Dr.Waleed
lecture: 4
1
PLEURAL TUMORS:
o They are classified as primary and secondary tumors.
PRIMARY PLEURAL TUMORS
Are Mesotheiloma which may be:
1. Localized benign
2. Diffuse Malignant
MALIGNANT MESOTHELIOMA:
causes chest pain, bloody pleural effusion and chest X-ray findings of diffused
pleural thickening with nodularity and limited pleural effusion.
- There is a possible relationship with asbestos exposure .
- Metastases are uncommon. Death usually occurs within 1-2 years.
- It has a poor response to surgery, radiotherapy and chemotherapy.
o Pleural involvement by metastatic diseases is more common than primary tumor
and usually comes from lung, breast and stomach.
BENIGN TUMORS OF TRACHEA AND BRONCHI:
Are rare, more in males. They are slowly growing.
Their presentation is as a result of luminal obstruction or mucosal irritation.
Patients may present with dyspnea, cough and haemoptysis. A sub
glottictumor presents with stridor.
The diagnosis is by bronchoscopy and treatment is surgical excision.
e.g. Papilloma, Haemangioma, Chondroma and Fibroma
Bronchial Adenomas: (Neither benign nor malignant)
1. Bronchial Carcinod.
2. MucoepidermoidTumors.
3. Adenoid Cystic Carcinomas (Cylindromas).
Pleural tumors
2016
2
4. Mucous Gland Adenomas.
The first three are potentially malignant, the 4th is benign
The first three are slowly growing, invade locally and surgical excision is the
treatment of choice.
BRONCHIAL CARCINOID TUMORS:
Resemble intestinal carcinoid as the cytoplasm of their cells contains
neurosecretory granules. In the bronchus these tumors arise from the neuro
endocrine argentafin cells of bronchial mucosa (Kultchitsky's cells). They
are grouped among APUD tumors (Amine Percursor Uptake
Decaboxylation). They are capable of producing a number of hormones
likeSerotonin, histamine and gastrin.
They are slowly growing tumors, but sometime they are aggressive termed
(atypical carcinoid).
They present with cough, haemoptysis and dyspnea.
Carcinoid Syndrome
is a rare; presents with episodes of flushing, diarrhea and in addition to the
systemic manifestations, there may be cardiac manifestations.
Elevated 5-HIAA may be detected in the urine, which may bediagnostic.
Bronchoscopic appearance is diagnostic and severe bleeding may follow a
biops.
Surgical excision is the treatment of choice.
CARCINOMA OF THE LUNG:
Affects both sexes, It is however commoner in men.
It has poor prognosis.
Pleural tumors
2016
3
The incidence has shown a marked rise during recent years partly because
of improved methods of diagnosis and partly due to:
1. Excessive cigarette smoking, both active & passive smoking are implicated.
2. Inhalation of irritants, such as silica, cobalt dust .
Pathology:
A. Central type is the commonest (75%). It arises in one of the main bronchi or
their primary division leading to bronchial obstruction with secondary changes in
the lung such as atelectasis.
B. Peripheral type (25%) arises from the smaller bronchi and remains symptom
less for long time .
Histologically:
Squamous cell Carcinoma (SCC): 60%, smoker, centrally located,
metastasizes to mediastinal& supraclavicular LN.
Adenocarcinoma: 15%, located peripherally, more in women.
Tends to metastasizes to the liver, brain, bone & adrenals in addition to the LN.
Undifferentiated carcinoma: (oat) cell carcinoma and large cellcarcinoma
(20-30%) which includes small ma.
Alveolar cell carcinoma: located peripherally, metastasizes to the liver and
adrenals.
Recent classification: Non small & small cell carcinoma.
SUPERIORSULCUS TUMOR OF PANCOAST:
It is a low grade epidermoid carcinoma that grows slowly andmetastasize late,
infiltrates and involves lower root of Brachial plexus, intercostal nerves, Cervical
sympathetic nerves & eroding the upper ribs, producing pain in the shoulder &
Horner's syndrome.
