
Professor Dr. H.D.El-Yassin 2014
1
Biochemistry and
Disorders of
Hormones of the
Hypothalamic and
pituitary gland
(hypothalamus
and pituitary axis)
1. Hormones of the hypothalamus
Prof. Dr. Hedef Dhafir El-Yassin 2014
Professor Dr. H.D.El-Yassin 2014
2
Lecture 3
Objectives:
1. to describe the structure and function of the hypothalamus
2. to list the hormones secreted from the hypothalamus
3. to understand how the hypothalamus controls the secrection of hormones of
the pituitary gland.
1. Hormones of the hypothalamus
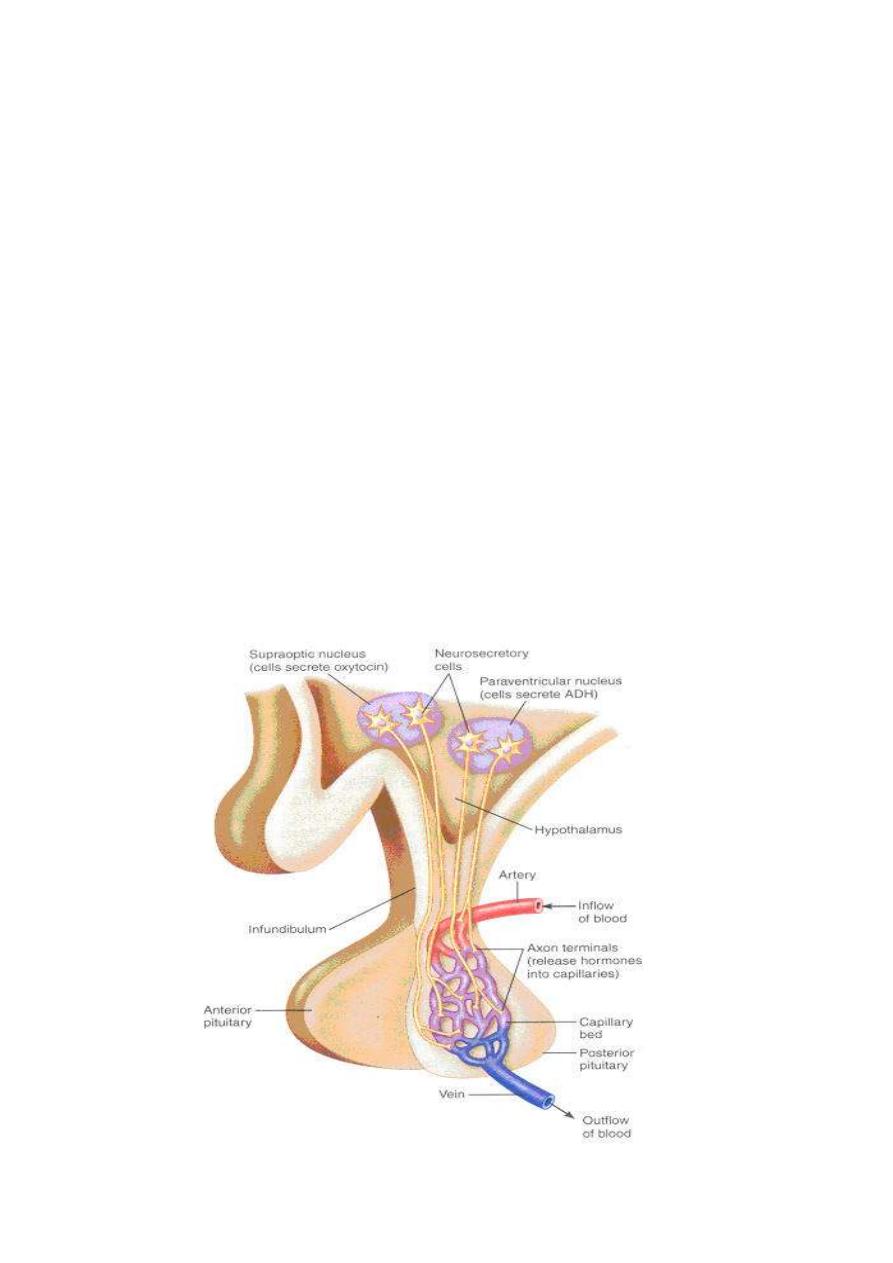
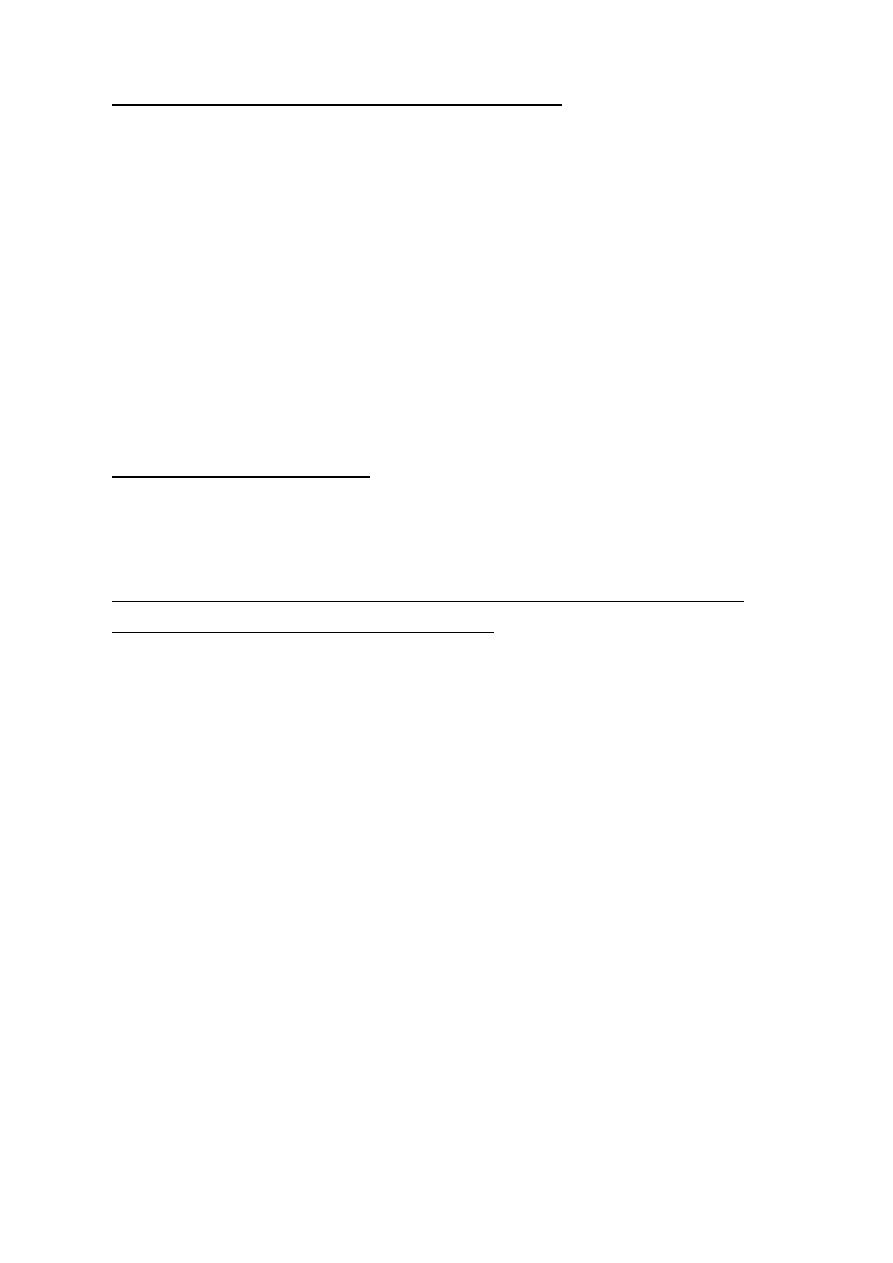
The hypothalamus is an integral part of the substance of the brain. A small cone-shaped
structure, it projects downward, ending in the pituitary stalk, a tubular connection to the
pituitary gland, which is a double lobed structure that produces the endocrine secretions
when stimulated by the hypothalamus.
