Histology
Prof.Dr.Faraid
Lec.6
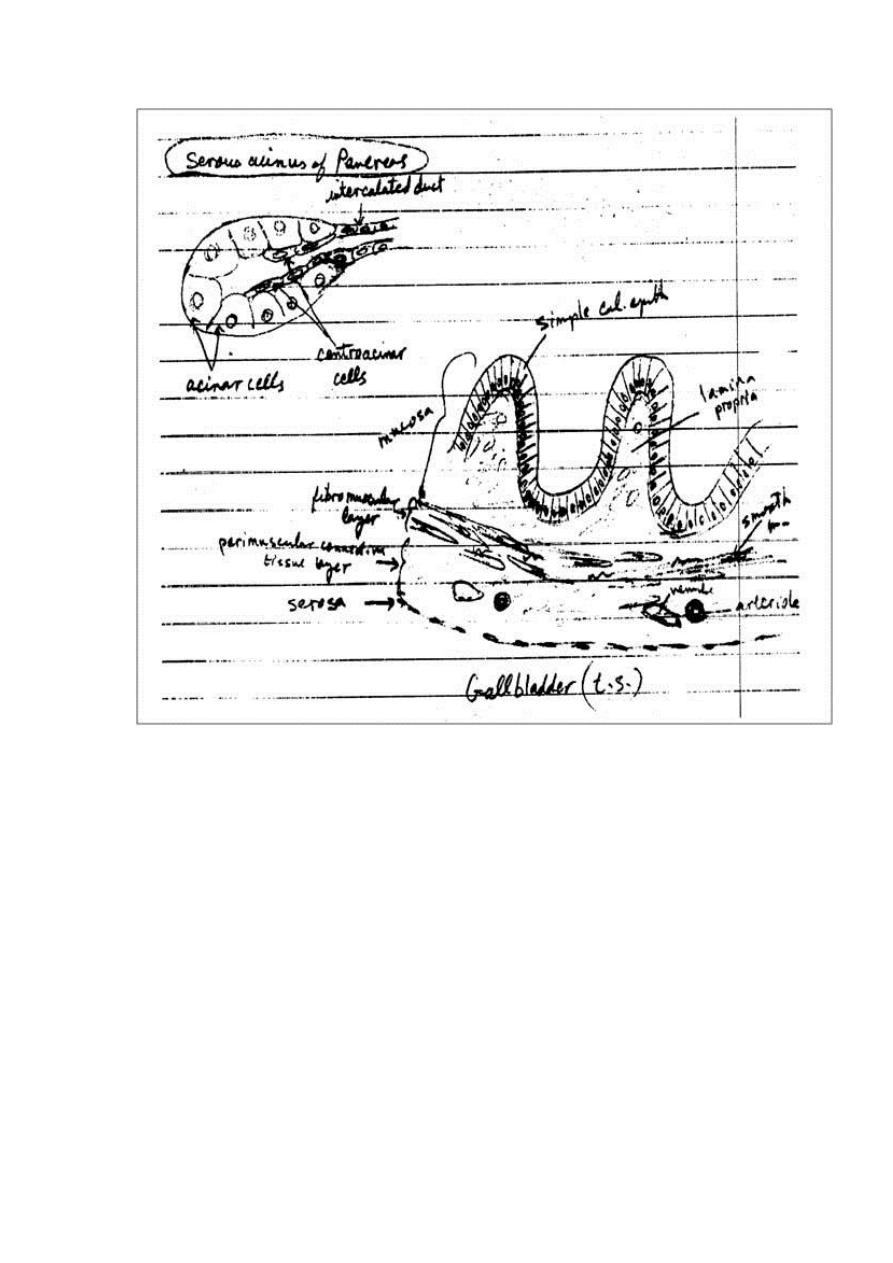
Gallbladder:
It is a hollow, pear-shaped organ attached to the lower surface
of the liver. It can store 30-50 ml of bile. The gallbladder
absorbs water from the bile and stores the bile in a concentrated
form. The wall of the gallbladder consists of the following
layers:
1. Mucosa: is composed of a simple columnar epithelium
and a richly vascularized lamina propria. The mucous
membrane is thrown into folds that are particularly evident
in the empty bladder. There is no gland in the gallbladder
except in the neck region.
