Lecture 5
Tuesday 1/10/2013
Prof. Dr. H.D.El-Yassin
2013
1
ABSORPTION IN THE SMALL INTESTINE
II: ABSORPTION OF AMINO ACIDS, LIPIDS
MINIRALS AND METALS
Aim and objectives of lecture 5:
1. to describe the mechanism of absorption in the small intestin
a. of amino acids and peptides
b. of lipids
c. of minerals and metals
2. to give examples of clinical disorderes of the above mechanisms
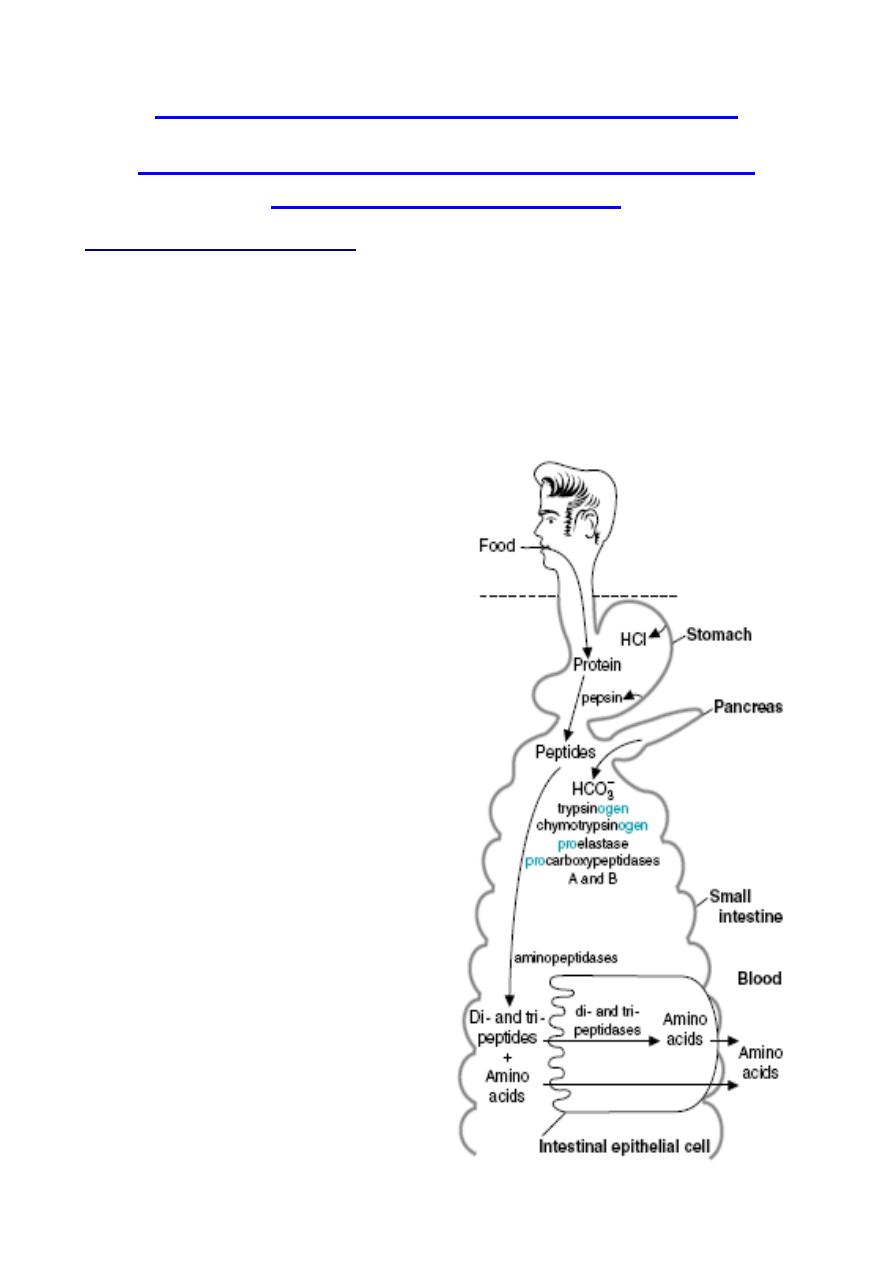
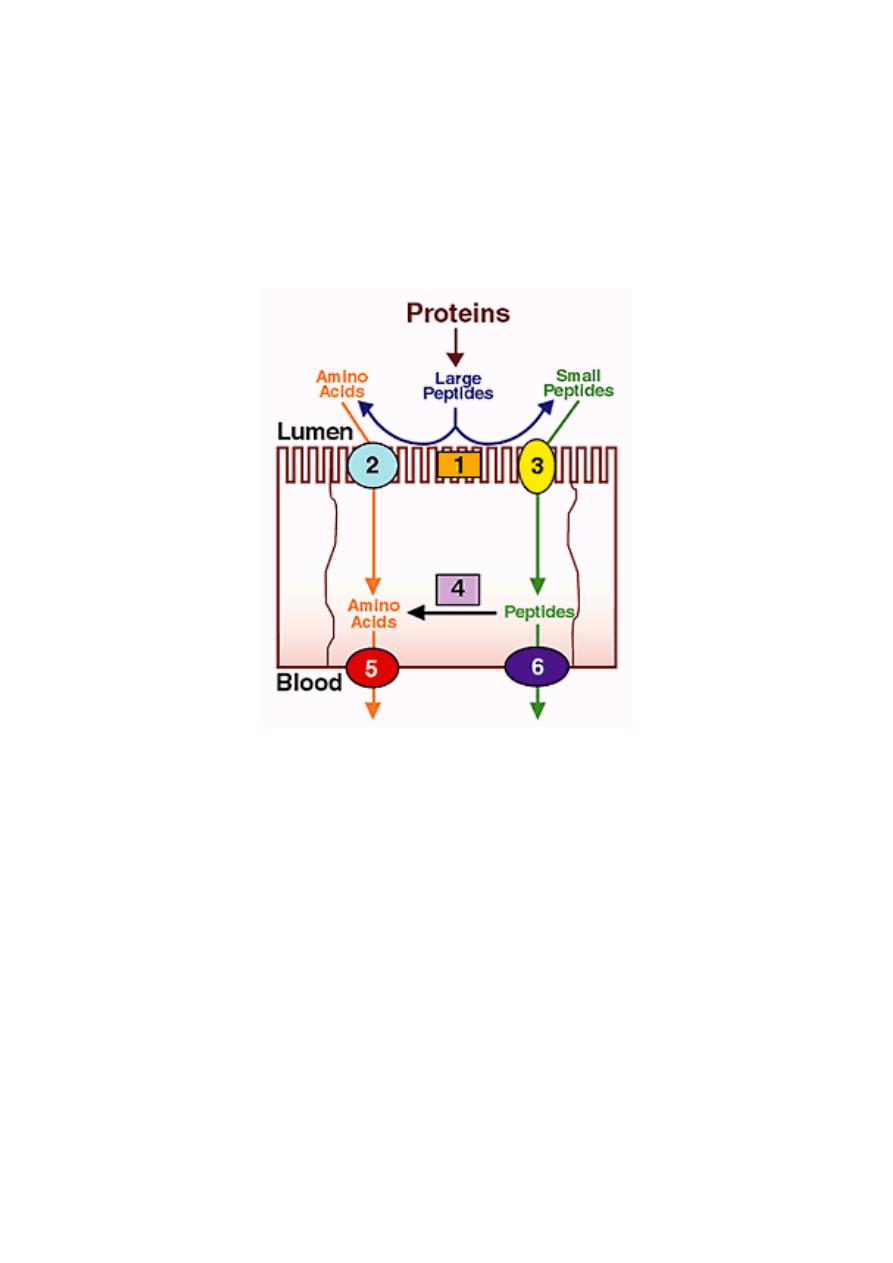
1) Absorption of Amino Acids and
Peptides
Dietary proteins are, with very few
exceptions, not absorbed. Rather, they
must be digested into amino acids or di-
and tripeptides first, through the action
of gastric and pancreatic proteases. The
brush border of the small intestine is
equipped with a family of peptidases.
Like lactase and maltase, these
peptidases are integral membrane
proteins rather than soluble enzymes.
They function to further the hydrolysis of
lumenal peptides, converting them to
free amino acids and very small
peptides. These end products of
digestion, formed on the surface of the
enterocyte, are ready for absorption.