Professor Dr. H.D.El-Yassin 2014
3
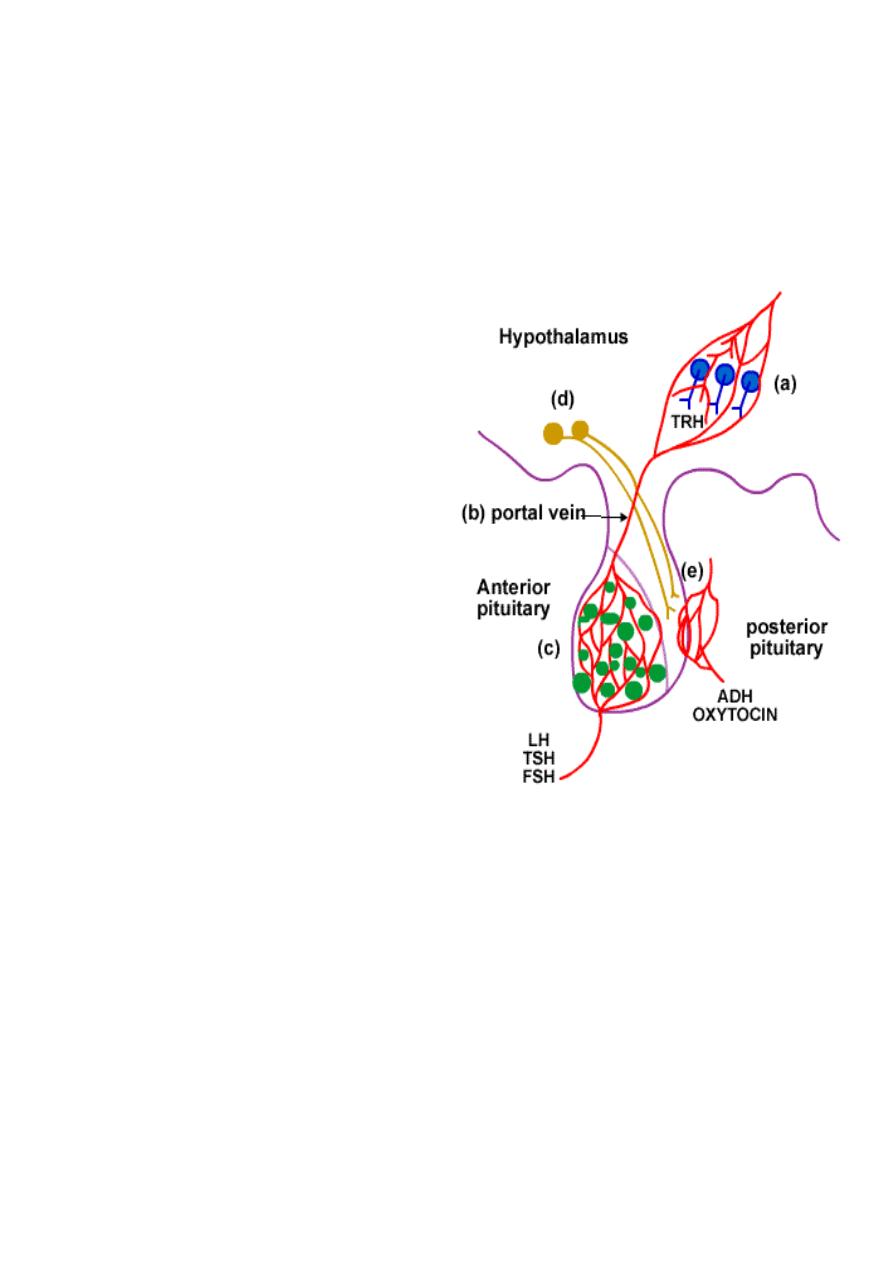
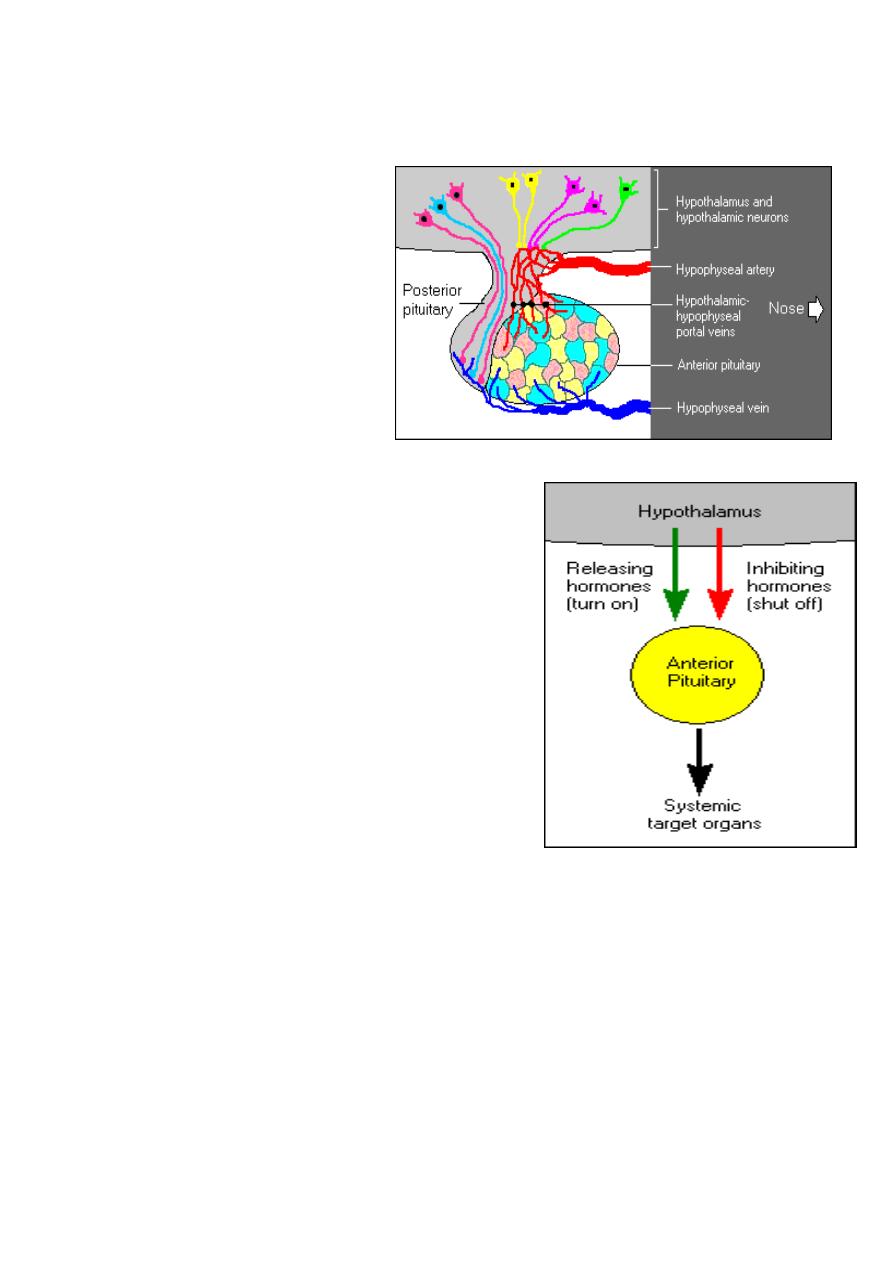
The hypothalamus controls each lobe of the pituitary slightly differently.
1. control of Anterior lobe
a. The hypothalamus acts as an endocrine gland.
b. Hormones are sent from the hypothalamus to the anterior pituitary via a
blood vessel called the portal vein.
c. The target tissue is the anterior lobe of the pituitary e.g. LH, TSH, and FSH.
2. control of the Posterior lobe
d. Neuro-hormones are
synthesized in the
hypothalamus neurons.
They are transported and
stored in vesicles in the
axon ending located in the
posterior pituitary.
e. Nerve impulses travel down
the axon into the posterior
pituitary. This causes the
release of the vesicles of
hormones into the blood
stream at the posterior
pituitary e.g. oxytocin , and
ADH.
Professor Dr. H.D.El-Yassin 2014
4
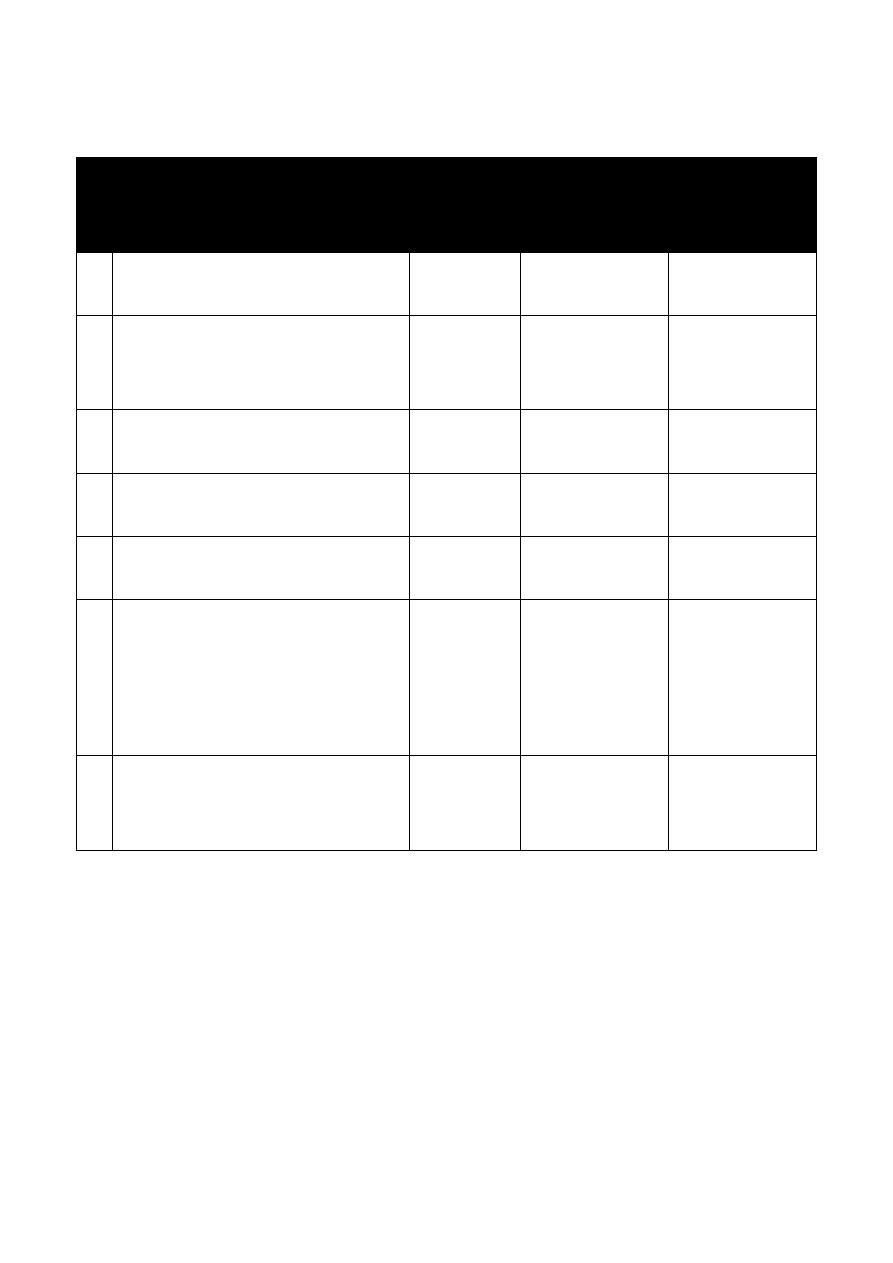
Many hormonal systems involve hypothalamus.