Pleural tumors
2016
4
Clinical features:
1. Cough, dry or productive.
2. Haemoptysis.
3. Chest pain.
4. Dyspnea.
5. Pleural effusion.
6. Anorexia & loss of weight.
7. Clubbing of the fingers.
8. Hoarseness of the voice (recurrent LN).
9. Dysphagia (involvement of the esophagus).
10. Hormonal syndromes: ectopic ACTH, ADH, hypercalcaemia, carcinoid
syndrome.
Diagnosis:
Clinical, sputum cytology.
Chest X-ray, CT chest.
Bronchoscopy, BAL (bronchoalveolar lavage), bronchial brush & biopsy.
FNAC or Tru-cut biopsy, pleural fluid aspiration & cytology.
Diagnostic thoracoscopy&mediastinoscopy
TNM classification for staging
Signs of inoperability (*IMP)
1-Bloody pleural effusion .positive for malignant cells
2-Horner’s syndrome .
3-Vocal cord paralysis
4-Phrenic nerve palsy(elevated hemi diaphragm)
5-SVC obstruction
Pleural tumors
2016
5
6-Distant metastasis
7-If during surgery ,the tumor locally spreading or cannot be remover technically
or fixed to the PA or to the heart ,it is technically irresectable
Treatment:
1. Surgery: more than 50%of the patients have distant metastases at the time of
diagnosis. 50% irresectable per operatively.
15-20% resectability rate.
Surgery: segmentecomy, lobectomy, pneumectomy.
2. Radiotherapy: pre-operative or post-operative.
3. Chemotherapy: Vincristine or Adriamycin.
Bleomycin for malignant effusion.
Differential diagnosis of a solitary lung lesion (COIN LESION):
1. Hydatid cyst.
2. Tuberculoma.
3. Angiomatous malformation (AVfistula).
4. Primary benign lesion.
5. Primary malignancy of the lung.
6. Metastatic tumors.
PULMONARY ECHINOCOCCOSIS (HYDATID CYST)
Hydatid disease of the lung is caused by the small tape worm
(TaeniaEchinococcus ) or (EchinococcusGranulosis) .

Pleural tumors
2016
6
Hydatid cyst means cyst full of water .It has a life cycle between dogs &
sheep .
Parasites in the elementary tract of the dog shed ova that excreted in the dog
faeces , contaminated the food of the sheep in which hydatid cyst will
develops in the viscera .
Including the lung .Infected sheep when slaughtered and its entrails are eaten
by dogs , the life cycle is completed .When a human being hands or food
become contaminated with canine fecal material containing ova which will
be ingested .
The parasitic larva burrow through the gastric mucosa and are carried to the
liver in the portal venous circulation where most of them filtered out to
formhydatid cyst of the liver ,
some escape the liver &lodge in the lung to form one or more hydatid cyst
which grows slowly or rapidly over years .
The cyst consists of a germinal layer & cyst fluid containing broad
capsule &scoleses .
A cellular white hyaline layers are laid down outside the cyst so that the
cyst is enclosed by a laminated cyst membrane .
As the cyst enlarged , it usually reaches the pleural surface .
Compression of the lung tissues produces a thin fibrous layer of atelectatic
lung tissue around the cyst (capsule , pericyst or adventia)
Pleural tumors
2016
7
Clinical Manifestation
A-Asymptomatic
Any smooth homogenous opacity of uniform density with clear cut border and
little or no reaction around it on a chest X-Ray is a hydatid cyst unless proved the
other wise .
B-Cough &haemoptysis
due to rupture of the cyst , or it can lead to severe dyspnea , or asphyxia ,or a hyper
sensitivity reaction ,
If the cyst get infected ,it will lead to formation of lung
abscess or bronchiectatic changes
Radiological Findings
1-Smooth homogenous opacity (Intact H.C).
2-Partial rupture (per vesicular pneumocyst).
