AFTER MID
TOTAL LEC: 36
Gynaecology
Dr. Yusra
Lec 36 - Principles of Chemotherapy
DR. YUSRA - LEC 5
مكتب املدينة
Principles of cancer therapy
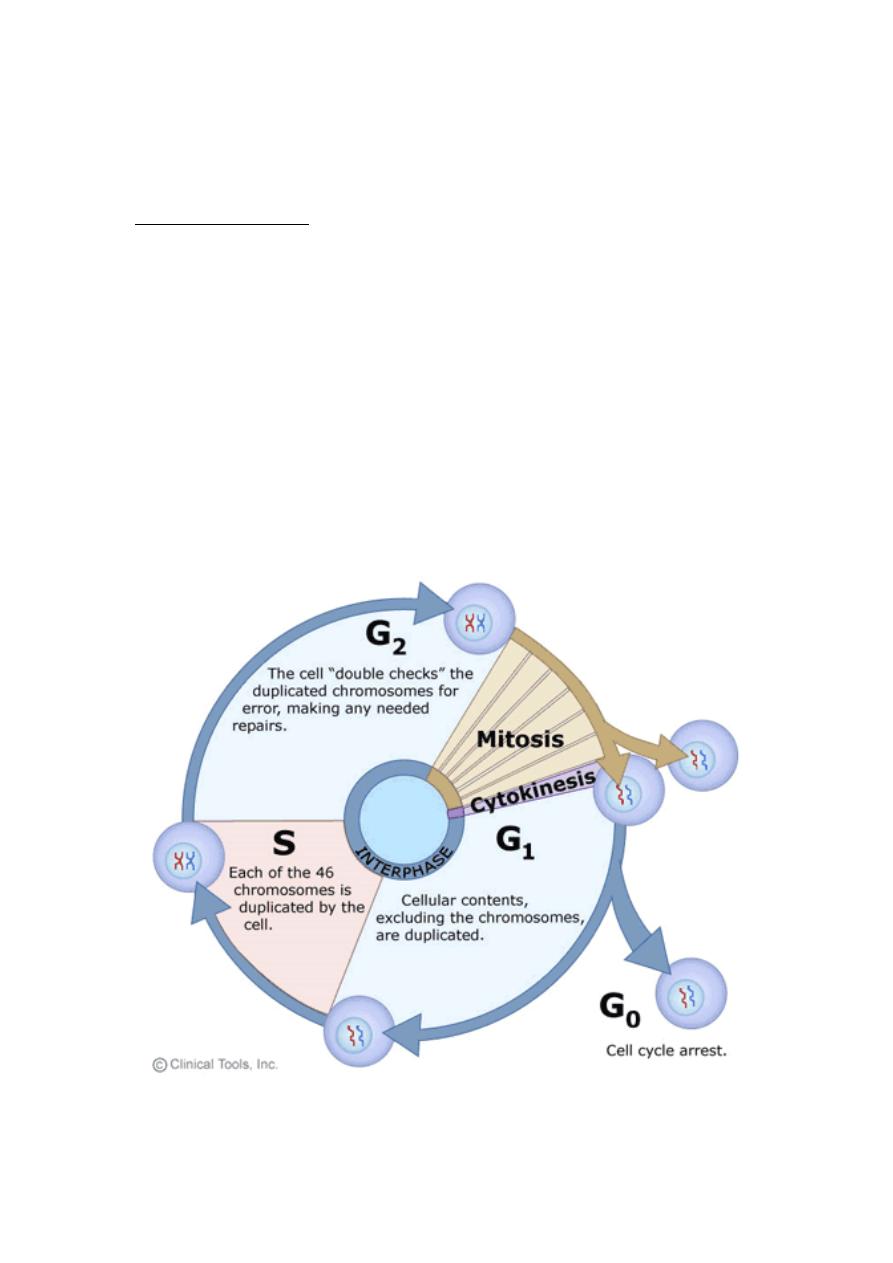
Cellular biology
There are two distinct phases in the life cycle of all cells which are
mitosis (M phase) and interphase (the interval between successive
mitoses).
Interphase is subdivided into three phases: G1 phase (of variable
duration during which the diploid cells increase their supply of proteins
and synthesize RNA) S phase (shorter duration and involves duplication
of DNA), and G2 phase (the cells continue to grow and are tetraploid).
Some cells leave the cycle temporarily or permanently and enter the G0
or resting phase.
The growth fraction of the tumor is the proportion of actively
dividing cells. Chemotherapeutic agents and radiation kill cells by first –
order kinetics, which means that a constant proportion of cells is killed
for a given dosage regardless of the number of cells present.
Chemotherapy
Classification of chemotherapeutic agents
1) Cell cycle – nonspecific agents: such as alkylating agents, cisplatin
, and paclitaxel.
2) Cell cycle-specific agents: for example hydroxyurea and
methotrexate act during S phase, bleomycin acts in G2 and vinca
alkaloids act in M phase.
Principles of chemotherapy
1) They are selected on the basis of previous experience.
2) The drugs are usually given systemically so the tumor can be
treated regardless of its anatomic location.
3) To increase the local concentration, certain drugs may
occasionally be administered topically by intraarterial infusion or
by intrathecal or intracavitary.
4) Chemotherapy is generally not administered if the white cell
count is less than 3000/mm3 or if the platelet count is less than
100,000/ mm3.
