Clinically
Important
Enzymes and
Diagnostic
Applications
(part I)
Prof. Dr. H.D.El-Yassin
October 2013
Prof. Dr. H.D.El-Yassin
2013
2
Objectives
1. To list some clinically important enzymes
2. To state the distribution and applications of clinically important enzymes
3. to interpret the biochemical results of serum enzymes for three cases of different
liver diseases
4. To illustrate the serum enzyme patterns in different diseases
5. To assess the serum enzyme patterns in viral hepatitis
Clinically Important Enzymes and
Diagnostic Applications
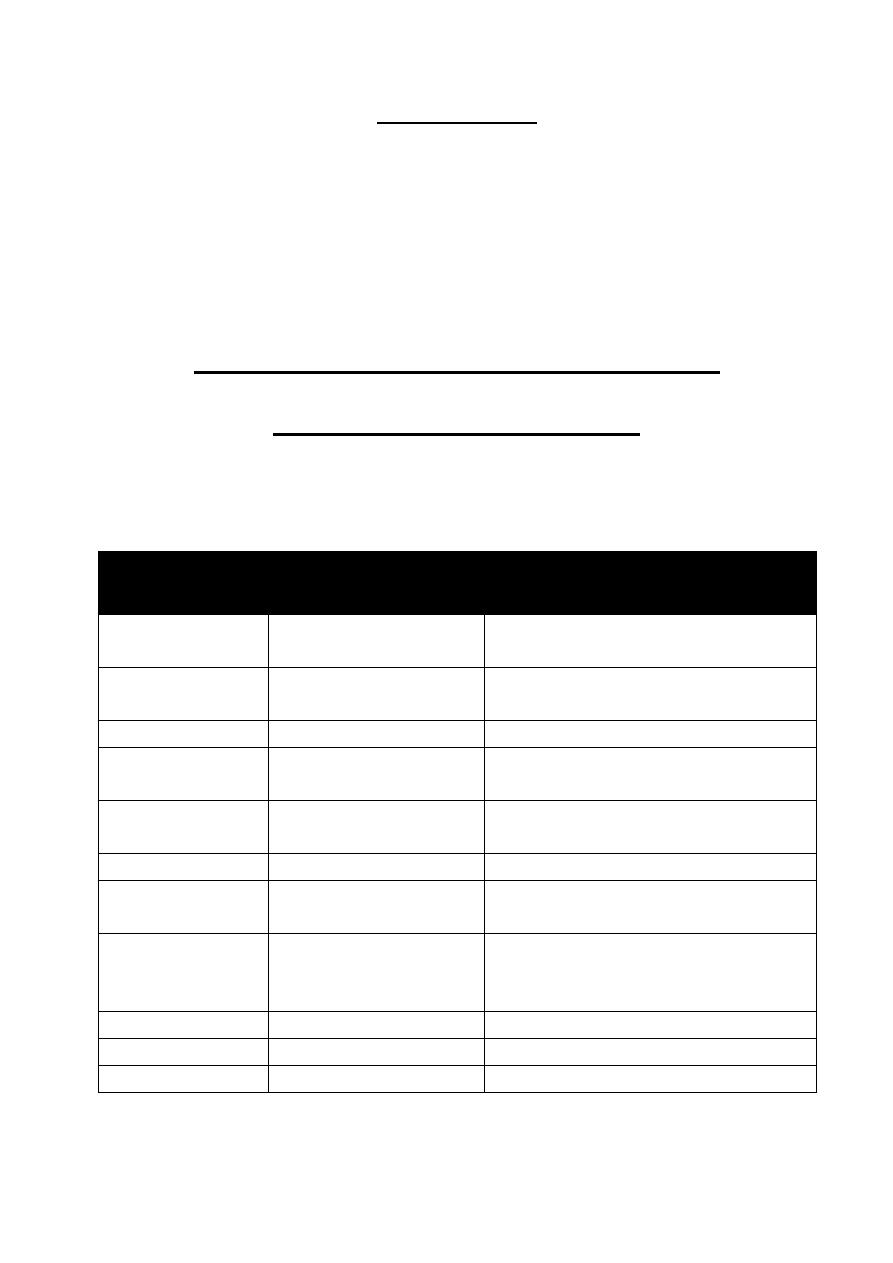
Distribution and application of clinically important enzymes
Enzyme
Principle Sources of
Enzyme in blood
Clinical applications
Alanine
aminotransferase
Liver
Hepatic parenchymal diseases
Alkaline
phosphetase
Liver, bone, intestinal
mucosa, placenta
Bone diseases, hepatobiliry diseases
Amylase
Salivary glands, pancreae
Pancreatic diseases
Aspartate
aminotrasferase
Liver, skeletal muscle,
heart erythrocytes
Hepatic parenchymal disease, muscle
disease
Cholinesterase
Liver
Organophosphorus insecticide poisoning,
hepatic parenchymal disease
Creatine kinase
Skeletal muscle, heart
Muscle diseases(M.I.)
γ-glutamyl
transferase
Liver
Hepatobiliary diseases, marker of alcohol
abuse
Lactate
dehydrogenase
Heart, liver, skeletal
muscle, erythroctes,
platelets, lymph nodes
Hemolysis, hepatic parenchymal diseases,
tumor marker
lipase
Pancreas
Pancreatic diseases
5'-nucleotidase
Liver
Hepatbiliary diseases
Trypsin
pancreas
Pancreatic diseases
Prof. Dr. H.D.El-Yassin
2013
3
Pancreatic enzymes:
Acute pancreatitis is an inflammatory process in which pancreatic enzymes are
activated and cause autodigestion of the gland. It is a result of anatomical changes that
arise from two events.