3-Complete rupture (Water –lilly sign) .
4-Formation of lung abscess(Air –fluid level) .
5-Completely coughed out cyst(empty cavity )
6-Rupture into the pleura (hydropneumothorax)
If the cyst get infected ,it will lead to formation of lung abscess or bronchiectatic
changes .
Treatment

Pleural tumors
2016
8
Surgical
A-Inoculation means to remove it intact.
B-Aspiration &evacuation technique
C-Wedge resection or excision of the cyst with adjacent lung tissue.
D-Segmentectomy,Lobectomy or Pneumonectomy (rare ).
BRONCHIECTASIS
Is a persistent abnormal dilatation of the bronchi generally beyond the sub
segmental level , generally classified as three types cylindrical , varicose
&saccular . The left lower lobe is more commonly involved then the right lower
lobe
Aetiology :-
1-Congenital causes (25%)
2-Acquired causes (75%)
The acquired causes include
air way infection (bact. Or viral)
bronchial obstruction (F.B., neoplasm.,LN)
It present in 40% of patients with chronic middle lobe infection (middle lobe
syndrome) which involved impaired clearance of secretion mostly due to a
pressure of enlarged LN.
Pleural tumors
2016
9
CONGENITAL BRONCHIECTASIS (KARTAGNER’S SYNDROME)
It includes (Bronchiectasis ,situsinversus ,sinusitis ,sperms hypo motility ) .
It represents genetic disorder with abnormal ciliary motility so impaired
clearance of sputum with the resultant bronchiectasis .
Clinical manifestation :-
The onset is mostly in childhood whereas symptoms generally appear in the
second or third decade of life .
The disease is more common in females .
Major symptom cough with the production of purulent sputum with fetor
oris .
50% of the patients presented with haemoptysis .
Others present with repeated respiratory tract infection .,others develop
osteoarthropathy& finger clubbing which will resolve with treatment .
Diagnosis :-
1-History chronic cough with purulent sputum.
2-Plain CXR may shows prominent vascular marking .
3-Bronchoscopy to diagnose obstructive lesion & to obtain bronchial wash for
C&S test .
4-Bronchography through giving radio opaque dye through the bronchoscope &
into bronchial tree ,now replaced completely by CT.
Pleural tumors
2016
10
5-Chest CT is the single non invasive tool for both diagnosing &assessing the
severity of the disease .
6-X-Ray paranasl sinuses to treat any excistinginfection .
7-Pulmonary function tests very important specially in pre operative assessment .
Treatment :-
Medical treatment is the main stay of treatment ,it includes antibiotics ,
chest physiotherapy &postural drainage .
Surgical treatment in cases of failure of medical treatment and it includes
segmentectomy , lobectomy &pneumonectomy
LUNG ABSCESS
It is a localized area of suppuration and cavitations in the lung.
It includes TB ,mycotic or parasitic cavitations ,bronchiectasis ,ruptured
infected hydatid cyst , even pulmonary infarction with abscess formation
&cavitating tumors
Simple lung abscess (pyogenic)
can occurs as a result of aspiration of a septic debris from the oropharynx into
the lung or following dental or tonsillar operations .
Esophageal diseases
that lead to regurgitation &subsequent aspiration of esophageal content into the
lung is another cause.
Usually the aspiration is into the RMB leading to severe pnemonitis and
liquefaction may occurs .As the liquefied necrotic material empties through the
Pleural tumors
2016
11
bronchus , a necrotic cavity containing pus and air is formed .The organism
responsible may be streptococcus , staphylococus&eschrescia coli .
Clinically
cough & foul smelling sputum
fever , pleuritic chest pain
night sweat & weight loss
in severe cases dyspnea & cyanosis
Chest X-Ray (*imp)
Can shows the characteristic air fluid level ,may associated with
pleural thickening , pneumothorax
CT chest is helpful in demonstrating the abscess .