5) Nadir blood count (describes the lowest value of blood counts
after chemotherapy) are obtained 7 to 14 days after treatment,
and subsequent doses may need to be reduced.
6) Dosage reduction may also be necessary because of toxicity to
other organs , such as GIT, liver or kidneys
7) Resistance to chemotherapy may be temporary or permanent.
Temporary resistance is mainly related to the poor vascularity of
bulky tumors and an increasing proportion of cells in the relatively
resistant G0 phase.
Permanent resistance mainly results from spontaneous mutation
to phenotypic resistance and occurs most commonly in bulky
tumors. Permanent resistance may also be acquired by frequent
exposure to chemotherapeutic agents.
Chemotherapeutic agents
The common agents used in gynecological malignancies are:
§
Alkylating agents: Cyclophosphamide
§
A
ntimetabolites: Methotrexate
§
Antibiotics: Bleomycin ,Doxorubicin
§
Plant alkaloids: Vincristine
§
Other drugs: Cisplatin
Radiation therapy
Radiation may be defined as the propagation of energy through
space or matter.
It includes two types: electromagnetic and particulate.
Electromagnetic radiation
o
Visible light
o
Infrared light
o
Ultraviolet light
o
X-rays (photons)
o
Gamma rays (photons)
Particulate radiation
Particulate radiation consists of moving particles of matter, their
energy is equivalent to the kinetic energy of moving particles. The
particles include the following: Neutrons, Protons, Electrons
Unit of radiation measurement
The Gray is equivalent to an absorbed energy of 1 joule per
kilogram of absorbing material
Biologic considerations
1.
Ionization of molecules: radiation damage is caused by the
ionization of molecules in the cell with the production of free
radicals.
2.
Oxygen effect: in the absence of oxygen, cells show a twofold to
threefold increase in their capacity to survive radiation exposure.
3.
Pharmacologic modification of the effect of radiation: a variety of
chemical compounds are capable of enhancing the lethal effects
of radiation.
4.
Time - dose fraction of radiation: a dose that is too high sterilizes
the tumor but results in an unacceptably high complications rate.
if the interval between each fraction increases, the total dose
must be increased as well to produce the same biologic effect.
Major factors influencing the outcome of radiation therapy
•
Normal tissue tolerance
•
Malignant cell type
•
Total volume irradiated
•
Total dose delivered
•
Total duration of therapy
•
Number of fractions
•
Type of equipment used
•
Tissue oxygen concentration
Modalities of radiation therapy
In general, there are two radiation techniques: Teletherapy and
Brachytherapy. In Teletherapy, an external device outside the patient's
body is used, as with external beam techniques. In Brachytherapy, the
radiation source is placed either within or close to the target tissue, as
with intracavitary and interstitial techniques.
External beam therapy
External radiation allows a uniform dose to be delivered to a given
field and is used to shrink a large tumor mass before brachytherapy.
Intracavitary radiation
It is used particularly in the treatment of cervical and vaginal
cancer. All applicators now in use should be “after loaded” which means
that they are placed in the patient and their position checked by
radiography before the radioactive substance is loaded into the
applicator.
Interstitial radiation
In which the radioactive source is placed directly in the tumor, it
may be delivered by removable or permanent implants. Permanent
implants are used for inaccessible tumors, they use radioisotopes such
as radon 222 or iodine 125. Removable implants are placed in tumors
that are accessible (cervical or vaginal tumors).
Complications associated with radiation
Acute complications: Cellular swelling, tissue edema, tissue necrosis,
acute cystitis, proctosigmoiditis, enteritis, and bone marrow depression.
Chronic complications: occur 6 months or more after radiation which
are:
a) Radiation enteropathy: proctosigmoiditis, ulceration, rectovaginal
fistula, rectal or sigmoid stenosis, small bowel injuries.
b) Vaginal vault necrosis
c) Urological injuries: hemorrhagic cystitis and fistula
Hormonal therapy
The estrogen receptor (ER) status of primary and metastatic
breast cancer has shown therapeutic and prognostic significance. and
Both (ER) and progesterone receptor (PR) status of endometrial cancer
are also of significance.

Clinical applications
Estrogen exposure increases the production of both ER and PR,
where as progesterone inhibits their production. In breast cancer,
patients whose tumors contain both ER and PR have an 80% response
rate to hormonal manipulation. An objective response to progestin
therapy occurs in about one third of patients with recurrent or
metastatic endometrial carcinoma.
Pain management
Pain in gynecologic cancer may be the result of soft tissue
infiltration, bone involvement, neural involvement, muscle spasm,
infection within or near tumor masses, or bowel colic.
Peripherally acting drugs such as acetaminophen (paracetamol)
should rarely be omitted from analgesic regimes, and rectal
suppositories are useful if oral intake is not appropriate. Opioid use will
be necessary for severe pain.
Controlled - release morphine tablets represent a significant
advance in convenience of administration as they need to be given only
every 12 to 24 hours.
When pain is neurogenic in origin, an opioid and a peripherally
acting drug should usually be supplemented by a tricyclic
antidepressant, an anticonvulsant or a corticosteroid.
End of life issues
When it becomes clear that the patient is dying, the goal is to
control symptoms. Any unnecessary tube or equipment should be
removed. Nursing care should focus on pressure areas, mouth care and
sublingual lorazepam if the patient is agitated.