1. The first is the autodigestion of the acinar cells by inappropriate activation of the
pancreatic enzymes (especially trypsinogen) within the cell.
2. The second is the cellular injury response that is mediated by proinflammatory
cytokines.
There are some enzymes that are synthesized and stored as the active enzymes in the
zymogen granules. These include
α-amylase, lipase, colipase, RNase, and DNase.
1.
α-Amylase: (EC3.2.1.1; 1,4- α-D-glucan glucanohydrolase; AMY) is an
enzyme of the hydrolyase class that catalyzes the hydrolysis of 1,4-
α-glycosidic
linkages in polysaccharides. AMYs are calcium metaloenzymes, with the
calcium absolutely required for functional integrity.
AMYs normally occurring in human plasma are small molecules with molecular
weights varying from 54 to 62 kDa. The enzyme is thus small enough to pass the
glumeruli of the kidneys and AMY is the only plasma enzyme physiologically found in
urine. The AMY activity present in normal serum and urine is of pancreatic (P-AMY)
and salivary gland (S-AMY) origin.
Clinical Significance
Normal values of amylase: 28-100 U/L =0.48-1.7 µkat/L
CAUSES OF RAISED PLASMA AMYLASE ACTIVITY
Marked increase (five to 10 times the upper reference limit):
o acute pancreatitis:
o severe glomerular impairment:
o perforated peptic ulcer especially if there is perforation into the lesser
sac.
Pancreatic pseudocyst. If the plasma amylase activity fails to fall after an attack of
acute pancreatitis there may be leakage of pancreatic fluid into the lesser sac (a
pancreatic pseudocyst). Urinary amylase levels are high, differentiating it from
macroamylasaemia. This is one of the few indications for estimating urinary amylase
activity, which is inappropriately low relative to the plasma activity if there is glomerular
impairment or macroamylasaemia
Prof. Dr. H.D.El-Yassin
2013
4
Macroamylasaemia. In some patients a high plasma amylase activity is due to a low
renal excretion of the enzyme, despite normal glomerular function. The condition is
symptomless; it is thought that either the enzyme is bound to a high molecular
weight plasma component such as protein, or that the amylase molecules form large
polymers that cannot pass through the glomerular membrane. This harmless