TREATMENT
1- Primary treatment is Medical
Prolonged antibiotics treatment
Bronchoscopy useful to remove a FB or drainage of abscess
2-Surgery indicated in
o Failure of medical treatment
o Massive haemoptysis
o persistent of a thick wall cavity
Pleural tumors
2016
12
o when malignancy is suspected
o when empyaema develops
Complications :-
Empyaema , septicaemia ,metastatic brain abscess ,bronchogenic spread
&development of chronicity
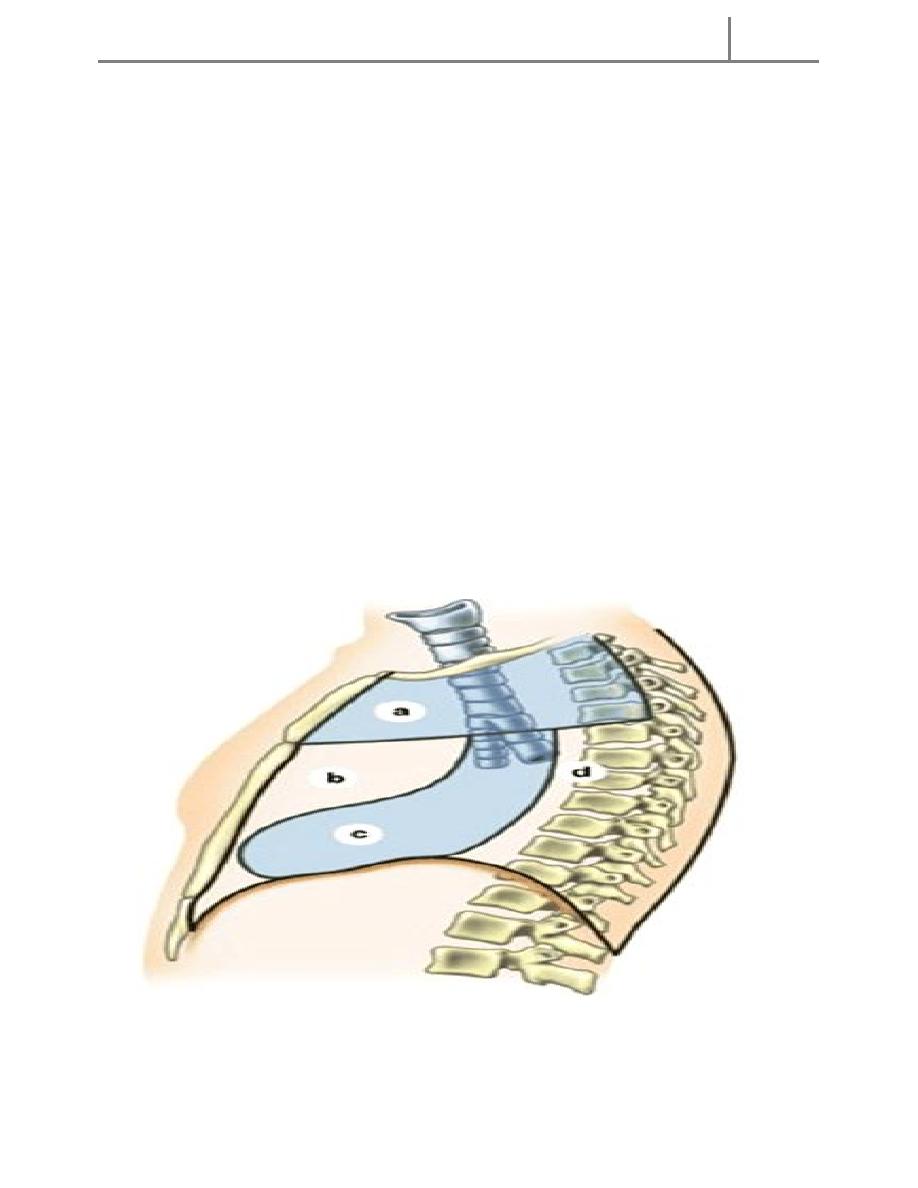
THE MEDIASTINUM
Mediastinum :-
It is part of the chest , which is bounded above by the thoracic inlet , below
by the diaphragm , anteriorly by the sternum , posteriorly by the dorsal
vertebrae , and laterally by mediastinal pleura
.It is divided by a transverse plane between the angle of Lewis anteriorly
and the lower border of the 4
th
dorsal vertebra posteriorly into superior and
inferior medistinum ,and the inferior
medistinum is further subdivided by the presence of the pericardial sac into
anterior , middle and posterior mediastinum
Mediastinal tumors or cysts occur in a chractersticlocation so a mass in
the superior medistinum is mostly thymomaor lymphoma ,while a
neurogenic tumor occur mostly in the posterior mediastinum
.Pericardial cyst or bronchogenic cysts occur in the middle mediastinum
.(*MCQs)
Pleural tumors
2016
13
MEDIASTINITIS
Causes :-
1-Perforation of the esophagus or leakage from anastomosis .