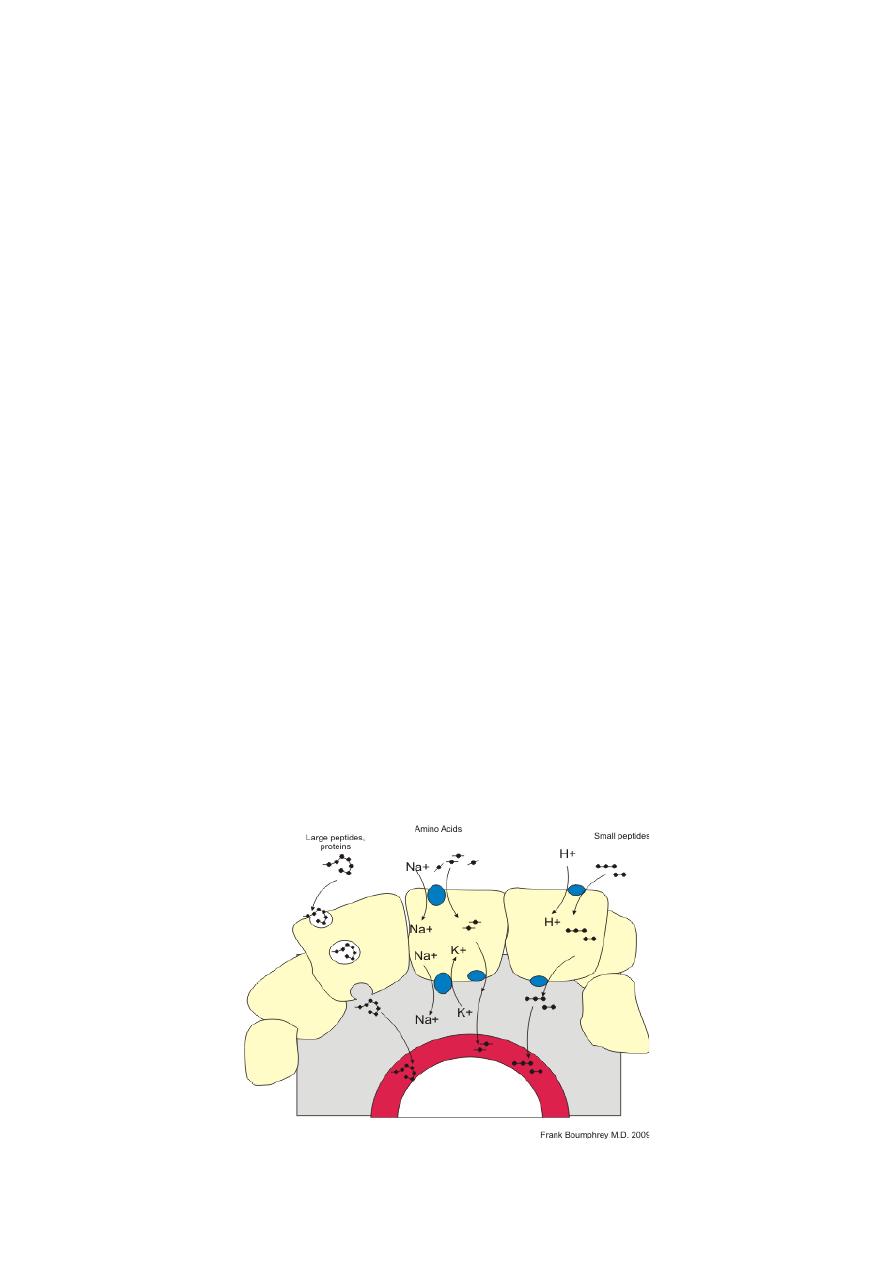
a) Absorption of Amino Acids
The mechanism by which amino acids
are absorbed is conceptually identical to
that of monosaccharides. The lumenal
plasma membrane of the absorptive cell
bears at least four sodium-dependent
amino acid transporters - one each for
acidic, basic, neutral and amino acids.
These transporters bind amino acids
only after binding sodium. The fully
loaded transporter then undergoes a
conformational change that dumps
sodium and the amino acid into the
Lecture 5
Tuesday 1/10/2013
Prof. Dr. H.D.El-Yassin
2013
2
cytoplasm, followed by its reorientation back to the original form.
Thus, absorption of amino acids is also absolutely dependent on the electrochemical
gradient of sodium across the epithelium.
Further, absorption of amino acids, like that of monosaccharides, contributes to generating
the osmotic gradient that drives water absorption.
The basolateral membrane of the enterocyte contains additional transporters which export
amino acids from the cell into blood. These are not dependent on sodium gradients.
CLINICAL CORRELATION
1.
Neutral Amino Aciduria (Hartnup Disease)
Transport functions, like enzymatic functions, are subject to modification by mutations. An example
of a genetic lesion in epithelial amino acid transport is Hartnup disease, named after the family in
which the disease entity resulting from the defect was first recognized. The disease is
characterized by the inability of renal and intestinal epithelial cells to absorb neutral amino acids
from the lumen. In the kidney, in which plasma amino acids reach the lumen of the proximal tubule
through the ultrafiltrate, the inability to reabsorb amino acids manifests itself as excretion of amino
acids in the urine (amino aciduria). The intestinal defect results in malabsorption of free amino
acids from the diet. Therefore the clinical symptoms of patients with this disease are mainly those
due to essential amino acid and nicotinamide deficiencies. The pellagra-like features are explained
by a deficiency of tryptophan, which serves as precursor for nicotinamide. Investigations of patients
with Hartnup disease revealed the existence of intestinal transport systems for di- or tripeptides,
which are different from the ones for free amino acids. The genetic lesion does not affect transport
of peptides, which remains as a pathway for absorption of protein digestion products
Q:
Why do patients with cystinuria and Hartnup disease have a hyperaminoaciduria without an
associated hyperaminoacidemia?
