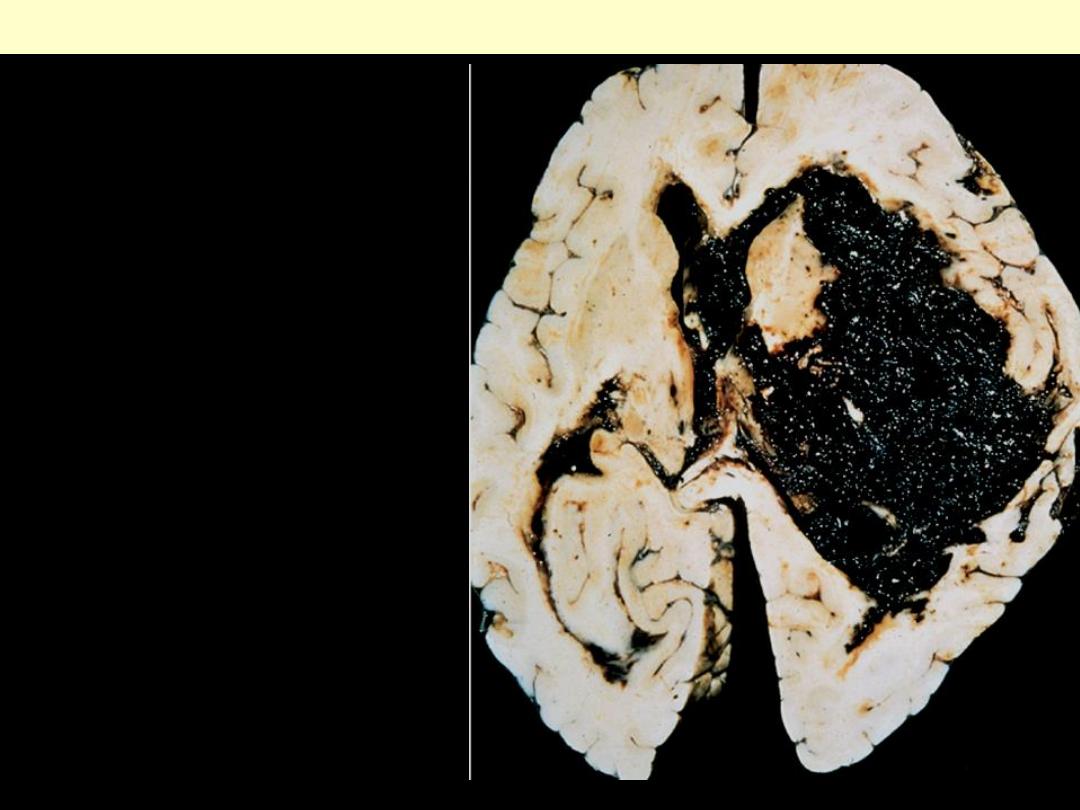
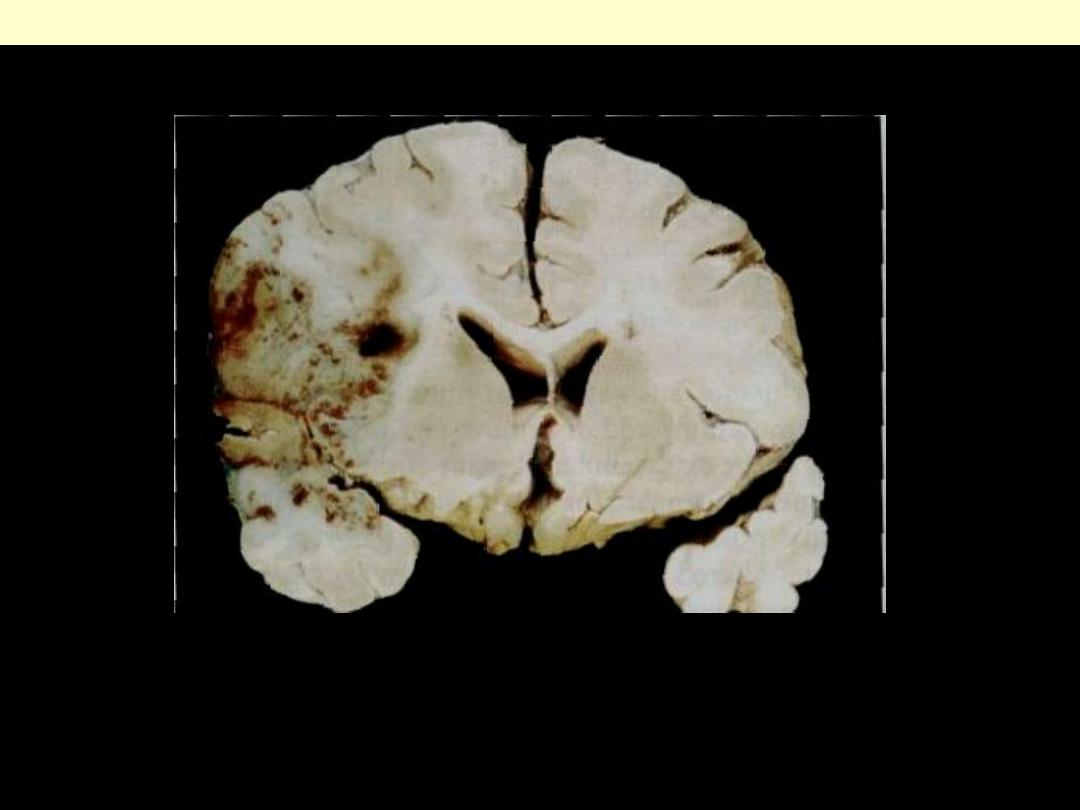
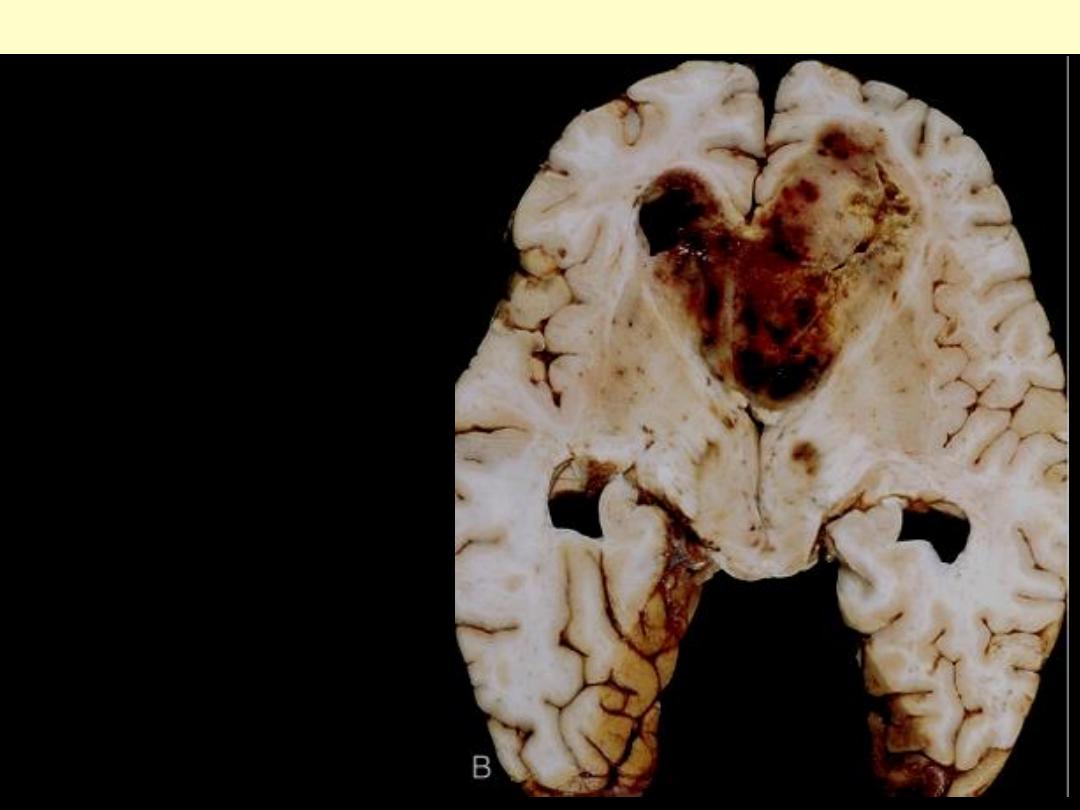
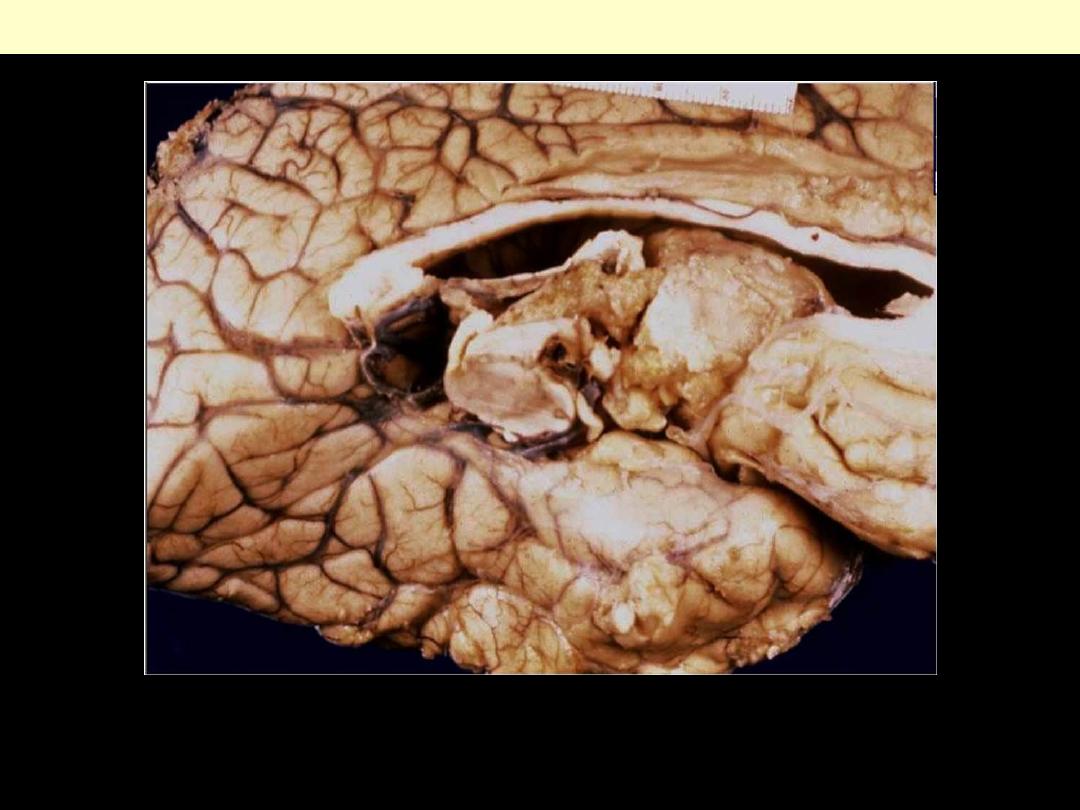
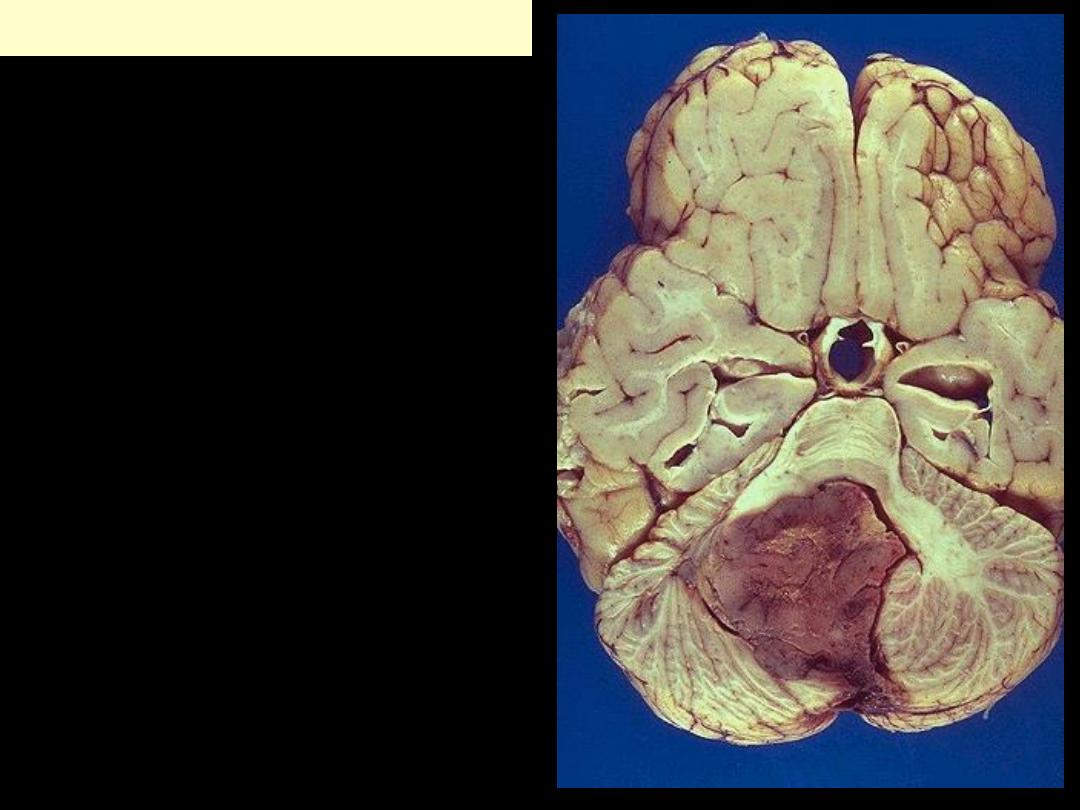
