Prof. Dr.Hedef.D.El-Yassin
1
Biochemistry and Disorders of Hormones of the
Kidney, Heart and Adipose tissue
And
Hormones that regulate calcium homeostasis
Lecture 8
Objectives
1. to list the hormones secreted by kidney and state their functions
2. to list the hormones secreted by heart and state their functions
3. to list the hormones secreted by the adipose tissue and state their functions
4. to list the hormones that regulate calcium homeostasis and state their functions
The Kidney
The human kidney secretes two hormones
Erythropoietin
Calcitriol (1,25[OH]
2
Vitamin D
3
) (discussed later)
Erythropoietin
(EPO) is a glycoprotein hormone that is a growth factor for erythrocyte (red blood cell)
precursors in the bone marrow.
In adults primarily by peritubular cells in the kidneys, where its production is stimulated
by low oxygen levels in the blood.
Some EPO is also produced by the liver, which is the primary source in the fetus.
Actions
EPO acts by binding to a specific erythropoietin receptor (EpoR) on the surface of red cell
precursors in the bone marrow, stimulating them to transform into mature red blood cells.
As a result the oxygen level in blood reaching the kidney rises and the amount of EPO
produced decreases.
People with failing kidneys can be kept alive by dialysis. Nevertheless, dialysis only
cleanses the blood from wastes. Without a source of EPO, these patients suffer from
anemia.
Prof. Dr.Hedef.D.El-Yassin
2
The heart
In response to a rise in blood pressure, the heart releases two peptides
A-type Natriuretic Peptide (ANP)
This hormone of 28 amino acids is released from stretched atria (hence the "A").
B-type Natriuretic Peptide (BNP)
This hormone (29 amino acids) is released from the ventricles. (It was first discovered in