Lecture 5
Tuesday 1/10/2013
Prof. Dr. H.D.El-Yassin
2013
3
A:
Patients with cystinuria and Hartnup disease have defective transport proteins in both the
intestine and the kidney. These patients do not absorb the affected amino acids at a normal rate
from the digestive products in the intestinal lumen. They also do not readily resorb these amino
acids from the glomerular filtrate into the blood. Therefore, they do not have a hyperaminoacidemia
(a high concentration in the blood). Normally, only a few percent of the amino acids that enter the
glomerular filtrate are excreted in the urine; most are resorbed. In these diseases, much larger
amounts of the affected amino acids are excreted in the urine, resulting in a hyperaminoaciduria.
Pop quiz: Hartnup disease patients are able to get some of the benefit of the protein they consume
because:
a. Only the neutral amino acid carrier is defective
b. Their endo- and exopeptidases are normal
c. All of the above
d. None of the above
2.
Kwashiorkor,
A common problem of children in Third World countries, is caused by a deficiency of protein in a
diet that is adequate in calories. Children with kwashiorkor suffer from muscle wasting and a
decreased concentration of plasma proteins, particularly albumin. The result is an increase in
interstitial fluid that causes edema and a distended abdomen that make the children appear
“plump”. The muscle wasting is caused by the lack of essential amino acids in the diet; existing
proteins must be broken down to produce these amino acids for new protein synthesis. These
problems may be compounded by a decreased ability to produce digestive enzymes and new
intestinal epithelial cells because of a decreased availability of amino acids for the synthesis of new
proteins.
b) Absorption of Peptides
