Nephrology
Dr. Mohamad hanoon
Medicine
”
Inherited glomerular diseases & Cystic kidney diseases
“
Dr.Mohamad
#5
Lecture
Total lec 42

2

3
Inherited glomerular diseases & Cystic kidney diseases
:
Inherited glomerular diseases
Uncommon diseases may affect the glomerulus in childhood,
-The most important one affecting adults is
Alport’s syndrome
- 5% of ESRD in childhood or adolescence.
- Most commonly, it is an X-linked recessive 85%,
from a mutation or deletion of the COL4A5 gene , encodes
type IV collagen
- less common, it is an autosomal recessive disease Mutations in COL4A3
or COL4A4 genes
- The accumulation of abnormal collagen results in a progressive
degeneration of the GBM
1.
Alport’s syndrome
Affected patients present with
- haematuria,
- proteinuria (less than 1–2 g/day),
- progressive to ESRD in their late teens or twenties.
Female carriers usually have haematuria but rarely develope significant renal disease.
- Cochlea involvement ,
high-frequency sensorineural deafness
- Ocular involvement
15% anterior lenticonus and macular and perimacula retinal flecks
4
Alport’s syndrome
• No specific treatment is available,
• early , ACE inhibitors may attenuate proteinuria.
• experimental ;- that mesenchymal stem cells can transdifferentiate into podocytes
and repair basement abnormalities and slow the progression.
• but patients with Alport’s syndrome are good candidates for renal replacement
therapy RRT, as they are young and usually otherwise healthy.
•
Some of these patients develop an immune response to the normal collagen
antigens present in the GBM of the donor kidney , and in a small minority anti-GBM
disease develops and destroys the allograft
.
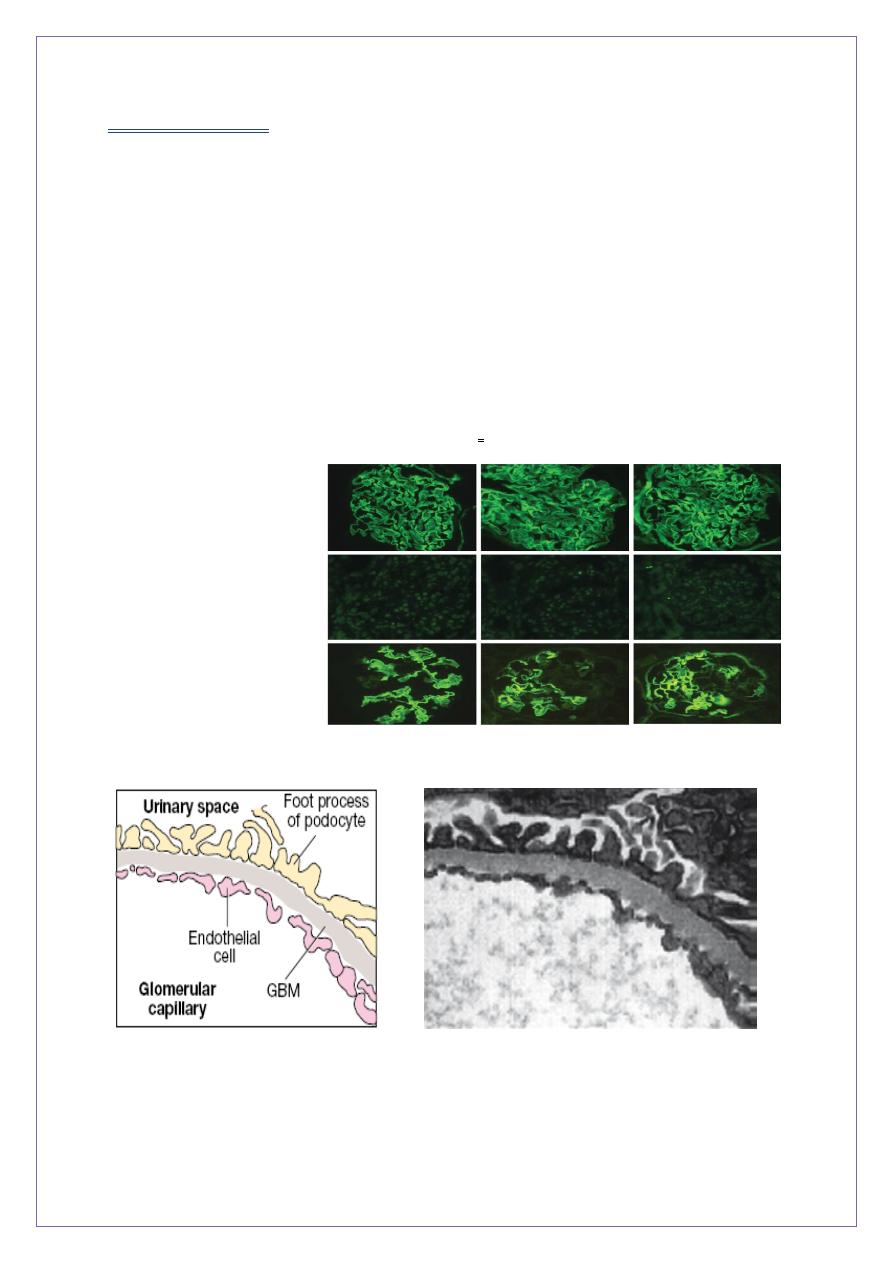
Immunohistochemistry
(GBM)
X-linked Alport’s
syndrome
Normal
male XL
female AS
Diagrammatic structure of
the normal GBM...
The normal GBM (electron micrograph)
contains mostly the tissues pecificα3, α4 and
α5 chains of type IV collagen
5
Ocular abnormalities in Alport’s
syndrome.
A, Anterior lenticonus shown by slit-lamp
ophthalmoscopy.
B, Perimacular flecks
2. Thin GBM disease
• There is glomerular bleeding, usually only at the microscopic or dipstick level,
• Without hypertension, proteinuria or reduction of GFR.
• light microscopy The glomeruli appear normal
• electron microscopy the GBM is abnormally thin.