condition may be confused with other causes of hyperamylasaemia
2. Lipase: (EC 3.1.1.3; triacylglycerol acylhydrolase; LPS).is a single
–
chain glycoprotein with molecular weight of 48 kDa. For full catalytic
activity and greatest specificity the presence of bile salts and a cofactor
called colipase, which is secreted by the pancreas, is required. LPS is a
small molecule and is filtered through the glomerulus. It is totally
reabsorbed by the renal tubules, and it is not normally detected in urine.
Clinical Significance
Normal values: 40-200 U/L
Plasma lipase levels are elevated in acute pancreatitis and carcinoma of the
pancreas.
Note: serum amylase is increased in mumps, pancreatic disease or due to some other
cause, where as lipase is increased only in pancreatitis. Therefore, the determination of
both amylase and lipase together helps in the diagnosis of acute pancreatitis.
Prof. Dr. H.D.El-Yassin
2013
5
Liver enzymes:
The assay of serum enzymes is very useful for the differential diagnosis and monitoring
of various heptobiliy disorders.
There are three types of enzymes:
1. Enzymes which are normally present inside the hepatocytes released into the
blood when there is a hepatocellular damage= markers of hepatocellular
damage.
2. Enzymes which are primary membrane bound (plasma membrane or side of
hepatocytes) = markers of cholestasis.
3. Enzymes which are synthesized in the hepatocyte= indicates disturbances in
the hepatocellular synthesis.
1.Markers of hepatocellular damage.
1. Aminotransaminases
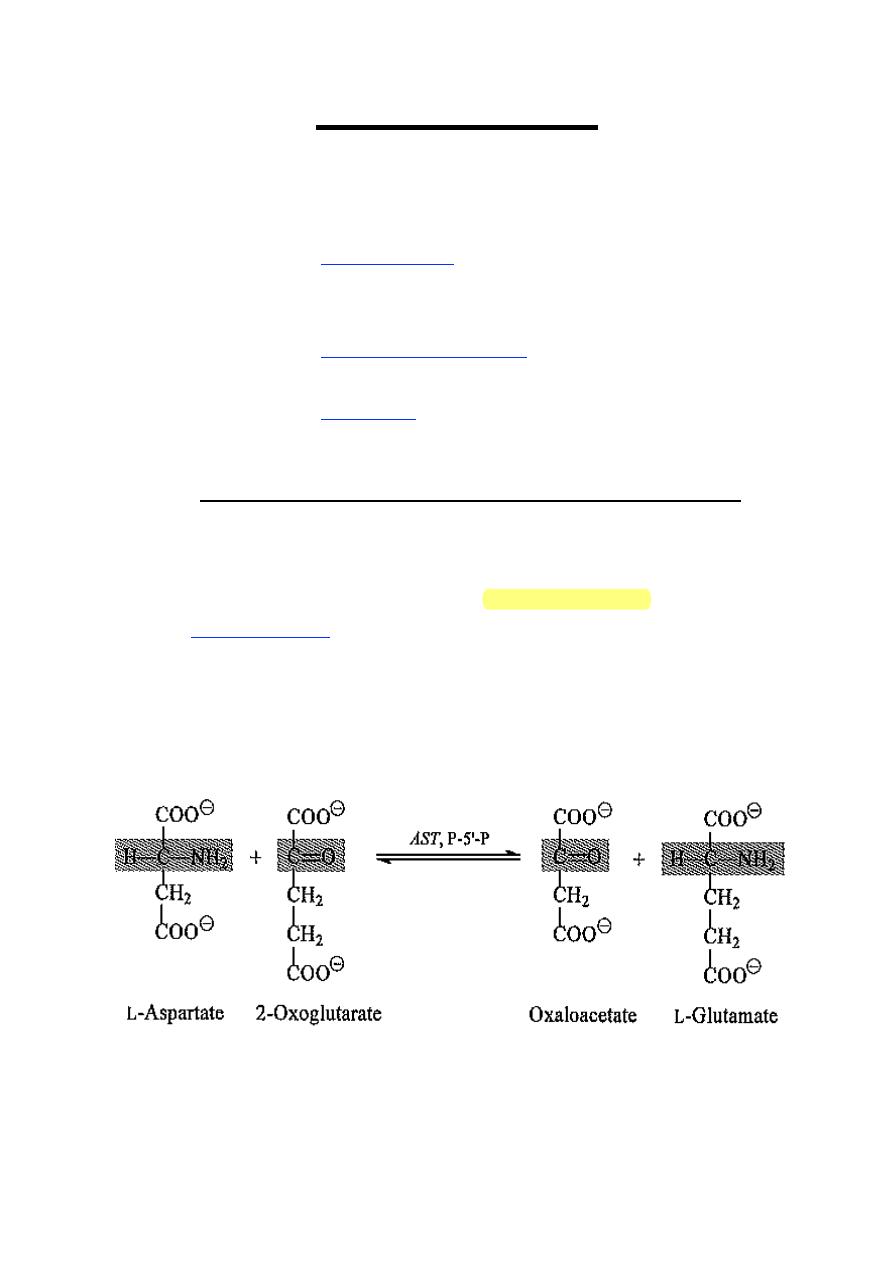
The transaminases are enzymes involved in the transfer of an amino group from a 2-
amino- to a 2-oxoacid: they need the cofactor, pyridoxal phosphate for optimal activity.
They are widely distributed in the body.
The 2-oxoglutarate/L-glutamate couple serves as one amino group acceptor and donor
pair in all amino-transfer reactions; the specificity of the individual enzymes derives from
the particular amino acid that serves as the other donor of an amino group. Thus AST
catalyzes the reaction:
Prof. Dr. H.D.El-Yassin
2013
6
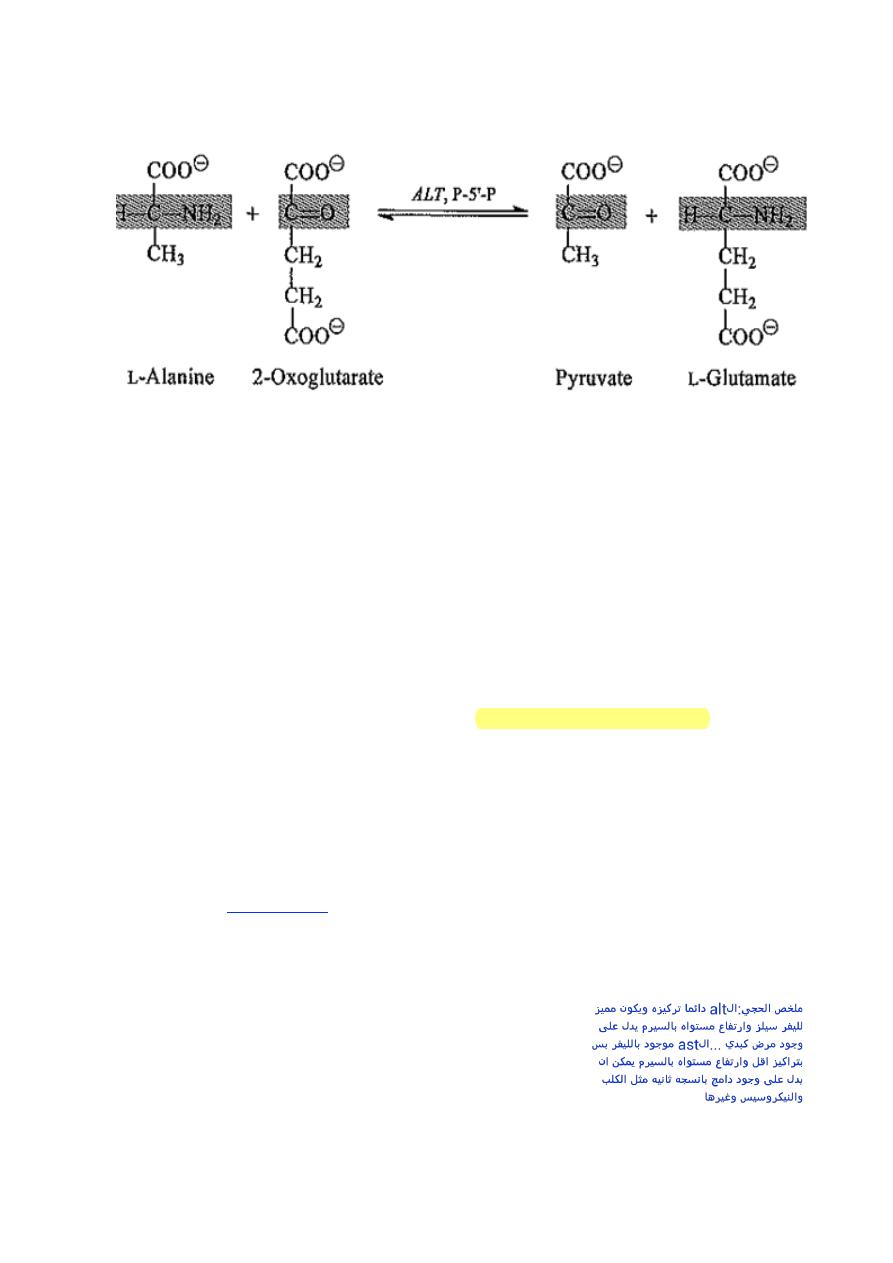
ALT catalyzes the analogous reaction:
The reactions are reversible, but the equilibrium of AST and ALT reactions favor formation
of aspartate and alanine respectively.