There is virtually no absorption of peptides longer than four amino acids. However, there is
abundant absorption of di- and tripeptides in the small intestine. These small peptides are
absorbed into the small intestinal epithelial cell by cotransport with H
+
ions via a transporter called
PepT1.
Once inside the enterocyte, the vast bulk of absorbed di- and tripeptides are digested into amino
acids by cytoplasmic peptidases and exported from the cell into blood. Only a very small number of
these small peptides enter blood intact.
c) Absorption of Intact Proteins
Absorption of intact proteins occurs only in a few circumstances. Normal" enterocytes do not have
transporters to carry proteins across the plasma membrane and they certainly cannot permeate
tight junctions.
One important exception is that for a very few days after birth, neonates have the ability to absorb
intact proteins. This ability, which is rapidly lost, is of immense importance because it allows the
newborn animal to acquire passive immunity by absorbing immunoglobulins in colostral milk. The
small intestine rapidly loses the capacity to absorb intact proteins.
Lecture 5
Tuesday 1/10/2013
Prof. Dr. H.D.El-Yassin
2013
4
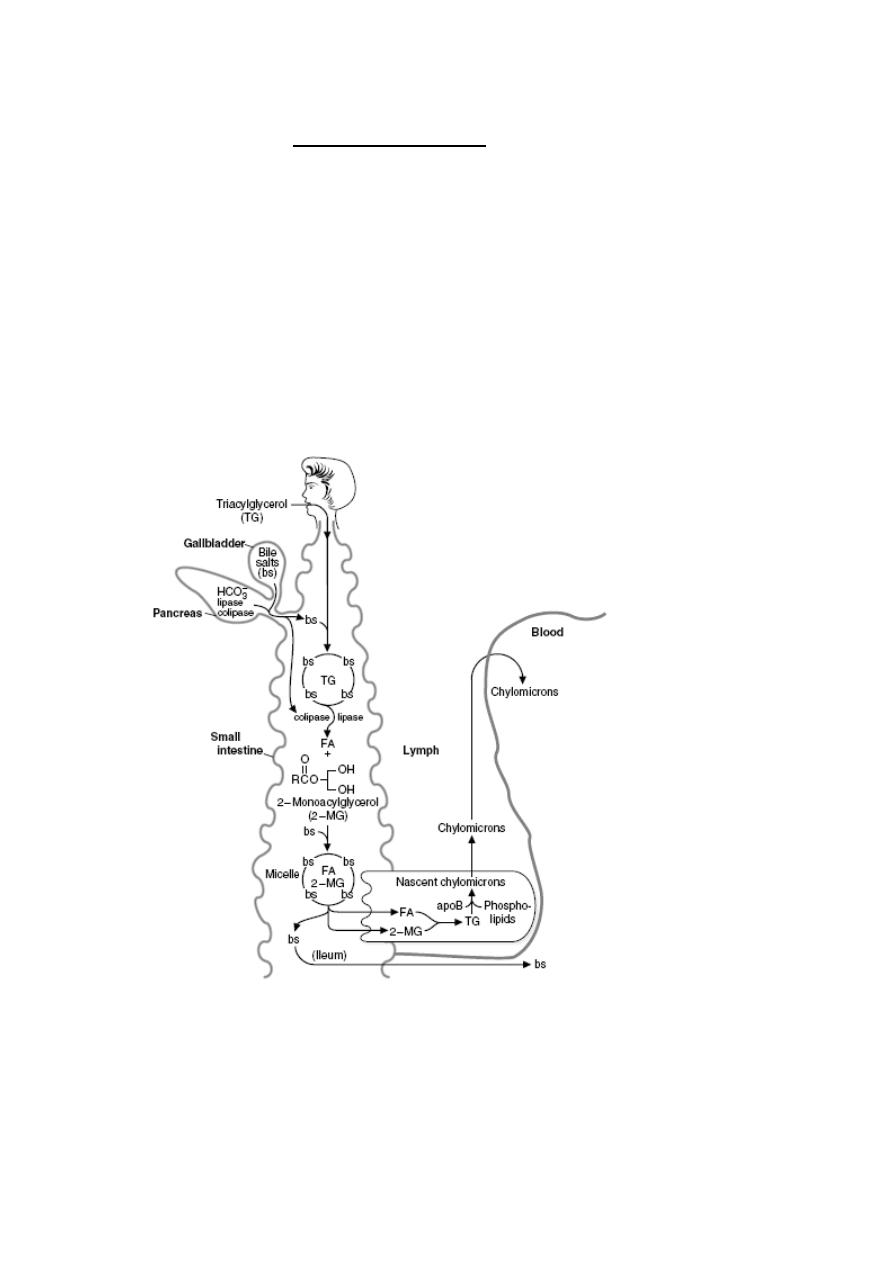
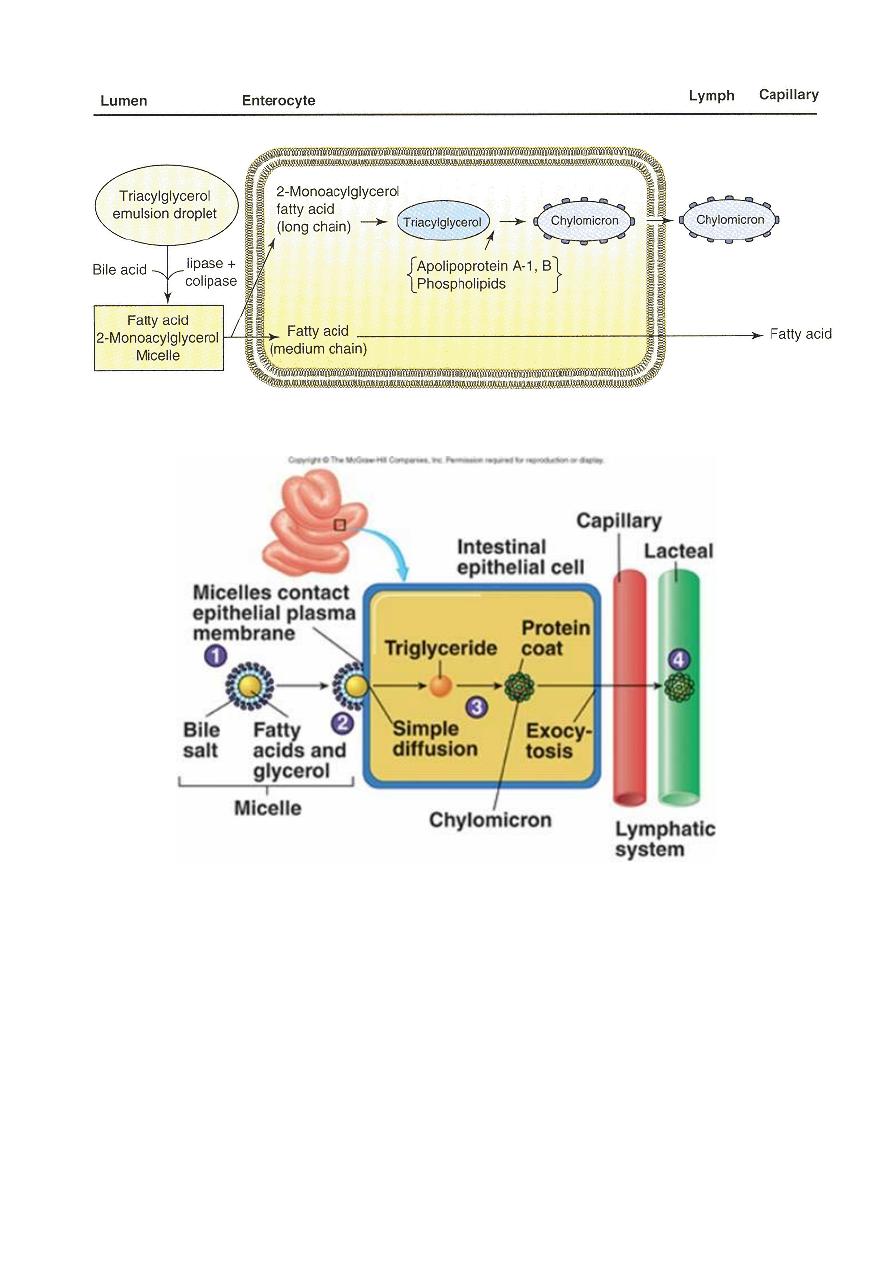
2) Absorption of Lipids
The bulk of dietary lipid is neutral fat or triglyceride, composed of a glycerol backbone with
each carbon linked to a fatty acid. Additionally, most foodstuffs contain phospholipids,
sterols like cholesterol and many minor lipids, including fat-soluble vitamins. In order for
the triglyceride to be absorbed, two processes must occur:
•
Large aggregates of dietary triglyceride, which are virtually insoluble in an aqueous
environment, must be broken down physically and held in suspension - a process
called emulsification.