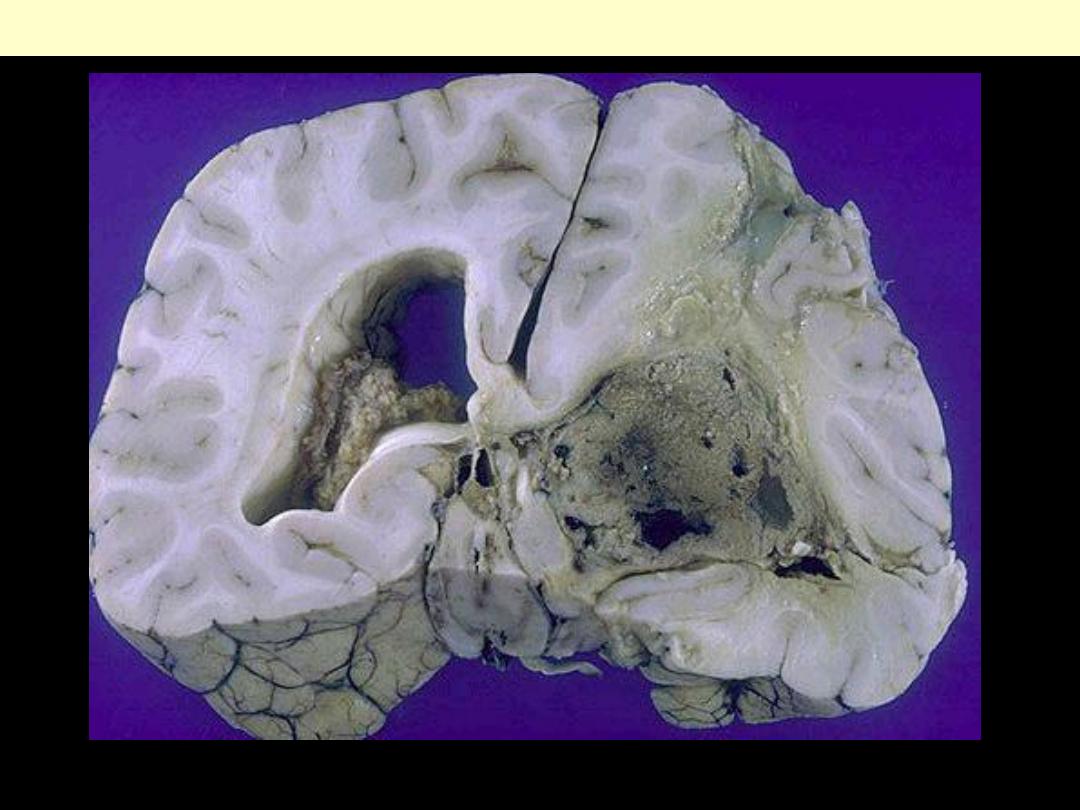
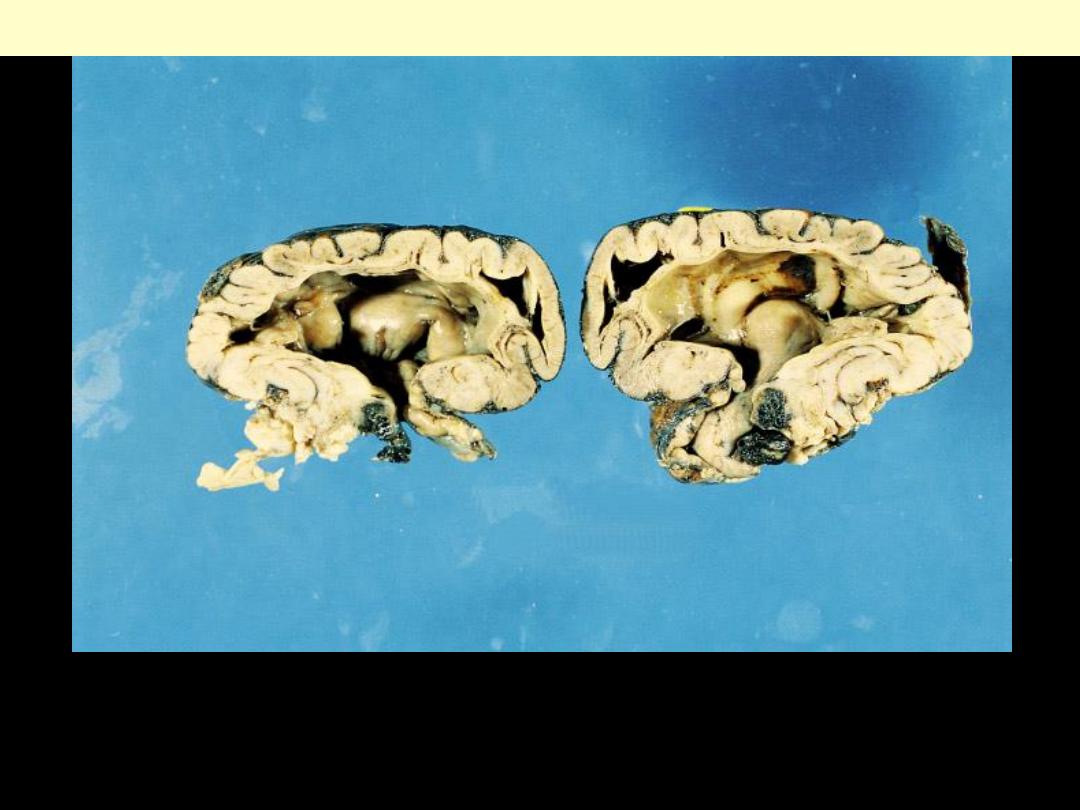
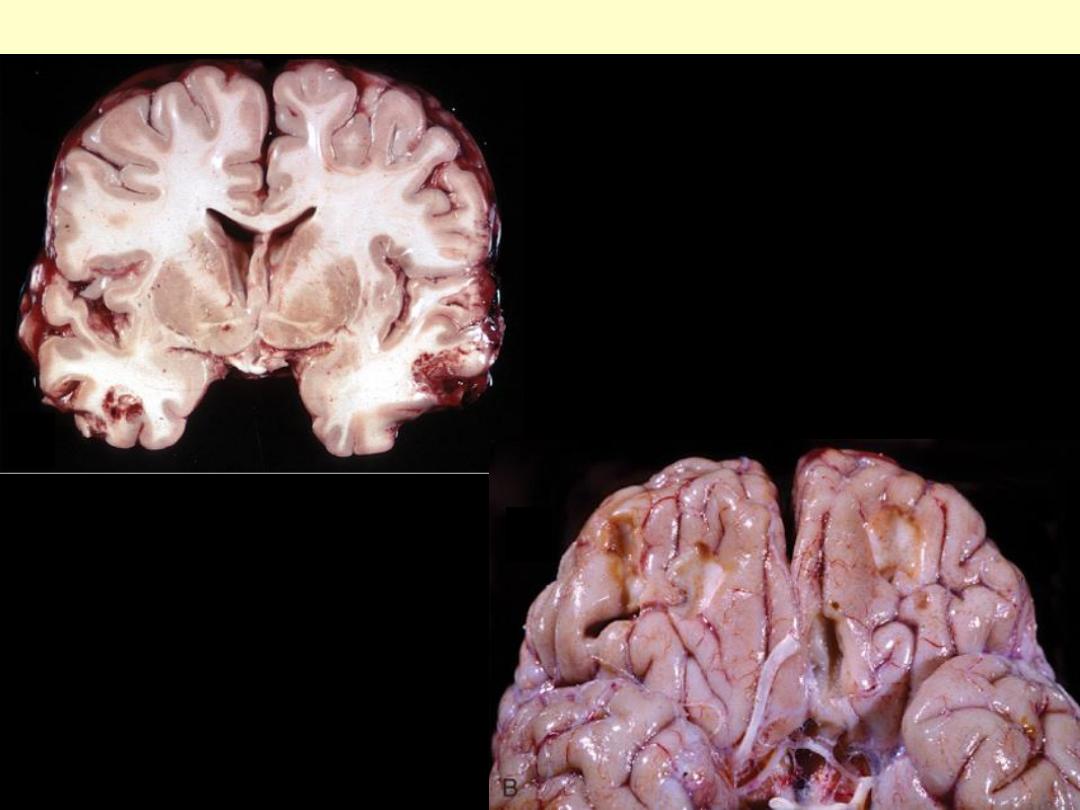
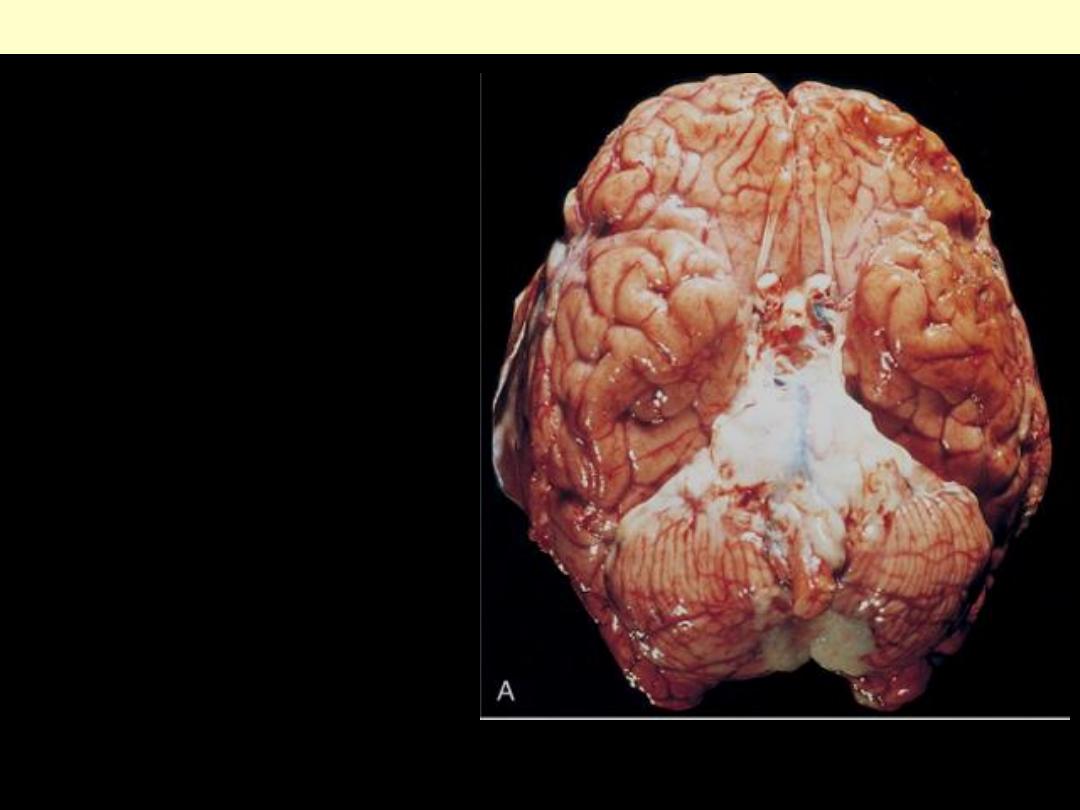
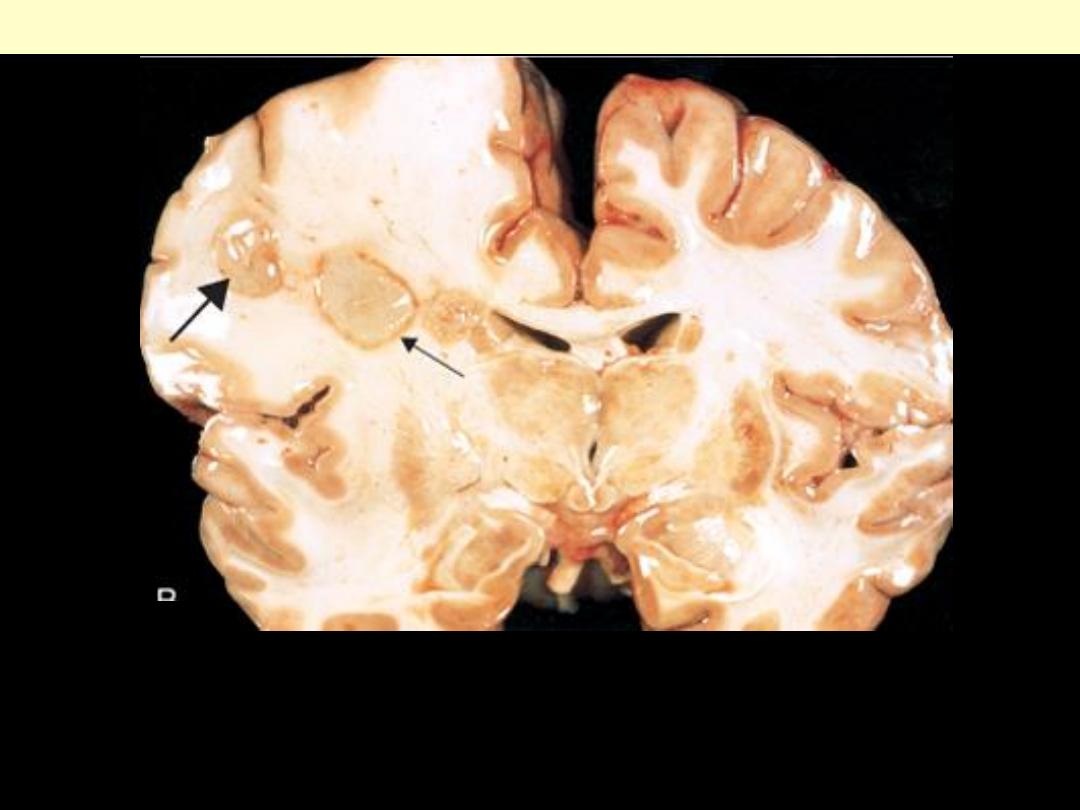