o Location:
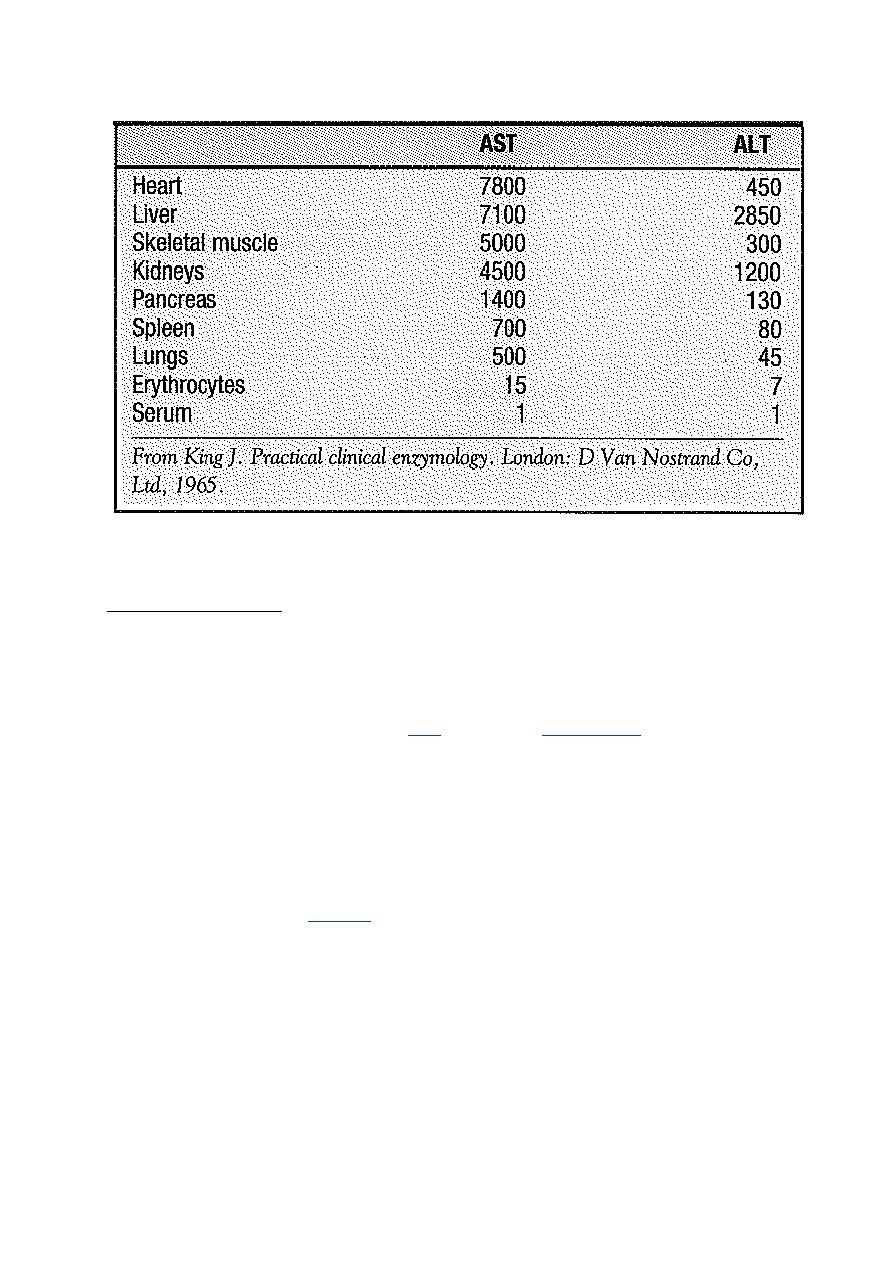
o AST present in cytosol and mitochondria
o ALT located in cytosol of liver
o In the liver, the concentration of ALT per unit weight of the tissue is more than AST.
o These enzymes are more important in assessing and monitoring the degree of liver
cell inflammation and necrosis.
o The highest activities of ALT are found in hepatocytes and muscle cells.
o Hepatocytes have very high activity of ALT, therefore elevations in serum ALT are
considered to be relatively specific for liver disease.
o AST may be elevated in other forms of tissue damage, such as myocardial
infarction, muscle necrosis and renal disorders.
o In liver disease, the ALT level is increased markedly compared to AST.