•
Triglyceride molecules must be enzymatically digested to yield monoglyceride and
fatty acids, both of which can efficiently diffuse into the enterocyte
The key players in these two transformations are bile salts and pancreatic lipase, both of which are
mixed with chyme and act in the lumen of the small intestine.
Digestion of triacylglycerols in the intestinal lumen. TG _ triacylglycerol; bs _ bile
salts; FA _ fatty acid; 2-MG _ 2-monoacylglycerol
Lecture 5
Tuesday 1/10/2013
Prof. Dr. H.D.El-Yassin
2013
5
Digestion and absorption of lipids
CLINICAL CORRELATION
A-
β-Lipoproteinemia
A-b-lipoproteinemia is an autosomal recessive disorder characterized by the absence of all
lipoproteins containing apo-
β-lipoprotein, that is, chylomicrons, very low density
lipoproteins (VLDLs), and low density lipoproteins (LDLs). Serum cholesterol is extremely
low. This defect is associated with severe malabsorption of triacylglycerol and lipid-soluble
vitamins (especially tocopherol and vitamin E) and accumulation of apo B in enterocytes
and hepatocytes. The defect does not appear to involve the gene for apo B, but rather one
of several proteins involved in processing of apo B in liver and intestinal mucosa, or in
assembly and secretion of triacylglycerol-rich lipoproteins, that is, chylomicrons and VLDLs
from these tissues, respectively.
Lecture 5
Tuesday 1/10/2013
Prof. Dr. H.D.El-Yassin
2013
6
2. In A-b-Lipoproteinemia, all true except
a. There is a severe malabsorption of triacylglycerol
b. accumulation of apo B in enterocytes and hepatocytes.
c. The defect involve the gene for apo B,
d. The defect involve the gene of one of several proteins involved in assembly and
secretion of triacylglycerol-rich lipoproteins, that is, chylomicrons and VLDLs from
these tissues, respectively.
3) Absorption of Minerals and Metals
The vast bulk of mineral absorption occurs in the small intestine. The best-studied
mechanisms of absorption are clearly for calcium
and iron, deficiencies of which are significant health
problems throughout the world.
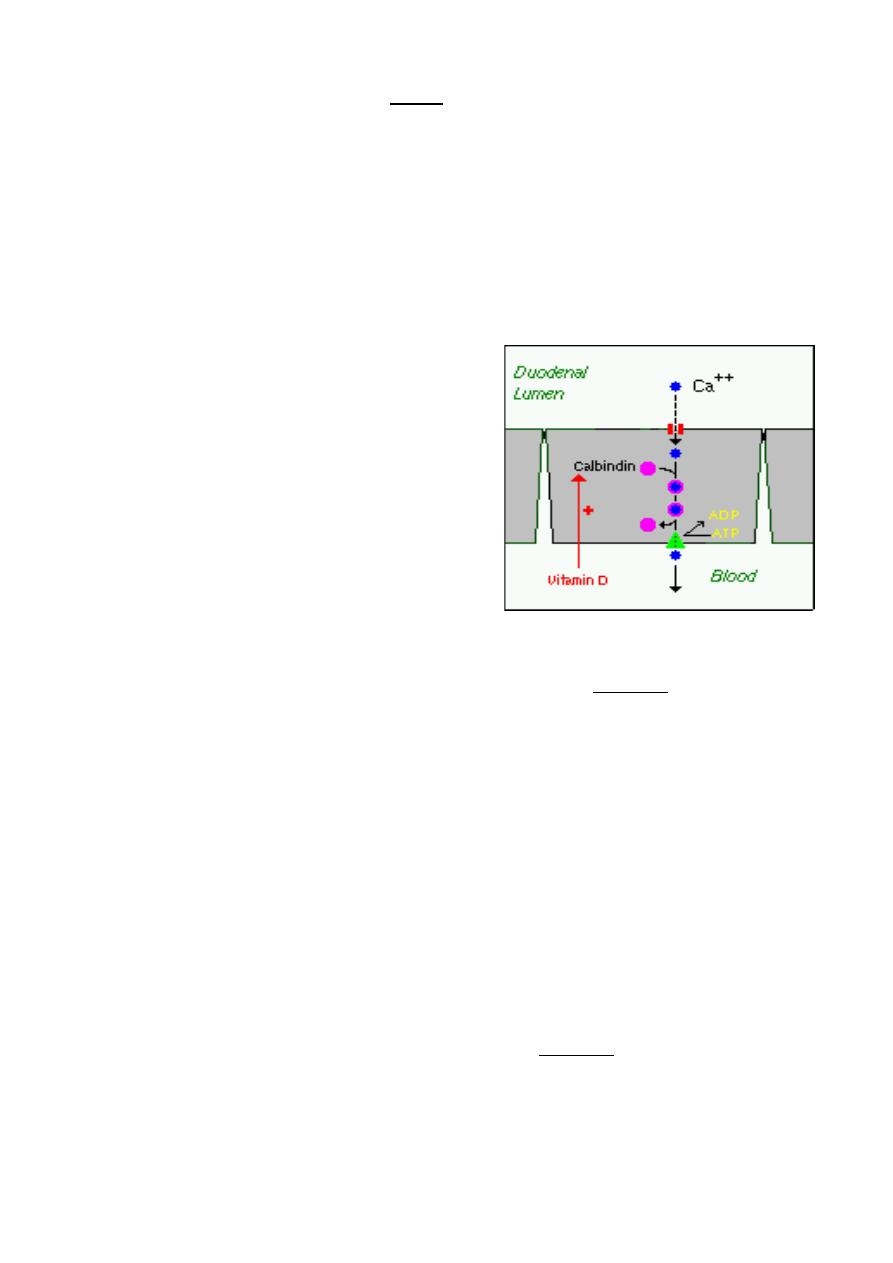
a) Calcium
The quantity of calcium absorbed in the intestine is
controlled by how much calcium has been in the diet
during recent periods of time. Calcium is absorbed