brain tissue; hence the "B")
Both hormones lower blood pressure by:
Relaxing arterioles
Inhibiting the secretion of renin and aldosterone
Inhibiting the reabsorption of sodium ion by the kidneys.
The latter two effects reduce the reabsorption of water by the kidneys. So the volume of
urine increases as does the amount of sodium excreted in it. Te net effect of these actions
is to reduce blood pressure by reducing the volume of blood in the circulating system.
These effect give ANP and BNP their name (natrium= sodium; uresis= urinate)
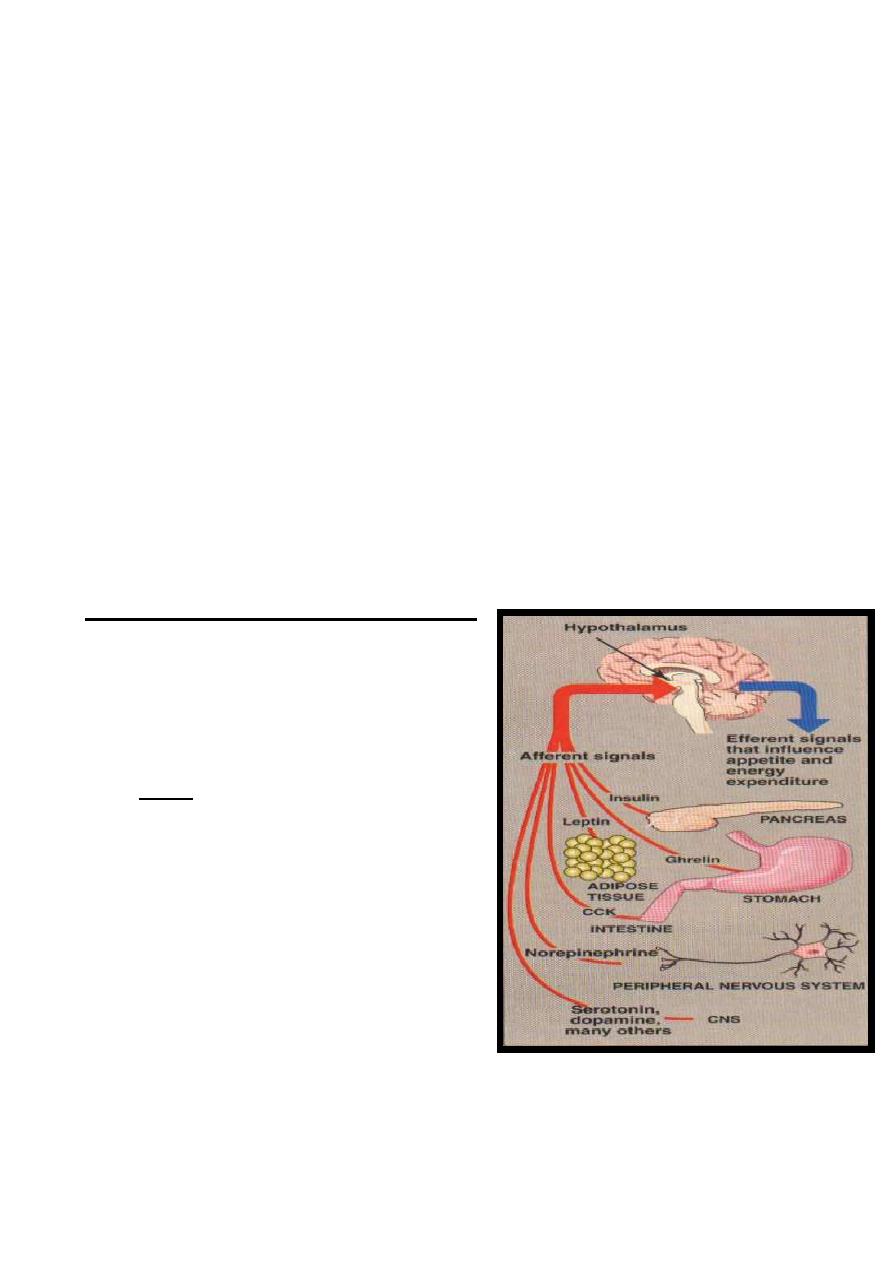
Hormones of adipose tissue
Although the adipocyte's primary role is to store
fat, it also functions as an endocrine cell that
releases numerous regulatory molecules, such as
leptin, adiponectin, and resistin
1. Leptin: Studies of the molecular genetics
of mouse obesity have led to the isolation
of at least six genes associated with
obesity. The most well-known mouse
gene, named Ob (for obesity), leads to
severe hereditary obesity in mice. It has
been identified and cloned. In one strain of
fat mice, the gene was completely absent,
indicating that the gene's protein product is
required to keep the animals' weight under control. The product of the Ob gene is a
hormone called leptin.
Prof. Dr.Hedef.D.El-Yassin
3
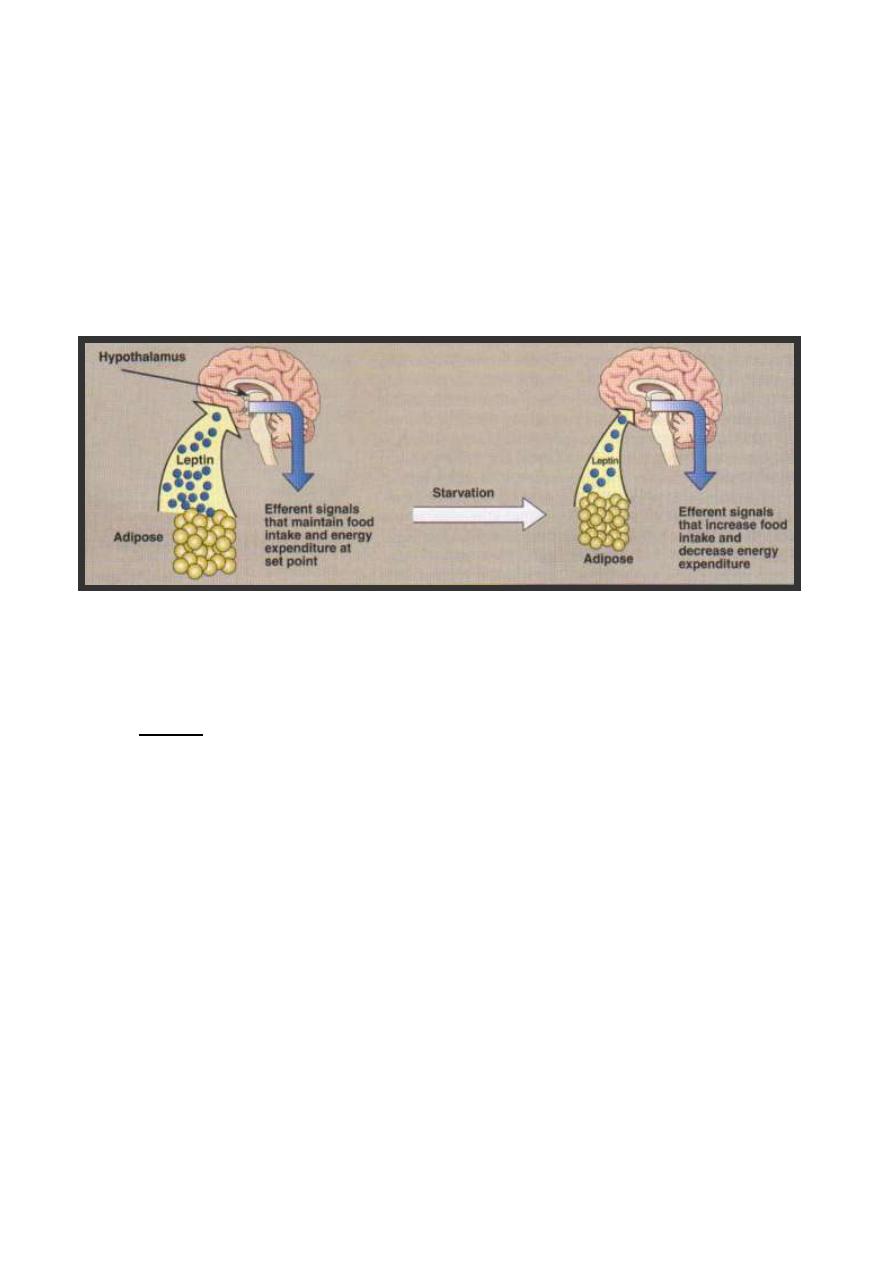
Leptin is produced proportionally to the adipose mass and, thus, informs the brain of
the fat store level. It is secreted by fat cells, and acts on the hypothalamus of the brain
to regulate the amount of body fat through the control of appetite and energy
expenditure. Leptin's secretion is suppressed by depletion of fat stores (starvation) and
enhanced by expansion of fat stores (well-fed state). Daily injection of leptin causes
