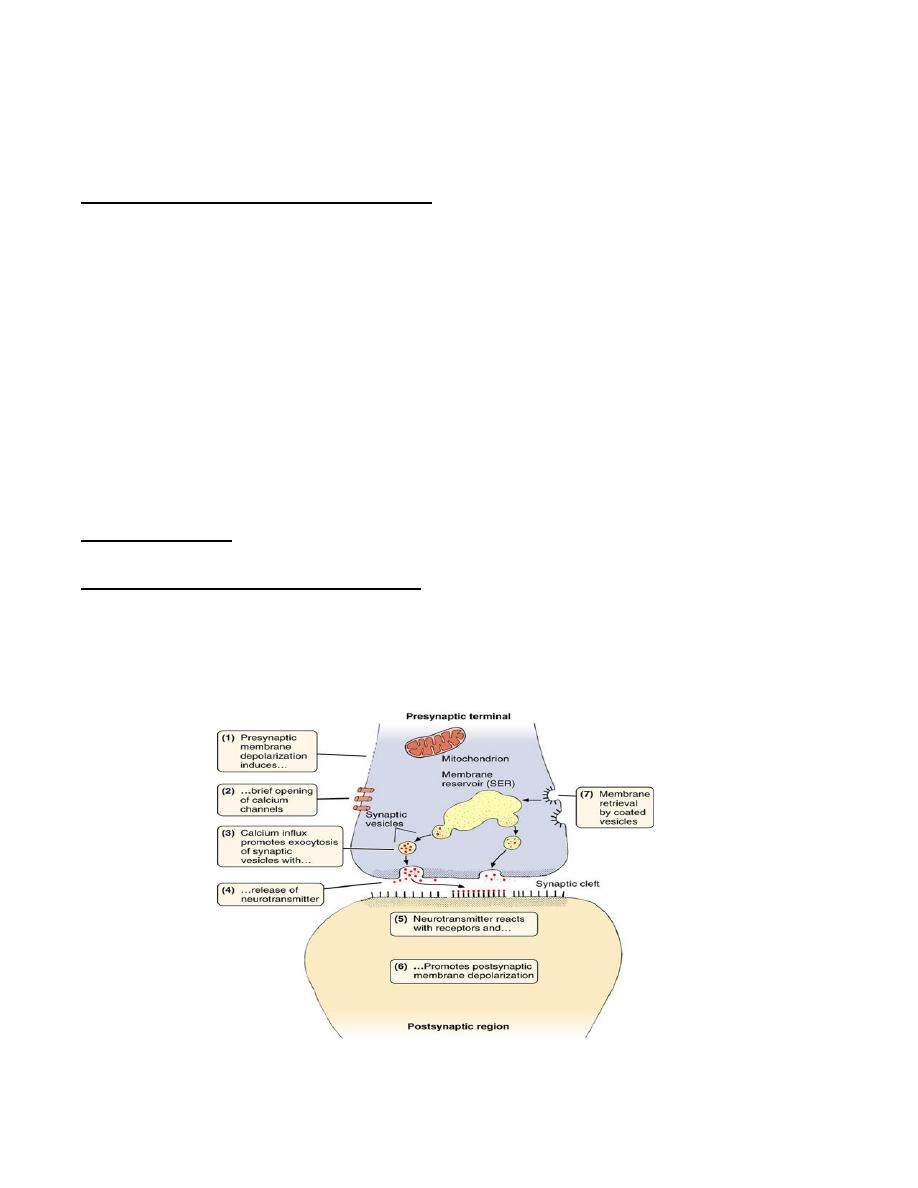
6
Structure of synapse:
The synapse lies at the axon terminal, which is the swollen terminal end of the axon
that is closely applied to the target cell. The synapse consists of the following structure:
Presynaptic terminal (membrane): lies at the axon terminal, slightly thickened,
contains special membrane proteins. It is rich in mitochondria, microtubules,
neurofillaments, and a membrane-bound vesicles of 40-60nm in diameter, called
neurosecretory vesicle. Each vesicle is small, round, with clear center, or dense-core
vesicle. These vesicles contain the neurotransmitter which is synthesized in the cell body.
Presynaptic membrane is characterized by having a grid-Like arrangement of
interconnected electron-dense projections on its cytoplasmic surface (presynaptic
density). The gaps between the projections are of suitable dimensions to direct the
synaptic vesicles into fusing with active zones in the presynaptic mernbrane when
impulses arrive at the terminal .
Nerve impulses are transient waves of depolarization that sweep rapidly across the
nerve cell membrane. A specific ATP-binding protein found on the membrane of
synaptic vesicles is required for formation, targeting, and fusion of these vesicles with the
presynaptic membrane.
Synaptic cleft: a small gap of 20 nm width, lies between pre and post synaptic
membranes. Sometimes, there are bridges at this cleft.
Post synaptic terminal (membrane): slightly thickened membrane at the target cells,
which contains receptor sites with which the neurotransmitter interacts. This component
is formed from a portion of the plasma membrane of the postsynaptic neuron and is
characterized by a layer of dense material, the postsynaptic density, on the cytoplasmic
side of the membrane.

7
When a wave of depolarization reaches synaptic terminal, it will open calcium channels
causing calcium influx that triggers the release of neurotransmitter from the
neurosecretory vesicle by exocytocytosis. The membrane of the vesicle is integrated into
the presynaptic membrane, and the neurotransmitter is released into the cleft then interact
with receptors in the post synaptic membrane of the target cell. The vesicle then recycle
back as a coated vesicle into the endosome compartment (membrane reservoir), where a
new synaptic vesicle can bud off again.
Most neurotransmitters are amines, amino acids, or small peptides (neuropeptides).
Several peptides that act as neurotransmitters are used elsewhere in the body,and are
important in regulating feelings and drives, such as pain, pleasure, hunger, thirst, and sex.
The release of neurotransmitter by the presynaptic component can cause either
excitation or inhibition at the postsynaptic membrane.
In excitatoty synapses, the release
of neurotransmitters such as acetyicholine, glutarnine, or serotonin opens calcium
channels, prompting depolarization. This leads to initiation of an action potential and
generation of a nerve impulse. In an inhibitary synapses, release of neurotransrnitters
such as gama-aminobutyric acid (GABA) or glycine, opens anion channels, causing
hyperpolarization at the postsynaptic membrane, making it even more negative, In these
synapses, the generation of an action potential then becomes more difficult.
Parkinson’s disease is a slowly progressive neurologic disorder caused by the loss of
dopamine -secreting cells in the substantia nigra and basal ganglia of the brain. Dopamine
is a neurotransmitter responsible for synaptic transmission in the nerve pathways
coordinating smooth and focused activity of skeletal muscles. Loss of dopamine secreting
cells is associated with a classic pattern of symptoms, including
• Resting tremor in the limb.
• Rigidity or Increased tone (stiffness) in all muscles
• Slowness of movement and Inability to initiate movement (akinesla)
• Loss of postural reflexes, which leads to poor balance and abnormal walking.
• Slurred speech; slowness of thought; and small, cramped handwriting
L-Dopa is a precursor of dopamine that can cross the blood—brain barrier and is then
converted to dopamine. it is often the primary agent used to treat Parklnsons disease.
Several new surgical procedures are being developed and are still in experimental
stages. These include transplantation of dopamine-secreting neurons into the substantia
nigra to replace lost neurons.
Alzheimer
’
s disease is due to deficiency of acetylecholin in the hippocampal and
cerebral cortex synapses. It is treated by choline esterase inhibitors.