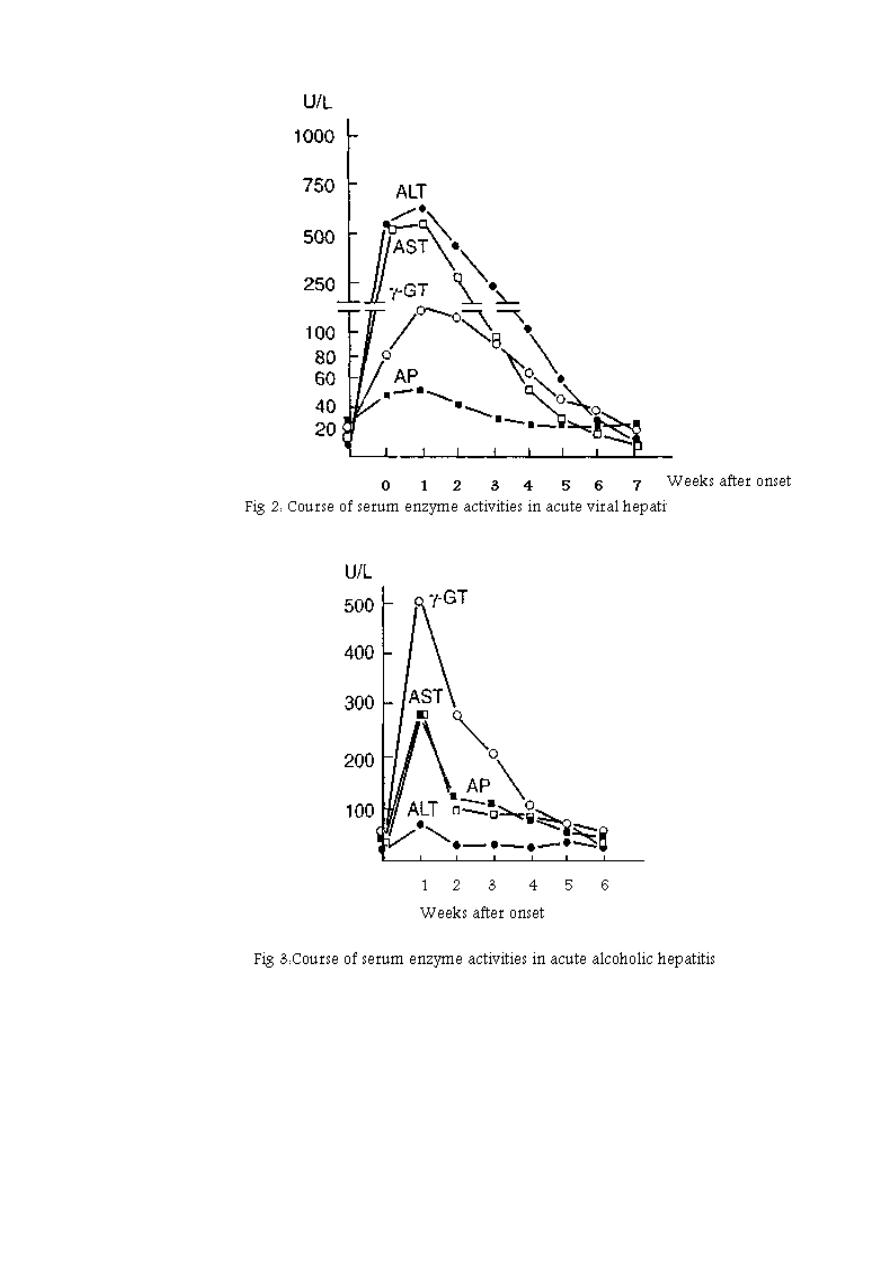
o In acute viral hepatitis there is a 100-1000 times increase in both ALT and AST but
ALT level is increased more than that of AST
Prof. Dr. H.D.El-Yassin
2013
7
Table: Aminotransferase activities in human tissues, relative to serum as unity
a. Aspartate Transaminase (EC 2.6.1.1; L-aspartate:2-oxoglutarate
aminotransferase; AST)
Clinical Significance
Normal values of AST:
male:
<35 U/L = <0.60 µkat/L
Female:
<31 U/L = <0.53 µkat/L
AST (glutamate oxaloacetate transaminase. GOT) is present in high concentrations in
cells of cardiac and skeletal muscle, liver, kidney and erythrocytes. Damage to any of
these tissues may increase plasma AST levels. Half- life = 17 hours.
CAUSES OF RAISED PLASMA AST ACTIVITIES
• Artefactual.
Due to in vitro release from erythrocytes if there is haemolysis or if separation of
plasma from cells is delayed.
• Physiological.
During the neonatal period (about 1.5 times the upper adult reference limit).
• Marked increase (10 to 100 times the upper adult reference limit):
Circulatory failure with 'shock' and hypoxia:
Myocardial infarction
Acute viral or toxic hepatitis.
Prof. Dr. H.D.El-Yassin
2013
8
b. Alanine Transaminase (EC 2.6.1.2; L-alanine:2-oxoglutarate
aminotransferase; ALT)
Clinical Significance
Normal values of ALT:
male:
<45 U/L = <0.77 µkat/L
Female:
<34 U/L = <0.58 µkat/L
ALT (glutamate pyruvate transaminase. GPT) is present in high concentrations in liver
and to a lesser extent, in skeletal muscle, kidney and heart. Half- life = 47 hours
In liver damage, both enzymes are increased but ALT increases more. In myocardial
infarction AST is increased with little or no increase in ALT.
CAUSES OF RAISED PLASMA ALT ACTIVITIES
Marked increase (10 to 100 times the upper limit of the adult reference range
circulatory failure with 'shock' and hypoxia:
Acute viral or toxic hepatitis.