overweight mice to lose weight and maintain weight loss. The protein also causes
weight loss in mice that are not obese. In humans, leptin increases the metabolic rate
and decreases appetite.
However, plasma leptin in obese humans is usually normal for their fat mass,
suggesting that resistance to leptin, rather than its deficiency, occurs in human obesity.
Other hormones released by adipose tissue, such as adiponectin and resistin, may
mediate insulin resistance observed in obesity
2. resistin
The hormone resistin is one amongst a novel family of three proteins , known as
resistin-like molecules (RELMs). They are cysteine-rich secreted proteins associated
with pulmonary inflammation (also known as FIZZ3, found in inflammatory zone). It has
11 cysteine-residues synthesized as a propeptide of 108 amino acids and secreted as
a dimmer, build by a disulfide bridge of cysteine residues. Beside this intermolecular
disulfide bridge, 5 additional intramolecular ones exist.
Source of reistin
In humans, resistin expression in adiposite can be detected at a low level. it is higher in
abdominal fat stores than in thigh adipose tissue, this suggest a potential role in linking
central obesity to type 2 diabetes and/or cardiovascular disease. Human resistin is
expressed mainly in pancreatic islet, preadiposites, macrophages and bone marrow. So
resistin is of relevance for inflammation processes as well as for lipid metabolism.

Prof. Dr.Hedef.D.El-Yassin
4
In mice a correlation between adiposity, insulin resistance and resistin expression was
found empirically. In humans respective studies are not clear. Several show an association
of resistin serum concentration and adiposity or insulin resistance.