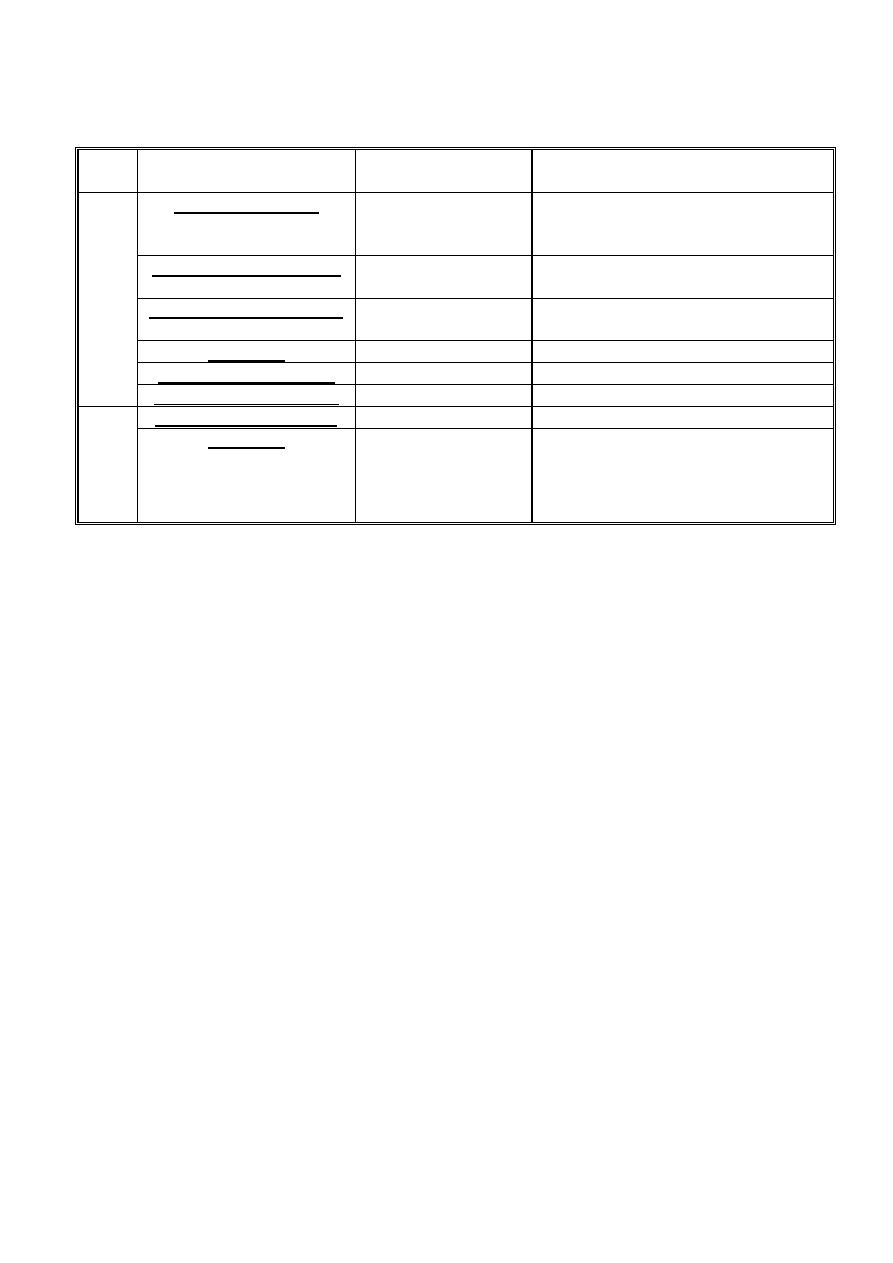
Table: Hypothalamic hypophysial-target gland hormones form integrated feedback loops
Hypothalamic hormones
No. of A.A
in structure
Pituitary
Hormone
Affected
1
Target Gland
Hormone
Affected
1
Thyrotropin-releasing hormone
(TRH)
3
TSH (PRL)
T
3
, T
4
2
Gonadotropin-releasing
hormone (GnRH)
10
LH, FSH
Androgens,
estrogens,
progestins
3
Corticotropin-releasing
hormone (CRH)
41
ACTH
Cortisol
4
Growth hormone-releasing
hormone(GHRH or GRH)
49
GH
IGF-1
5
Prolactin release factor
Not
established
PRL
neurohormones
6
Somatostatin (Growth hormone
release-inhibiting hormone;
somatotropin release-inhibiting
hormone (GHRIH or SRIH)
14
GH (TSH, FSH,
ACTH)
IGK-1; T
3
andT
4
7
Prolactin- release-inhibiting
hormones (Dopamine and GAP)
(PRIH or PIH)
PRL
neurohormones
1
The hypothalamic hormone has a secondary or lesser effect on the hormones in parentheses.
Professor Dr. H.D.El-Yassin 2014
5
1) Thyrotropin-releasing hormone(TRH)
Is the simplest of the hypothalamic neuropeptides. It consists essentially of three amino
acids. Its basic sequence is glutamic acid-histidine-proline, The simplicity of this structure
is deceiving for TRH is involved in an extraordinary array of functions. Some of which are:
a. It stimulates the secretion of thyroid-stimulating hormone from the pituitary.
b. It also affects the secretion of prolactin from the pituitary.
The TRH-secreting cells are subject to stimulatory and inhibitory influences from higher
centers in the brain and they also are inhibited by circulating thyroid hormone.
2) Gonadotropin-releasing hormone (GnRH)
Also known as luteinizing hormone-releasing hormone (LHRH), is a peptide chain of 10
amino acids. It stimulates the synthesis and release of the two pituitary gonadotropins,
luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
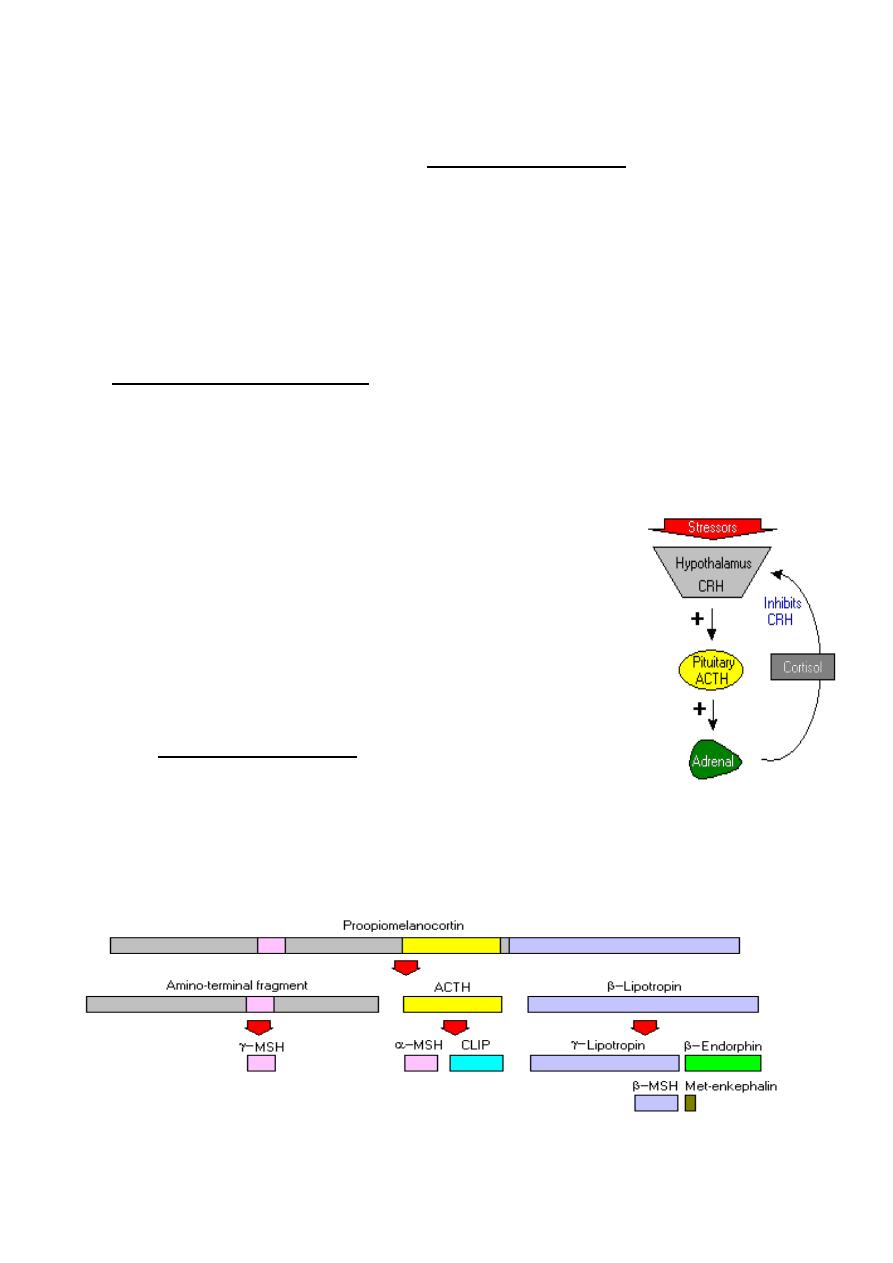
3) Corticotropin-releasing hormone (CRH)
Is a large peptide consisting of a single chain of 41 amino acids. It stimulates not only
secretion of corticotropin in the pituitary gland but also the synthesis of corticotropin in the
corticotropin-producing cells (corticotrophs) of the anterior lobe of the pituitary gland. Many
factors, both neurogenic and hormonal, regulate the secretion of CRH. Among the
hormones that play an important role in modulating the influence of CRH is cortisol, the
major hormone secreted by the adrenal cortex, which, as part of the negative feedback
mechanism. Vasopressin, the major regulator of the body's excretion of water, has an
additional ancillary role in stimulating the secretion of CRH.
Excessive secretion of CRH leads to an increase in the size and number of corticotrophs
in the pituitary gland, often resulting in a pituitary tumor. This, in turn, leads to excessive
stimulation of the adrenal cortex, resulting in high circulating levels of adrenocortical
hormones, the clinical manifestations of which are known as Cushing's syndrome.
Conversely, a deficiency of CRH-producing cells can, by a lack of stimulation of the
pituitary and adrenal cortical cells, result in adrenocortical deficiency.
Professor Dr. H.D.El-Yassin 2014
6
4) Growth hormone-releasing hormone (GHRH or GRH)
Like CRH, growth hormone-releasing hormone (GHRH) is a large peptide. A number of
forms have been described that differ from one another only in minor details and in the
number of amino acids (varying from 37 to 49). It is stimulated by stresses, including
physical exercise, and secretion is blocked by a powerful inhibitor called somatostatin.