• This autosomal dominant condition accounts for a large
• proportion of ‘benign familial haematuria’
• excellent prognosis.
• Some families may be carriers of autosomal recessive Alport’s syndrome but this
does not account for all cases.
•
In Alport’s syndrome this network is
disrupted and replaced by α1 and α2
chains. Although the GBM
•
appears structurally normal in early life, in
time thinning appears, progressing to
thickening, splitting and degeneration
6
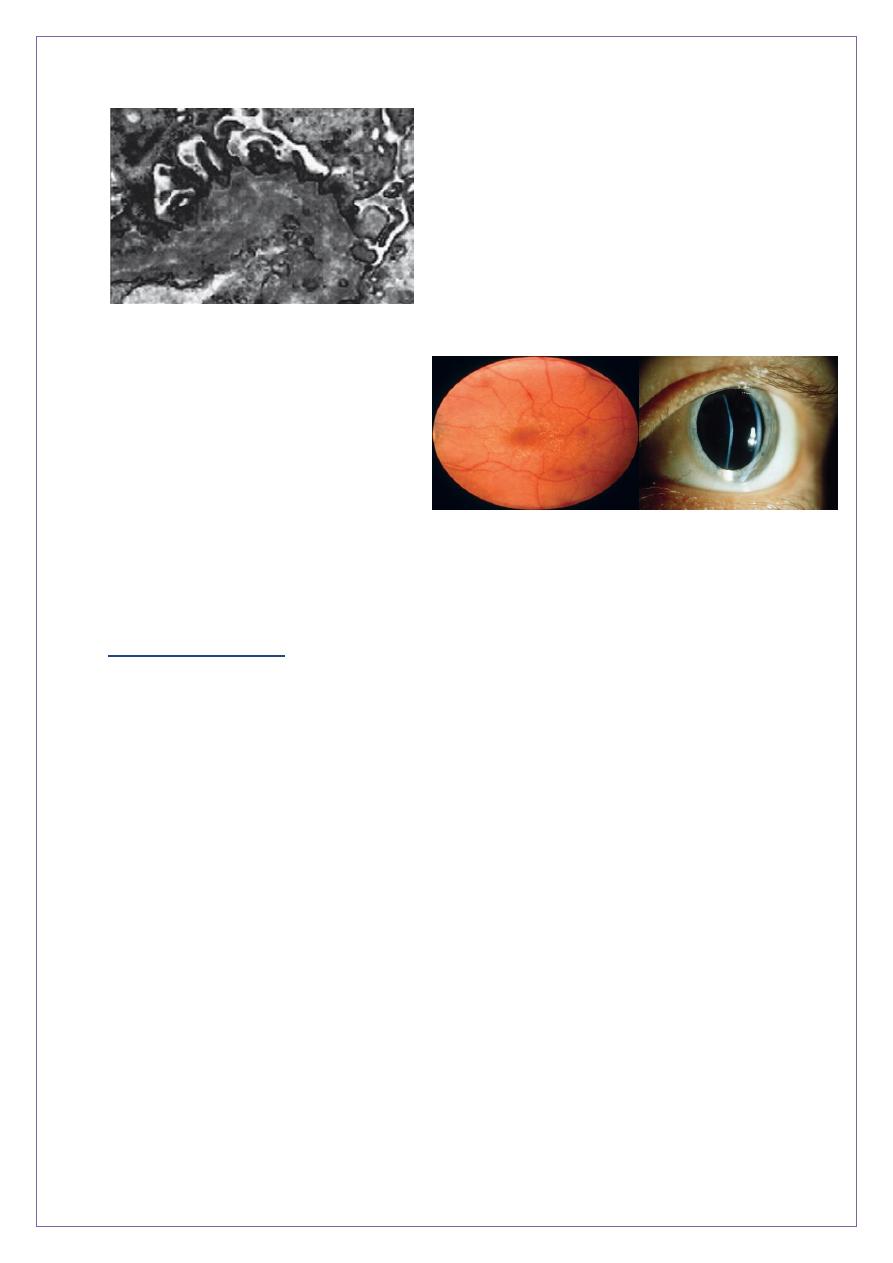
Cystic kidney
diseases
Cystic kidney diseases
Solitary or multiple simple renal cysts
:-
are common, with advancing age:-
50 % of > 50 years have one or more such cysts.
No special significance except in the Diff. Dx of renal tumours.
often asymptomatic, accidental finding on U/S exam( which is echo free by US)
Occasionally they may cause ;-
- pain and/or haematuria owing to their large size(but they rarely get a large)
- bleeding may occur into the cyst.
Adult polycystic kidney disease AKPD
- APKD a prevalence rate of 1:1000.,.
I 3–10 % of all patients on regular dialysis in the West .