Resistin putative role(s):
Relevance of resistin in physiological processes other than energy metabolism was
investigated. Experiments with endothelial cells gave interesting results, in which resistin
shown to be potentially able to influence endothelial inflammation and thereby
atherosclerosis.
Resistin shares some qualities with another protein secreted by fat cells and associated
with obesity, the hormone leptin. This hormone, discovered in 1995, seems to regulate
food intake.
There is still much to learn about resistin. But with each new piece fitted into the diabetes
puzzle, new possibilities arise.
There are two putative roles of resistin:
a. To directly cause insulin resistance
b. To block adipocyte differentiation
The latter might lead to ectopic fat storage (increased amounts of fat in skeletal
muscle and liver.
Future work….
Future research in this area aims to establish the role of resistin in human disease.
Measurement of resistin in a simple blood test might then be useful in detecting insulin
resistance and prediabetic conditions. Looking forward, counteracting resistin's affects on
the body might be a new approach to preventing and treating diabetes.

Prof. Dr.Hedef.D.El-Yassin
5
Hormones that regulate
calcium homeostasis
Calcium ions regulate a number of important physiological and biochemical process.
These include:
1. neuromuscular excitability
2. blood coagulation
3. secretory processes
4. membrane integrity and plasma membrane transport
5. enzyme reactions
6. the release of hormones and neurotransmitters
7. and the intracellular action of a number of hormones.
In addition the proper extracellular fluid and periosteal concentration of Ca
+2
and
PO
4
-3
are required for bone mineralization.
To ensure that these processes operate normally, the plasma Ca
+2
concentration is maintained within very narrow limits by the actions of the
following hormones:

Prof. Dr.Hedef.D.El-Yassin
6
1. Vitamin D
3
Vitamin D is a fat-soluble steroid hormone precursor that contributes to the
maintenance of normal levels of calcium and phosphorus in the bloodstream.
It is also known as calciferol. Vitamin D
3
is produced in the skin by
conversion of 7-dehydrocholesterol by UV.
Calciferol travels in the blood to the liver where it is converted into 25[OH]
Vitamin D
3
. This compound travels to the kidney where it is converted into
Calcitriol (1,25[OH]
2
Vitamin D
3
). This final step is promoted by the PTH.
Although called a vitamin, calciferol and its products fully qualify as hormones
because they are:
Made in certain cells
Carried in the blood
Affect gene transcription in target cells
Diseases
Vitamin D deficiency is known to cause several bone diseases, due to
insufficient calcium or phosphate in the bones:
Rickets: a childhood disease characterized by failure of growth and
deformity of long bones.
Osteoporosis: a condition characterized by fragile bones.
Osteomalacia: a bone-thinning disorder in adults that is characterised
by proximal muscle weakness and bone fragility. Osteomalacia can only
occur in a mature skeleton.

Prof. Dr.Hedef.D.El-Yassin
7
2. Calcitonin
Calcitonin is a hormone secreted from the parafolicular of C cells in the
thyroid gland, known to participate in calcium and phosphorus metabolism.
Calcitonin is a 32 amino acid peptide cleaved from a larger prohormone. It
contains a single disulfide bond, which causes the amino terminus to assume
the shape of a ring.
Physiologic Effects of Calcitonin
Calcitonin plays a role in calcium and phosphorus metabolism. In particular,
calcitonin has the ability to decrease blood calcium levels at least in part by
effects on two well-studied target organs:
Bone: Calcitonin suppresses resorption of bone by inhibiting the activity
of osteoclasts, a cell type that "digests" bone matrix, releasing calcium
and phosphorus into blood.
Kidney: Calcium and phosphorus are prevented from being lost in urine
by reabsorption in the kidney tubules. Calcitonin inhibits tubular
reabsorption of these two ions, leading to increased rates of their loss in
urine.