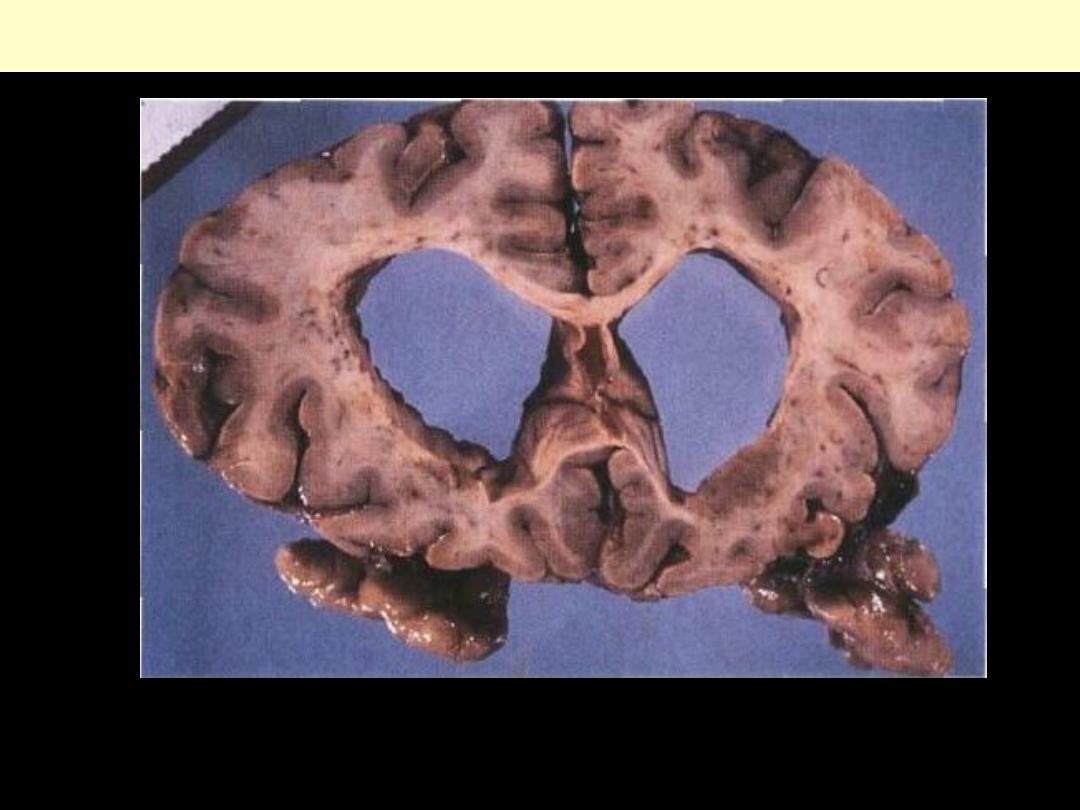
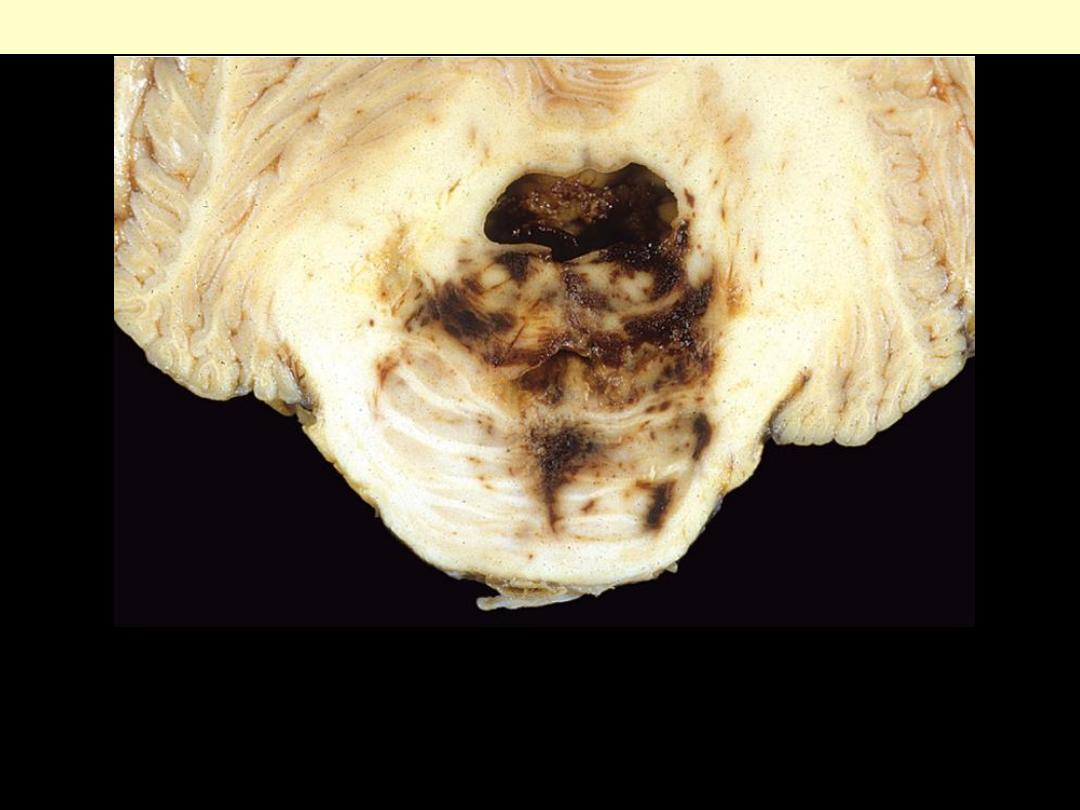
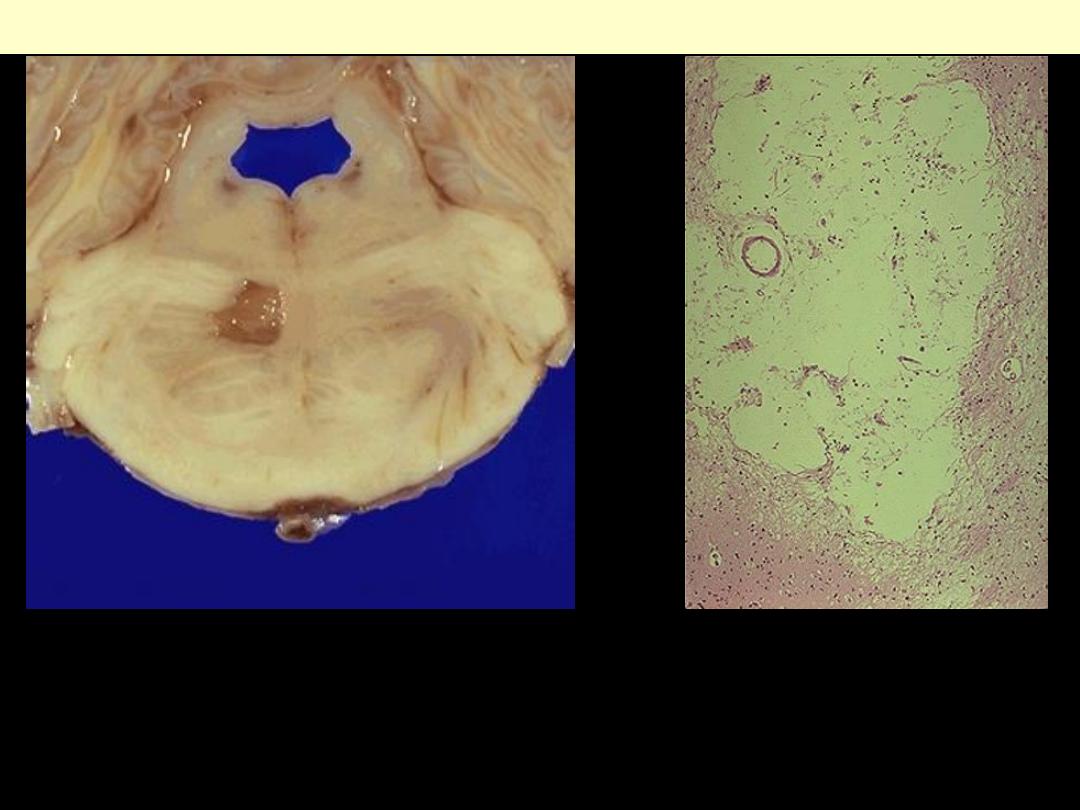
Massive hypertensive
hemorrhage rupturing into
a lateral ventricle.