7
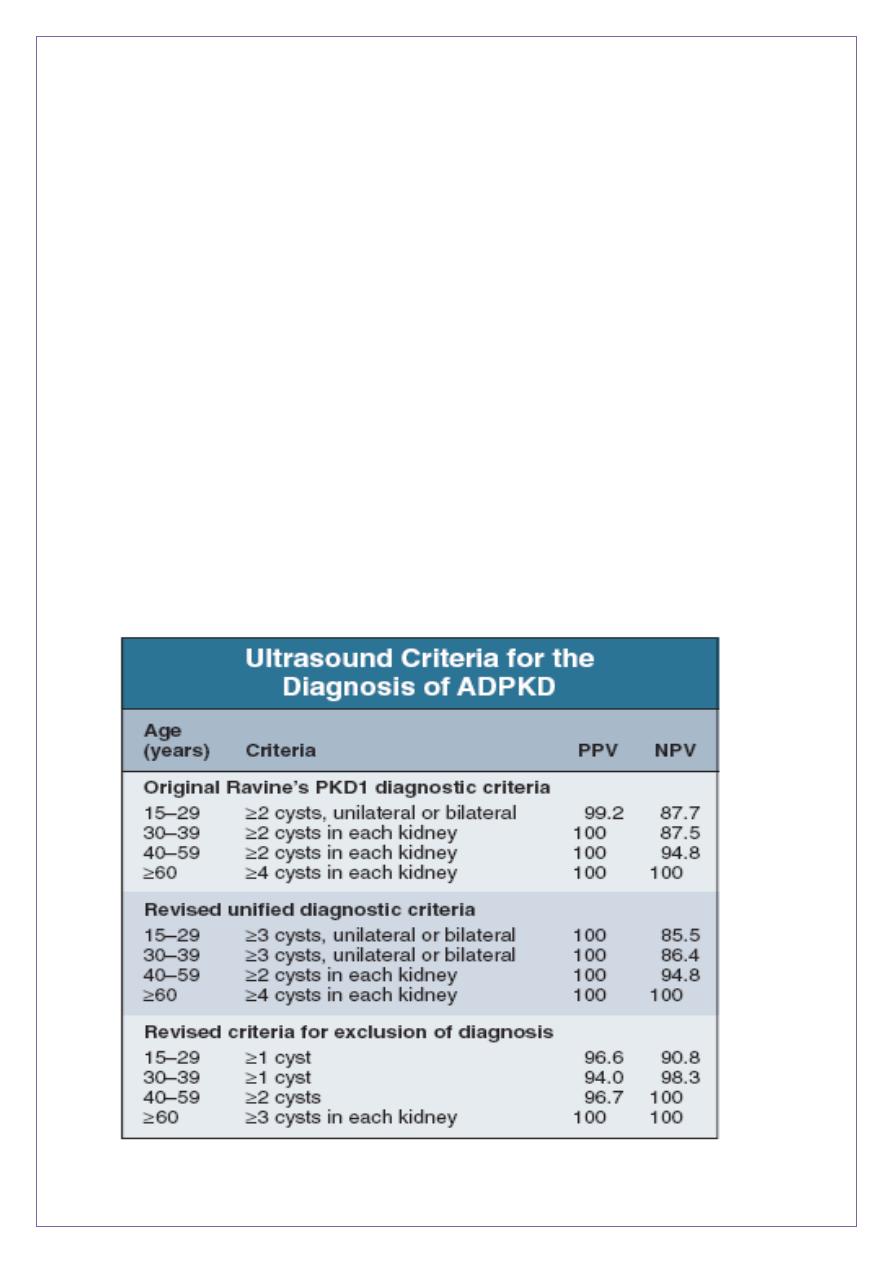
Pathology:-
- Small cysts lined by tubular epithelium
- develop from infancy or childhood
- enlarge slowly and irregularly.
- surrounding normal kidney tissue is progressively
attenuated.
- Renal failure is associated with grossly enlarged kidneys .
Clinical features
- usually asymptomatic until later life. After the age of 20 .
- insidious onset of hypertension. RAS (ACEI of choice)
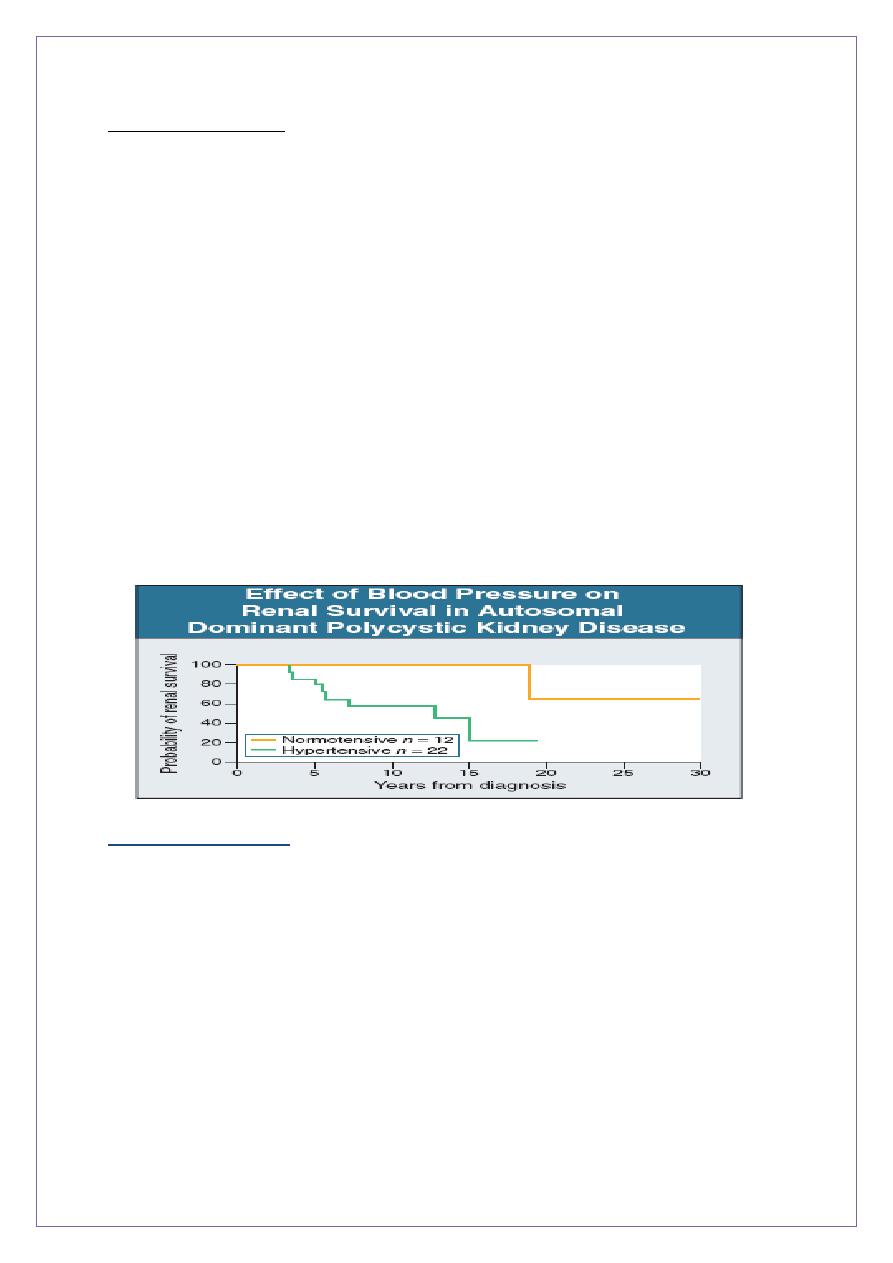
• Early control of BP is essential as cardiovascular
complications are a major cause of death in ADPKD
- Abdominal pain ;-
acute loin pain and/or haematuria owing to haemorrhage into a
cyst, cyst infection or urinary tract stone formation
loin or abdominal discomfort / increasing size of the kidneys(may reach to the level
of the umbilicus called kissing kidneys)
- One or both kidneys may be palpable +/- nodular surface.