8
GLIAL CELLS
They are non-neural cells, about ten times more in number than neurons. They are
found around neurons and their processes. Their main function is support. There are four
types of glial cells:
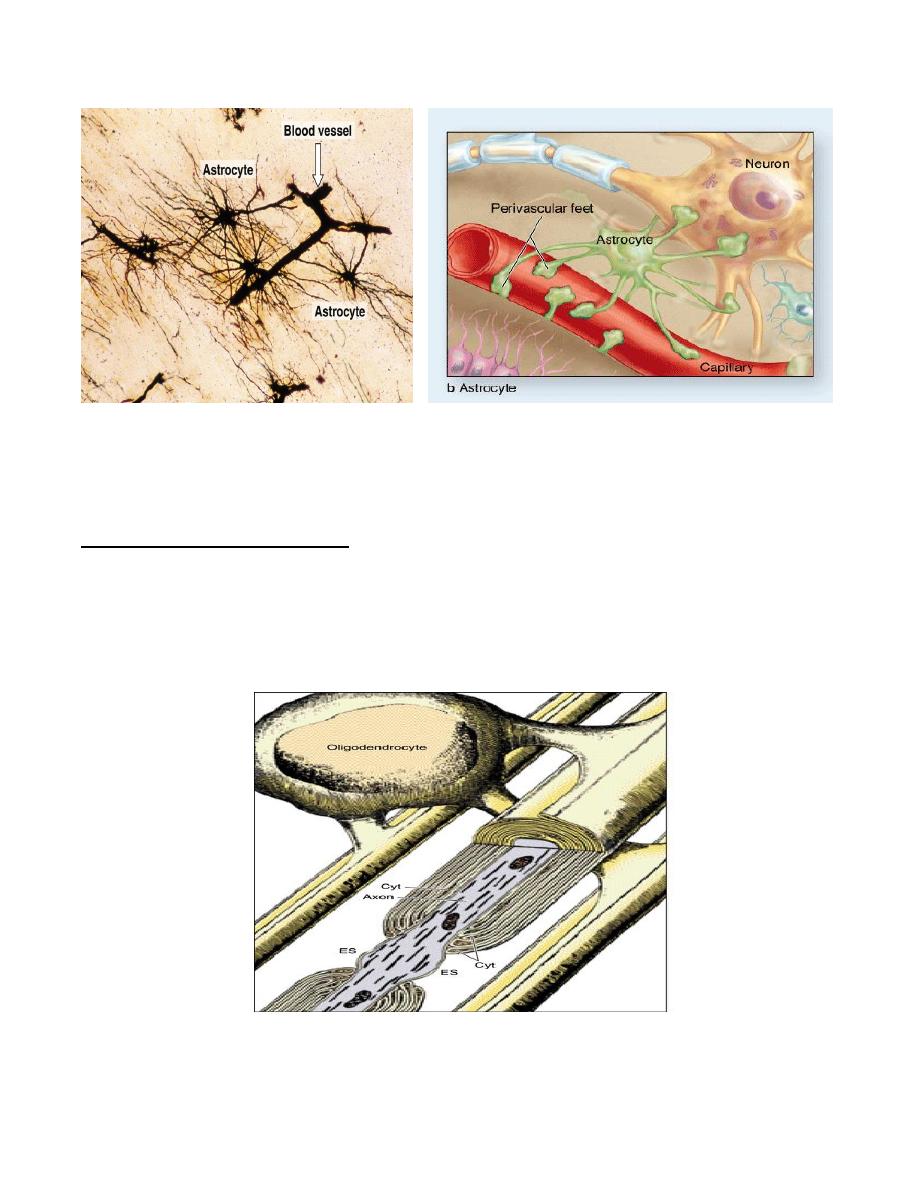
1- Astrocyte: large, star shaped cells, with multiple radiating processes. They have an
oval or slightly irregular nucleus, with dispersed chromatin. Their cytoplasm have
bundles of intermediate filaments, made of glial fibrillary acid protein(GFAP), to
maintain their structure . There are two types of astorcytes:
a- Fibrous astrocyte: found in the white matter, has few, long processes, and rich in
GFAP.
b- Protoplasmic astrocytes: found in the grey matter, with many short, branched
processes, and few GFAP. Cytoplasmic processes need a special stain to be demonstrated
histologically.
Functions of astrocyte:
●- Support.
●- Control of ionic and chemical environment of the neuron.
●- Form a scar tissue after CNS damage. The term gliosis or astrogliosis refers to the
proliferative astrocyte response, where astrocyte shows abundant intermediate filaments.
●- Their processes form the limiting glia which separates CNS from CSF.
●- Have a different receptors for several stimuli to regulate the CNS functions. They can
also secrete metabolic substances and neuroacive molecules, such as vasoactive
endothelins, opioid precursors called enkephalins, and the potentially neurotrophic
somatostatin
●- They can transfer informations from one point to another for distant site through gap
junctions
between
adjacent
astrocytes,
for
example,
the
interaction
with
oligodendrocytes, to influence the process of myelination.
●- provide coverings for bare areas of myelinated axons as the node of Ranvier and
synapses.
●- Participation in the blood-brain-barrier(B.B.B.): the astrocytes develop proceses with
an expanded end feet that are linked to the endothelial cells by juctional complexes,
forming a continuous barrier enveloping these endothelial cells. Endothelial cells are
linked together by an occluding junctions providing a continuous barrier. The cytoplasm
of endothelial cells is non- fenestrated, and the cytoplasm has few pinocytotic
vesicles.This barrier prevents the passage of toxic and harmfull substances from blood to
brain.
9
2- Oligodendrocyte: in routine section, only the nucleus is seen, as small, rounded, with
densely stained chromatin. Special stain is needed to demonstrate their cytoplasmic
processes, which are few, and small.
Functions of oligodendrocyte:
●- Myelination of axons in the C.N.S., where single cell can myelinate several axons.
Oligodendrocyte give off several cytoplasmic processes that wrap around adjacent axons.
Myelin of the CNS has fewer Schmidt-Lanterman clefts, and there is no external lamina,
so the myelin of adjacent axons may come in contact. Areas of node of Ranvier in CNS
are larger than those of the PNS.