Negative feedback control of GHRH secretion is mediated largely through compounds
called somatomedins, growth-promoting hormones that are generated when tissues are
exposed to growth hormone itself.
Isolated deficiency of GHRH (in which there is normal functioning of the hypothalamus
except for this deficiency) may be the cause of one form of dwarfism, a general term
applied to all individuals with abnormally small stature.
5) Prolactin release factor (PRF):
Appears to be released from the hypothalamus in a pulsatile fashion and it is the
fluctuation in PRF that regulates the circulating level of prolactin.
6) Somatostatin (Growth hormone release-inhibiting hormone; somatotropin
release-inhibiting hormone ( GHRIH or SRIH)
Somatostatin refers to a number of polypeptides consisting of chains of 14 to 28 amino
acids. Somatostatin is also a powerful inhibitor of pituitary TSH secretion. Somatostatin,
like TRH, is widely distributed in the central nervous system and in other tissues. It serves
an important paracrine function in the islets of Langerhans, by blocking the secretion of
both insulin and glucagon from adjacent cells. Somatostatin has emerged not only as a
powerful blocker of the secretion of GH, insulin, glucagon, and other hormones but also as
a potent inhibitor of many functions of the gastrointestinal tract, including the secretion of
stomach acid, the secretion of pancreatic enzymes, and the process of intestinal
absorption.

Professor Dr. H.D.El-Yassin 2014
7
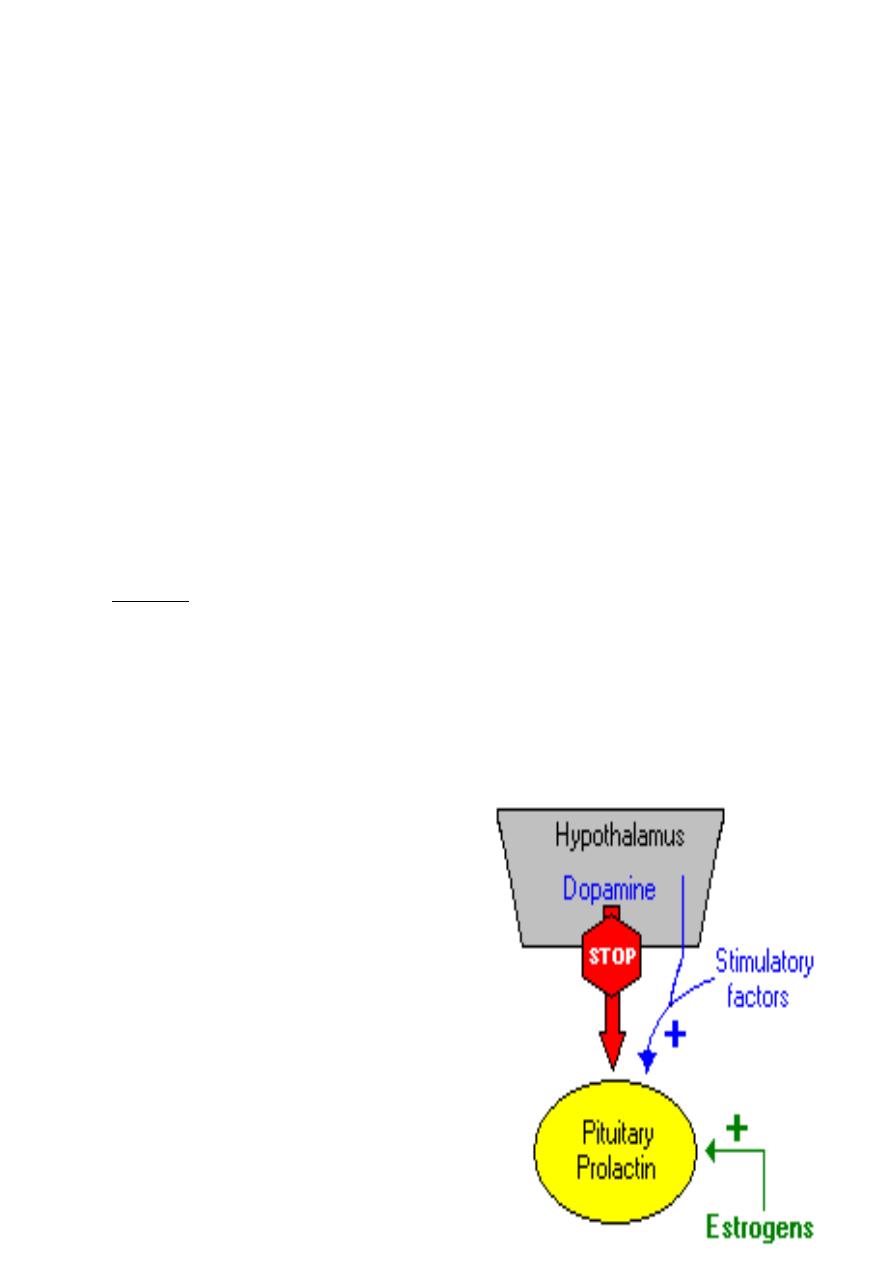
7) Prolactin release-inhibiting hormones (Dopamine and GAP)
GAP= GnRH-associated peptide
The hypothalamic regulation of prolactin secretion from the pituitary is different from the
hypothalamic regulation of other pituitary hormones in two respects:
1. First, the hypothalamus primarily inhibits rather than stimulates the release of
prolactin from the pituitary.
2. Second, this major inhibiting factor is not a neuropeptide, but rather the
neurotransmitter dopamine. Prolactin deficiency is known to occur, but only rarely.
Excessive prolactin production (hyperprolactinemia) is a common endocrine
abnormality.
Quick quiz 1:
which of the following statement is incorrect for hypothalamus?
1. it releases the hormones which regulate the secretion of anterior pituitary gland
2. hypothalamic hormones are absent from the tissues
3. the higher brain enters are necessary to control their secretion
4. the prolactin has no release hormone but has release inhibiting hormone
Quick quiz 2:
one of the following hormones is synthesized in the hypothalamus but
not secreted from it:
1. vasspressin
2. MSH
3. prolactin
4. serotonin
Conclusion
1. The hypothalamus is a small cone-shaped structure, part of the brain, it projects
downward, ending in the pituitary stalk.
2. The pituitary gland, a roundish organ that lies immediately beneath the
hypothalamus composed of two distinctive parts:
a. The anterior pituitary (adenohypophysis).
b. The posterior pituitary (neurohypophysis)
3. The hypothalamus controls the secrection of hormones from each lobe of the
pituitary slightly differently

Professor Dr. H.D.El-Yassin 2014
8
Biochemistry and
Disorders of
Hormones of the
Hypothalamic and
pituitary gland
(hypothalamus
and pituitary axis
2. Hormones of the pituitary gland
Prof. Dr. Hedef Dhafir El-Yassin 2013

Professor Dr. H.D.El-Yassin 2014
9
Lecture 4
Objectives:
1. to list the hormones secreted from the pituitary gland
2. state the peripheral effects of hormone release for each hormone synthesized
or stored in the pituitary gland
3. to state the peripheral effects of increased and decreased hormone release
for each hormone synthesized or stored in the pituitary gland.
At the end of this lecture you will be able to discus the following case scenario
(case 1): A 32-year-old male was seen in the emergency department
yesterday after suffering a concussion and head trauma from a motor vehicle
accident. The patient was stabilized in the emergency department and
transferred to the intensive care unit (ICU) for observation. The patient had
computed tomography (CT) scan of the head that revealed a small amount of
cerebral edema but was otherwise normal. During the second day in the ICU,
the nurse informs the physician that the patient has had a large amount of
urine output in the last 24 hours.
The nursing records report his urine output over the last 24 hours was 6400
cc.
He has been given no diuretic medications. A urine osmolality was ordered
and was found to be low. His physician remarks that the kidneys are not
concentrating urine normally. He was diagnosed as having diabetes insipidus.
1. What is the biochemical mediator (hormone) that is responsible for this
disorder?
2. From where is this hormone secreted?
3. What are the other hormone(s) secreted from this gland?
4. What is the control of secretion of this hormone
5. What is( are) the clinical biochemical test(s) used for diagnosis.
Professor Dr. H.D.El-Yassin 2014
10
Hormones of the Pituitary gland
The pituitary gland, also known as
the hypophysis, is a roundish organ
that lies immediately beneath the
hypothalamus.
Careful examination of the pituitary
gland reveals that it composed of
two distinctive parts:
1. The
anterior pituitary
(adenohypophysis) is a
classical gland composed
predominantly of cells that secrete protein
hormones.
2. The
posterior pituitary
(neurohypophysis) is not
really an organ, but an extension of the
hypothalamus. It is composed largely of the axons
of hypothalamic neurons which extend downward
as a large bundle behind the anterior pituitary.
The target cells for most of the hormones produced in
these tissues are themselves endocrine cells.
The pituitary gland is often called the "master gland"
of the body. The anterior and posterior pituitary secretes
a number of hormones that collectively influence all cells
and affect virtually all physiologic processes.
Professor Dr. H.D.El-Yassin 2014
11
Table: The major hormones synthesized and secreted by the pituitary gland, along
with summary statements about their major target organs and physiologic effects.
Hormone
Major target
organ(s)
Major Physiologic Effects
Anteri
or
Pitui
tary
Growth hormone
Liver, adipose
tissue
Promotes growth (indirectly),
control of protein, lipid and
carbohydrate metabolism
Thyroid-stimulating h.
Thyroid gland
Stimulates secretion of thyroid
hormones
Adrenocorticotropic h. Adrenal gland
(cortex)
Stimulates secretion of
glucocorticoids
Prolactin
Mammary gland
Milk production
Luteinizing hormone
Ovary and testis
Control of reproductive function
Follicle-stimulating h.