2-Extension from a nearby infection (lung , vertebra ,pleura ).
3-Following median sternotomy for cardiac surgery .
Clinical manifestations :-
Fever , tachycardia , chest pain
Barium swallow is useful to demonstrate esophageal perforation.
Esophagoscopy will confirms the perforation .
Chest X-ray & CT –scan of great value in the diagnosis .
Treatment :-
1-Treatment of the cause .
2-Antibiotics according to culture and sensitivity .
3-Tube thoracostomy to drain any pleural collection .
4-Supportive therapy .
هاي محاضرة لخ
Pleural tumors
2016
14
Surgical Treatment of Pulmonary Tuberculosis
Indications :-
1-Massive or recurrent haemoptysis . Surgery is indicated to remove the
source of bleeding .
2-Broncho pleural fistula
3-Open cavity with positive sputum resistant to 3-6 months of treatment .
4-TB bronchiectasis .
5-When malignancy is suspected as TB and malignancy can co exist
.Carcinoma can arise in TB scar (Scar carcinoma ) .
5-Patients with (Trapped lung syndrome ) after chronic empyaema .
It includes segmetectomy ., lobectomy ., or pneumonectomy ., or to remove
thickened adherent parietal and visceral pleura( decortication ) alone or in
combination with pulmonary resection .
Superior Vena Cava Obstruction
A number of benign and malignant lesions involving the mediastinum may lead
to obstruction of SVC with the production of the classical syndrome
Which characterizes by elevation of the venous pressure and edema of the face
, neck and upper extremity with the appearance of the dilated venous
chandelles in the chest wall and cyanosis .It may be caused by the carcinoma of
the lung and in (25%) of the cases ,it may be caused by a benign lesion such as
idiopathic mediastinal fibrosis .
Congenital Deformities of the Chest Wall
Pectus Excavatum in which the costal cartilages developed in a concave
position and thus depress the sternum towards the vertebral column. Few
patients may have cardio- respiratory problems . The best time of correction
obtained at the age of 2-3 years .

Pleural tumors
2016
15
Pectus carinatum ( Pigeon Breast )
Less common , consists of protrusion of the sternum ,caused by an upward
curve in the lower costal cartilages , generally 4
th
. To 8
th
. Cartilages pushing
the sternum forward .Surgery is the treatment of choice in symptomatic patients
.
Thoracoscopy
It is the examination of the pleural cavity with an endoscope .
Hans Jacobaeus was the originator of the thoracoscopy in 1910 .It is done
under general anesthesia with double lumen intubation ,
Indications
1-Diagnostic
1-Diagnosis of pleural diseases
2-Evaluation of carcinoma of the bronchus .
3- Biopsy of a discrete pulmonary nodules .
4-Evaluation of mediastinal mass .
Therapeutics :-
1-Treatment of pleural effusion .
2-Treatment of recurrent pneumothorax .
3-Removal of intra- pleural FB .
4-Debridement of empyaema space .