10
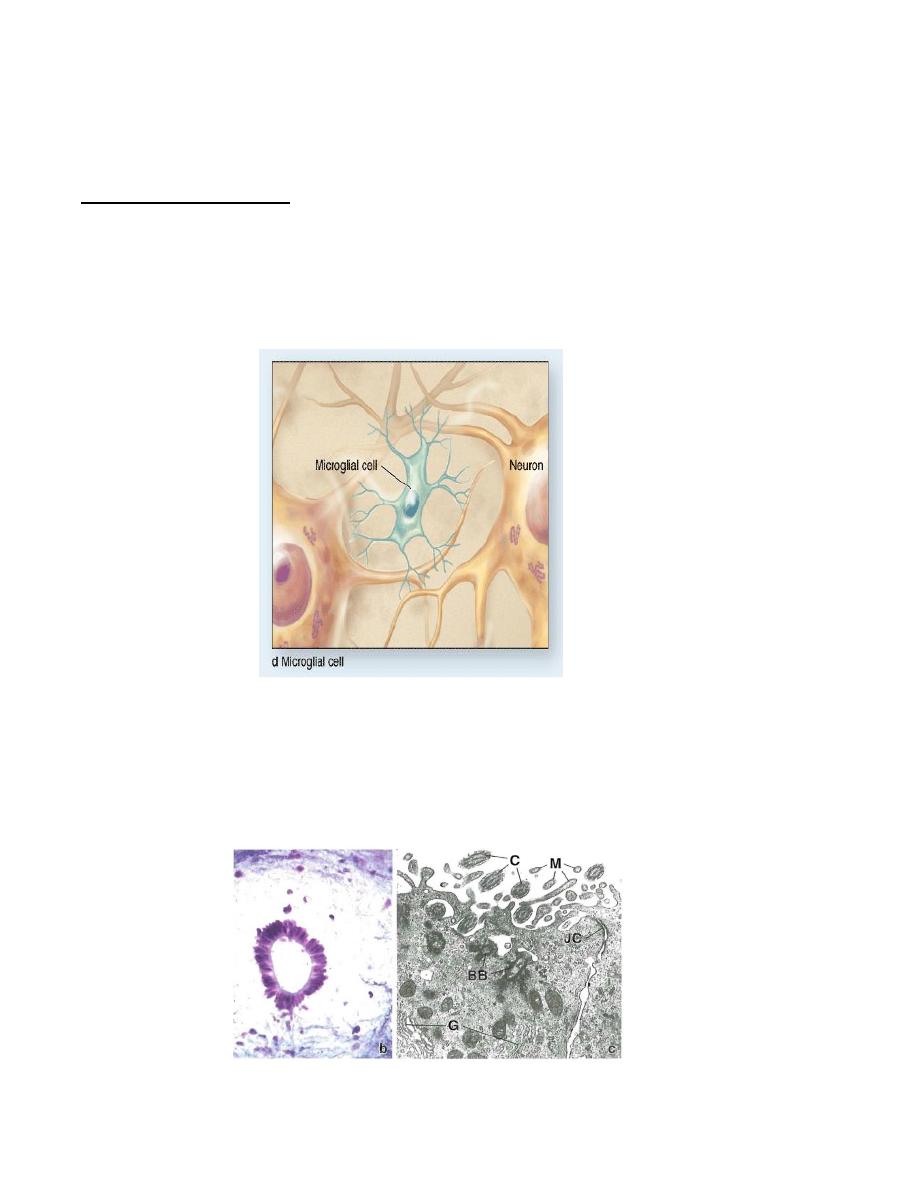
3- Microglia: In routine stain only the nucleus is seen as a dense, rod –like structure.
Special stain is needed to demonstrate the cytoplasmic processes, where they appear as
fine, irregular, ramifying processes.
Functions of microglia:
●- Act as a macropgage, as part of the mononuclear phagocytic system. There is a clear
evidence that microglia are derived postnataly from blood monocytes
●- Repair of C.N.S.
●- act as part of the immune system in C.N.S., by secreting a number of
immunoregulatory substances and dispose unwanted cellular debries.
3- Epindymal cells: epithelial like cells, cuboidal or low columnar, with an oval basal
nucleus of dense chromatin. They have an apical micro villi, with cilia. These cells
are bound together by desmosomal junctions, forming the blood-CSF barrier, to
protect CSF from foreign materials in the blood. Epindymal cells line the cavities of
brain and central canal of spinal cord.
11
PERIPHERAL NERVOUS SYSTEM
Consists of nerve fibers , ganglia, and nerve endings.
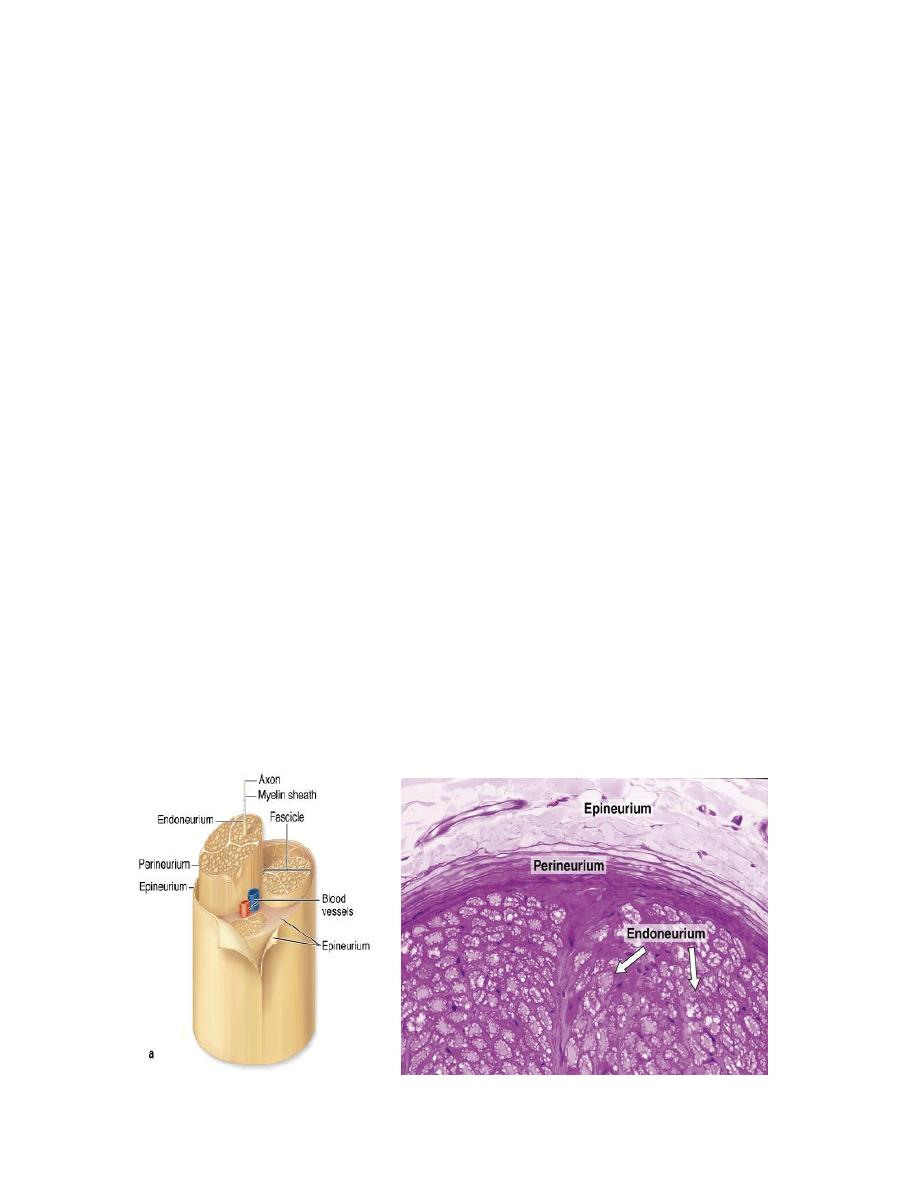
NERVE
Is a bundle of nerve fibers surrounded by a series of connective tissue sheaths. It
appears
white,
glistening,
homogenous, because of
its
myelin
sheath.
Each nerve fiber consists of :
Axon.
Special sheath of myelin produced by Schwann cell.
Fibro collagenous tissue produced by fibroblasts.
Blood vessels.
Each nerve has three types of support tissue:
1- Epineurium: an external fibrous coat of dense C.T. , with adipose tissue, and blood
vessels. It fills the spaces between bundles of nerve fibers.
2- Perineurium: consists of 7-8 concentric layers of epithelial like flattened cells, joined
by tight junctions, with collagen layers in between these cells. This makes the
peirneurium act as a barrier to protect the bundles of nerve fibers; the blood-nerve
barrier. Perineural cells posess receptors, enzymes, and transporters for active
transport of substances across perineurium. Their cytoplasm has actin filaments, so
they have a contractile ability.
3- Endoneurium: consists of longitudinally oriented reticular fibers, extracellular
matrix, with few fibroblasts and mast cells. It surrounds the individual axon and its
myelin sheath with capillary blood vessels. It is produced by Schwan cell.