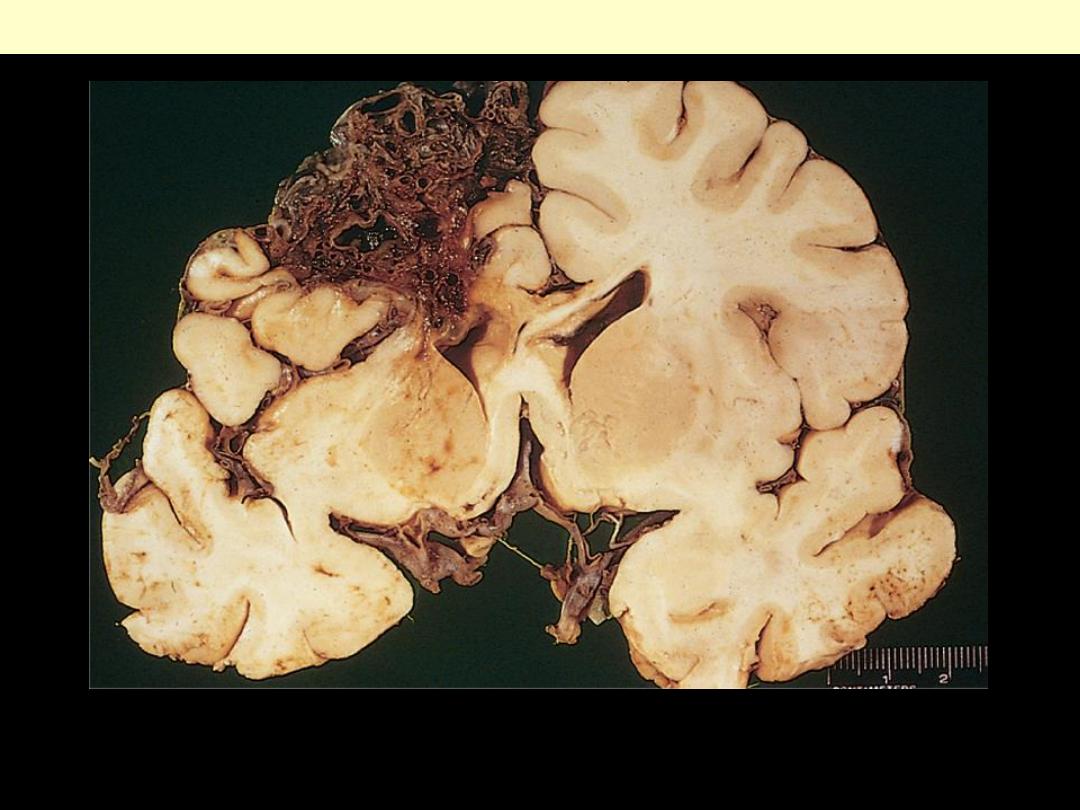
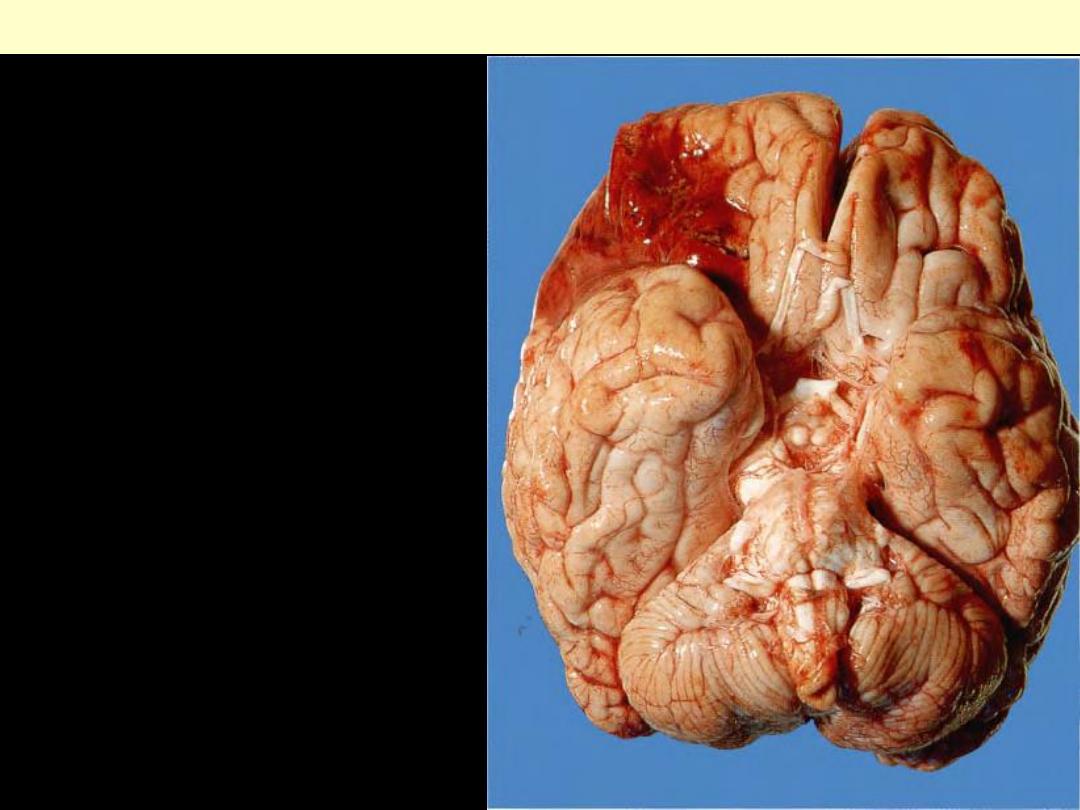
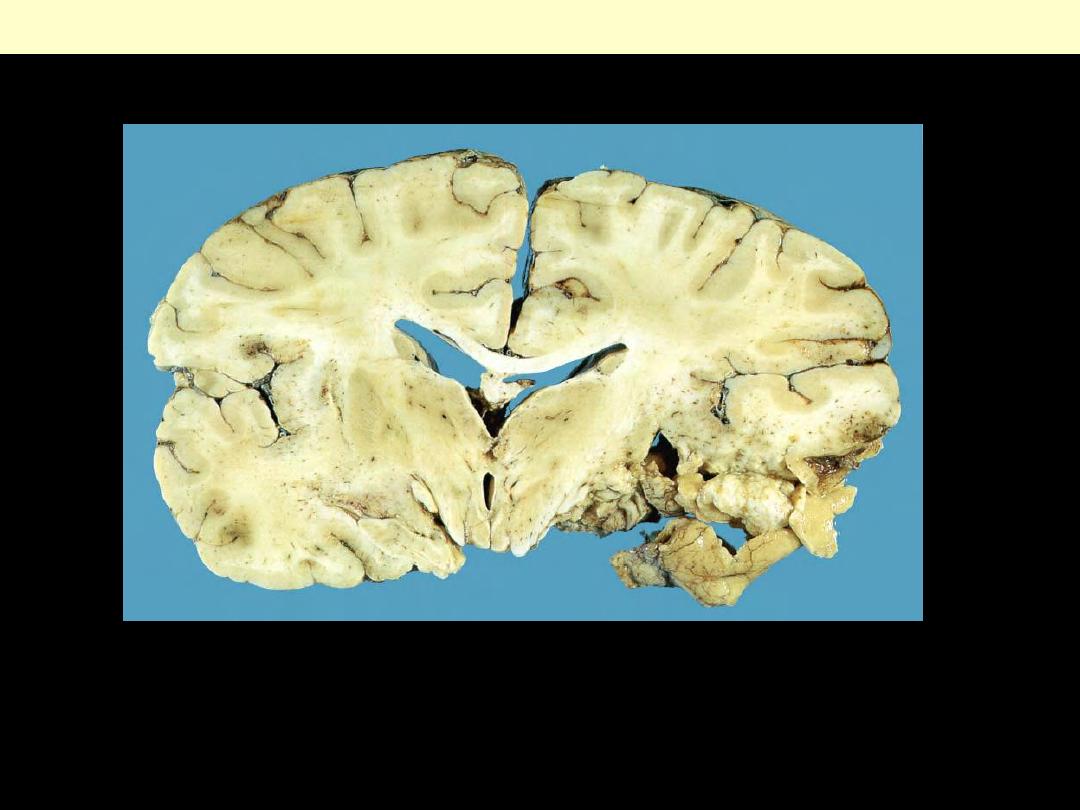
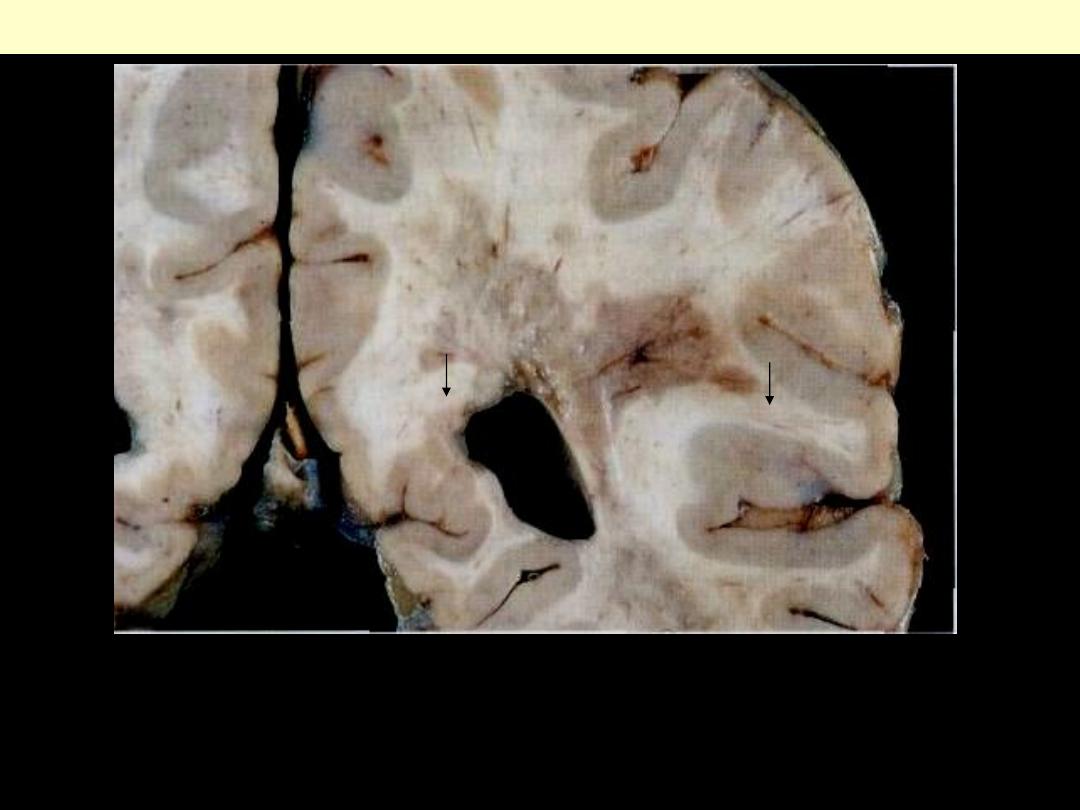
Cerebral hemorrhage
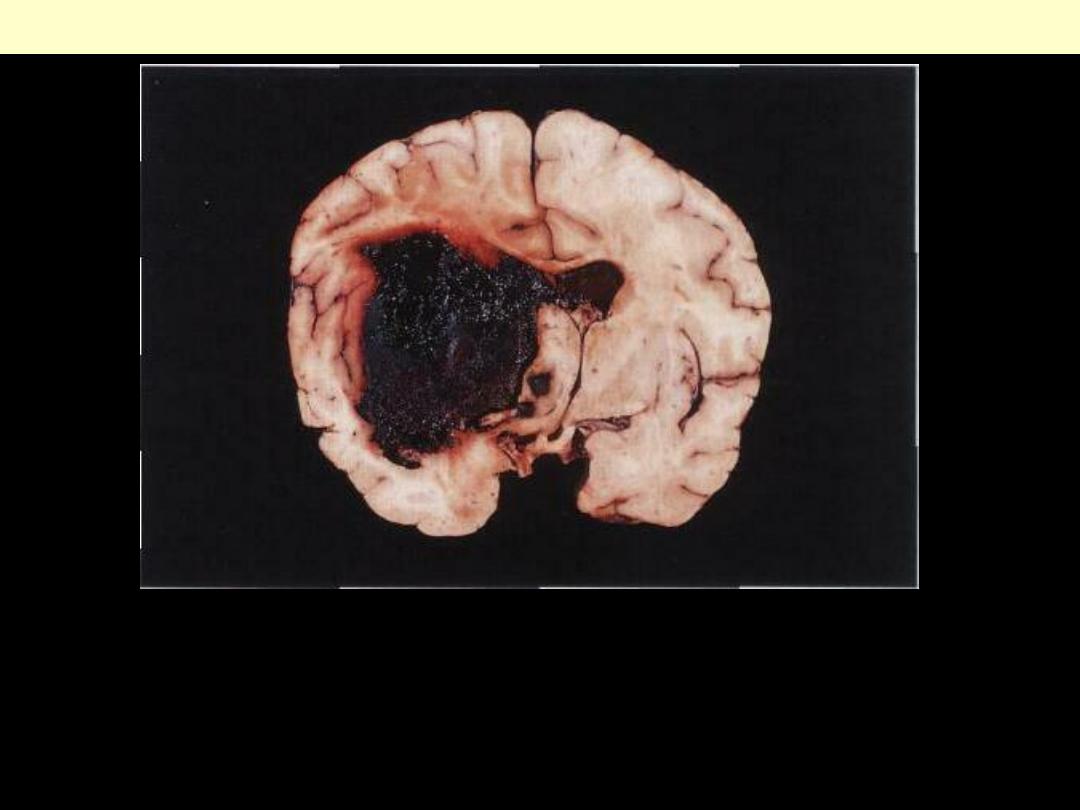
Acute intracerebral hemorrhage
A fresh hematoma has disrupted and expanded the left cerebral
hemisphere, causing the midline structures to shift to the right.
Uncontrolled hypertension is an important cause of this catastrophic
lesion.
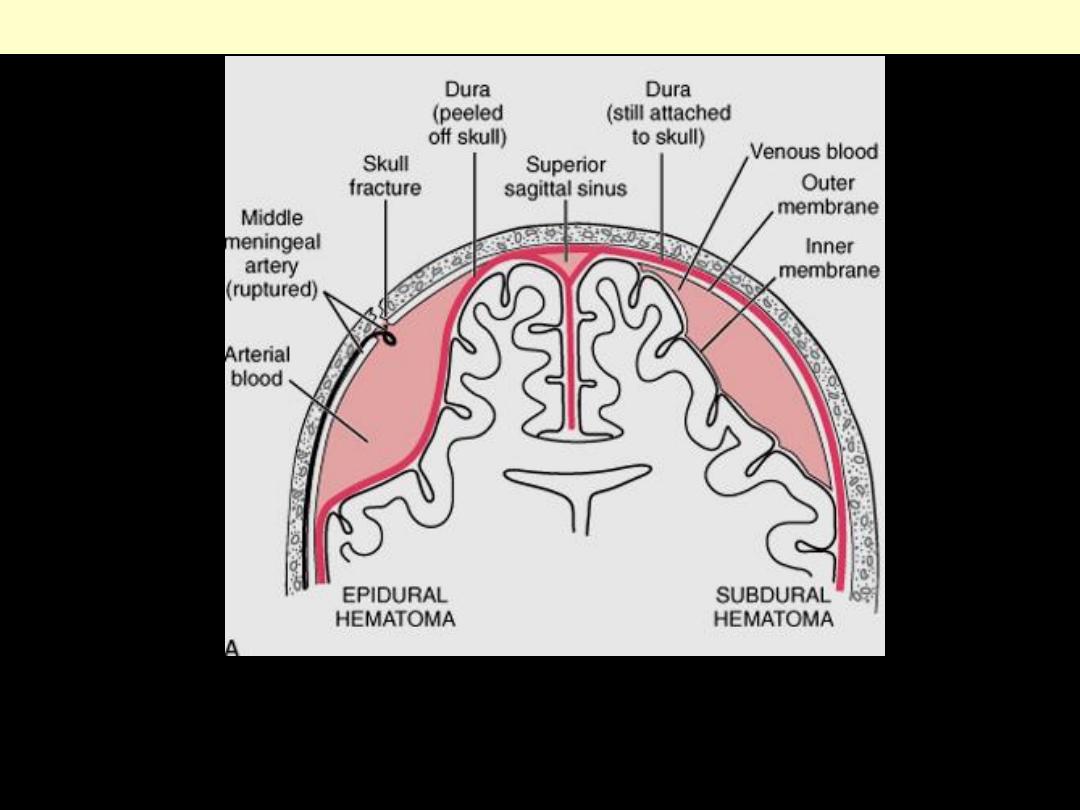