- Haematuria (with little or no proteinuria)
- Urinary tract or cyst infections
• Progressive renal failure
• the most serious complication
• GFR below 50 mL/min, decline in averages 5 mL/min/year, which is more rapid than
in other primary renal disorders
• Survival rates on haemodialysis and after renal transplantation in ADPKD are better
than other primary renal diseases

8
• Symptoms of uraemia and /or anaemia associated with CRF(anemia is a late feature)
PKD is not a pre-malignant condition
• Associations:-
-
30 % Hepatic cysts ,
- 20% Mitral and aortic valves regurgitation
- 10% Berry aneurysms of brain +/- SAH
- Colonic diverticulae
- Abdominal wall hernias may occur.
MRI images of kidneys. A Normal kidneys. B Polycystic kidneys; although the
kidney enlargement is extreme, this patient had only slightly
reduced GFR.
9
AKPD Investigations and screening
• Family Hx(the main feature in Dx) , clinical findings & U/S exam.
• U/S cysts in 95% of patients over 20 years ,
( bilateral, multiple cysts, not just two or three).
not detect small developing cysts in youngers
-
sometime possible to make a specific genetic diagnosis,
- Screening for intracranial aneurysms is not generally indicated, where non-invasive MR
angiography is available, some centers screen patients in families with a history of
subarachnoid haemorrhage
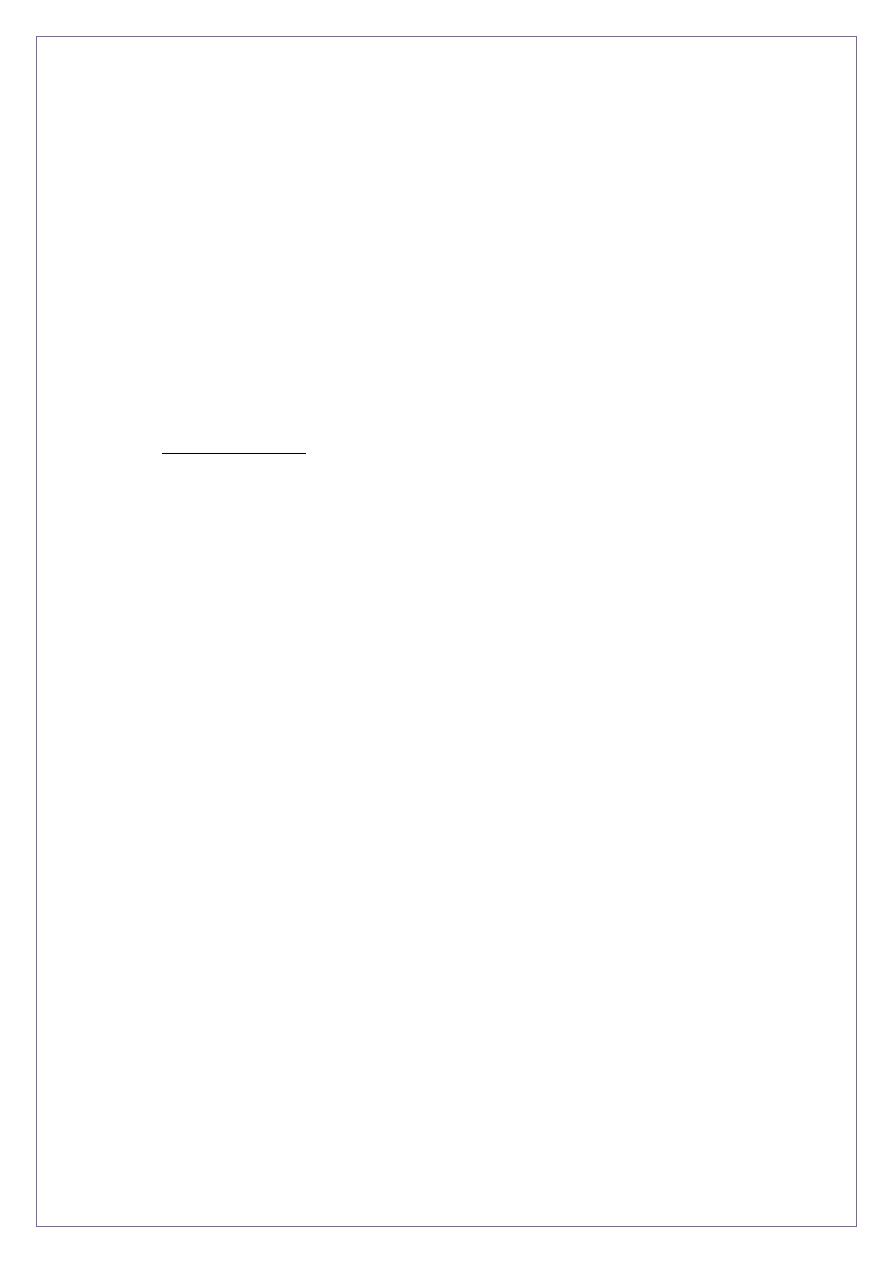
Ultrasound criteria for diagnosis of ADPKD.
NPV,negative predictive value; PPV, positive predictive value
01
-the aim of the table above is to keep in mind that you can not take the transplanted kidney
from any family member who is around 20 years old of age as there is a risk for this kidney
taken from a family member donor to develop cystic changes.and even if he is 30 years
old,we can accept the donation only when there is no other donor as the risk of cystic
changes can occur even after 50s.