2. Fibromuscular layer: is composed of a thin layer of
smooth muscle fibers interspersed within the layers of
loose c.t. that are rich in elastic fibers. The muscle
contracts and empties the gallbladder in response to
cholecystokinin released by entero endocrine cells (I-cells)
in the intestinal mucosa when dietary fat enters the small
intestine.
3. Perimuscular connective tissue layer: is a wide layer of
connective tissue, which contains blood vessels, lymphatic
and nerves.
A thick layer of c.t. binds the superior surface of the
gallbladder to the liver.
4. Serosa: covers its free surface.
Pancreas:
The pancreas is a mixed exocrine-endocrine gland that produces
digestive enzymes and hormones. The enzymes are stored and
released by cells of the exocrine portion. The hormones are
synthesized in clusters of endocrine epithelial cells known as
islets of Langerhans. The pancreas is a retroperitoneal gland. It
has a head, body, and tail. The head is lodged in the concavity of
the C-shaped duodenum and its narrower boy and tail extend to
the hilus of the spleen.
A thin capsule of c.t. covers the pancreas and sends septa into it,
separating the pancreatic lobules. These septa convey blood and
lymphatic vessels into and out of the parenchyma and house the
interlobular ducts.
The exocrine portion of the pancreas is a compound acinar
serous gland, similar in structure to the parotid gland. In
histologic sections, a distinction between the two glands can be
made based on the absence of striated ducts and the presence of
the islets of Langerhans in the pancreas. Another characteristic
is that in the pancreas the initial portions of intercalated ducts
penetrate the lumens of the acini. Nuclei, surrounded by a pale
cytoplasm, belong to centroacinar cells that constitute the intra-
acinar portion of the intercalated duct. Centroacinar cells are
found only in the pancreatic acini. Intercalated ducts are
tributaries of larger interlobular ducts. There are no striated
ducts in the pancreatic ducts system.
The exocrine pancreatic acinus is composed of several serous
cells surrounding a lumen. These cells are highly polarized, with
a spherical nucleus, and are typical protein-secreting cells. The
number of zymogen (secretory) granules present in each cell
varies according to the digestive phase and attains its maximum
in animals that have fasted. Myoepithelial cells do not surround
the acini in the pancreas.
The human exocrine pancreas secretes, besides water and
ions, the following enzymes and proenzymes: trypsinogens,
chymotrypsinogen,
carboxy
peptidases,
ribonuclease,
deoxyribonuclease, amylase, lipase, phospholipase and elastase.
The majority of the enzymes are stored as proenzymes in the
secretory granules of acinar cells, being activated in the lumen
of the small intestine after secretion. This is very important for
the protection of the pancreas. In acute pancreatitis, the
proenzymes may be activated and digest the whole pancreas,
leading to very serious complications.
Pancreatic secretion is controlled mainly through two
hormones secretin and cholecystokinin that are produced by
enteroendocrine cells of the duodenal mucosa. Stimulation of
the vagus nerve (parasympathetic stimulation) will also produce
pancreatic secretion.
Secretin promotes secretion of an abundant fluid, poor in
enzyme activity and rich in bicarbonate.
Cholecystokinin promotes secretion of a less abundant but
enzyme-rich fluid.
Islets of Langerhans (endocrine pancreas):
They appear as rounded clusters of cells embedded within
exocrine pancreatic tissue. Most islets are 100-200 µm in
diameter and contain several hundred cells, small islets also are
found. There may be more than one million islets in the human
pancreas, with a slight tendency for islets to be more abundant
in the tail region.
In sections, each islet consists of lightly stained polygonal
or rounded cells, arranged in cords separated by a network of
blood capillaries. A fine capsule of reticular fibers surrounds
each islet.
Using immunocytochemical methods four types of cells A,
B, D, and F have been located in the islets. The ultrastructure of
these cells resembles that of cells synthesizing polypeptides.
A or α-cells ≈ 20% produce the hormone glucagon whose
effects are opposite those of insulin. They are located mostly at
periphery of islets. By using special stain, the granules in their
cytoplasm stain acidophilic.