by two distinct mechanisms:
1. Active, transcellular absorption occurs only in the
duodenum when calcium intake has been low. This
process involves import of calcium into the enterocyte, transport across the cell, and
export into extracellular fluid and blood. The rate limiting step in transcellular calcium
absorption is transport across the epithelial cell, which is greatly enhanced by the carrier
protein calbindin, the synthesis of which is totally dependent on vitamin D.
Pop quiz: absorption of calcium in the small intestine is enhanced by:
1) Parathyroid hormone
2) 1, 25-DHCC
3) 24,25-DHCC
4)
None
2. Passive, paracellular absorption occurs in the jejunum and ileum, and, to a much lesser
extent, in the colon when dietary calcium levels have been moderate or high. In this case,
ionized calcium diffuses through tight junctions into the basolateral spaces around
enterocytes, and hence into blood. Such transport depends on having higher
concentrations of free calcium in the intestinal lumen than in blood.
a) Phosphorus
Phosphorus is predominantly absorbed as inorganic phosphate in the upper small
intestine. Phosphate is transported into the epithelial cells by cotransport with sodium, and
expression of this (or these) transporters is enhanced by vitamin D.
Lecture 5
Tuesday 1/10/2013
Prof. Dr. H.D.El-Yassin
2013
7
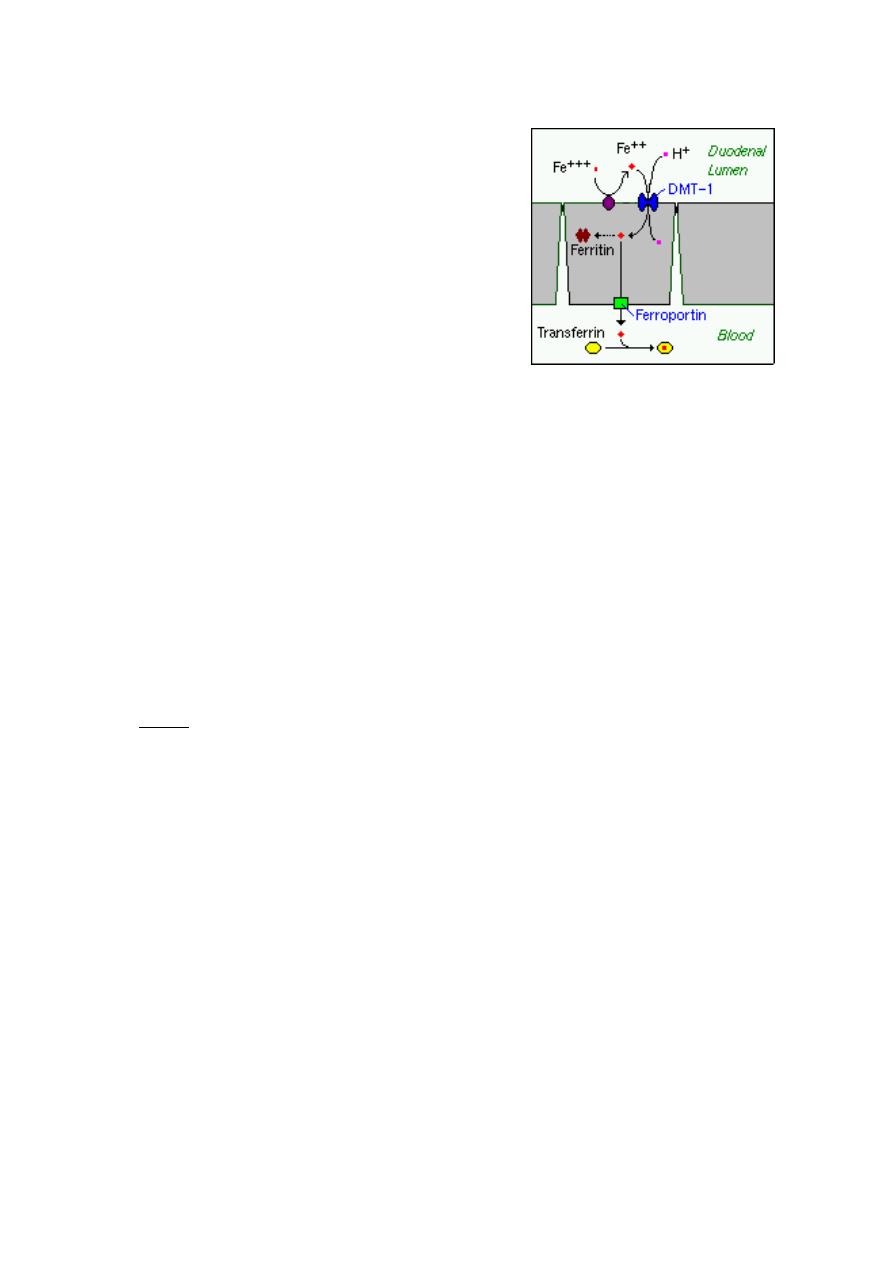
b) Iron
Iron homeostasis is regulated at the level of intestinal
absorption, and it is important that adequate but not
excessive quantities of iron be absorbed from the diet.
Inadequate absorption can lead to iron-deficiency
disorders such as anemia. On the other hand,
excessive iron is toxic because mammals do not have a
physiologic pathway for its elimination.
Iron is absorbed by villus enterocytes in the proximal
duodenum. Efficient absorption requires an acidic
environment.
Ferric iron (Fe+++) in the duodenal lumen is reduced to its ferrous form through the action
of a brush border ferrireductase. Iron is then co transported with a proton into the
enterocyte via the divalent metal transporter DMT-1. This transporter is not specific for
iron, and also transports many divalent metal ions.
Pop quiz: in the small intestine, iron is absorbed in the form of :