12
Types of nerve fibers:
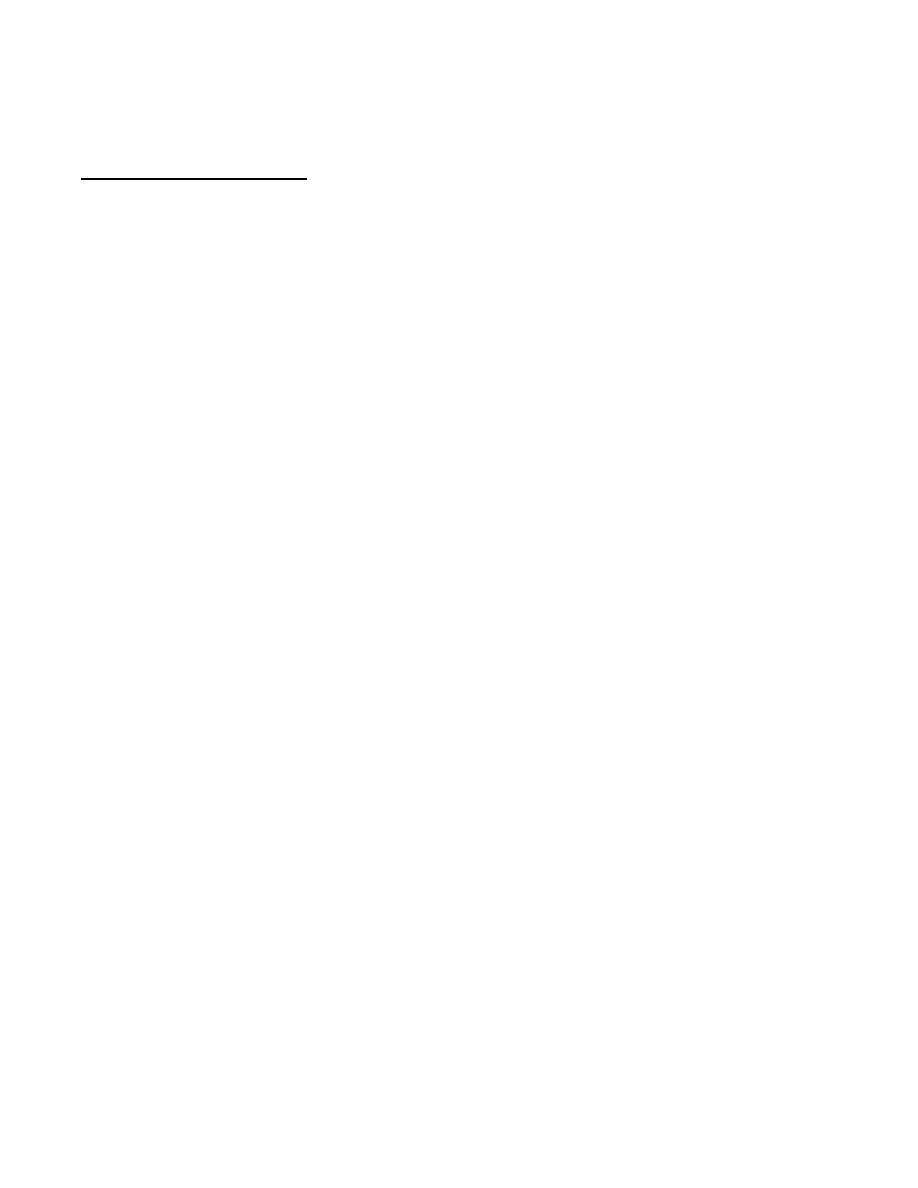
І- Myelinated nerve fiber:
Most axons are covered by a single or multiple folds of sheath cells. In the P.N.S., this
cell is Schwann cell, while in the C.N.S., it is the oligodendrocyte. This sheath is called
myelin. It increases the speed of conduction.
Schwann cell has a well defined external lamina which separates the cell from
endoneurium. Each Schwann cell produce myelin for one axon. It also support non-
myelinated nerve fibers which burry themselves into Schwann cell cytoplasm.
Myelin consists of many layers of the cell membrane of Schwann cell, which is rich in
lipid. Myelination begins with the invagination of a single axon into Schwann cell, which
brings its outer cell membrane into close apposition and seals them together, to form a
sheet of internal membrane; the inner mesaxon, which represents the narrow
intercellular space of the innermost rigs. In E.M examination these fused laminae appear
opaque and called major dense lines. These concentric dense lines alternate with a
slightly less dense intraperiod lines which are formed by fusion of the outer membrane
leaflets. The apposition of plasma membrane of the last layer as it is closes the ring
produce the outer mesxon, the narrow intercellular space adjacent to the external lamina.
Myelination continues by wraping of mesaxon around the axon, while the cytoplasm of
Schwann cell is excluded from most of the space between the membrane layers, but it
will remain in the myelin sheath at four sites to maintain the cell membrane. These sites
are:
a- Inner collar: between the axon and myelin.
b- Outer collar: adjacent to the cell body on the outer aspect of the myelin.
c- Schmidt-Lanterman cleft: lies in between the lamellae of Schwann cell at the
internodal area. The cytoplasm of the clefts contains lysosomse,mitochondria,
and microtubules. Larger axons have more clefts.
d- Paranodal area (perinodal area ): lies at each end of the myelin segment
adjacent to the node of Ranvier.
The thickness of myelin sheath depends on the number of lamellae wrapped around the
axon. The myelin sheath is interrupted through out its length by the node of Ranvier,
which represents a space between adjacent Schwann cells that has no myelin and the
axon is covered only by the interdigitations of cyotplasmic processes of Schwann cell.
The distance between two nodes is called internode, which is about 1-2mm in length,
and represents one Schwann cell. Myelin can be stained by substance that have an
affinity for lipid and protein components of the myelin such as Osmium tetraoxide.
Axon hillock and collateral branches are not myelinated .
Demyelinating diseases affects Schwan cell causing damage to the myelin sheath, and
cause a decrease or lose of the conductivity of nerve impulse along nerve fiber.
13
Multiple seclerosis is a disease affecting myelin sheath of CNS, while Guillain-Barre
syndrome affects the myelin sheath of PNS.
ІІ- Unmyelinated nerve fiber:
Found in both C.N.S. and P.N.S. They are found embedded or enveloped within the
cytoplasm of Schwann cell. They have no node of Ranvier. In C.N.S. they have no
sheath, and run freely among other processes.

14
GANGLIA
Ovoid structure consists of neuronal cells, supportive cells, Schwann cells, and satellite
cells. These cells are supported by fibro-collagenous tissue.
There are two types of ganglia:
1- Sensory ganglia: They receive afferent impulses, then transmit them to the C.N.S. if
they are associated with cranial nerves, they are called cranial ganglia, or with dossal
root of spinal cord, where they are called spinal ganglia. Ganglia is surrounded by a
layer of connective tissue rich in adipose tissue, and blood vessels. This layer is
continuous with the epineurium of the dorsal root nerve. The type of neuron present is
pseudounipolar neuron. This neuron is large, round, with central, vesicular nucleus,
and prominent nucleolus. The cytoplasm is filled with Nissll bodies. These neurons
are clumped together more at the periphery of the ganglion. Each neuron is
surrounded by satellite cells, which have spherical nuclei, of neuro-ectodermal origin.
These satellite cells form a well developed inner capsule around the neuron. Satellite
cells help to maintain a controlled microenviroment around neural cells, providing an
electrical isolation and pathway for metabolic exchange. Another outer capsule of
fibroblasts and connective tissue surrounds the inner capsule. In between ganglionic
cells, run the myelinated axons , which are seen more at the center of the ganglia.