B or β-cells are the most numerous ≈ 70%. Produce insulin and
tend to be concentrated in the center of the islet their granules
stain blue.
D or delta cells 5% produce somatostatin.
F or PP cells 1-2% secrete pancreatic polypeptide.
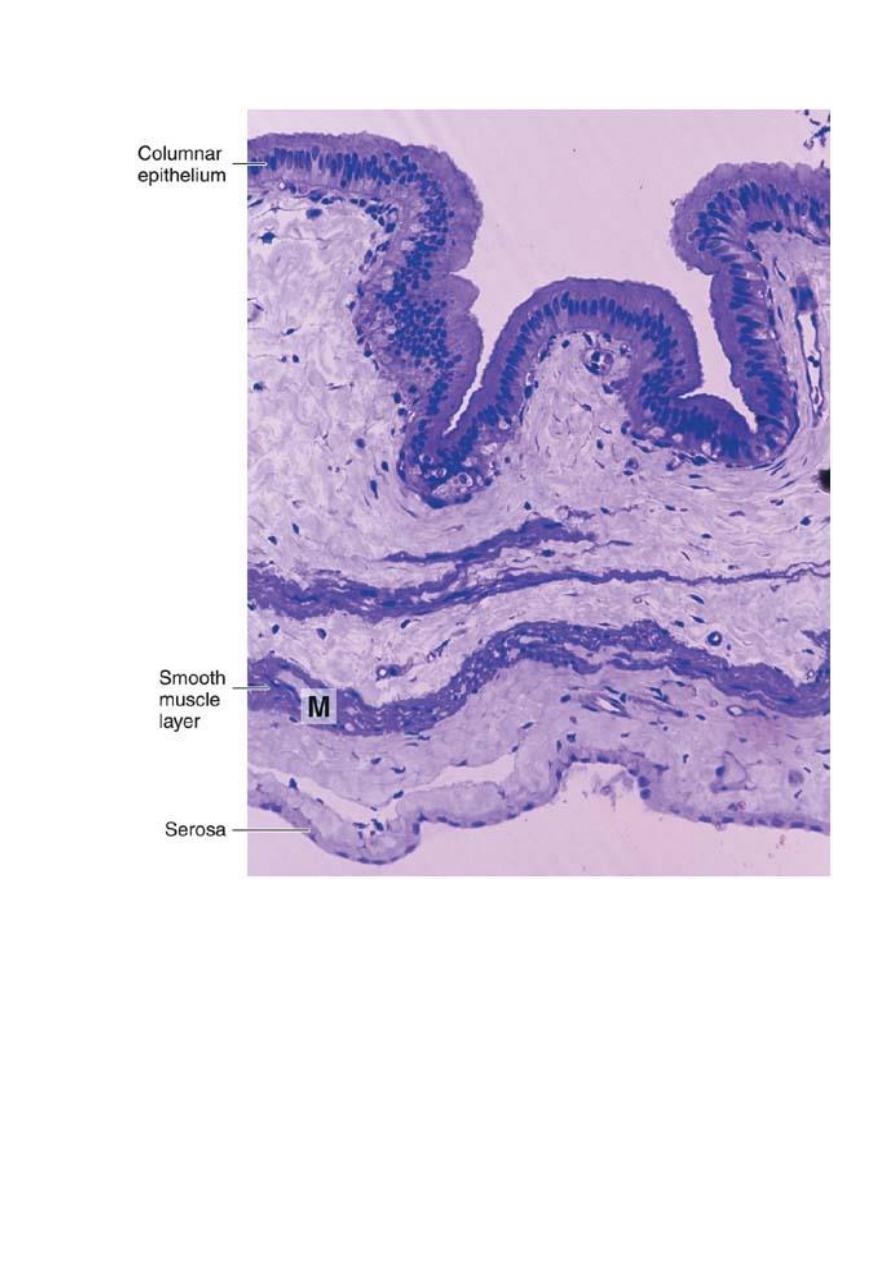
Photomicrograph of a section of gallbladder. Note the lining
of columnar epithelium and the smooth muscle layer (M).