1) Ferric
2) Ferrous
3) Both
4) None
Once inside the enterocyte, iron follows one of two major pathways:
•
Iron abundance states: iron within the enterocyte is trapped by incorporation into
ferritin and hence, not transported into blood. When the enterocyte dies and is
shed, this iron is lost.
•
Iron limiting states: iron is exported out of the enterocyte via a transporter
(ferroportin) located in the basolateral membrane. It then binds to the iron-carrier
transferrin for transport throughout the body.
a) Copper
There appear to be two processes responsible for copper absorption:
i) a rapid, low capacity system and
ii) a slower, high capacity system, which may be similar to the two processes seen
with calcium absorption.
Many of the molecular details of copper absorption remain to be elucidated. Inactivating
mutations in the gene encoding an intracellular copper ATPase have been shown
responsible for the failure of intestinal copper absorption in Menkes disease.
A number of dietary factors have been shown to influence copper absorption. For
example, excessive dietary intake of either zinc or molybdenum can induce secondary
copper deficiency states.
Lecture 5
Tuesday 1/10/2013
Prof. Dr. H.D.El-Yassin
2013
8
b) Zinc
Zinc homeostasis is largely regulated by its uptake and loss through the small intestine.
Although a number of zinc transporters and binding proteins have been identified in villus
epithelial cells, a detailed picture of the molecules involved in zinc absorption is not yet in
hand.
A number of nutritional factors have been identified that modulate zinc absorption. Certain
animal proteins in the diet enhance zinc absorption. Phytates from dietary plant material
(including cereal grains, corn, rice) chelate zinc and inhibit its absorption. Subsistence on
phytate-rich diets is thought responsible for a considerable fraction of human zinc
deficiencies.
Conclusion
1. The mechanism by which amino acids are absorbed is conceptually identical to that
of monosaccharides
2.
Triglyceride molecules must be enzymatically digested to yield monoglyceride and
fatty acids, both of which can efficiently diffuse into the enterocyte
3. examples of clinical disorderes of the above mechanisms are mentioned in the text..