2- Autonomic ganglia: Bulbous dilatations in the autonomic nerves. Sometimes, they
are found within the walls of some organs, especially the digestive wall, where they
are called intramural ganglia. The type of neuron is multipolar neuron, which has an
irregular shape, small size, and an eccentric nucleus. These cells are dispersed
uniformly in the ganglia. The satellite cells are few in number, and the type of axon is
usually unmyelinated.
Sensory ganglia Autonomic ganglia
15
CENTRAL NERVOUS SYSTEM
It consists of brain, spinal cord, and glial cells. These organs are relatively soft, gel-
like, because they have no connective tissue, so, they are protected by the skull, and
vertebral column. They are also covered by a membranes of connective tissue called
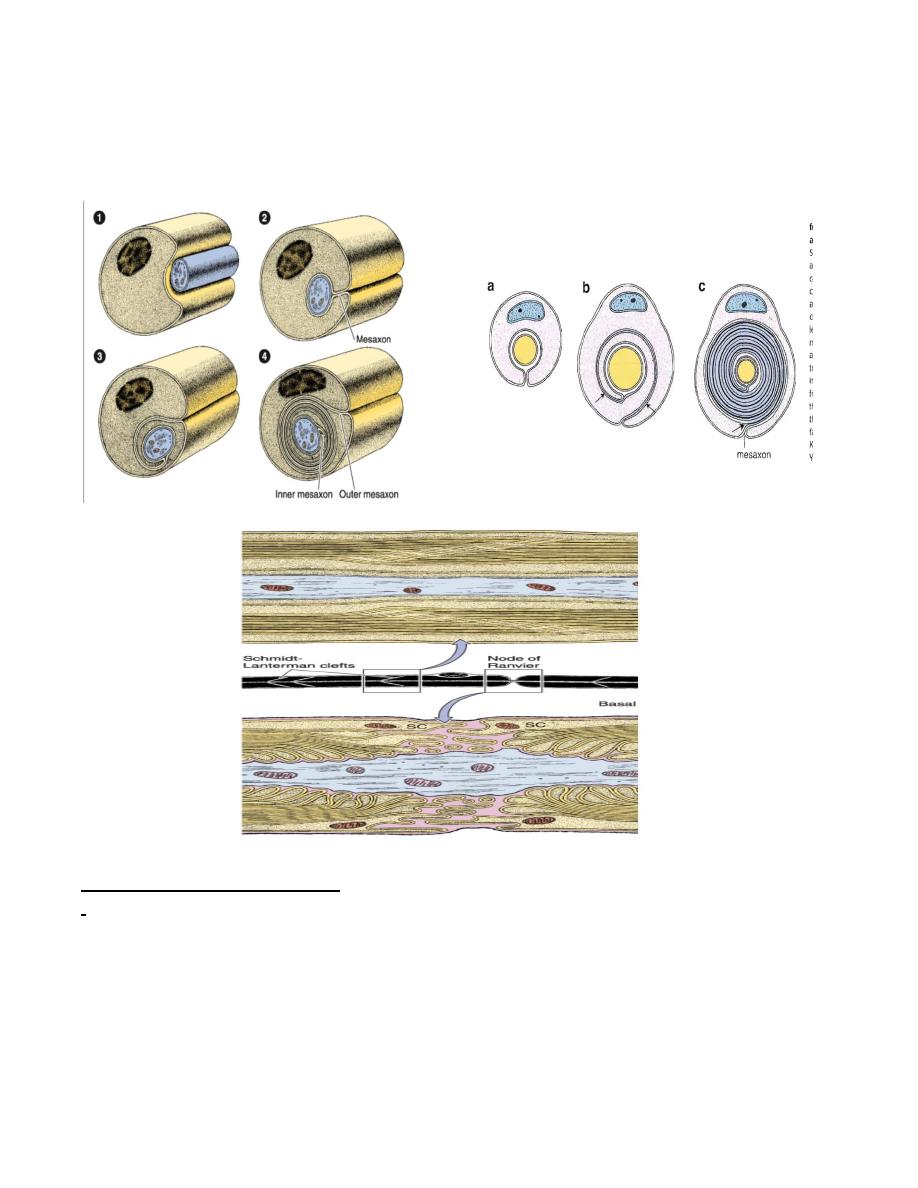
meninges. These meninges are arranged from outside as:
1-Dura mater: composed of dense connective tissue, continuous with the
periosteum of the skull, while it is separated from the periosteum of the vertebral column
by the epidural space, which contains veins, loose connective tissue, and adipose tissue.
Dura mater is separated from the next layer; the arachnoid, by a thin sub dural space.
Both surfaces of dura are covered by simple seq. epith. of mesenchymal origin.
Sheats-like extensions from the inner surface of dura penetrates parts of brain giving
support and carry arachnoid to deeper parts of brain.
2- Arachnoid mater: consists of connective tissue devoid of blood vessels. It is found as
two layers; one is in contact with the dura; the roof layer, while the other is a system of
trabeculae extends to the pia mater. The cavities between these trabeculae represents the
sub arachnoid space. This space is filled with the cerebrospinal fluid(C.S.F.). Both
surfaces of arachnoid are covered by simple seq. epith.
Arachnoid, in some areas perforates the dura, forming the arachnoid villi. These villi
are covered by endothelial cells and terminates in the venous sinuses of the dura. These
villi reabsorbe C.S.F. into the blood of venous sinuses.
3- Pia mater: composed of loose connective tissue, rich in blood vesels. It is separated
from the neural element by a layer of neuroglial processes of astrocytes, called
limiting glia. This membrane separates C.N.S. from C.S.F. Pia mater is covered by
simple seq. epith. , and it follows all the irregularities of the C.N.S.