5-Dorsal sympathectomy .
There is no absolute contra indications for thoracoscopy .
دقايق وكملو
Pleural tumors
2016
16
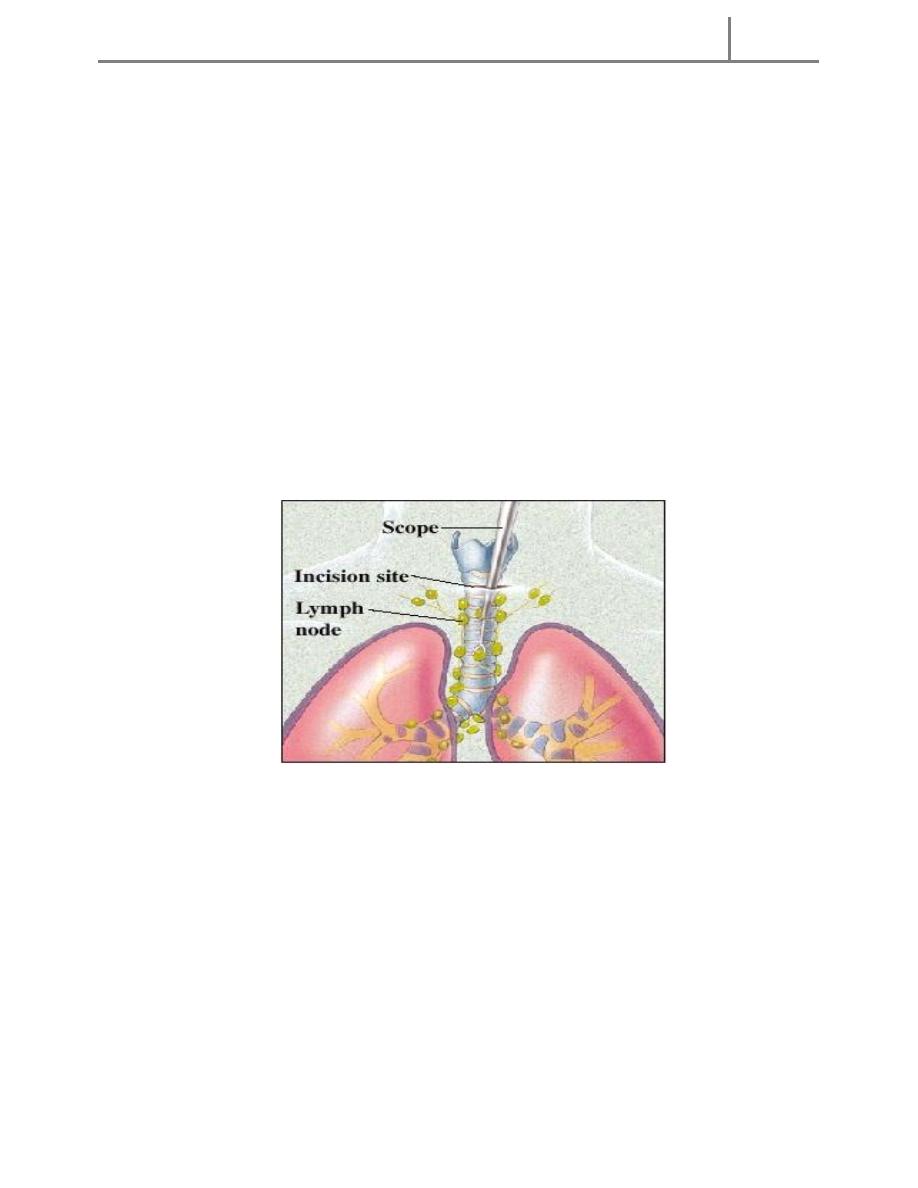
Mediastinoscopy
Is a surgical procedure that enables visualization of the contents of the
mediastinum, usually for the purpose of obtaining a biopsy . Mediastinoscopy is
often used for staging of lymph node of lung cancer or for diagnosing other
conditions effecting structures in the mediastinum such as sarcoidosis or
lymphoma .