Control of Calcitonin Secretion
The most prominent factor controlling calcitonin secretion is the
extracellular concentration of ionized calcium. Elevated blood calcium
levels strongly stimulate calcitonin secretion, and secretion is suppressed
when calcium concentration falls below normal.
Disease States
A large number of diseases are associated with abnormally increased or
decreased levels of calcitonin, but pathologic effects of abnormal calcitonin
secretion per se are not generally recognized.

Prof. Dr.Hedef.D.El-Yassin
8
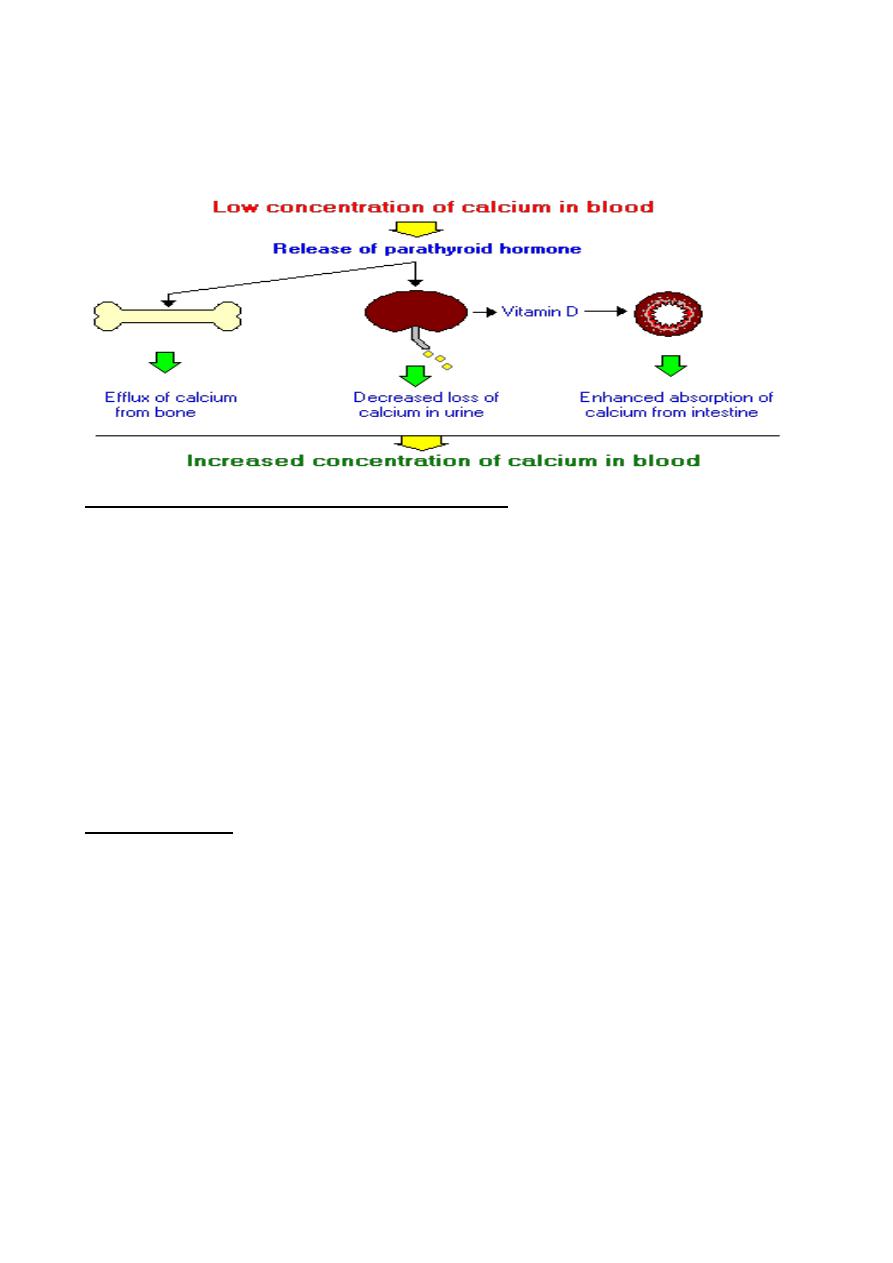
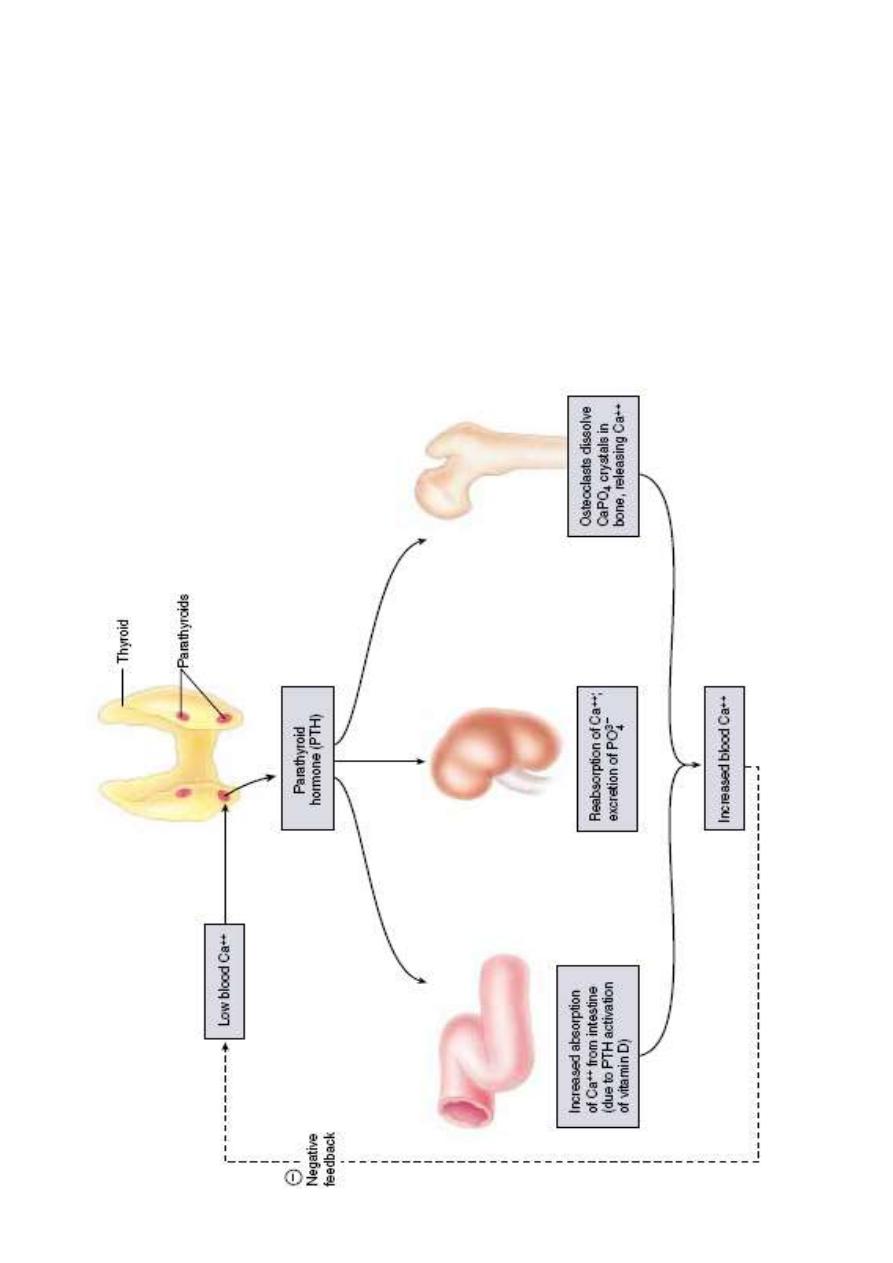
3. Parathyroid Hormone (PTH)
Parathyroid hormone is the most important endocrine regulator of
calcium and phosphorus concentration in extracellular fluid. This
hormone is secreted from cells of the parathyroid glands and finds its major
target cells in bone and kidney. Like most other protein hormones,
parathyroid hormone is synthesized as a preprohormone. After intracellular
processing, the mature hormone is packaged within the Golgi into secretory
vesicles, then secreted into blood by exocytosis. Parathyroid hormone is
secreted as a linear protein of 84 amino acids.