PT stain. Low magnification.
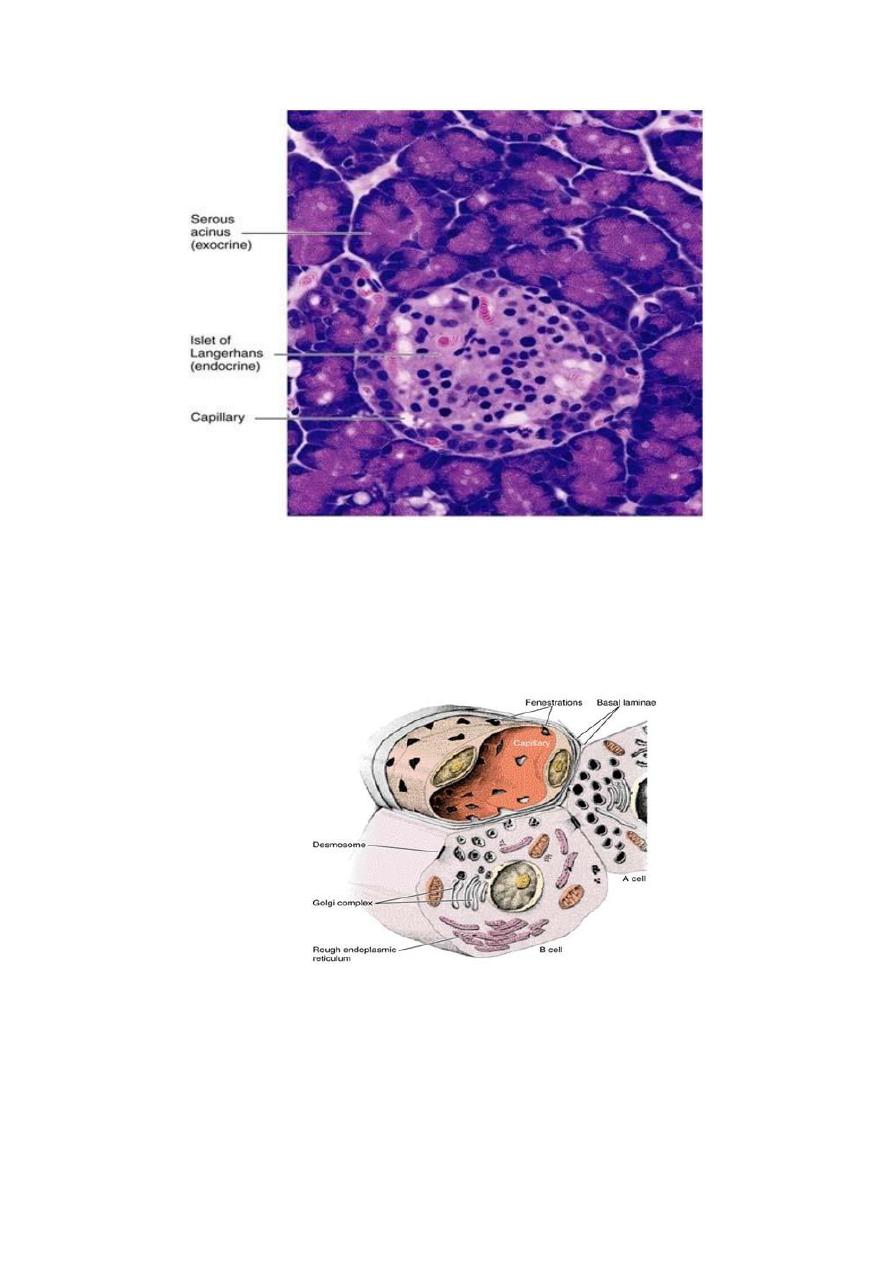
Photomicrograph of a pancreas showing the exocrine portion (acini)
and the endocrine portion (islet of Langerhans). The acini contain
secretory cells with basophilic cytoplasm. Different types of
endocrine cells are seen in the islet. PT stain. Medium magnification.
Drawing of the A and B cells; showing their main ultrastructural
features. The B cell’s granules are irregular, whereas the A cell’s
granules are round and uniform.