Ovary and testis
Control of reproductive function
Pos
teri
or
Pitui
tary
Antidiuretic hormone
Kidney
Conservation of body water
Oxytocin
Ovary and testis
Stimulates milk ejection and uterine
contractions
As seen in the table above, the anterior pituitary synthesizes and secreted six major
hormones. Individual cells within the anterior pituitary secrete a single hormone (or
possibly two in some cases). Thus, the anterior pituitary contains at least six distinctive
endocrinocytes
The cells that secrete thyroid-stimulating hormone do not also secrete growth hormone,
and they have receptors for thyroid-releasing hormone, not growth hormone-releasing
hormone.
Hormonal cascade of signals from CNS to ultimate hormone.
The target "gland" is the last hormone-producing tissue in the cascade, which is stimulated
by an appropriate anterior pituitary hormone. Examples are thyroid gland, adrenal cortex,
ovary and testes. Ultimate hormone feedback negatively on sites producing intermediate
hormones in the cascade. Amounts (nanogram (ng), microgram (µg), and milligram (mg)
represent approximate quantities of hormone released
Professor Dr. H.D.El-Yassin 2014
12
Posterior Pituitary Hormones
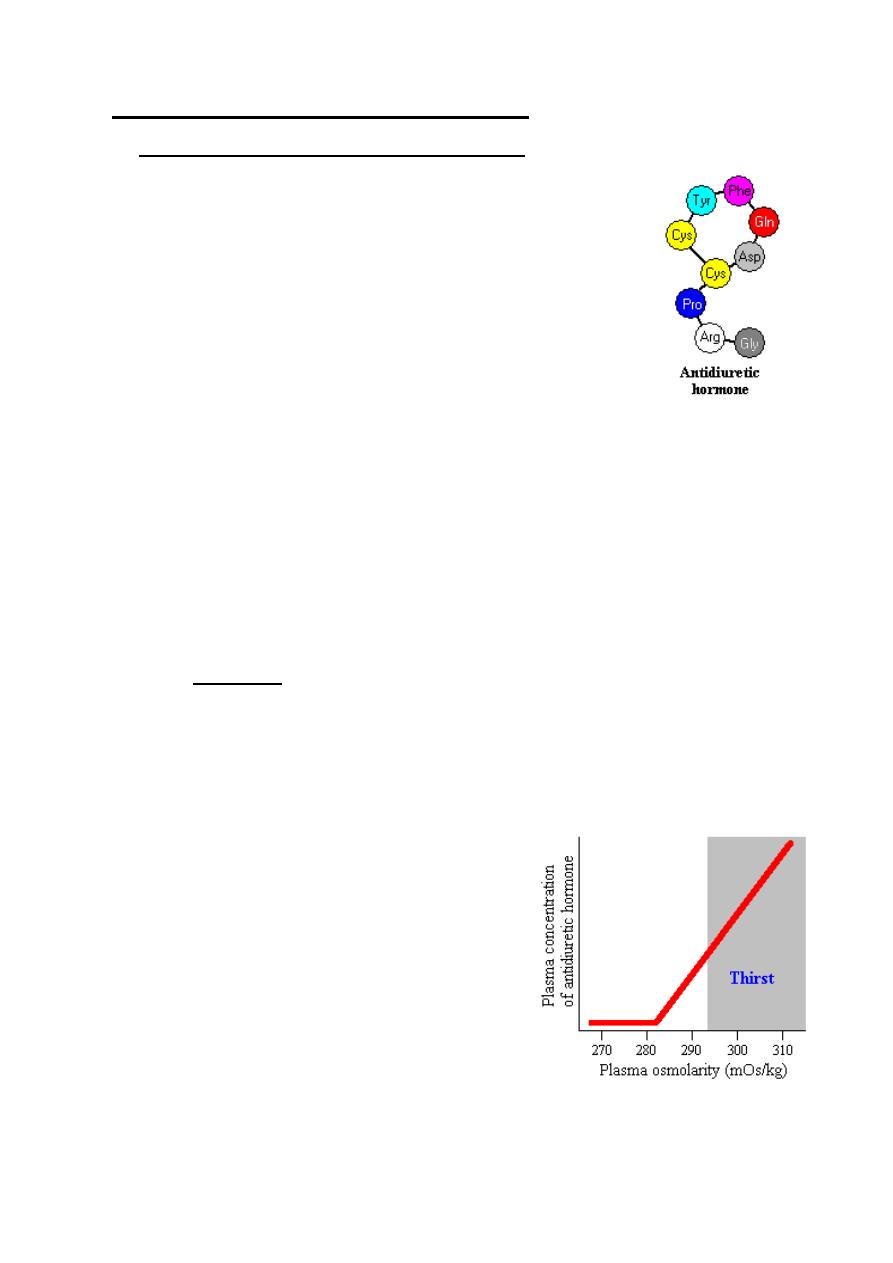
1. Antidiuretic Hormone (Arginine Vasopressin)
Roughly, 60% of the mass of the body is water, and despite wide
variation in the amount of water taken in each day, body water
content remains incredibly stable. Such precise control of body
water and solute concentrations is a function of several hormones
acting on both the kidneys and vascular system, but there is no doubt
that antidiuretic hormone is a key player in this process.
Antidiuretic hormone, also known as vasopressin, is a nine
amino acid peptide secreted from the posterior pituitary. The
single most important effect of antidiuretic hormone is to conserve body water by reducing
the output of urine
Effects of Antidiuretic Hormone
1.
stimulates contraction of the muscles of the capillaries and arterioles, raising
blood pressure
2.
promotes contraction of the intestinal musculature , increasing peristalsis
3.
stimulates water reabsorbtion by stimulating insertion of "water channels" or
aquaporins into the membranes of kidney tubules. These channels transport
solute-free water through tubular cells and back into blood, leading to a
decrease in plasma osmolarity and an increase osmolarity of urine.
Control of Antidiuretic Hormone Secretion
1. The most important variable regulating
antidiuretic hormone secretion is plasma
osmolarity, or the concentration of solutes in
blood. When plasma osmolarity is below a
certain threshold, the osmoreceptors are not
activated and antidiuretic hormone secretion is
suppressed. When osmolarity increases above
the threshold, the ever-alert osmoreceptors
recognize this and stimulate the neurons that
secrete antidiuretic hormone. As seen the figure, antidiuretic hormone
concentrations rise steeply and linearly with increasing plasma osmolarity.

Professor Dr. H.D.El-Yassin 2014
13
2. Secretion of antidiuretic hormone is also simulated by decreases in blood
pressure and volume, conditions sensed by stretch receptors in the heart and
large arteries. Changes in blood pressure and volume are not nearly as sensitive a
stimulator as increased osmolarity, but are nonetheless potent in severe conditions.
For example, Loss of 15 or 20% of blood volume by hemorrhage results in massive
secretion of antidiuretic hormone.
Another potent stimulus of antidiuretic hormone is nausea and vomiting.
Disease States
The most common disease of man and animals related to antidiuretic hormone is diabetes
insipidus. This condition can arise from either of two situations:
Hypothalamic ("central") diabetes insipidus
results from a deficiency in
secretion of antidiuretic hormone from the posterior pituitary. Causes of this disease
include head trauma, and infections or tumors involving the hypothalamus.
Nephrogenic diabetes insipidus
occurs when the kidney is unable to respond to
antidiuretic hormone. Most commonly, this results from some type of renal disease,
but mutations in the ADH receptor gene or in the gene encoding aquaporin-2 have
also been demonstrated in affected humans.
The major sign of either type of diabetes insipidus is excessive urine production.
Some human patients produce as much as 16 liters of urine per day! If adequate water is
available for consumption, the disease is rarely life-threatening, but withholding water can
be very dangerous.
To confirm diagnosis of diabetes isipidus:
1. Urine (S.G.)- Normal urine (S.G.) is between 1.015-1.025
If low:
a. Diabetes insipidus
b. Glomerular nephritis
c. Tubular damage
2.
Water deprivation test
helps determine whether diabetes insipidus is caused by one
of the following:
a. Excessive intake of fluid
b. A defect in ADH production
c. A defect in the kidneys' response to ADH
This test measures changes in body weight, urine output, and urine composition when
fluids are withheld.
Professor Dr. H.D.El-Yassin 2014
14
2. Plasma vasopressin at end of water deprivation test:
a. Low for plasma osmolality (central)
b. Normal for plasma osmolality (nephrogenic)
Quick quiz: Increased reabsorption of water from the kidney is the major consequence o
which of the following hormones?