16
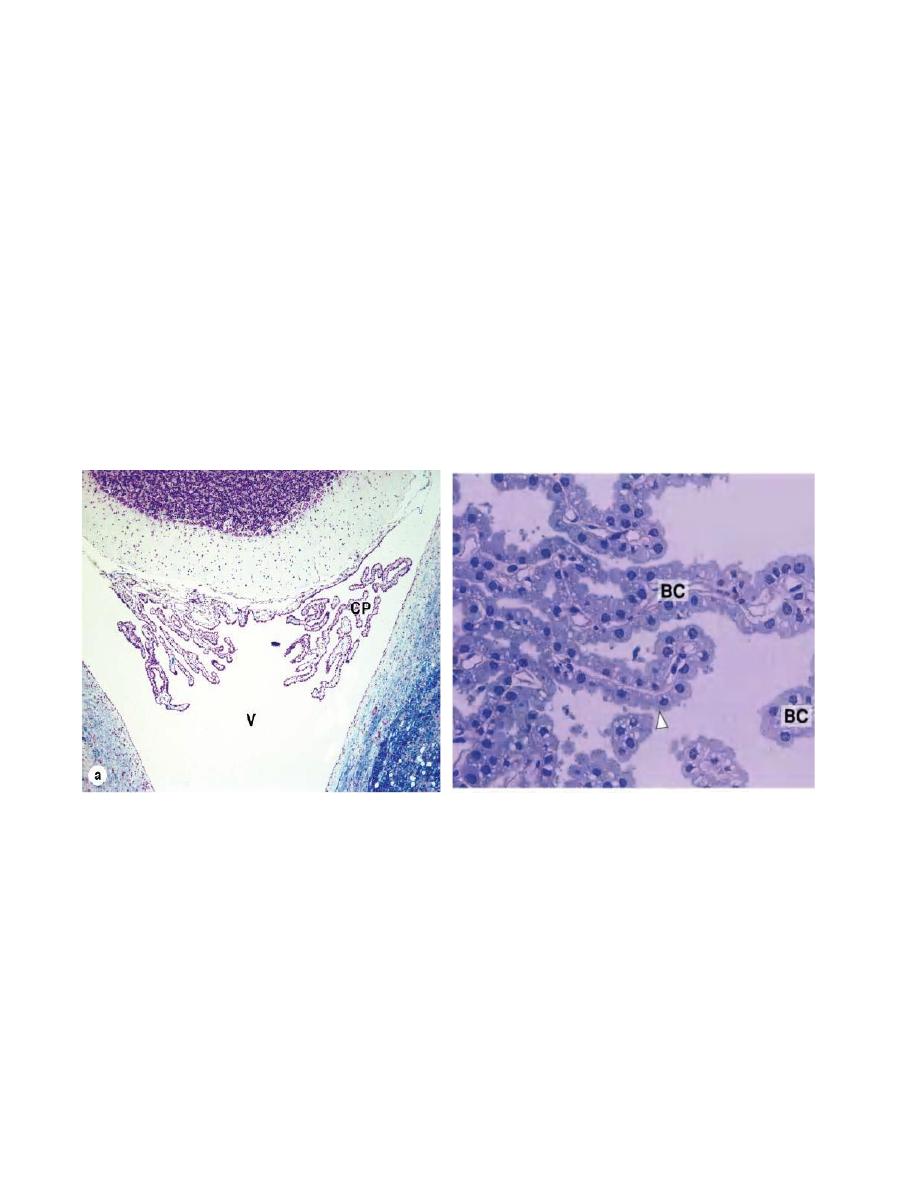
Choroid plexus: is an invagination of pia mater into the ventricles of brain. It consists
of vascular stroma of loose connective tissue rich in dilated fenestrated capillaries,
covered by cuboidal or law columnar epith. cells. These epith. cells rest on a basement
membrane linked by junctional complexes, have an apical microvilli, and have the
characteristics of ion transport. Choroid plexus secrets C.S.F. which runs in the brain
ventricles, central canal of spinal cord, sub arachnoid space, and perivascular spaces.
C.S.F. will be reabsorbed by the arachnoid villi into the venou system.
C.S.F. is clear, low density, with low protein content. It contains few desequamated
cells, and about 2-5 lymphocytes/ml. C.S.F. is important in the metabolism of C.N.S., and
for its protection.
A decrease in the absorption of C.S.F. or any blockage in its flow in the ventricles will
cause hydrocephalus, which will increase the intra cranial pressure. Congenital
hydrocephalus cause impairment in brain development and muscle weakness, while in
adults it will cause neural damage to brain.
BRAIN
It consists of two parts:
І- Cerebrum: when sectioned, it shows two different regions; the superficial one appears
grey and called grey matter, and the inner or deep one which appears white and called
white matter.
1- Grey matter: forms the cerebral cortex. It contains neural cell bodies, dendrites, and
the initial portion of axons, and glial cells. It consists of six layers which are poorly
defined from each other. The most prominent neuron is the pyramidal cell. It has a
triangular shape, the dendrites are oriented at the periphery, while axon arise from
the base of the cell body, and is directed towards the medulla.
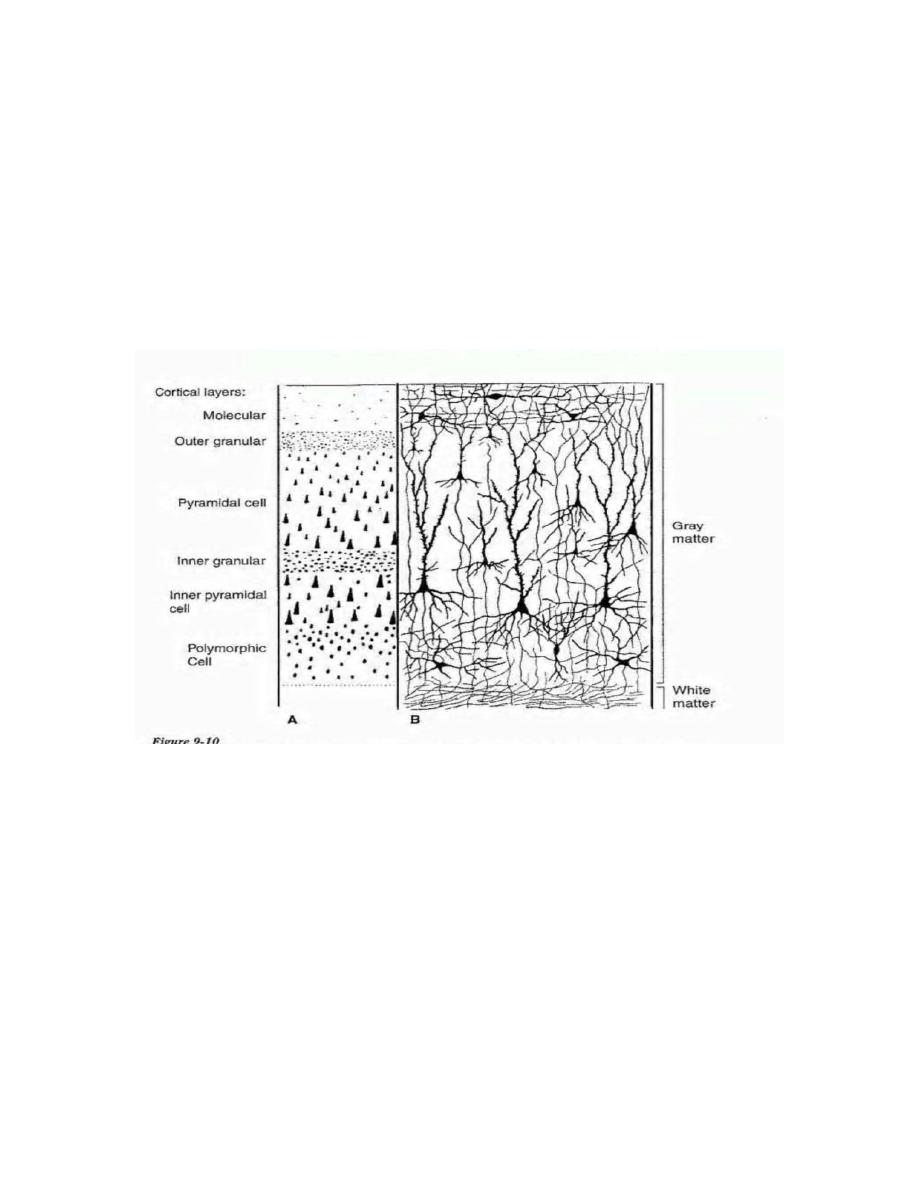
17
The large pyramidal cells of the motor cortex , occasionally referred to as Betz
cells, represent upper motor neurons, which are efferent neurons situated entirely
within the CNS that control voluntary movements and skeletal muscle tone. Their
efferent impulses pass down descending supraspinal pathways to reach lower motor
neurons situated in the anterior horns of the spinal cord. The efferent impulses from
lower motor neurons then elicit the contraction of skeletal muscle fibers.
2- White matter: The main component is the myelinated nerve fibers , and
oligodendrocytes. It has no neuronal cell bodies.
ІІ- Cerebellum: like cerebrum, it consists of an external grey matter, and an inner white
matter; the medulla.
1- Grey matter: consists of three layers:
a- Molecular layer: it is the superficial layer, contains scattered stellate cells, whose
unmyelinated axons run in a horizontal direction. Deeeper in this layer, basket cells
and their collaterals are found. This layer contains also the axons of granule cells,
and the dendrites of Purkinje cells.
b- Purkinje cell layer: consists of one row of flask shaped cell body. It gives off one
or two thick dendrites, which extend into the molecular layer, and branch more like
a fan. Their axons are directed towards the granular layer, then to the medulla.