A, Epidural hematoma (left) in which rupture of a meningeal artery, usually associated with a skull
fracture, leads to accumulation of arterial blood between the dura and the skull. In a subdural
hematoma (right), damage to bridging veins between the brain and the superior sagittal sinus leads to
the accumulation of blood between the dura and the arachnoid.
Traumatic intracranial hemorrhages
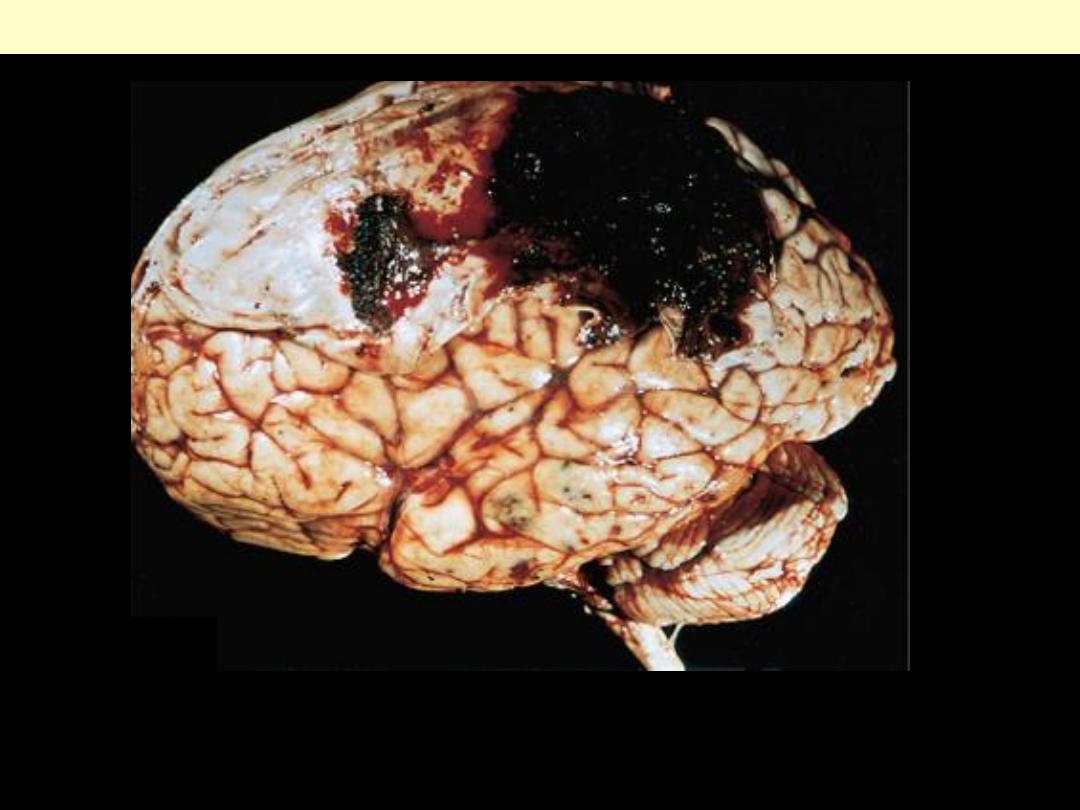
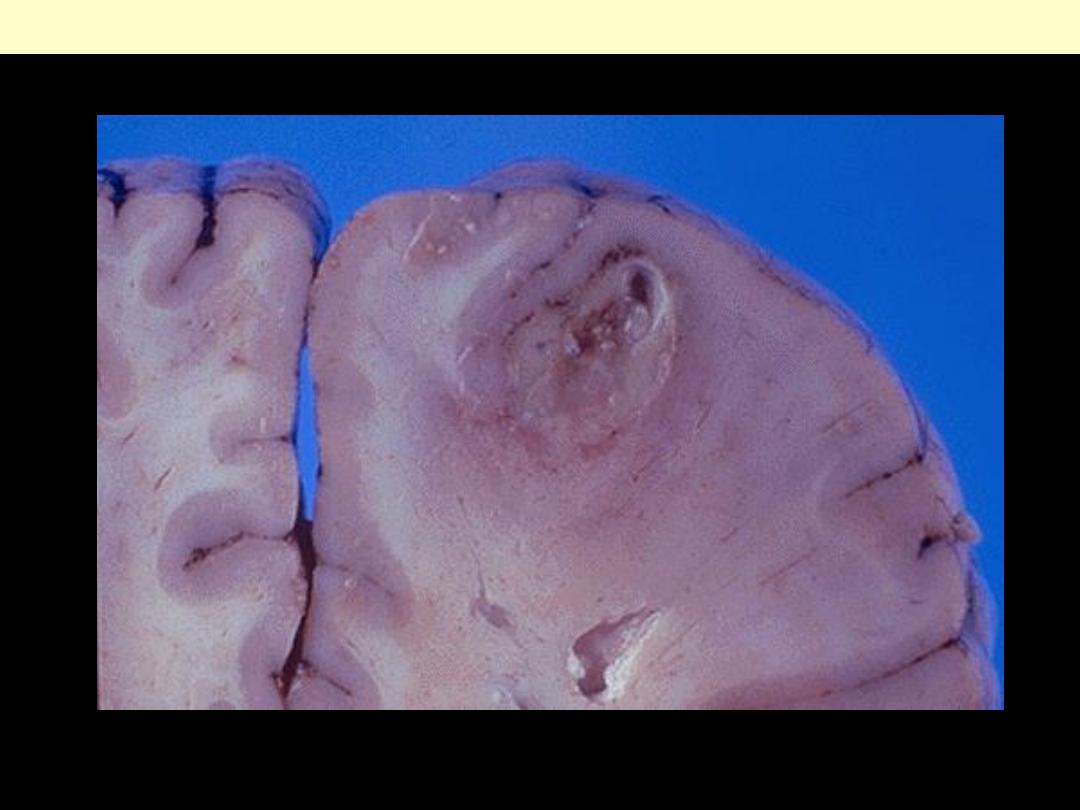
Epidural hematoma covering a portion of the dura.