1. cortisol
2. insulin
3. vasopressin
4. glucagons
Quick quiz syndrome of inappropriate secretion of ADH (SIADH) is caused by:
1. malignant disease of lung/prostate
2. chest disease like pneumonia and TB
3. brain tumors and meningitis
4. all the above
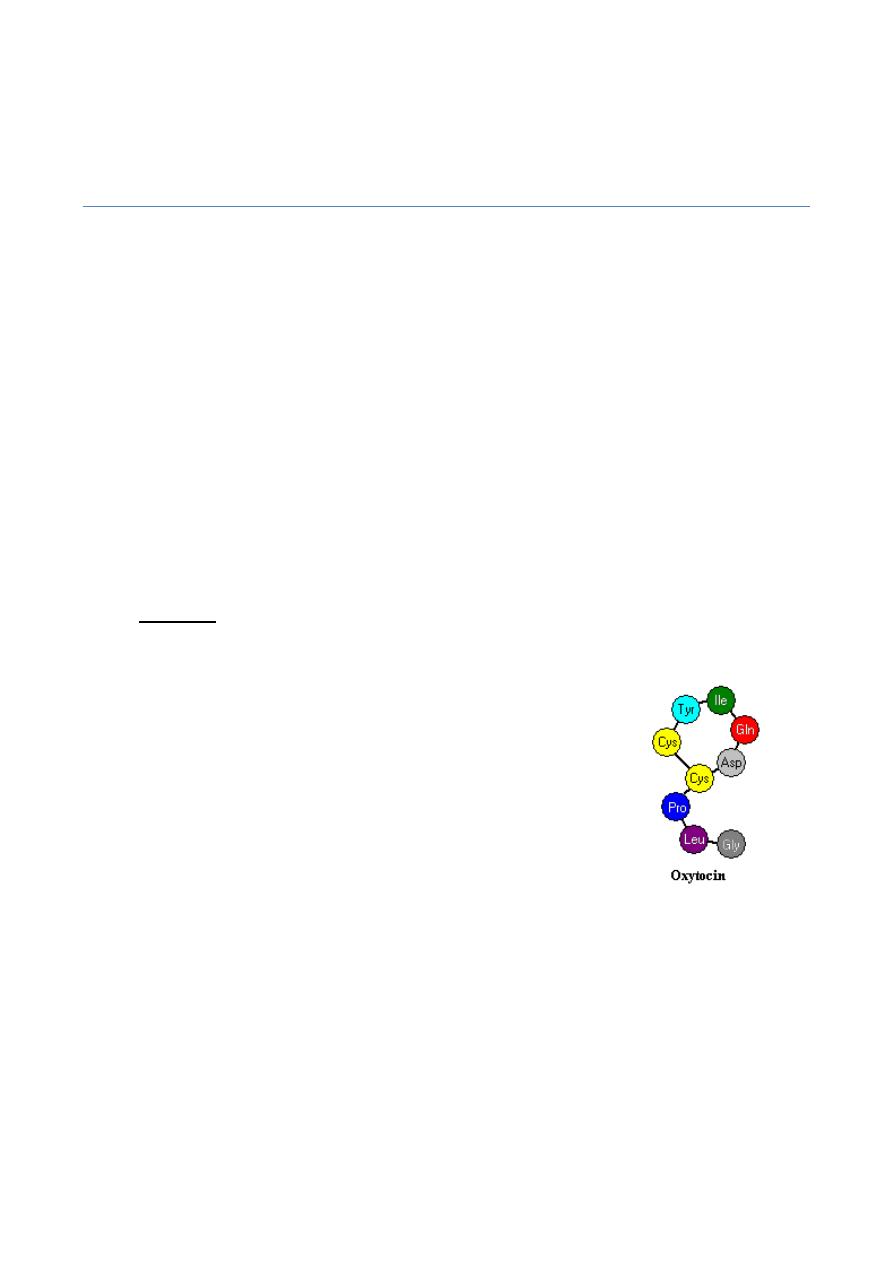
2. Oxytocin
Oxytocin in a nine amino acid peptide that is synthesized in hypothalamic neurons and
transported down axons of the posterior pituitary for secretion into
blood. Oxytocin differs from antidiuretic hormone in two of the nine
amino acids. Both hormones are packaged into granules and
secreted along with carrier proteins called neurophysins.
Control of Oxytocin Secretion
A number of factors can inhibit oxytocin release, among them acute
stress. For example, oxytocin neurons are repressed by
catecholamines, which are released from the adrenal gland in response to many types of
stress, including fright.
Quick quiz true or false
Oxytocin stimulates synthesis of steroids in ovary
Professor Dr. H.D.El-Yassin 2014
15
Overview of anterior pituitary hormones with hypothalamic releasing
hormones and their actions
Anterior Pituitary Hormones
Case (2):
A 36-year-
old male comes into the physician’s office because his
hands and feet are “swelling,” and his face has coarse features with oily skin.
On examination, he was noted to have some coarse facial features including
large nose, large tongue, and frontal bossing of his forehead. His hands are
enlarged with soft tissue swelling, and his heel pad is thickened. He is noticed
to have a slightly enlarged liver and spleen. The remainder of the examination
was otherwise normal. He was diagnosed as having acromagaly.
1. What is the biochemical mechanism of this disorder?
2. From where is this hormone secreted?
3. what is the control of secretion of this hormone?
4. What is( are) the clinical biochemical test(s) used for diagnosis.
Growth hormone, also known as somatotropin, is a
protein hormone of about 191 amino acids and two
intramoleculare disulfide bridges. that is synthesized and
secreted by cells called somatotrophs in the anterior
pituitary.
During daytime, its plasma concentration in health adult
remain relatively low (<2 g/ml) with several secoratory
spikes occurring after meals or exercise.
However it shows a marked rise in the evening in both
adults and children and reach a peak value during the
period of deepest sleeps.
It is a major participant in control of several complex physiologic processes, including
growth and metabolism. Growth hormone is also of considerable interest as a drug used in
both humans and animals.
Professor Dr. H.D.El-Yassin 2014
16
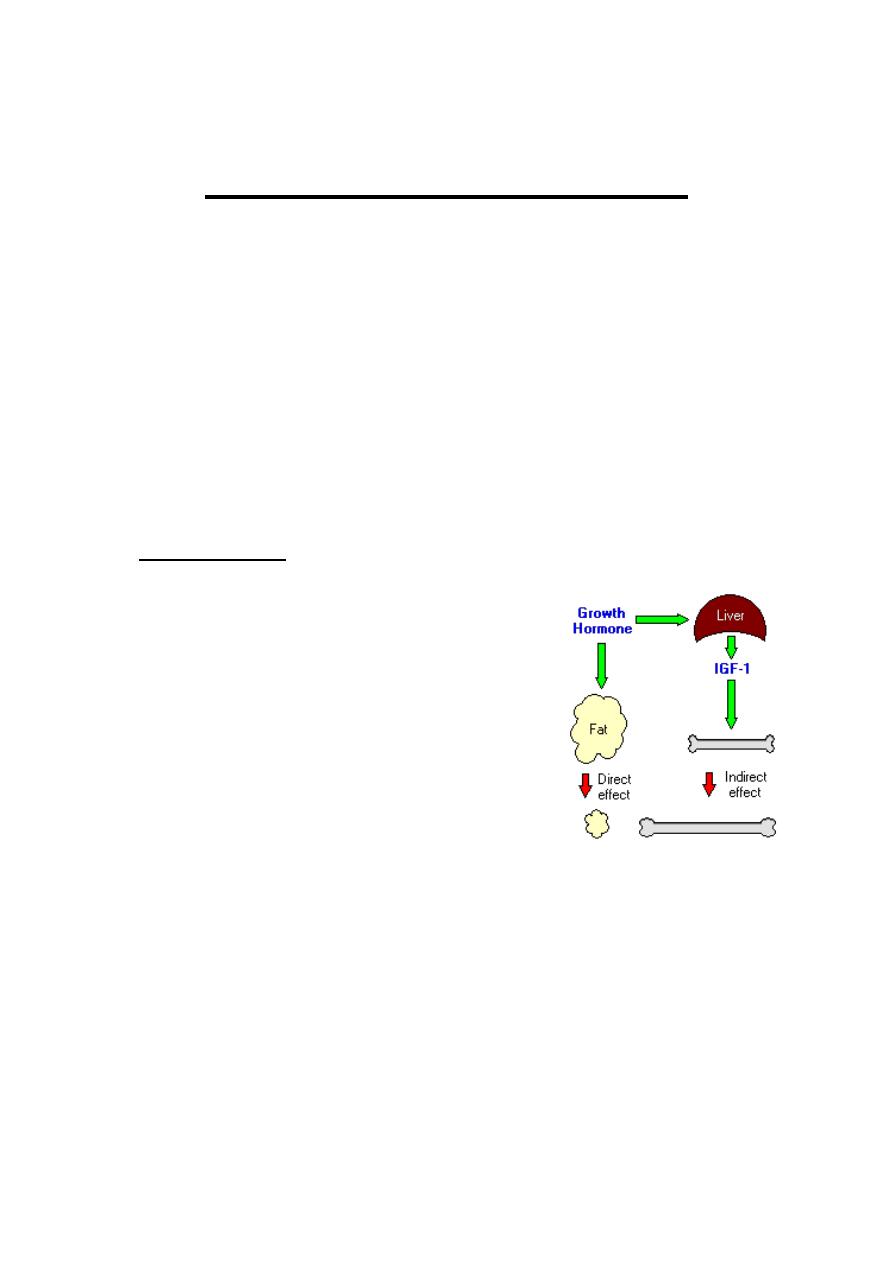
Physiologic Effects of Growth Hormone
A critical concept in understanding growth hormone activity is that it has two distinct types
of effects:
Direct effects
are the result of growth hormone binding its receptor on target cells.
Fat cells (adipocytes), for example, have growth hormone receptors, and growth
hormone stimulates them to break down triglyceride and suppresses their ability to
take up and accumulate circulating lipids.
Indirect effects
are mediated primarily by a insulin-like growth factor-1 (IGF-1), a
hormone that is secreted from the liver and other tissues in response to growth hormone.
A majority of the growth promoting effects of growth hormone is actually due to IGF-1
acting on its target cells. IGF-1 also appears to be the key player in muscle growth. It
stimulates amino acid uptake and protein synthesis in muscle and other tissues.
Metabolic Effects
Protein metabolism: In general, growth hormone stimulates protein anabolism in
many tissues. This effect reflects increased amino acid uptake, increased protein
synthesis and decreased oxidation of proteins.
Fat metabolism: Growth hormone enhances the utilization of fat by stimulating
triglyceride breakdown and oxidation in adipocytes.
Carbohydrate metabolism: Growth hormone is one of a battery of hormones that
serves to maintain blood glucose within a normal range. Growth hormone is often
said to have anti-insulin activity, because it suppresses the abilities of insulin to
stimulate uptake of glucose in peripheral tissues
and enhance glucose synthesis in the liver.
Mineral metabolism: promotes a positive
calcium, magnesium and phosphate balance
and causes the retention of Na
+
, K
+
and Cl
-
.