Moderate increase:
Cirrhosis (may be normal or up to twice the upper adult reference limit): infectious
mononucleosis (due to liver involvement):
Liver congestion secondary to congestive cardiac failure:
cholestatic jaundice (up to 10 times the upper reference limit in adults); surgery or
extensive trauma and skeletal muscle disease (much less affected than AST)
same AST except
Myocardial infarction
Prof. Dr. H.D.El-Yassin
2013
9
2.Markers of cholestasis
I. Alkaline phosphatase (EC 3.1.3.1; orthophosphoric-monoester
phosphohydrolase [alkaline optimum]; ALP). Half-life= 10 days
Clinical Significance
The alkaline phosphatases are a group of enzymes that hydrolyse organic phosphates
at high pH. They are present in most tissues but are in particularly high concentration in
the osteoblasts of bone and the cells of the hepatobiliary tract, intestinal wall, renal
tubules and placenta. The exact metabolic function of ALP is unknown but it is probably
important for calcification of bone.
In adults plasma ALP is derived mainly from bone and liver in approximately equal
proportions: the proportion due to the bone fraction is increased when there is
increased osteoblastic activity that may be physiological
Causes of raised Plasma ALP activity
Physiological:
There is a gradual increase in the proportion of liver ALP with age:
in the elderly the plasma bone isoenzyme activity may increase slightly.
Bone disease
rickets and osteomalacia
secondary hyperparathyroidism .
Liver disease-.
Malignancy.
bone or liver involvement or direct tumor production.
POSSIBLE CAUSES OF LOW PLASMA ALP ACTIVITY
• Arrested bone growth
• Hypophosphatasia: an autosomal recessive disorder, associated with rickets or
osteomalacia.
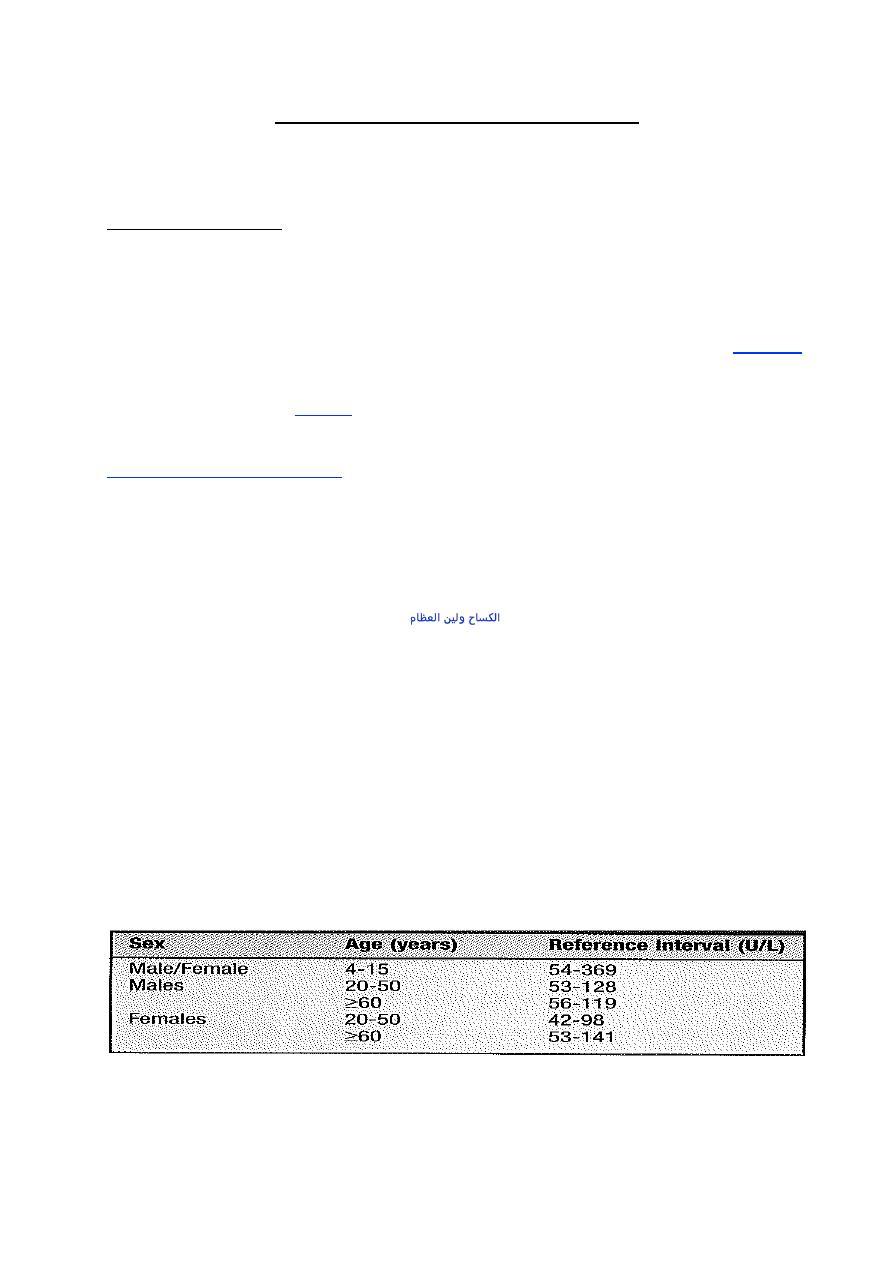
Table: reference intervals for alkaline phosphatase activities inn serum
ISOENZYMES OF ALKALINE PHOSPHATASE
Prof. Dr. H.D.El-Yassin
2013
01
Bone disease with increased osteoblastic activity, or liver disease with involvement of the
biliary tracts, are the commonest causes of an increased total alkaline phosphatase
activity.
Assays for ALP isoenzymes are needed when:
I. The source of an elevated ALP in serum is not obvious and should be
clarified.
II. The main clinical question is concerned with detecting the presence of
liver or bone involvement
III. In the case of metabolic bone disorders, to ascertain any modifications in
the activity of osteblastes to monitor the disease activity and the effect of
appropriate therapies.