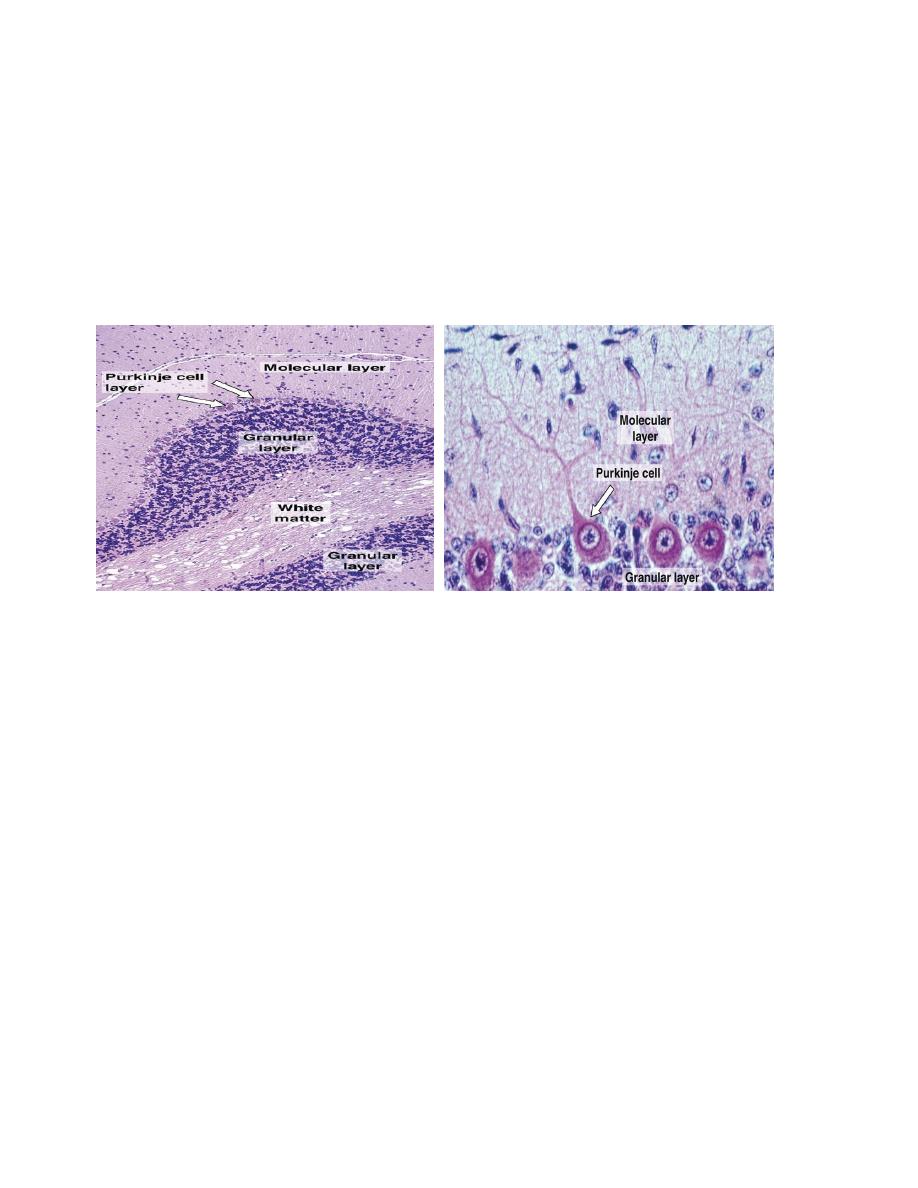
18
c- Granular layer: consists of smallest cells in the body; the granule cells. They have
darkly stained nuclei, and very little amount of cytoplasm. This layer also contains
large satellite cells or Golgi type ІІ cells, which have vesicular nucleus, and more
cytoplasm. In between granule cells, there is a small irregular clear space, where the
cells are absent, and only synaptic complexes are found. These spaces are called
glomeruli.
2- White matter: consists of myelinated nerve fibers.
SPINAL CORD
In cross section, two regions are recognized; an outer white matter, and an inner grey
matter, with a central opening called central canal.
1- Grey matter: it has an H- shape, where the horizontal bar represents the grey
commissure. It is divided into an anterior and posterior commissures in relation to the
central canal. The arms of the H represent the posterior horns, while the legs
represent the anterior horns.
Anterior horn(ventral horn) is wider and shorter than the posterior (dorsal) horn. It
contains large motor neurons, whose axons form the ventral roots. Posterior horn contains
large and small neurons. It receives sensory fibers from neurons in the spinal
ganglia(dorsal roots).
On the dorsal surface of the spinal cord, there is a longitudinal groove in the middle
called the dorsal median sulcus. From this sulcus, a neuroglial membrane extends
towards the central canal called dorsal median septum, which divides the white matter
into two halves. Each half is divided by the dorso-intermediate septum into
dorsomedial column, and dorsolateral column.
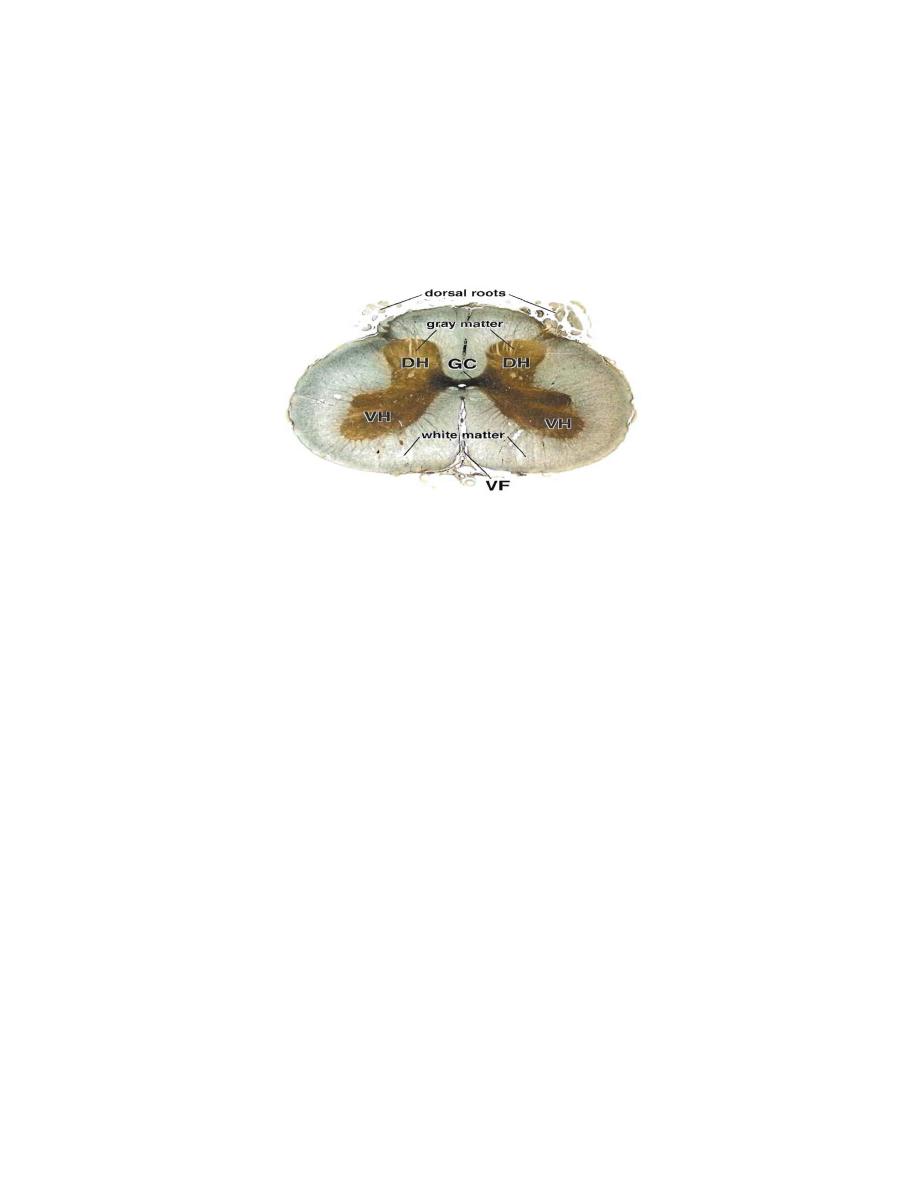
19
On the ventral surface of spinal cord, white matter is divided into two halves by a deep
groove; the ventral(anterior) median fissure, where pia mater runs in this groove.