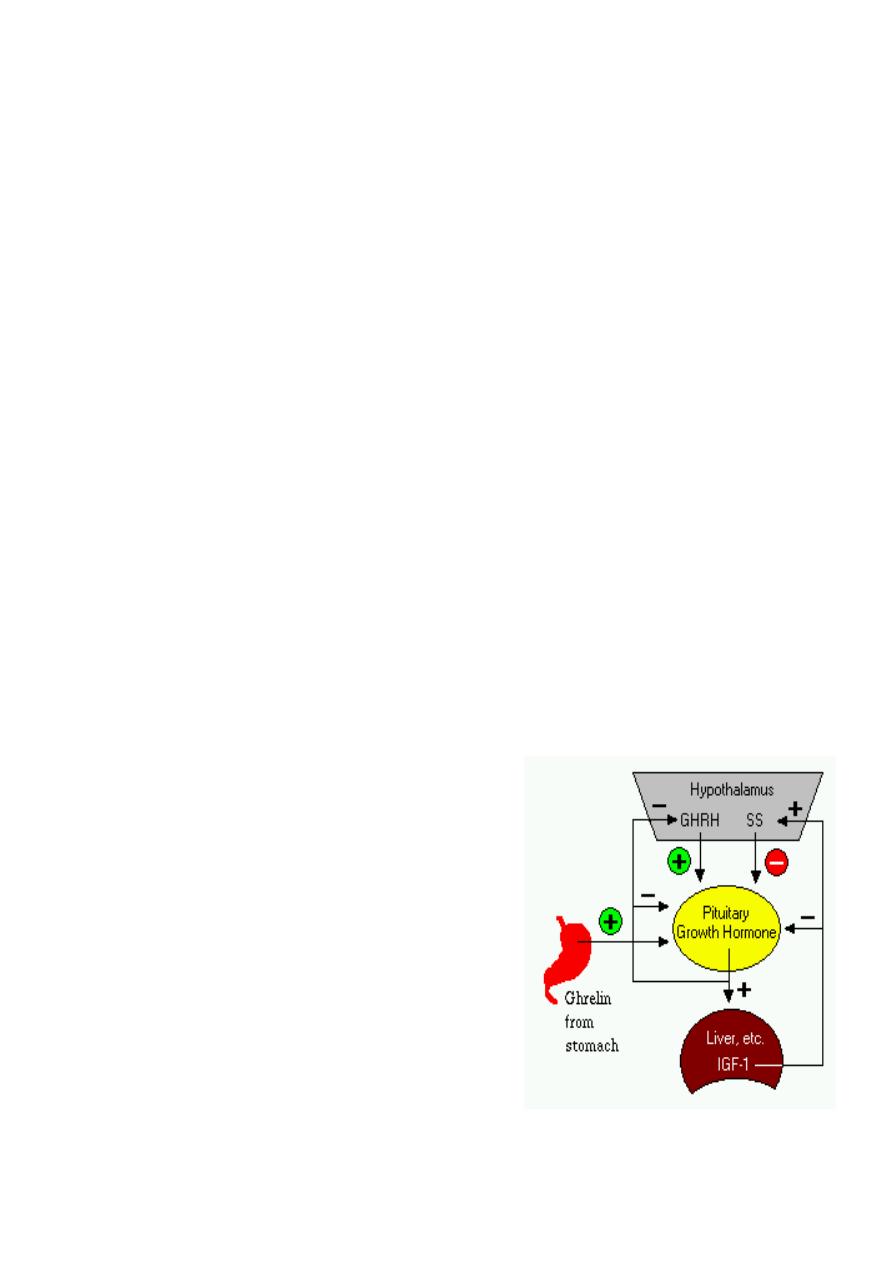
Control of Growth Hormone Secretion
Production of growth hormone is modulated by many
factors, including stress, exercise, nutrition, sleep and
growth hormone itself. However, its primary controllers
are two hypothalamic hormones and one hormone
from the stomach:

Professor Dr. H.D.El-Yassin 2014
17
Growth hormone-releasing hormone (GHRH) is a hypothalamic peptide that
stimulates both the synthesis and secretion of growth hormone.
Somatostatin (SS) is a peptide produced by several tissues in the body, including
the hypothalamus. Somatostatin inhibits growth hormone release in response to
GHRH and to other stimulatory factors such as low blood glucose concentration.
Ghrelin is a peptide hormone secreted from the stomach. Ghrelin binds to
receptors on somatotrophs and potently stimulates secretion of growth hormone.
Growth hormone secretion is also part of a negative feedback loop involving IGF-1.
High blood levels of IGF-1 lead to decreased secretion of growth hormone not only by
directly suppressing the somatotroph, but by stimulating release of somatostatin from the
hypothalamus.
Growth hormone also feeds back to inhibit GHRH secretion and probably has a direct
(autocrine) inhibitory effect on secretion from the somatotroph.
Integration of all the factors that affect growth hormone synthesis and secretion lead to a
pulsatile pattern of release. In children and young adults, the most intense period of growth
hormone release is shortly after the onset of deep sleep.
Disease States
A deficiency state can result not only from a deficiency in production of the hormone, but in
the target cell's response to the hormone.
Clinically, deficiency in growth hormone or receptor defects are known as growth
retardation or dwarfism. The manifestation of growth hormone deficiency depends upon
the age of onset of the disorder and can result from either heritable or acquired disease.
The effect of excessive secretion of growth hormone is also very dependent on the age of
onset and is seen as two distinctive disorders:
Gigantism is the result of excessive growth hormone secretion that begins in young
children or adolescents. It is a very rare disorder, usually resulting from a tumor of
somatotropes.
Acromegaly results from excessive secretion of growth hormone in adults. The excessive
growth hormone and IGF-1 also lead to metabolic derangements, including glucose
intolerance.
Professor Dr. H.D.El-Yassin 2014
18
Lab tests to confirm diagnosis:
Random growth hormone is not helpful.
GH is usually decreased with glucose. A standard 75g oral glucose tolerance test
must be performed and measurement of GH at 0, 30, 60, 90, and 120min must be
applied.
If GH failed to be suppressed then the diagnosis of acromagaly is confirmed.
The vast majority (99%) of cases of acromagaly are due to pituitary tumors. If a
pituitary tumor is not seen on MRI scanning yet acromagaly is confirmed, a GHRH
level should be requested to exclude ectopic production of this polypeptide by non-
pituitary tumors stimulating the release of growth hormone from the pituitary.
Quick quiz: Which of the following does not influence GH production?
1. Diet
2. Stress
3. Sleep
4. exercise
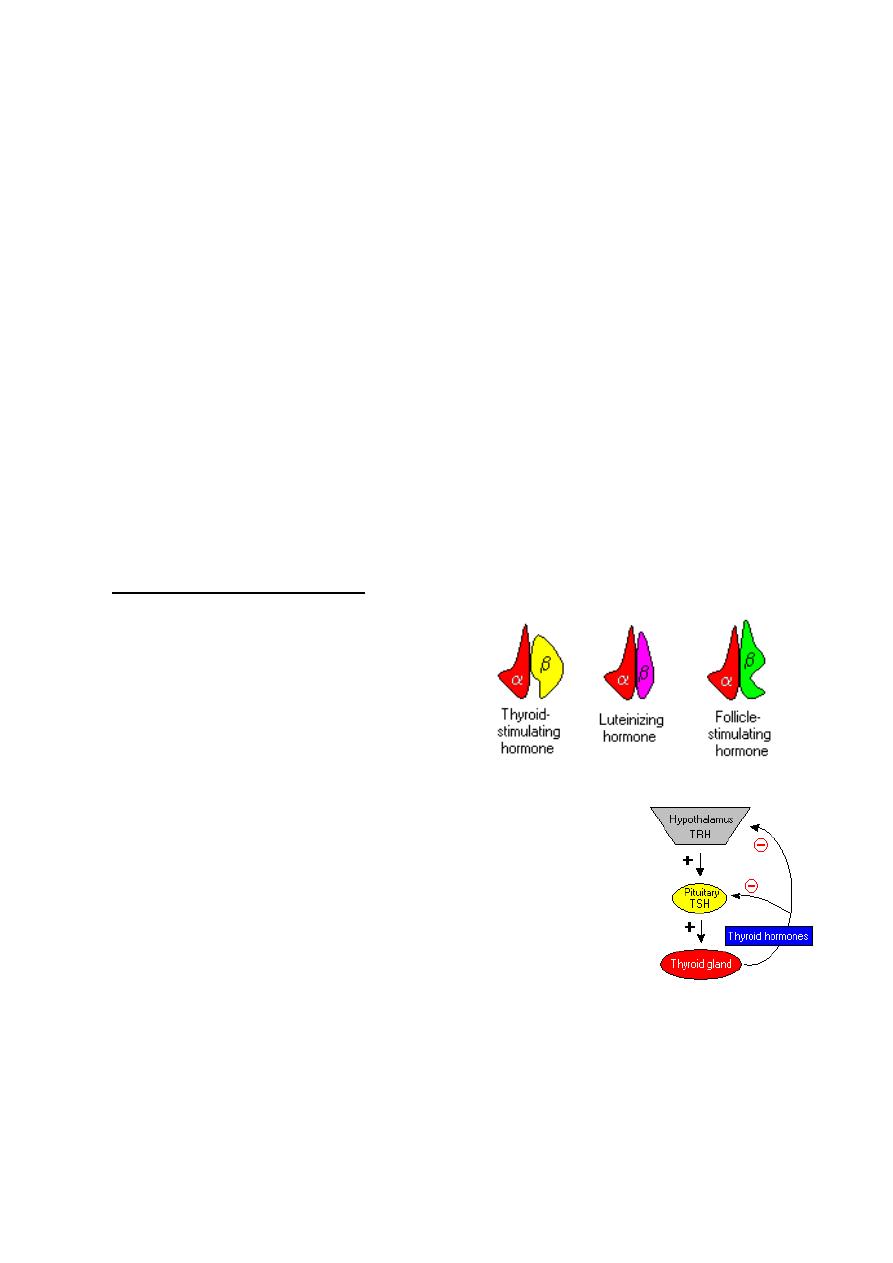
2. Thyroid Stimulating Hormone
Thyroid-stimulating hormone, also known as
thyrotropin, is secreted from cells in the
anterior pituitary called thyrotrophs, finds its
receptors on epithelial cells in the thyroid
gland, and stimulates that gland to
synthesize and release thyroid hormones.
TSH is a glycoprotein hormone composed of two subunits, which are
non-covalently bound to one another. The alpha subunit of TSH is
also present in two other pituitary glycoprotein hormones, follicle-
stimulating hormone and luteinizing hormone. In other words, TSH is
composed of alpha subunit bound to the TSH beta subunit, and TSH
associates only with its own receptor. Free alpha and beta subunits
have essentially no biological activity.
TSH has several acute effects on thyroid function. These occur in minutes and involve
increases of all phases of T
3
and T
4
biosynthesis. TSH also has several chronic effects on
the thyroid. These require several days and include increases in the synthesis of proteins,
phospholipids, and nucleic acids and in the size of number of thyroid cells.
Professor Dr. H.D.El-Yassin 2014
19
The most important controller of TSH secretion is thyroid-releasing hormone.