2. Gamma-glutamyl-transferase
(EC 2.3.2.21; γ-glutamyl-peptide: amino
acid γ -glutamyletransferase; GGT): catalyzes the transfere of the γ –
glutamyl group from peptides and compounds that contain it to an acceptor
Gamma-glutamyltransferase occurs mainly in the cells of liver, kidneys, pancreas
and prostate. Plasma GGT activity is higher in men than in women.
Clinical Significance
Normal values for GGT
male:
<55 U/L = <0.94 µkat/L
Female:
<38 U/L = <0.65 µkat/L
Causes of raised plasma GGT activity
• Induction of enzyme synthesis, without cell damage, by drugs or alcohol.
• Hepatocellular damage, such as that due to infectious hepatitis:
A patient should never be labeled an alcoholic because of a high plasma GGT activity
alone.
Other enzymes
Glutamate dehydrogenase (EC 1.4.1.3; L-glutamate: NAD(P)
+
oxidoreductase,
deaminating; GLD) is a mitochondrial enzyme found mainly in the:
a. liver
b. heart muscle
c. kideys
but small amounts occur in other tissue, including
d. brain
e. skeletal muscle tissue
f. leukocytes
Prof. Dr. H.D.El-Yassin
2013
00
Clinical significance
GLD is increased in serum of patients with hepatocellular damage offering differential
diagnostic potential in the investigation of liver disease, particularly when interpreted in
conjunction with other enzyme test results. The key to this differential diagnostic
potential is to be found in the intraorgan and intracellular distribution of the enzyme. As
an exclusively mitochondrial enzyme, GLD is released from necrotic cells and is of
value in estimation of the severity of liver cell damage. GLD activity in serum is stable at
4ºC for 48 hours and at -20ºC for several weeks. The GLD upper reference limits are
6U/L (women) and 8U/L (men), when a method optimized at 37ºC is used.
Clinical Cases:
Case1:
A healthy 43- year old male, on no medication, had the following
results of tests performed during a private healthcare screening program.
Plasma
Bilirubin 43µ mol/L (< 20)
Unconjucated bilirubin 36µ mol/L (< 5)
Alanine aminotransferase 21U/L (< 42)
Alakaline phosphatase 126 U/L (< 250)
Albumin 40 g/L (35-45)
Gamma-glutamyltransferase 42 U/L (< 55)
Urinary bilirubin negative
Normal full blood count, reticulocytes and blood film.
Discussion
The raised concentration of the plasma bilirubin is predominant ly unconjugated. There
is no evidence of haemolysis and the other liver function tests are normal. A likely
diagnosis is of Gilbert's syndrome. This is a common condition and its diagnosis is
based on the exclusion of liver disease and heamolisis in the presence of a modest
concentration of unconjugated hyper bilirubineamia.
Case2 :
A 50-year old known alcoholic make attended the general medical
clinic because of ascites and the following abnormal liver test results
Plasma:
Bilirubin 52µ mol/L (< 20)
Alanine amino transferase 76 U/L (< 42)
Alakaline phosphatase 271 U/L (< 250)
Albumin 18 g/L (35-45)
Gamma-glutamyltransferase 324 U/L (< 55)
Urinary bilirubin and protin normal.
Discussion
The abnormal liver test and hypoalbuminaemia together with ascites supported the
diagnosis of cirrhosis, secondary to his alcohol problem. Hypoalbumineamia may be
due to many disorders, such as gross protienuria, but in the presence of hepatic
disease suggests a reduction in hepatic synthetic typical of cirrhosis.
Prof. Dr. H.D.El-Yassin
2013
02
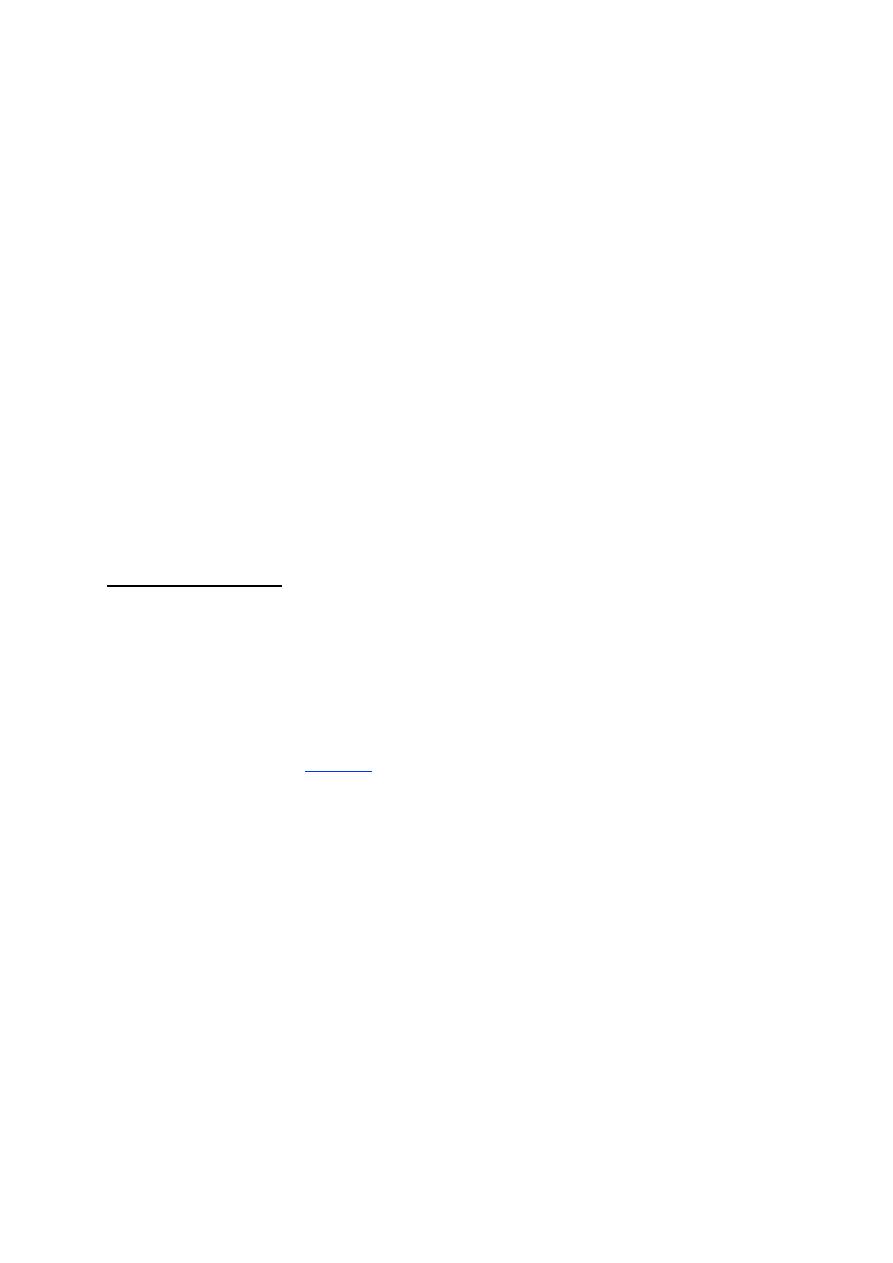
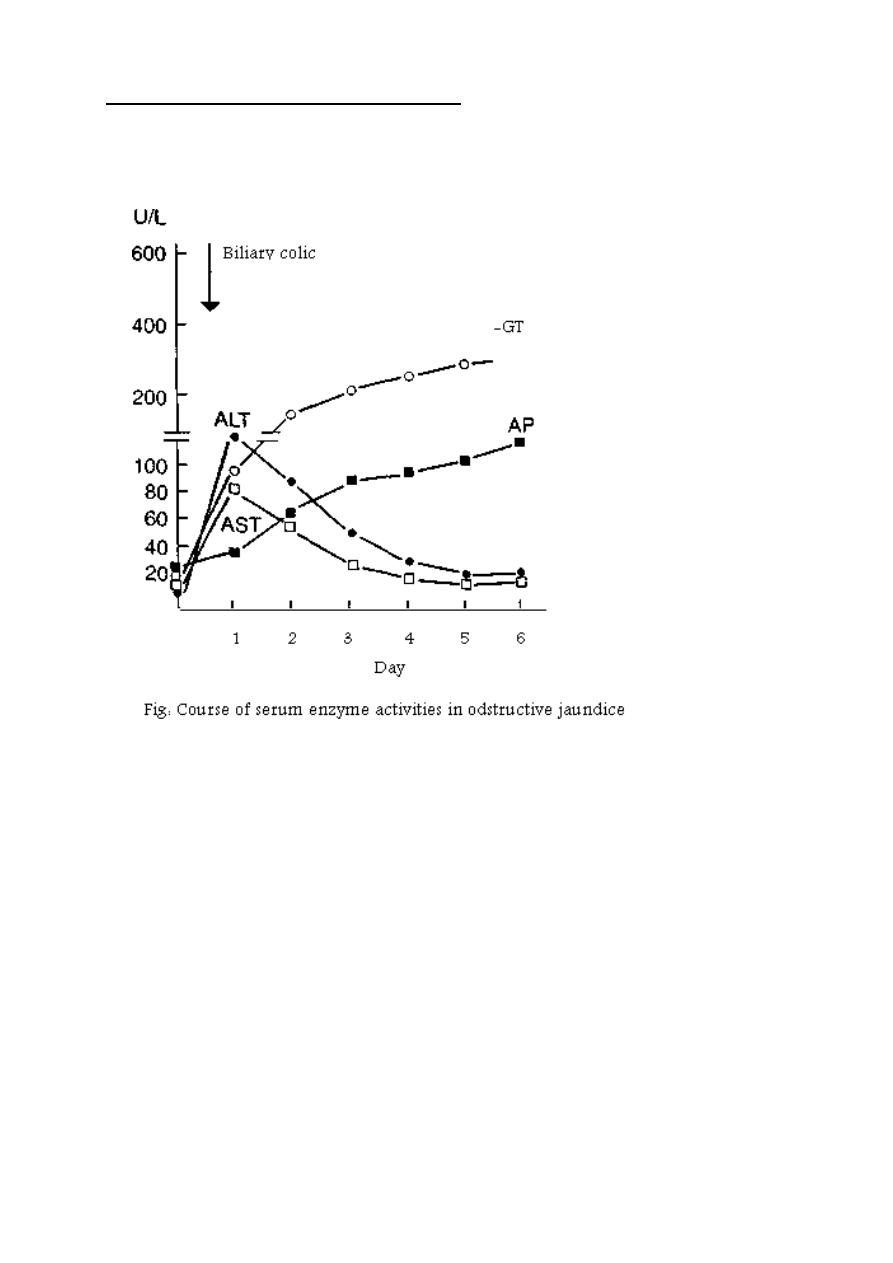
Serum Patterns in different liver diseases
Ref: Schmidt E, Schmidt FW.“Brief guide to practical enzyme diagnosis” , Houston,
1977, Boehringer Mann-heim Diagnostics.
Prof. Dr. H.D.El-Yassin
2013
03
