Clinical Cases on the biochemistry of digestive system disorders
Prof. Dr.Hedef Dhafir El-Yassin 2013
Clinical Cases on the biochemistry of digestive system disorders
Group A
Case 1: Peptic ulcer disease: Zollinger-Ellison Syndrome
A 47 year old male, experienced for several months a number of symptoms,
including indigestion, loss of appetite abdominal pain and "oily" diarrhea. He visited
his physician who referred him to a gastroenterologist. He underwent fibiroptic
endoscopy, which showed an ulcer in the duodenal bulb. To determine the cause of
the ulcer additional tests were performed, including a serum gastrin level, analysis of
gastric contents a pentagastrin stimulation test. Results are shown in table 1.
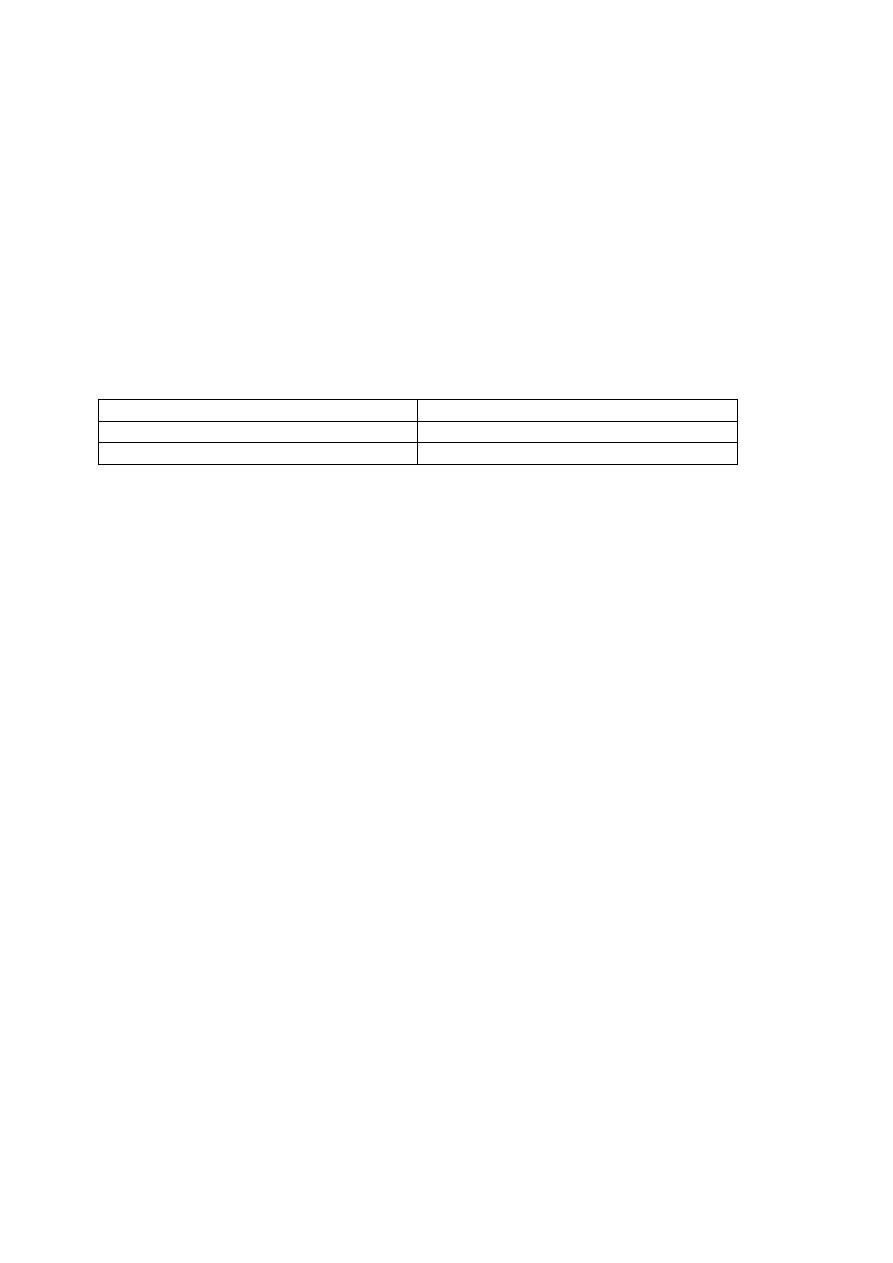
Table 1:
Serum gastrin level
800 pg/ml (normal 0-130pg/ml)
Basal gastric H
+
secretion
100 mEq/hr (normal 10 mEq/ml)
pentagastrin stimulation test
No increase in H
+
secretion
Computed tomography scan showed a 3-cm mass on the head of the pancreas. The
mass was thought to be a gastrinoma (gastrin-secreting tumor). The patient
underwent laparoscopic surgery during which the tumor was localized and removed,
the ulcer subsequently healed, and symptoms disappeared.
QUESTIONS:
1. The patient had peptic ulcer disease, which is caused by digestion of the
gastrointestinal mucosa by H
+
and pepsin. What is the mechanism of H
+
secretion by gastric parietal cells? What are the major factors that regulate H
+
secretion?
2. The gastroenterologist diagnosed the patient with Zollinger-Ellison syndrome,
or gastrinoma (a gastrin-secreting tumor). According to two important
laboratory findings that were consistent with this diagnosis:
a. an elevated serum gastrin level and
b. an elevated basal level of gastric H
+
secretion.
How does Zollinger-Ellison syndrome increase gastric H
+
secretion?
3. Why did the patient have a duodenal ulcer?
4. Pentagastrin, a gastrin analogue, did not stimulate gastric H
+
secretion. How is
this finding consistent with the diagnosis of Zollinger-Ellison syndrome? How
would a healthy person respond to the pentagastrin stimulation test?
5. Why did the patient have steatorrhea ( "oily" diarrhea)?
Group B
Case 2: Malabsorption of Carbohydrates:

Clinical Cases on the biochemistry of digestive system disorders
Prof. Dr.Hedef Dhafir El-Yassin 2013
Lactose Intolerance
A 21-year-old student experienced during the 6 months several bouts of abdominal
bloating and cramps, followed by diarrhea. At first, she thought these episodes were
caused by the stress of her demanding academic program. However, she noticed
that the symptoms occurred approximately 1 hour after drank drank milk or ate ice
cream. She was examined by her primary care physician, who found her to be in
excellent health.
Because the patient's symptoms were temporally related to ingestion of dairy
products, the physician ordered a lactose-H
2
breath test, which confirmed that has
lactose intolerance. As further confirmation of the diagnosis she abstained from dairy
products for 1 week and had no episodes of bloating, cramping, or diarrhea.
QUESTIONS:
1. How are dietary carbohydrates digested in the gastrointestinal tract? What are
the roles of salivary, pancreatic, and intestinal mucosal brush border enzymes
in carbohydrate digestion? What three monosaccharides are the final products
of these digestive steps?
2. How are dietary carbohydrates absorbed from the lumen of the
gastrointestinal tract into the blood? Draw a small intestinal epithelial cell that
shows the appropriate transporters in the apical and basolateral membranes.
3. Describe the steps involved in the digestion and absorption of lactose.
4. Why does lactose intolerance cause diarrhea?
5. What treatment do you recommended?
Group C
Case 3: Bile acid deficiency:
A 39 year-old male who was diagnosed with Crohn's disease (an inflammatory bowel
disease) when he was a teenager, had several bad remissions that ultimately lead to

Clinical Cases on the biochemistry of digestive system disorders
Prof. Dr.Hedef Dhafir El-Yassin 2013
small bowel obstruction and underwent emergency surgery that removed 80% of his
ileum. Since the surgery he suffered oily diarrhea. His stools are pale with foul-
smelling.
QUESTIONS:
1. What are bile salts? What purpose is served by converting bile acids to bile salts?
2. Describe the enterohepatic circulation of bile salts.
3. What role do bile salts play in the absorption of dietary lipids?
4. Why did the patient have steatorrhea ( "oily" diarrhea)after his ileal resecection?
5. The patient had "bile acid diarrhea." Why do bile acids cause diarrhea? (Big hint:
They stimulate colonic Cl- secretion.) Why don't healthy persons have bile acid
diarrhea?
Group D
Case 4: cystinuria and Hartnup disease
A 10 year old male was diagnosed with cystinuria. He suffered a painful episode of
renal colic, during which he passed a kidney stone. He had faithfully maintained a
high daily fluid intake and had taken the medication required to increase the pH of his
urine, to increase the solubility of the large amounts of cystine present in his urine
and, thereby, to prevent further formation of kidney stones (calculi). His mother heard
that some dietary amino acids were not absorbed in patients with cystinuria and
asked whether any dietary changes would reduce the patient’s chances of
developing additional renal stones
QUESTIONS:

Clinical Cases on the biochemistry of digestive system disorders
Prof. Dr.Hedef Dhafir El-Yassin 2013
1. What are the causes of cystinuria?
2. Why do patients with cystinuria and Hartnup disease have a
hyperaminoaciduria without an associated hyperaminoacidemia?
3. Do patients with cystinuria and Hartnup disease are able to get some of the
benefit of the protein they consume? Why
4. How does dietary changes reduce the patient’s chances of developing
additional renal stones?
5. why do think patients with the Hartnup biochemical phenotype eventually
develop pellagra-like manifestations? which usually include a photosensitivity
rash, ataxia, and neuropsychiatric symptoms?
Group E
Case 5: Acute pancreatitis
An alcoholic continued to abuse alcohol and to eat poorly. After a particularly heavy
intake of alcohol, a steady severe pain began in his upper mid-abdomen. This pain
spread to the left upper quadrant and eventually radiated to his mid-back. He began
vomiting nonbloody material and was brought to the hospital emergency room with
fever, a rapid heart beat, and a mild reduction in blood pressure. On physical
examination, he was dehydrated and tender to pressure over the upper abdomen.
His vomitus and stool were both negative for occult blood. Blood samples were sent
to the laboratory for a variety of hematologic and chemical tests, including a
measurement of serum amylase and lipase, which showed a decrease in their level.
QUESTIONS:
1. Give a brief explanation of the patient’s syndromes
2. List the digestive enzymes secreted from the pancreas together with their
functions.
3. How does excess alcohol affect the pancreas and cause acute pancreatitis?
4. Do you think that the patient may develop steatorrhea? Why?