Physiologic Effects of Parathyroid Hormone
If calcium ion concentrations in extracellular fluid fall below normal,
PTH brings them back within the normal range. In conjunction with
increasing calcium concentration, the concentration of phosphate ion in blood
is reduced. Parathyroid hormone accomplishes its job by stimulating at least
three processes:
Mobilization of calcium from bone: Although the mechanisms remain
obscure, a well-documented effect of parathyroid hormone is to stimulate
osteoclasts to reabsorb bone mineral, liberating calcium into blood.
Enhancing absorption of calcium from the small intestine: Facilitating
calcium absorption from the small intestine would clearly serve to elevate
blood levels of calcium. Parathyroid hormone stimulates this process, but
indirectly by stimulating production of the active form of vitamin D in the
kidney. Vitamin D induces synthesis of a calcium-binding protein in
intestinal epithelial cells that facilitates efficient absorption of calcium into
blood.
Suppression of calcium loss in urine: In addition to stimulating fluxes of
calcium into blood from bone and intestine, parathyroid hormone puts a
brake on excretion of calcium in urine, thus conserving calcium in blood.
Prof. Dr.Hedef.D.El-Yassin
9
This effect is mediated by stimulating tubular reabsorption of calcium. Another
effect of parathyroid hormone on the kidney is to stimulate loss of phosphate
ions in urine.
Control of Parathyroid Hormone Secretion
Parathyroid hormone is released in response to low extracellular
concentrations of free calcium. Changes in blood phosphate concentration
can be associated with changes in parathyroid hormone secretion, but this
appears to be an indirect effect and phosphate per se is not a significant
regulator of this hormone.
When calcium concentrations fall below the normal range, there is a steep
increase in secretion of parathyroid hormone. Low levels of the hormone are
secreted even when blood calcium levels are high.
Disease States
Excessive secretion of parathyroid hormone is seen in two forms:
Primary hyperparathyroidism is the result of parathyroid gland
disease.
Secondary hyperparathyroidism is the situation where disease