Central canal is lined by epindymal cells, which are low columnar, ciliated cells.
2- White matter: consists mainly of myelinated neve fibers.
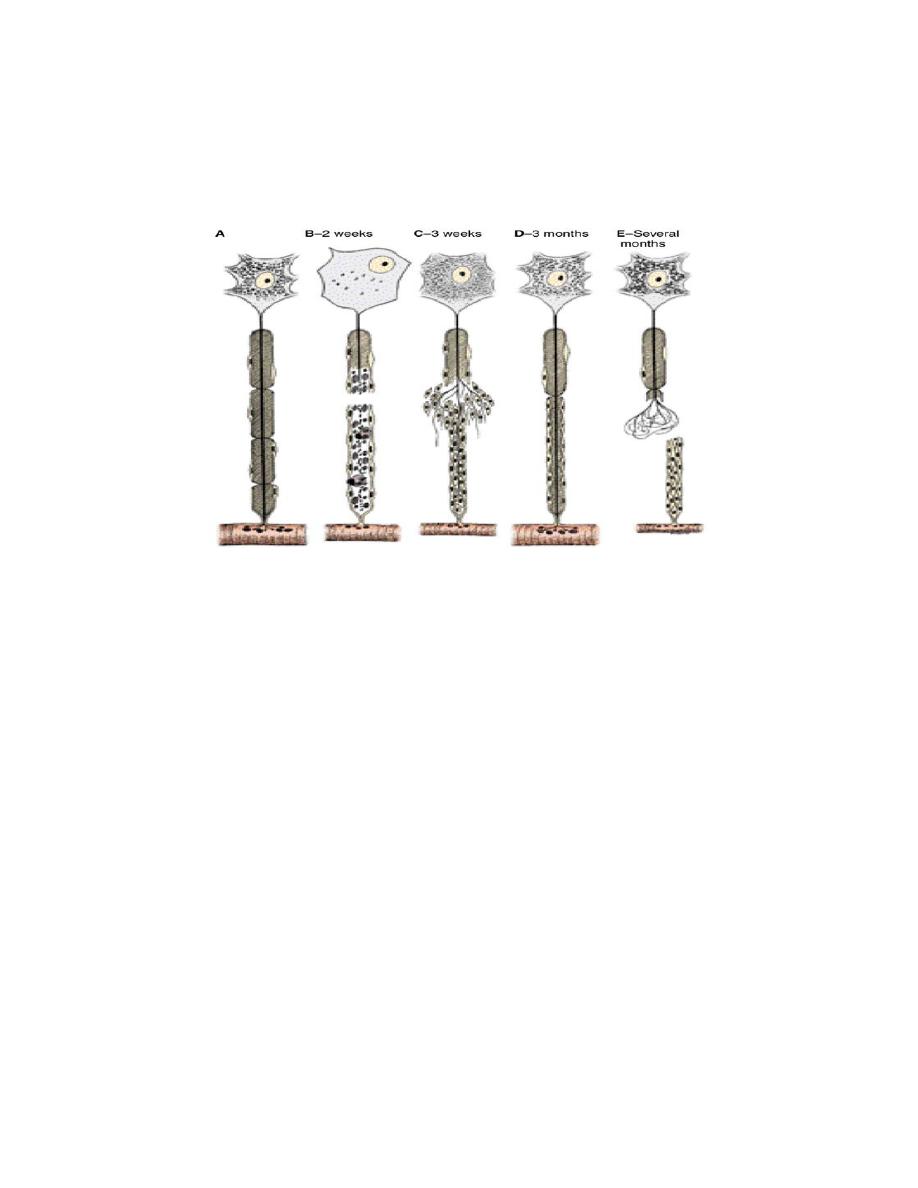
REPAIR OF NERVOUS SYSTEM
Neurones do not divide, so, when they are injured, they will not be repaired. Processes
could be repaired only when their perikarion is intact. After an injury to a nerve, the cell
body will show certain changes known as chromaotolysis, which begin after 1-2 days of
injury and reaches its peak at two weeks.The nucleus become eccentric, dissolution of
Nissll bodies, accumulation of nurofillaments, and swelling of the perikarion. The distal
part of the injured nerve will degenerate by Schwan cell lysosome and macrophages.
Macrophage will secrete interleukin-1 which stimulate Schwan cell to secrete substances
that promote nerve growth. In the proximal part, Schwan cell will proliferate and form a
longitudinal solid column which act as a guide for the sprouting axon, which will be
directed towards the column. The axon will grow and branch, forming several filaments,
until it reach the target organ.
If the distance between proximal and distal parts of the injured nerve is large or the
limb is amputated, the newly grown nerve will form a swelling known as neuroma,
which may cause continuous pain (phantom pain).
Neural plasticity:
After an injury, a new synapses might be formed to replace the lost ones, giving rise to
a new communications with functional recovery. This process is controlled by many
factors, known as neurotrophins, which are produced by neurons, glial cells, Schwan
cells, and target cells.
20
Recent studies showed that neural stem cells in some regions of mammals brain and
spinal cord might regenerate neurons, astrocytes, and oligodendrocytes, or even some
cells that not related to nevous tissue. Retinal stem cells could produce retinal neural
cells, photoreceptors, and neuroglial cells.
21
SOMATIC AND VISCERAL RECEPTOR SYSTEM
It consists of free and encapsulated nerve endings, or specialized non- nural cells.
І- Touch and pressure(mechano receptors): include:
1- Encapsulated type: such as capsule of Ruffini, Merkel, Krause, and Pacinian
corpuscle. They are covered by connective tissue capsule. They present more in the
dermis of digits, mesentery, and peritoneum. Pacinian corpuscle is composed of 20-70
layers of flatened fibroblasts, alternating with thin collagen fibers.
2- Free: found around most of the length of hair follicle as a longitudinal or
circumferential arrays of free unmyelinated fibers.
ІІ- Warmth, cold, and pain receptors: usually present as free nerve endings, branch in
the dermis, and penetrate the basement membrane, and extend into the cell layer of the
epidermis.
ІІІ- Proprioceptive system: include:
1-Encapsulated: as muscle spindle. It consists of connective tissue capsule
surrounding a fluid- filled space that contains few, long, and thick muscle fibers, with
some short, thinner fibers(intrafusal fibers). Several nerve endings penetrate muscle
spindle to detect any changes in the length of muscle fibers.
3- Free: as Glgi tendon organ. It is a sensory nerve at the myotendinous junction, to
detect tension differences in the tendon.
Pacinian corpuscle Motor end plate Muscle spindle