It involves making an incision approximately 1 cm above the suprasternal notch
of the sternum , or breast bone. Dissection is carried out down to the pretracheal
space and down to the carina . A scope (mediastinoscope) is then advanced into
the created tunnel which provides a view of the mediastinum. The scope may
provide direct visualization or may be attached to a video monitor.
Mediastinoscopy provides access to mediastinal lymph node
Mediastinoscopy is used to explore the superior and middle part of the
mediastinum. a. Superior mediastinum. b. Anterior mediastinum. c. Middle
mediastinum. d. Posterior mediastinum
Mediastinoscopy is usually performed in a hospital under general anesthesia..
Once the patient is under general anesthesia, a small incision is made, usually
Pleural tumors
2016
17
just below the neck or at the notch at the top of the sternum. The surgeon may
clear a path and feel the person's lymph nodes first to evaluate any
abnormalities within the nodes. Next, the physician inserts the mediastinoscope
through the incision. The scope is a narrow, hollow tube with an attached light
that allows the surgeon to see inside the area. The surgeon can insert tools
through the hollow tube to help perform biopsies. A tissue sample from the
lymph nodes or a mass can be removed and sent for study under a microscope,
or to a laboratory for further testing.
The person will remain in the surgerical recovery area until the effects of
anesthesia have lessened and it is safe to leave the area. The entire procedure
should require about an hour, not counting preparation and recovery time.
Studies have shown that mediastinoscopy is a safe, thorough, and cost-effective
diagnostic tool with less risk than some other procedures.
Aftercare
Following mediastinoscopy, patients will be carefully monitored and watched
for changes in vital sign , or symptoms of complications from the procedure or
anesthesia. The patient may have a sore throat from the endotracheal tube,
experience temporary chest pain, and have soreness or tenderness at the incision
site.
Risks
Complications from the actual mediastinoscopy procedure are relatively rare.
The overall complication rates in various studies have been reported in the
Pleural tumors
2016
18
range of 1.3–3%. However, the following complications, in decreasing order of
frequency, have been reported:
-hemorrhage
-pneumothorax (air in the pleural space)
-recurrent laryngeal nerve injury, causing hoarseness
-infection
-tumor implantation in the wound
-phrenic nerve injury (injury to a thoracic nerve)
-esophageal injury
-chylothorax (chyle is milky lymphatic fluid in the pleural space)
-air embolism (air bubble)
Chest Trauma
Causes :-
1-Blunt Trauma
2-Pentrating & perforating injuries
3-Blast injuries
Classification
1-Chest wall injury
Superficial chest wall injury affecting the skin and muscles of the chest wall
without affecting the ribs or the underlying pleura as proved by normal chest x-
ray .
Management is to arrest any bleeding and wound debridement with primary
closure if possible .
Pleural tumors
2016
19
2-Ribs & Sternal injuries
May lead to
Single rib fracture the important thing is to relief pain by analgesic , chest wall
strapping or intercostal nerve block
or Multiple ribs fractures , flail chest in that case four or more ribs are
fractured anteriorly and posteriorly which lead to paradoxical respiratory
movement with the resultant hypoxia and severe dyspnea that nictitates
emergency intubation and assisted ventilation and if the patient needs prolonged
intubation for more than one week then tracheostomy is indicated .
3-Pleurl injuries
Can lead to
A-Pneumothorax which can be partial or complete
closed or open sucking
or tension pnemothorax .
B-Haemothorax may be mild or severe and may be with pneumothorax
4-Pulmonary injuries
Trauma can lead to pulmonary contusion with interstitial edema which may
lead to consolidation of the lung tissues and can be manage by antibiotics
administration and clearing of secretion
5-Tracheo-bronchial injuries
It may lead to crushing or complete tracheal separation which needs immediate
air way management and repair of the trachea.