Epidural hematoma
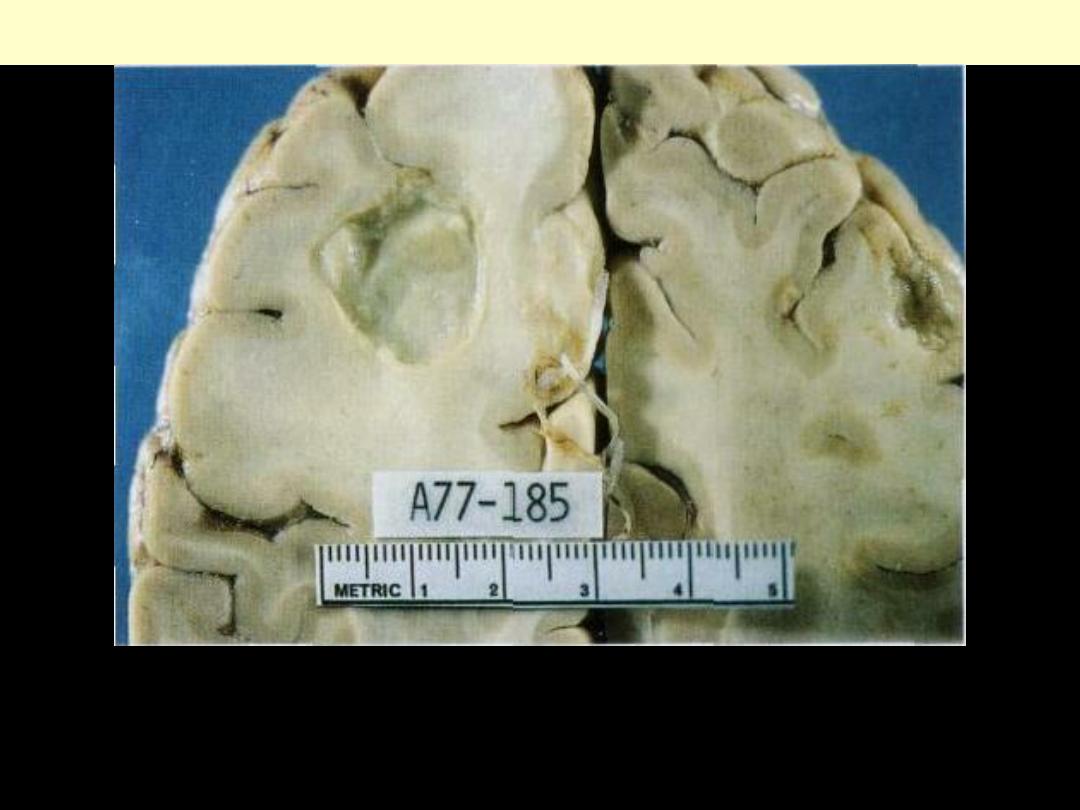
Large organizing subdural hematoma
attached to the dura.
Subdural hematoma
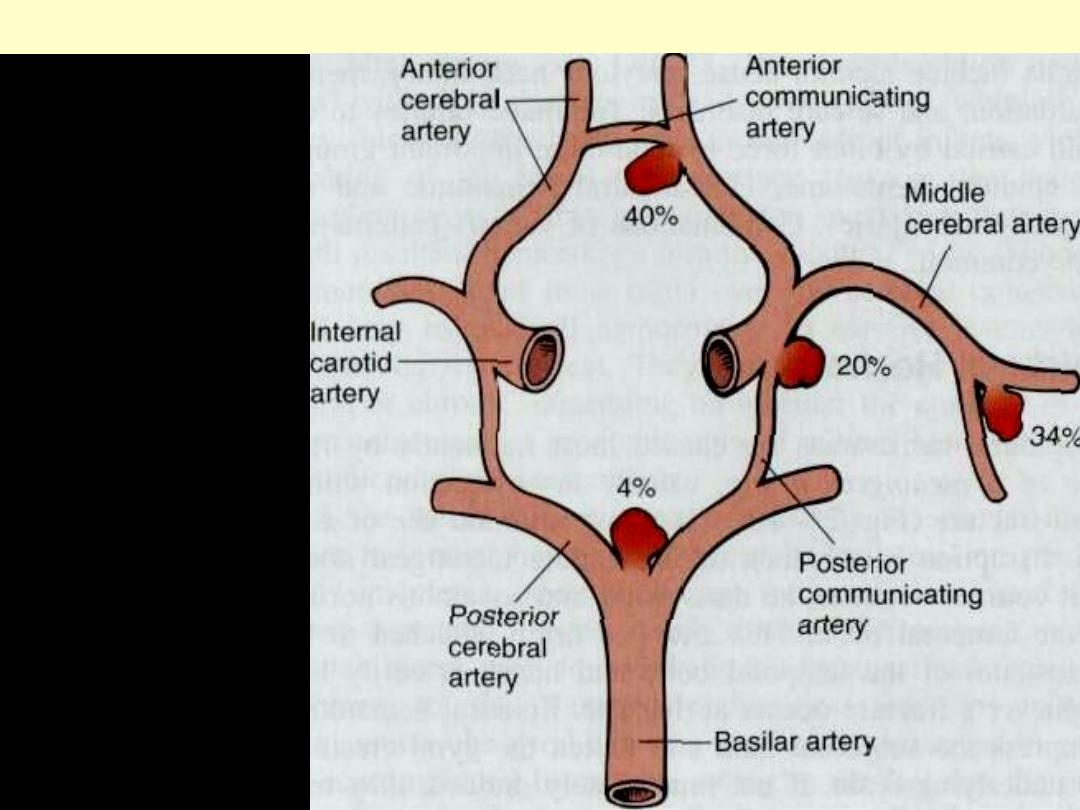
Frequency distribution of Berry aneurysms
Sites of saccular
aneurysms and their
relative frequencies.
Multiple aneurysms may
be present in an individual
patient.
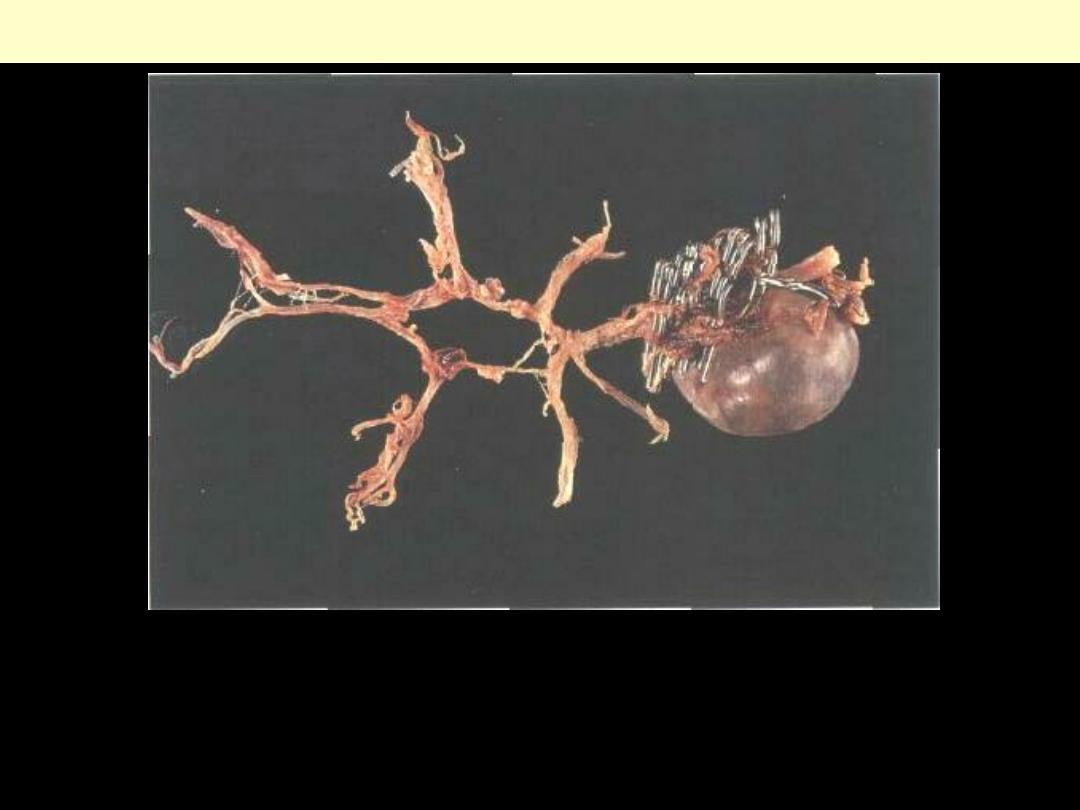
Intracranial giant saccular aneurysm
Gross view of a massive saccular aneurysm arising at the junction of the
vertebral and basilar arteries. The vessels have been dissected from the
brain. Multiple surgical clips, visible in the photograph, were placed on the
aneurysm before death in an attempt to prevent further bleeding.