Markedly enlarged polycystic kidneys in
comparison
to a normal kidney in the middle
Vascular manifestations of ADPKD. ,
Gross specimen
demonstrating bilateral aneurysms of
the middle cerebral arteries
polycystic liver disease.
A, a very large, cyst.
B several large cysts.
C, multiple smaller cysts
00
AKPD Management
drugs that seem to slow cyst growth
These therapies include;-
- the vasopressin V2 receptor inhibitor, roscovitine
- anti proliferative therapy with sirolimus
- Good control of BP is important
- Good candidates for dialysis and transplantation.
- Nephrectomy
- if it is large , to make space for a renal transplant.
- if it is a source of pain or infection,
**Patients with PKD and HrT at diagnosis have less probability of renal survival than those
with normal blood pressure
Other cystic diseases
• Medullary sponge kidney
- Cysts confined to papillary collecting ducts.
- Cause is unknown ,not inherited
- Patients usually present as adults with renal
stones ,often recurrent, complications
- Prognosis is generally good.
• The diagnosis is made by ultrasound or IVU.
02
• Contrast medium is seen to fill dilated or cystic tubules, which are sometimes
calcified.
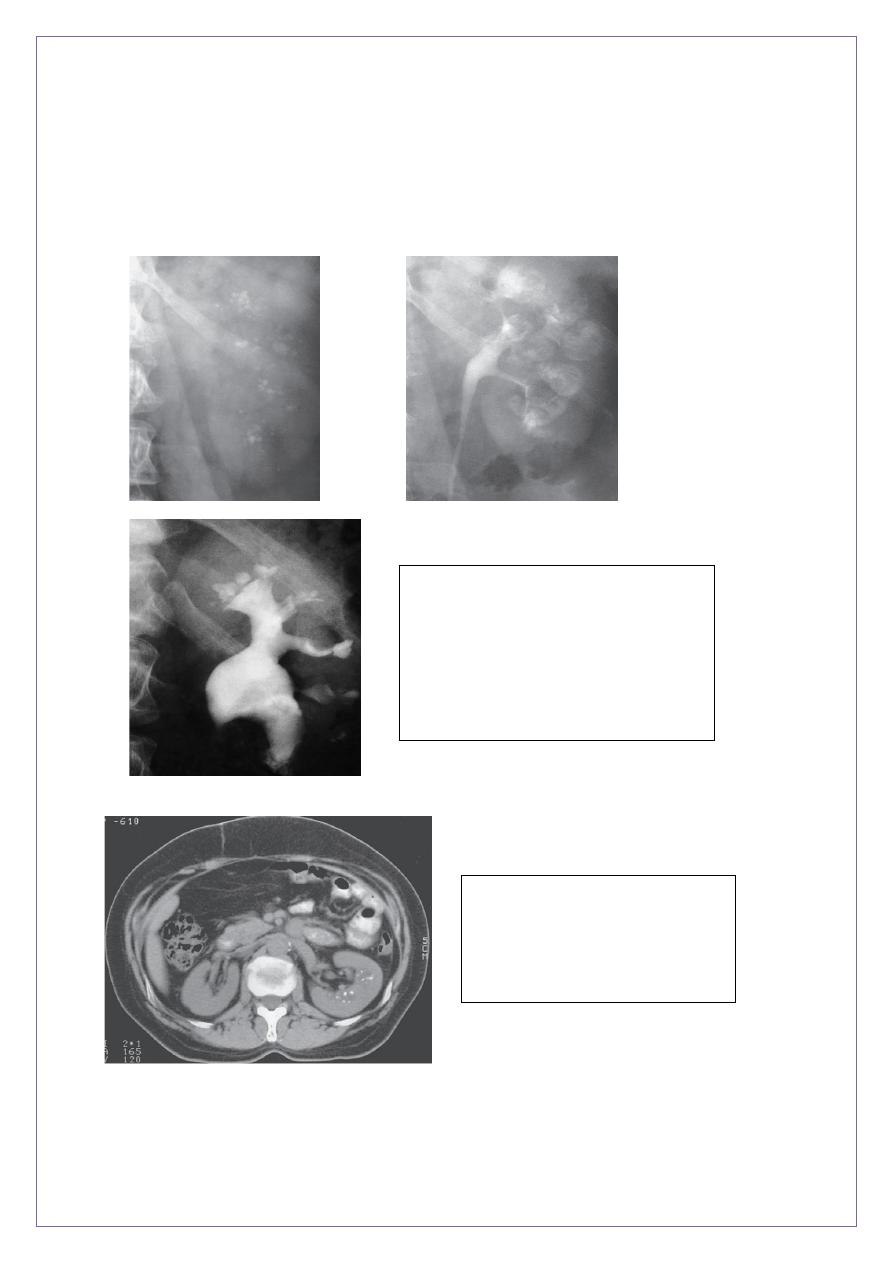
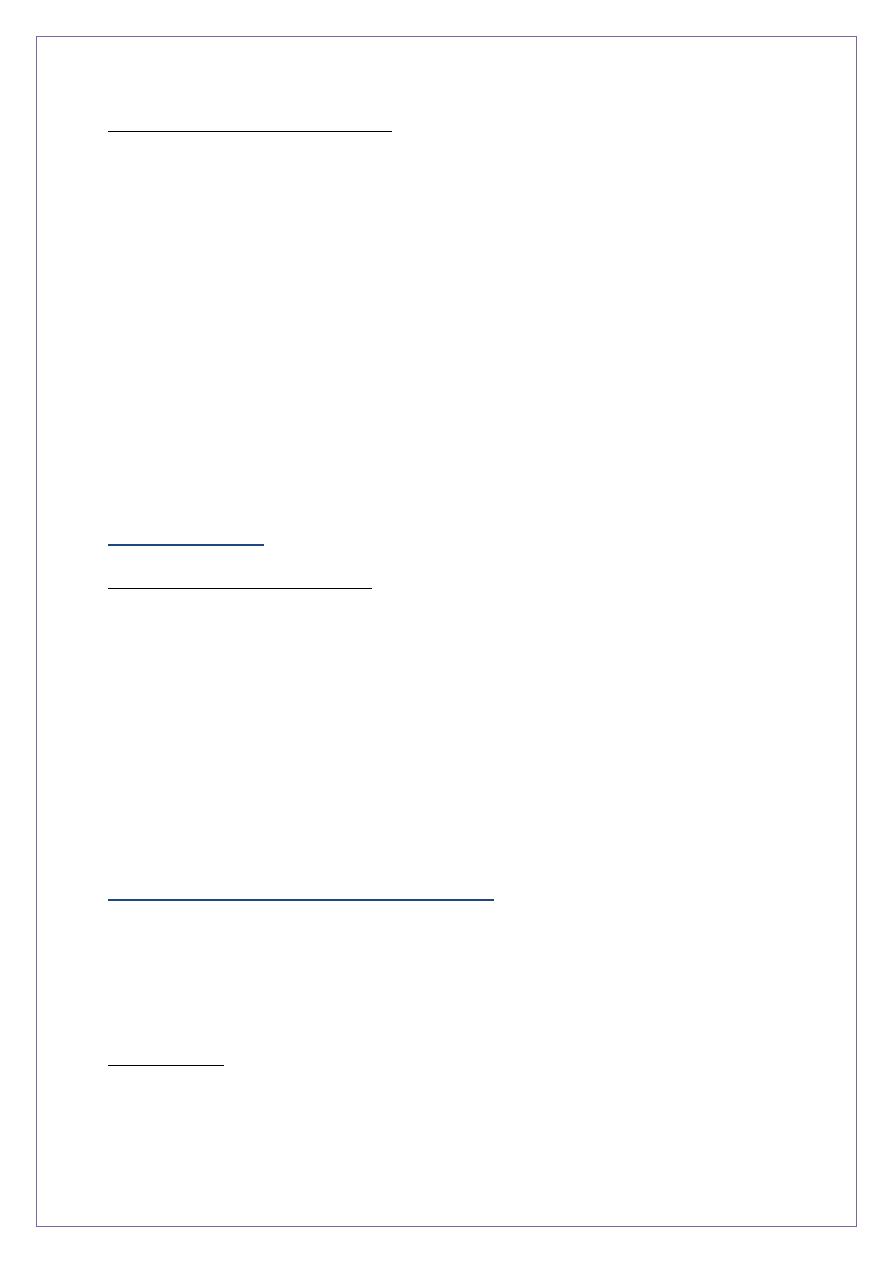
*MSK. A, plain film shows medullary nephrolithiases.
B, IVU 10-min, clusters of rounded densities in the papillae discrete linear opacities
(paintbrush appearance).
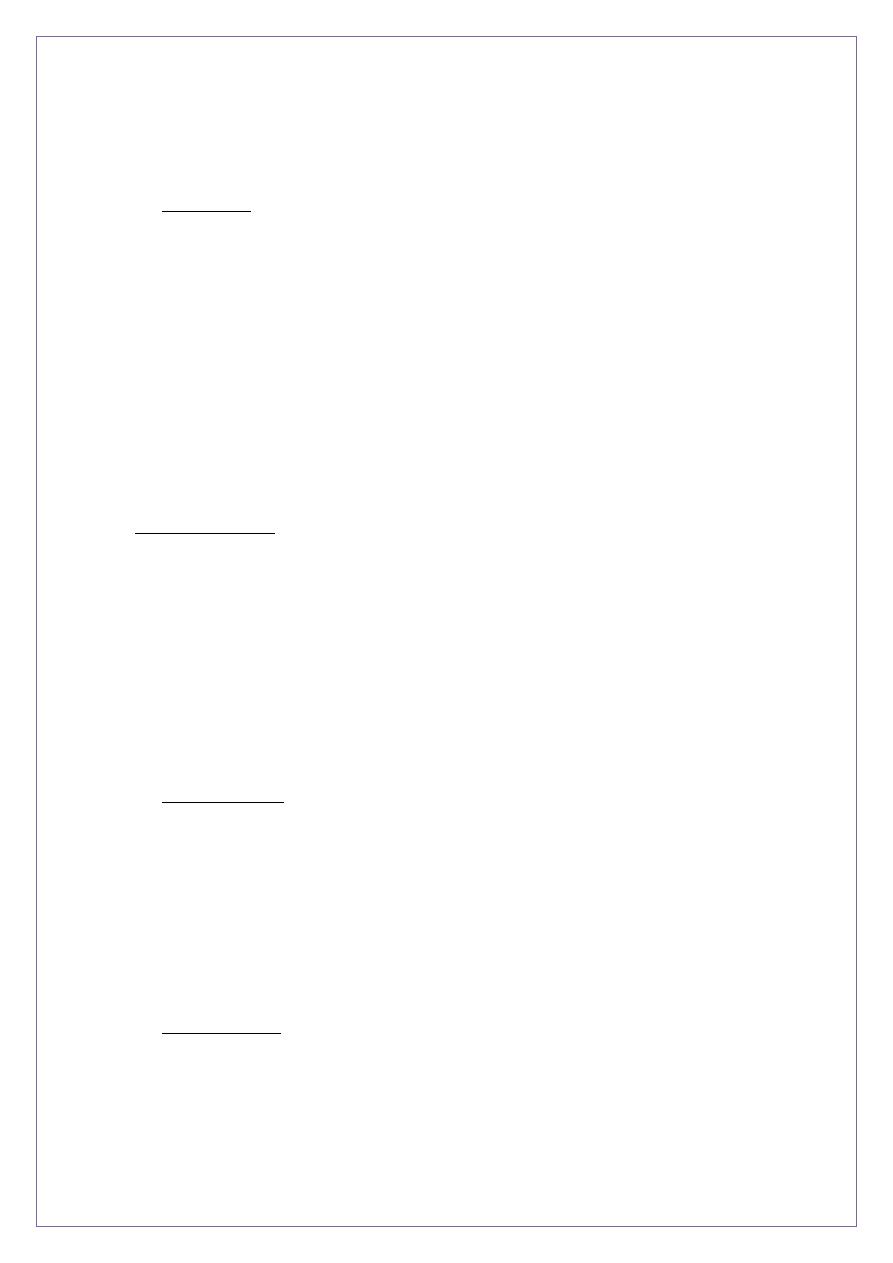
MSK. IVU
contrast medium filling both the collecting
system and cavities arising from collecting
ducts, The cavities have been likened to
bunches of grapes..