Bronchial injuries can be so severe that it lead to complete separation of the
bronchus which lead to pneumothorax with severe air leak, haemoptysis
&haemothorax .Bronchoscopy will establish the diagnosis and surgery is
mandatory to reanastomosed the bronchus
6-Great vessels injuries
Injuries to the thoracic aorta and its branches can occur mainly with
deceleration injury . Most patients with ruptured aorta die immediately but in
Pleural tumors
2016
20
10% of patients the per aortic tissues and pleura are able to maintain the
intravascular pressure producing false aneurysms ,which can be diagnose by CT
angiography and needs immediate surgery
7-Diaphragmatic injuries
Trauma can lead to rupture of the diaphragm ,most commonly the left side
affected ,leading to herniation of the viscera .Stomach is the most frequent
organ to herniated followed by the transverse colon , spleen leading to collapse
of the lung and mediastinal shift which can be seen on chest X-ray .Barium
study is of great help in the diagnosis .Treatment surgery through abdominal ,
thoracic ,combined approach or by laparoscopy
8-Esophageal injuries
Thoracic esophagus rarely injured but mostly the cervical esophagus due to
penetrating injury to the cervical region .Pain and dysphagia ,sometime fever
.Diagnosis can be established by contrast study which will visualized the site of
perforation.
Treatment may be conservative by intravenous fluid , heavy antibiotics &
NBM for 5-7 days which may be enough to seal the perforation , otherwise
surgery is indicated to close the perforation .
9-Cardic injuries
May vary from superficial laceration to transmural damage which lead to atrial
or ventricular septal defect or coronary artery injury .The patient may present
with dyspnea ,hypotension & tachycardia .Diagnosis can be accomplished by
Echocardiography .
Management includes resuscitation & immediate thoracotomy or sternotomy to
treat the injury
Thoracotomy in chest trauma
90% of chest injuries can be treated by chest tube (tube thoracostomy or intercostal
drain (ICD) ).
Thoracotomy may be …immediate (resuscitative thoracotomy )
Pleural tumors
2016
21
……emergency
.. … elective
Penetrating thoracic injury
- Traumatic arrest with previously witnessed cardiac activity (pre-hospital or
in-hospital)
- Unresponsive hypotension (BP < 70mmHg)
Blunt thoracic injury
- Unresponsive hypotension (BP < 70mmHg)
- Rapid exsanguinations from chest tube (>1500ml)
Immediate(urgent) thoracotomy
1-Massive haemoptysis
2-Massive haemothorax / initial dain1500 ml. or more than 200 ml /hr. for few
hrs.
3-Ruptured bronchus with massive air leak
4-when great vessels injury is suspected
5- In diaphragmatic injury
6-Some cases with esophageal injury .
7-In cardiac injury
8-In some cases of flail chest .
Elective thoracotomy
1-Clotted haemothorax
2-Trapped lung syndrome
3-Big foreign body
Complications of chest injuries
1-ARDS: Syndrome of acute RF with the formation of a non –cardiogenic
pulmonary edema leading to reduced lung compliance and hypoxaemia which
Pleural tumors
2016
22
is refractory to oxygen therapy characterized by bilateral diffuse pulmonary
infiltrate on chest X-ray (white lung) .
A less severe case (ALI=acute lung injury ) which consists of a non specific
pathological changes in the lung in response to a specific insult .
2-Atelectasis
3-Infection
4-Pulmonary embolism
5-Air embolism
6-Traecheal complications
7-Cardiac arrhythmias
Poly trauma Team Members
Team leader
Anesthetist + assistant
General surgeon
Orthopedic surgeons
A/E physician
Two (2) nurses
Radiographer
Scribe (nurse or doctor)
وهاي جانت اخر محاضرة جراحة وخلصت لهنا:D
ان شاءهلل الكل تفول بالفاينل
والتنسونا بالدعاء:D
Done By: Hussein Sadun Al-Nuaimy
# سجلوني حضور
اذية وهللا اذية