outside of the parathyroid gland leads to excessive secretion of
parathyroid hormone. A common cause of this disorder is kidney
disease. It can also result from inadequate nutrition - for example, diets
Prof. Dr.Hedef.D.El-Yassin
11
that are deficient in calcium or vitamin D, or which contain excessive
phosphorus.
Inadequate production of parathyroid hormone - hypoparathyroidism -
typically results in decreased concentrations of calcium and increased
concentrations of phosphorus in blood. Common causes of this disorder
include surgical removal of the parathyroid glands and disease processes
that lead to destruction of parathyroid glands.
Prof. Dr.Hedef.D.El-Yassin
11
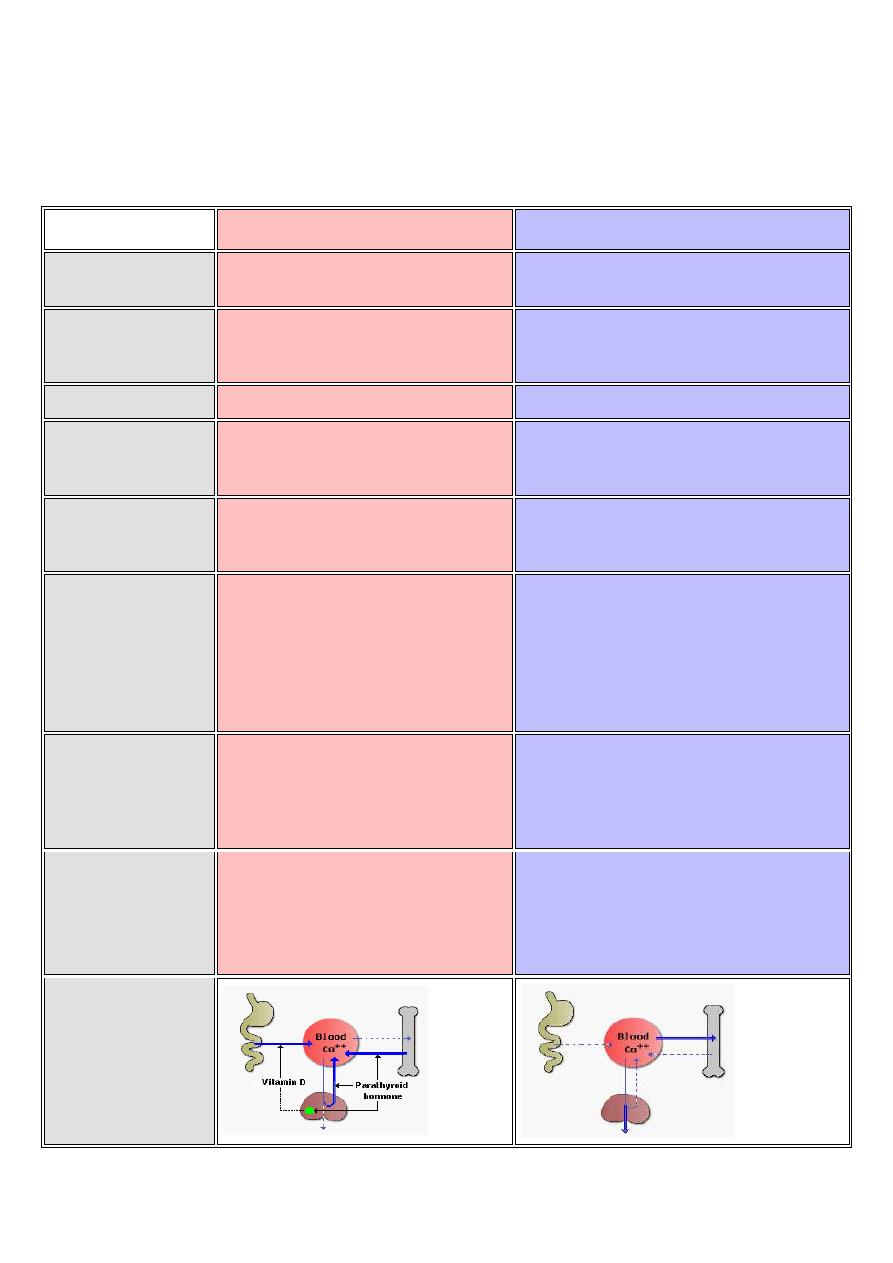
The following table summarizes body responses to conditions that would
otherwise lead to serious imbalances in calcium and phosphate levels in
blood
Calcium Deprivation
Calcium Loading
Parathyroid
hormone
Secretion stimulated
Secretion inhibited
Vitamin D
Production stimulated by increased
parathyroid hormone secretion
Synthesis suppressed due to low
parathyroid hormone secretion
Calcitonin
Very low level secretion
Secretion stimulated high blood calcium
Intestinal
absorption of
calcium
Enhanced due to activity of vitamin D
on intestinal epithelial cells
Low basal uptake
Release of calcium
and phosphate
from bone
Stimulated by increased parathyroid
hormone and vitamin D
Decreased due to low parathyroid hormone
and vitamin D
Renal excretion of
calcium
Decreased due to enhanced tubular
reabsorption stimulated by elevated
parathyroid hormone and vitamin D;
hypocalcemia also activates calcium
sensors in loop of Henle to directly
facilitate calcium reabsorption
Elevated due to decreased parathyroid
hormone-stimulated reabsorption.
Renal excretion of
phosphate
Strongly stimulated by parathyroid
hormone; this phosphaturic activity
prevents adverse effects of elevated
phosphate from bone resorption
Decreased due to hypoparathyroidism
General Response
Typically seen near normal serum
concentrations of calcium and
phosphate due to compensatory
mechanisms. Long term deprivation
leads to bone thining (osteopenia).
Low intestinal absorption and enhanced
renal excretion guard against development
of hypercalcemia.
Summary