Secretion of thyroid-releasing hormone, and hence, TSH, is inhibited by high blood
levels of thyroid hormones in a classical negative feedback loop.
Quick quiz: All statements regarding TSH are true except:
1. It is not involved in protein and phospholipids synthesis
2. It provides NADPH by stimulating HMP pathway
3. It increases proteolysis of TBG to release T3 and T4
4. It increases uptake of iodine
3. Adrenocorticotropic Hormone
Adrenocorticotropic hormone, stimulates the adrenal cortex by enhancing the
conversion of cholesterol to pregnenolone. More specifically, it stimulates secretion
of glucocorticoids such as cortisol, and has little control over secretion of aldosterone,
the other major steroid hormone from the adrenal cortex. Another
name for ACTH is corticotropin.
ACTH is secreted from the anterior pituitary in response to
corticotropin-releasing hormone from the hypothalamus.
Corticotropin-releasing hormone is secreted in response to many
types of stress, which makes sense in view of the "stress
management" functions of glucocorticoids. Corticotropin-releasing
hormone itself is inhibited by glucocorticoids, making it part of a
classical negative feedback loop.
Within the pituitary gland, ACTH is produced in a process that
also generates several other hormones. A large precursor protein named
proopiomelanocortin (POMC) is synthesized and proteolytically chopped into several
fragments as depicted below.
Professor Dr. H.D.El-Yassin 2014
20
The major attributes of the hormones other than ACTH that are produced in this process
are summarized as follows:
Lipotropin: Originally described as having weak lipolytic effects, its major
importance is as the precursor to beta-endorphin.
Beta-endorphin and Met-enkephalin: Opioid peptides with pain-alleviation and
euphoric effects.
Melanocyte-stimulating hormone (MSH): Known to control melanin pigmentation
in the skin of most vertebrates.
Quick quiz: All the statements regarding ACTH are true except:
1. It is a tropic hormone with 39 amino acids
2. It decreases insulin release
3. It promotes growth of the adrenal cortex
4. In increases pigmentation of the skin
4. Prolactin (PRL)
Prolactin is a single-chain protein hormone closely related to growth hormone. It is
secreted by so-called lactotrophs in the anterior pituitary. It is also synthesized and
secreted by a broad range of other cells in the body.
Prolactin contains 199 amino acids and has three intramoleculare disulfide brides.
PRL has effects on the immune system and is important in the control of osmolality ad
various events including:
a. Metabolism of subcataiuos fat
b. Carbohydrate metabolism
c. Calcium and Vit D metabolism
d. Fetal lung development
e. Steroidogenesis
PRL binds to its receptor on the cell membrane
of its target organs (breast, adrenal, ovaries,
testes, prostate, kidney ad liver) but with
unknown intracellular mechanism.
Professor Dr. H.D.El-Yassin 2014
21
Control of Prolactin Secretion
In contrast to what is seen with all the other pituitary hormones, the hypothalamus
suppresses prolactin secretion from the pituitary.
Dopamine serves as the major prolactin-inhibiting factor or brake on prolactin
secretion. In addition to inhibition by dopamine, prolactin secretion is positively regulated
by several hormones, including thyroid-releasing hormone, gonadotropin-releasing
hormone and vasoactive intestinal polypeptide.
Estrogens provide a well-studied positive control over prolactin synthesis and
secretion.
Quick quiz: Secondary causes of hyperprolactinemia are:
1. Hypoglycemia
2. Hypothyroidism
3. Pituitary tumors
4. All the above
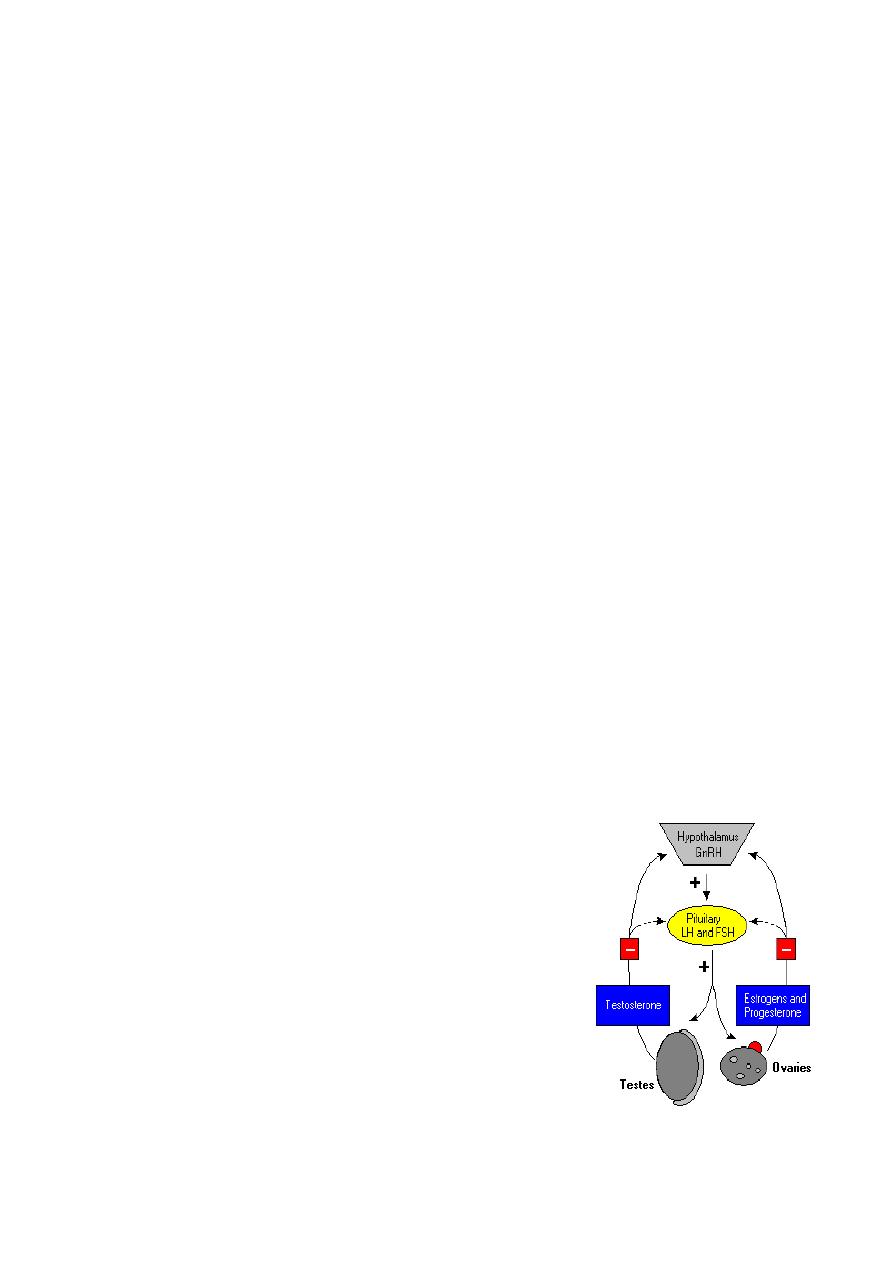
5. Gonadotropins: Luteinizing and Follicle Stimulating Hormones
Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) are called
gonadotropins because stimulate the gonads - in males, the testes, and in females,
the ovaries. As described for thyroid-simulating hormone, LH and FSH are large
glycoproteins composed of alpha and beta subunits. The alpha subunit is identical in all
three of these anterior pituitary hormones, while the beta subunit is unique for each
hormone with the ability to bind its own receptor.
a.
Luteinizing Hormone
In both sexes, LH stimulates secretion of sex steroids from the gonads. In the testes,
it stimulates the synthesis and secretion of testosterone. The
ovary respond to LH stimulation by secretion of
testosterone, which is converted into estrogen by adjacent
granulosa cells.
LH is required for continued development and function of
corpora lutea. The name luteinizing hormone derives from
this effect of inducing luteinization of ovarian follicles.
b.
Follicle-Stimulating Hormone
FSH stimulates the maturation of ovarian follicles. FSH is
also critical for sperm production. It supports the function
of Sertoli cells, which in turn support many aspects of sperm cell maturation.

Professor Dr. H.D.El-Yassin 2014
22
Control of Gonadotropin Secretion
The principle regulator of LH and FSH secretion is gonadotropin-releasing hormone
or GnRH . In a classical negative feedback loop, sex steroids inhibit secretion of GnRH
and also appear to have direct negative effects on gonadotrophs.
This regulatory loop leads to pulsatile secretion of LH and, to a much lesser extent, FSH.
Numerous hormones influence GnRH secretion, and positive and negative control over
GnRH and gonadotropin secretion is actually considerably more complex than described
in the figure. For example, the gonads secrete at least two additional hormones - inhibin
and activin , which selectively inhibit and activate FSH secretion from the pituitary.
Quick quiz The following hormones have structural homology except:
1. TSH
2. LH and FSH
3. PRL
4. HCG
Conclusion
1. The pituitary gland, a roundish organ that lies immediately beneath the hypothalamus
composed of two distinctive parts:
a. The anterior pituitary (adenohypophysis).
b. The posterior pituitary (neurohypophysis)
2. knowledge of hormone structure and the ability to synthesize specific hormones
permits the diagnosis of the disease states

Professor Dr. H.D.El-Yassin 2014
23
Question : Hypopituitarism may result from trauma, such as an automobile accident
severing the stalk connecting the hypothalamus and anterior pituitary, or from tumors of
the pituitary gland. In trauma, usually all of the releasing hormones from hypothalamus fail
to reach the anterior pituitary. With a tumor of the gland, some or all of the pituitary
hormones may be shut off. Posterior pituitary hormones may also be lost. Hypopituitarism
can be life threatening. Usual therapy is administration of end-organ hormones in oral
form.
1) If the stalk between the hypothalamus and anterior pituitary is severed, the pituitary
would fail to cause the ultimate release of all of the following hormones except :
a) ACTH.
b) estradiol.
c) oxytocin.
d) testosterone.
e) thyroxine.
Answers:
1) C Oxytocin is released from posterior pituitary. A, B, D, and E all require releasing
hormones from hypothalamus for anterior pituitary to release them.