MSK Non enhanced CT reveals
densely echogenic
foci in the medulla.
03
Medullary cystic kidney diseases
• are a heterogeneous group of inherited disorders, known as nephronophthisis in
children.
• Small cortical cysts are associated with progressive destruction of the nephron.
• The childhood variants are characterized by thirst and polyuria due to nephrogenic
diabetes insipidus,
• often with a family history of similar disease.
• Sometimes, affected patients are ‘salt-losing’,
• Even when they are treated appropriately, serious renal failure is usual.
• ?? genetic basis
Other cystic diseases
Acquired cystic kidney disease
• Very long history of renal failure, usually including many years of dialysis or
transplanted.
-
Cystic degeneration (formation of multiple cysts which
enlarge with time)
- associated with increased erythropoietin production
- sometimes they develop malignant tumour formation
( renal cell carcinoma) More common than in the general population
Reflux nephropathy (chronic pyelonephritis)
This is a chronic interstitial nephritis associated(VUR) in early life,
- with the appearance of ‘scars’ in the kidney, by imaging .
- The incidence about 12%
Pathogenesis
-Susceptibility with genetic component,
- urine refluxes back from the bladder into the ureter,
04
-
recurrent UTI in childhood,
- Antenatal U/S ;- renal scars in utero in the absence of infection.
• Pathology
-
Reflux diminishes as the child grows and usually disappears.
-
It is often not demonstrable in an adult with a scarred kidney
* unilateral or bilateral
*Gross scarring of the kidneys, commonly at the poles, with reduced size and
narrowing of the cortex and medulla.
*In patients who develop heavy proteinuria and hypertension, renal biopsies show
glomerulomegaly and focal glomerulosclerosis, probably as a secondary response to
reduced nephron number and functional mass.
Clinical features
Usually asymptomatic, at any age with hypertension , proteinuria or
features of CKD.
- +/- recurrent UTI. and aching lumbar pain., may renal calculi
- Urinary white cells and proteinuria (usually < 1 g/24 hrs)
- first present with hypertension and/or proteinuria in pregnancy.
• In some families there is a clear inheritance pattern
• Investigations
• U/S is an insensitive For detecting renal scars, BUT it will detect major dysplasia ,
dysgenesis, and exclude significant obstruction.
• Radionuclide DMSA scans are more sensitive
• imaging by MRI or CT maybe useful.
micturating cysto-urethrography (MCUG)used less often.
• Management
- Infection, treated & prevented with prophylactic ABCS.
reduce recurrences of UTI but there is no evidence that they
05
protect against further renal scarring or dysfunction.’
• nephrectomy - pyelonephrosis
- unilateral renal infection or pain persists,.
- hypertension is cured by when the disease
is predominantly or entirely unilateral.
• As most childhood reflux tends to disappea spontaneously
and trials have shown small or no benefits from anti-reflux surgery, such
intervention is now less common
• Prognosis
- Children and adults with small or unilateral renal scars have a good prognosis,
provided renal growth is normal.
- With significant unilateral scars / usually compensatory hypertrophy of the
contralateral kidney.
-
In patients with more severe bilateral disease, prognosis is predicted by the severity
of renal dysfunction , hypertension and proteinuria.
-
If the serum creatinine is normal and hypertension and proteinuria are absent, then
the long-term prognosis is usually good.
The End
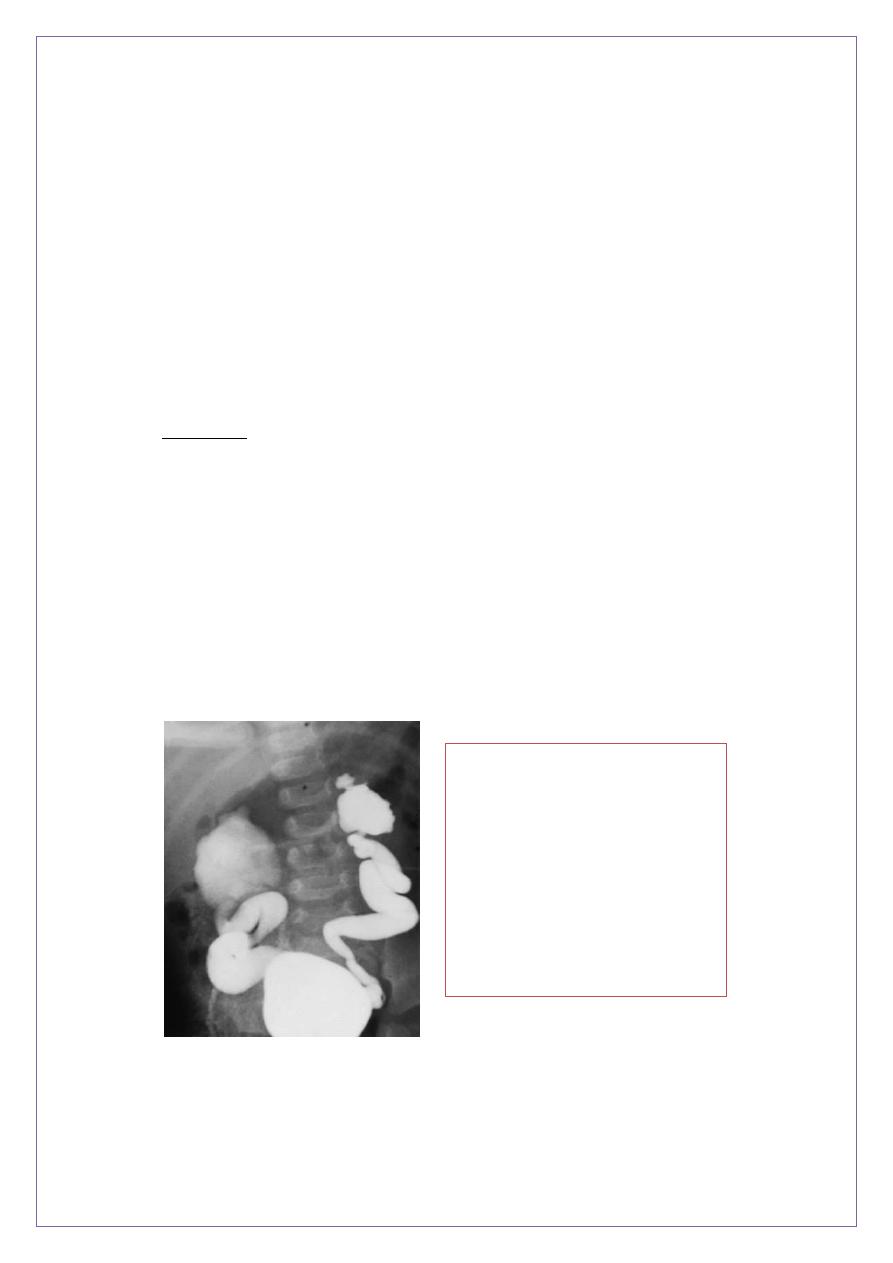
VUR (grade IV) shown by
micturating cystogram. The
bladder has been filled with
contrast medium through a urinary
catheter. After micturition there
was gross VUR into widely
distended ureters and pelvicalyceal
systems.