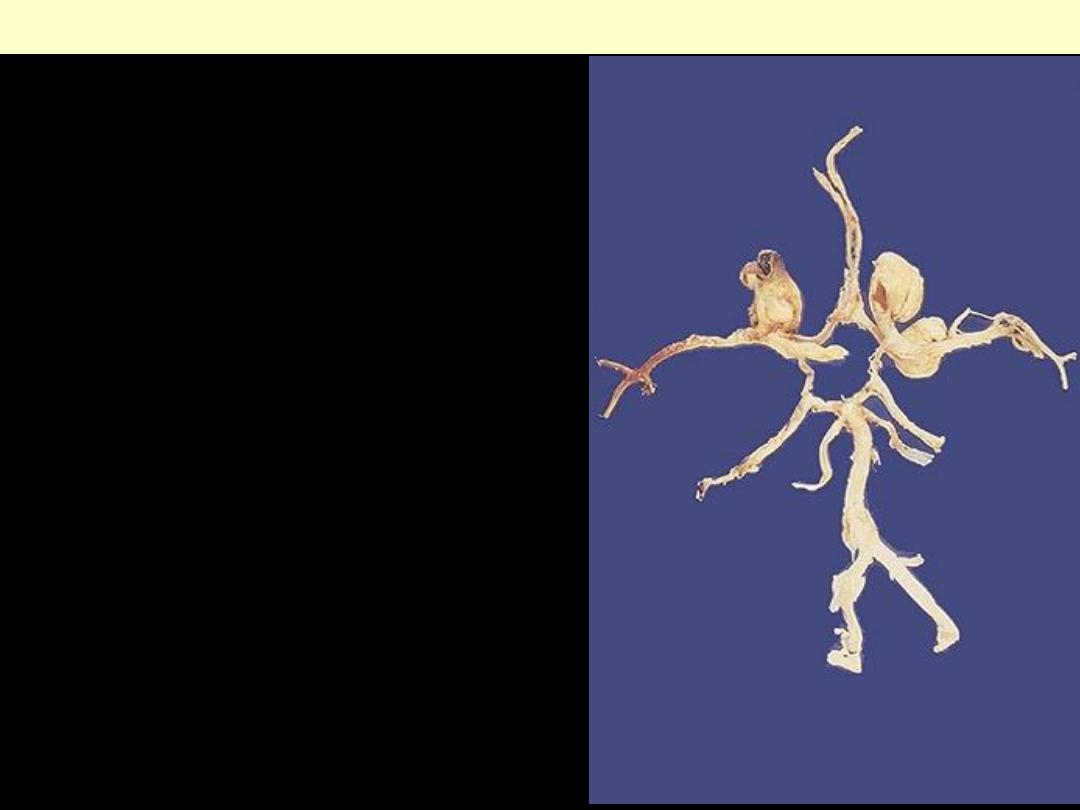
The circle of Willis has been
dissected, and three berry
aneurysms are seen. Such
aneurysms are "congenital" in the
sense that the defect in the arterial
wall is present from birth, but the
actual aneurysm takes years to
develop, so that rupture is most
likely to occur in young to middle
age adults.
Berry aneurysms circle of Willis
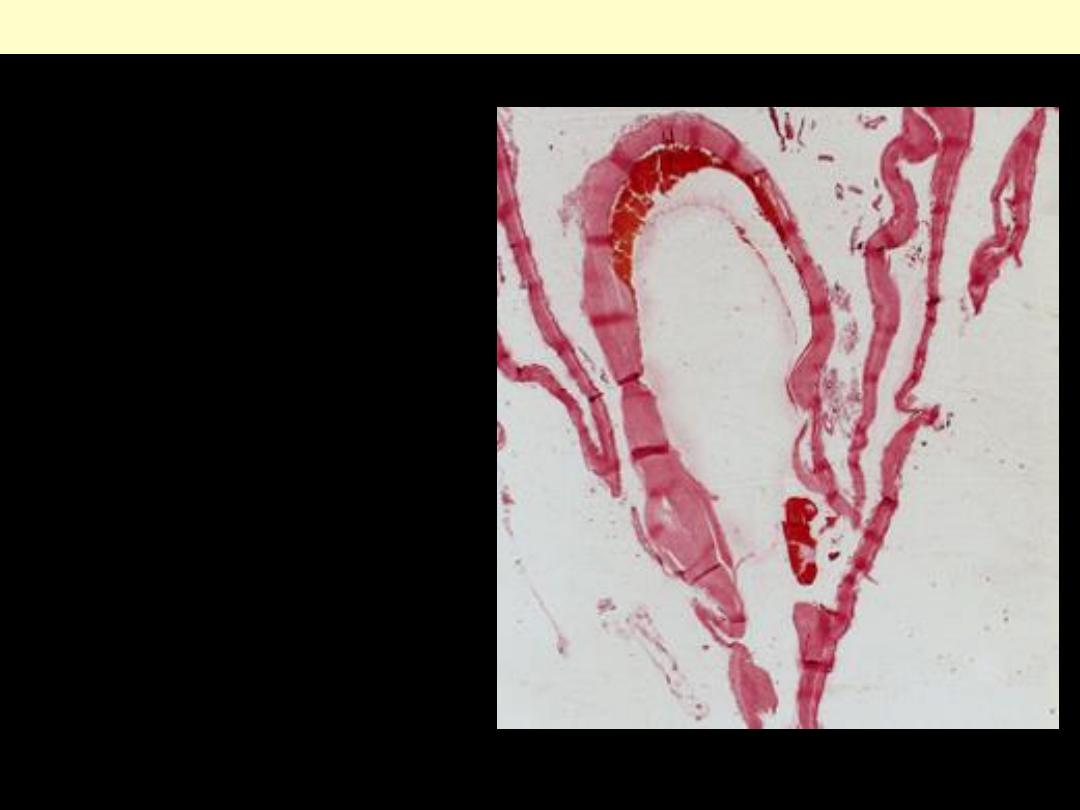
Section through a saccular
aneurysm showing the hyalinized
fibrous vessel wall (H&E).
Saccular aneurysms
This is the most common site i.e. the territory of the middle cerebral artery. They resemble a tangled
network of vascular channels
Arteriovenous malformation (AVM)
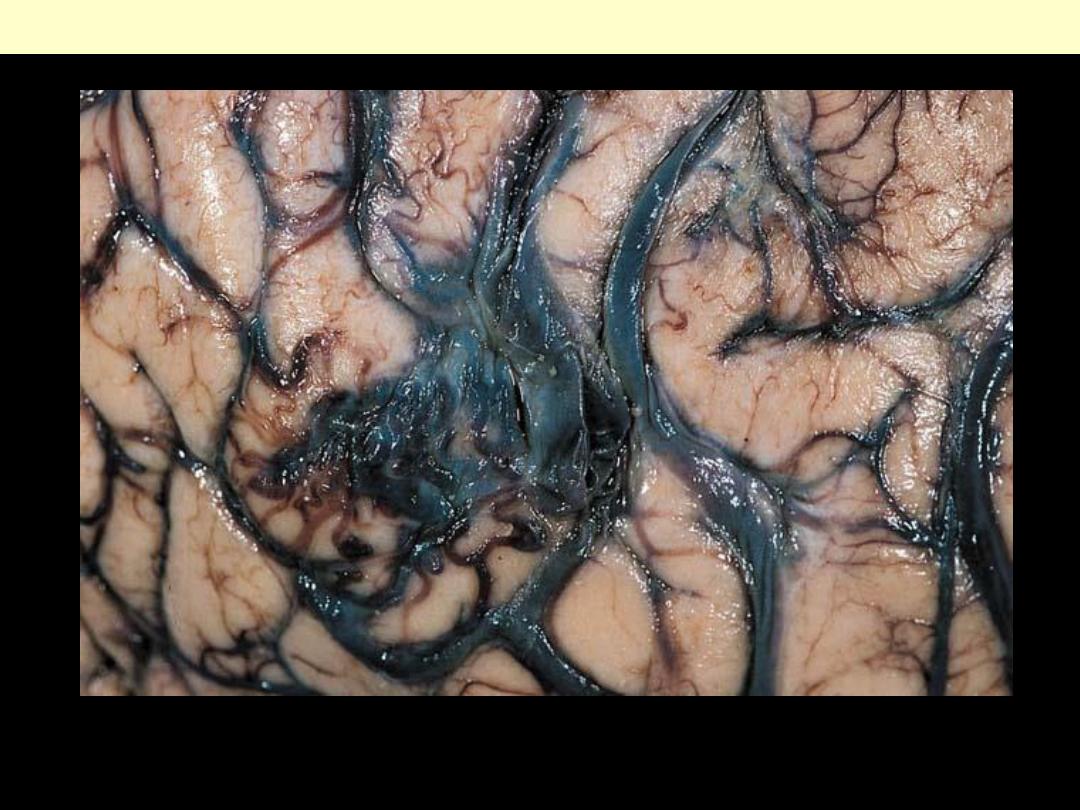
Arteriovenous malformation. This variety of vascular anomaly often involves the leptomeninges (as
well as underlying brain) and may be apparent on inspection of the cortical surface as a tangle of
vascular channels and ectatic, draining veins.
Arteriovenous malformation (AVM)
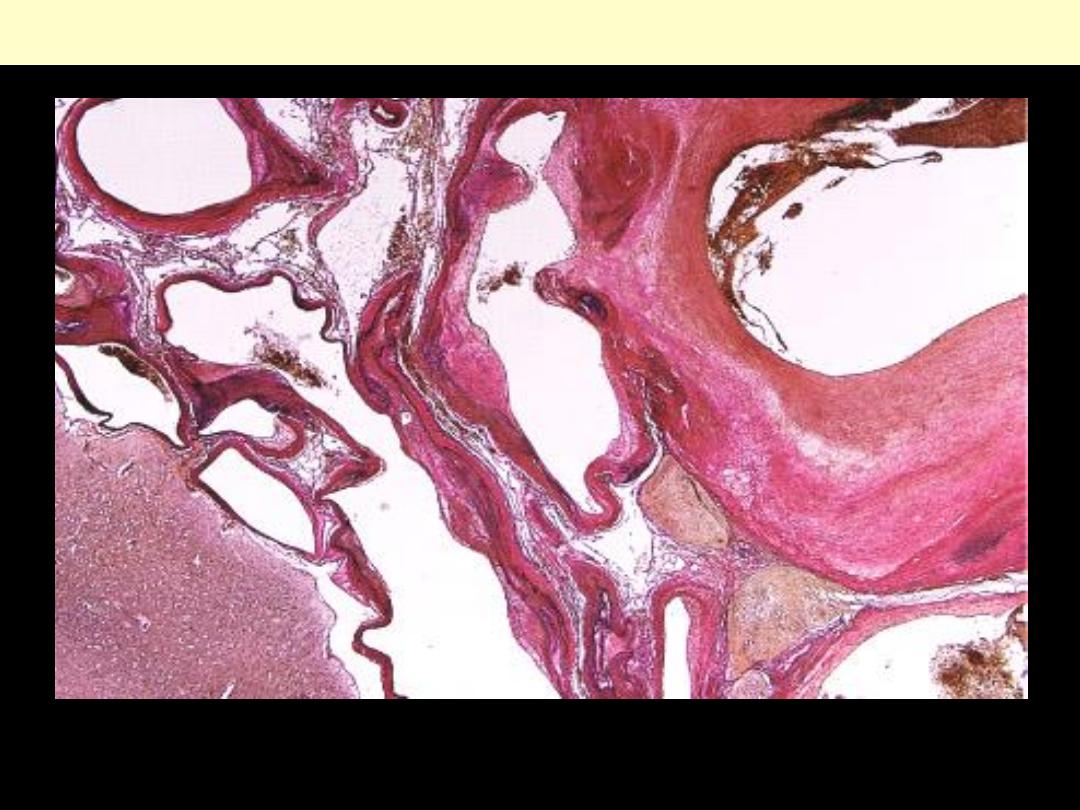
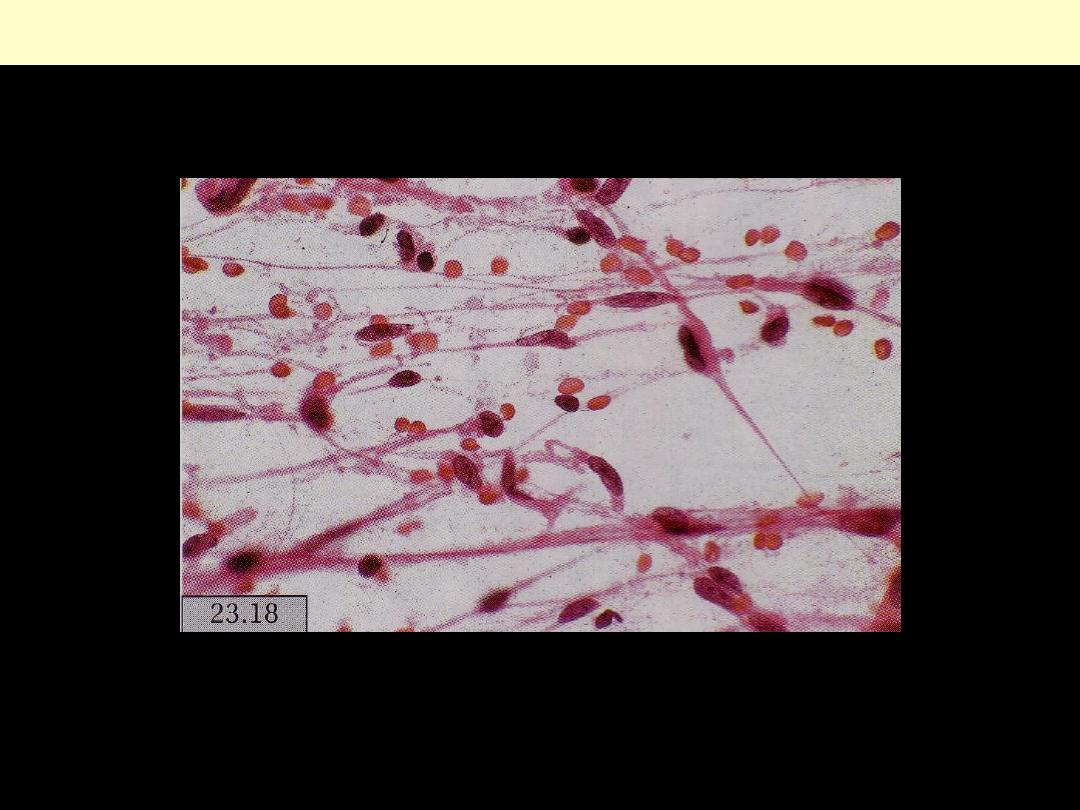
Arteriovenous malformation
Ectatic, variably muscularized blood vessels with interrupted elastic lamina and fibrotic intimal
thickening participate in this malformative lesion (Van Gieson stain).