06
Appendix:
Case1
A 15-year-old boy comes to the physician because of
hematuria
and
lower abdominal pain.
This is his third episode of hematuria in the past
2 years. He has a
family history of renal disease
. His temperature is
37.1 C (98 .9F), blood pressure is
140/90 mm Hg
, pulse is 80/min, and
respirations are 14/min. Examination shows mild
sensorineural
deafness
bilaterally. Urinalysis shows
hematuria
and
proteinuria
.
Laboratory studies show BUN of 50 mg/dl and serum creatinine of 3.1
mg/dl; serum complement levels are normal. Renal biopsy shows foam
cells, and immunofluorescence shows no immunoglobulins or
complement. Electron microscopy shows alternating areas
of thinned
and thickened capillary loops with splitting of GBM
. Which of the
following is the most likely diagnosis?
A. Alport syndrome
B.Thin basement membrane disease
C.systemic lupus erythematous
D.wegner`s granulomatosis
E.acute post infectious glomerulonephritis
The above vignette illustrated the classic presentation of Alport's
syndrome. This is a familial disorder which usually presents in childhood
as recurrent gross hematuria and proteinuria. Sensorineural deafness
usually occurs. Electron microscopy findings include alternating areas of
thinned and thickened capillary loops with splitting of the glomerular
basement membrane (GBM).
(Choice B) Thin basement membrane disease is also a familial disorder,
but it presents in adulthood as microscopic hematuria without
proteinuria. Renal biopsy reveals a markedly thinned basement
membrane.

07
So suspect Alport's syndrome in patients with recurrent episodes of
hematuria, sensorineural deafness and a family history of renal failure.
So the answer is A
Case2
A 51-year-old man is admitted to the hospital because of
renal failure
.
His past medical history is significant for recurrent episodes of
bilateral
flank pain
over the past several years as well as
nocturia
2 to 3 times
per night for the past 1 0 years. He has no weight loss. On physical
examination. his blood pressure is
164/100 mm Hg
. The liver is
enlarged and a
mass is felt at the right flank
on deep palpation. Which
of the following is the most likely diagnosis?
A. Horse shoe kidney
B. Nephrolithiasis
C. Papillary necrosis
D. Polycystic kidney disease
E. Renal cell carcinoma
This man most likely has autosomal dominant polycystic kidney disease
(ADPKD). ADPKD is one of the most common hereditary diseases in the
United States and accounts for 1 0% of dialysis patients. Patients will
often have hypertension and palpable kidneys on exam. Please note:
the enlarged right kidney is easier to palpate because it lies lower than
the left kidney! The liver might be enlarged due to cystic involvement.
So Autosomal dominant polycystic kidney disease is a heritable form of
renal disease characterized by multiple renal cysts and intermittent flank
pain. hematuria. urinary tract infections. and nephrolithiasis.
So the answer is D

08
Case3
A 34-year-old woman comes to the physician's office because of
occasional
headaches
and
palpitations
. She has no other medical
problems. She takes no medications. She smokes one and a half packs
of cigarettes daily. Her blood pressure is
170/100 mm Hg
in both arms.
and heart rate is 80/min. Physical examination shows
bilateral flank
masses
. Laboratory studies show:
Serum sodium 140 mEq/L Serum potassium 4.4 mEq/L BUN 26 mg/dl
Serum creatinine 1 .3 mg/dl
Urinalysis shows 10-12 red blood cells/hpf. but otherwise shows no
abnormalities. The most likely complication that can occur in this patient
is which of the following?
A. Liver necrosis
B. Intracranial bleeding
C. Restrictive cardiomyopathy
D. Pancreatic cancer
E. Aortic dissection
Explanation:
This patient most likely has autosomal dominant polycystic kidney
disease (ADPKD). The clues to the correct diagnosis are hypertension.
palpable bilateral abdominal masses and microhematuria. Intracranial
berry aneurysm is a common complication. and is seen in 5 to 1 0% of
the cases. Although such aneurysms are common and dangerous when
coupled with hypertension. routine screening for intracranial aneurysms
is not recommended.
The other major extra-renal complications of ADPKD are:
1 . Hepatic cysts - most common extrarenal manifestations of ADPKD 2.
Valvular heart disease - most often mitral valve prolapse and aortic
regurgitation 3. Colonic diverticula 4. Abdominal wall and inguinal hernia
So the answer is B