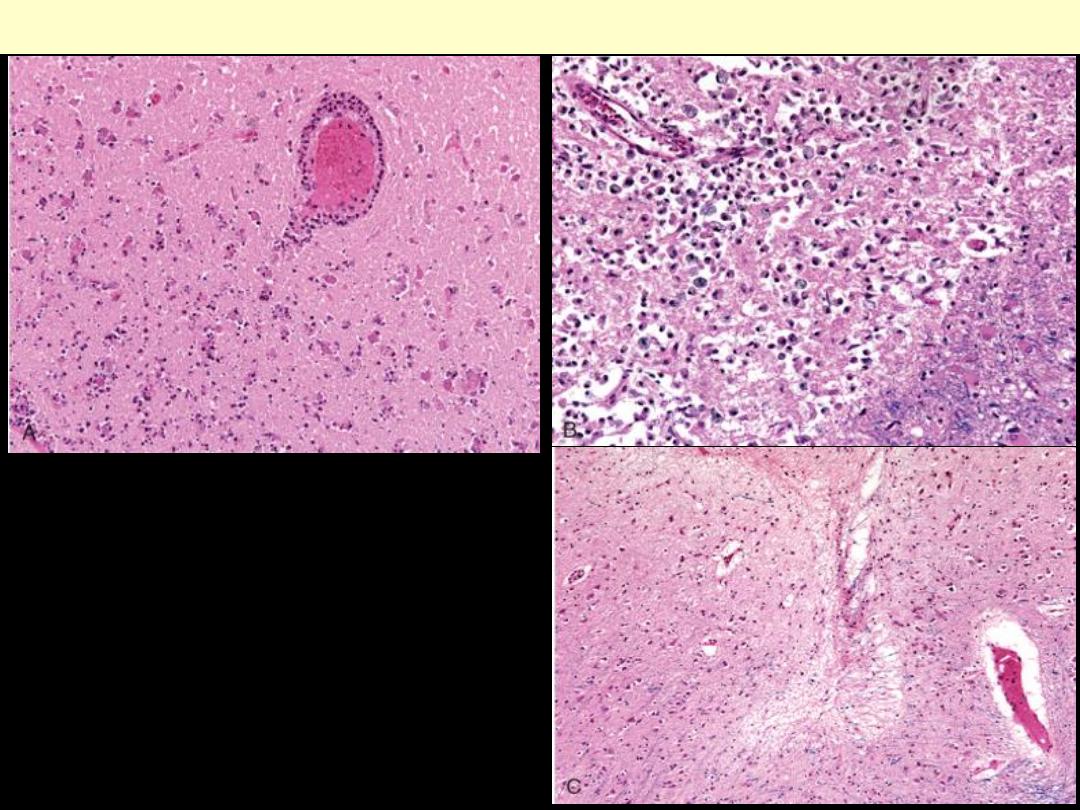
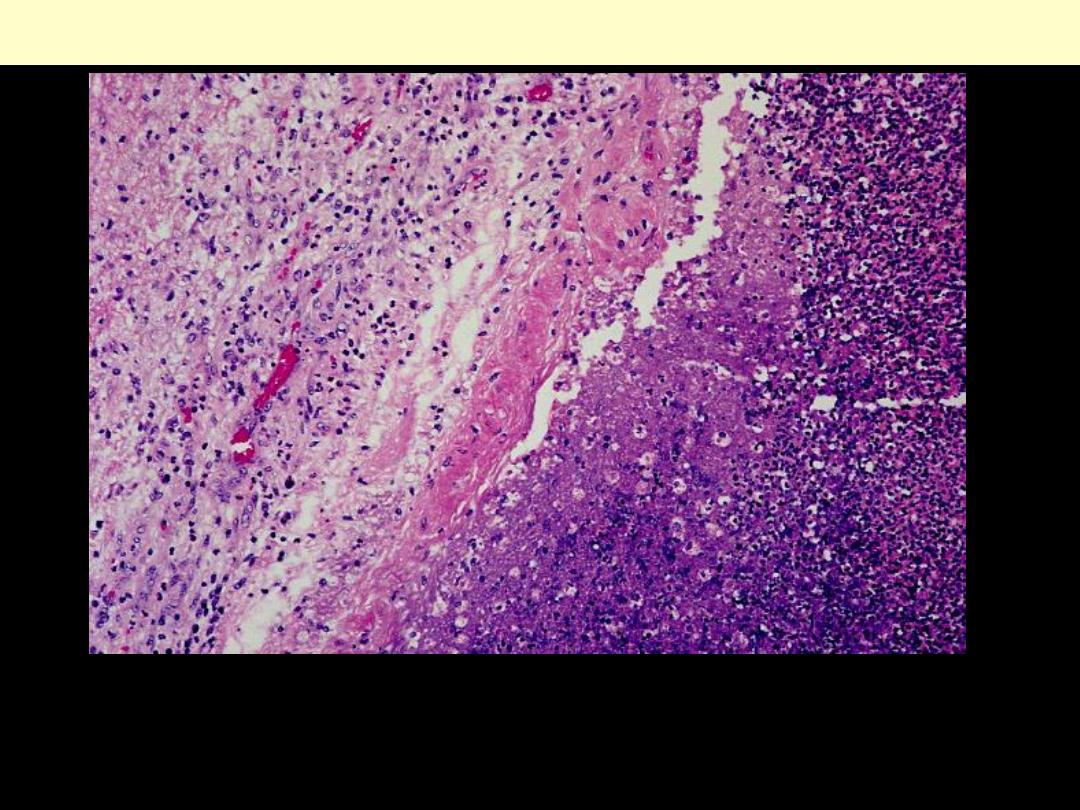
A: Infiltration of a cerebral infarction by
neutrophils begins at the edges of the lesion
where vascular supply has remained intact.
B: After about 10 days, an area of infarction
is characterized by the presence of
macrophages and surrounding reactive
gliosis.
C: Remote small intracortical infarcts are
seen as areas of tissue loss with a small
amount of residual gliosis.
Cerebral infarction
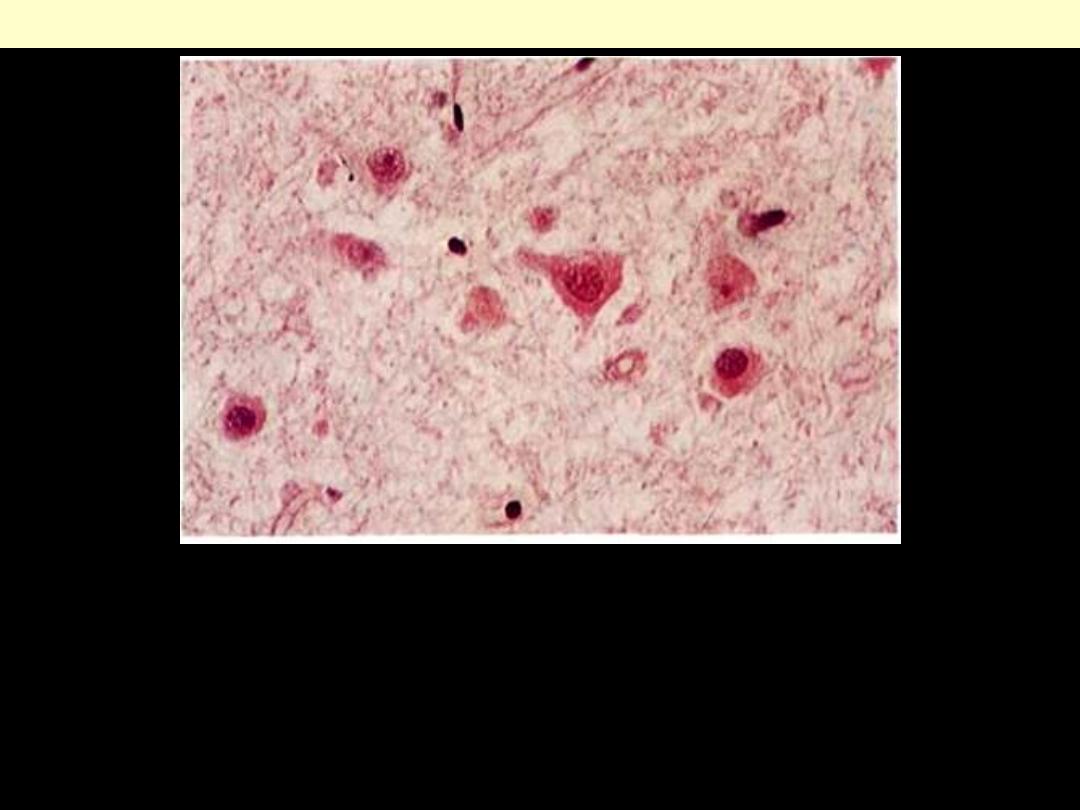
Ischemic (red) neurons
The cells are shrunken and have lost their Nissil substance and
cytoplasmic basophilia. Nuclei are preserved, but nucleoli are
indistinct. (H.&E.x 280)
Ischemic neuron later change
Cellular shrinkage is more pronounced and the nuclei have
almost disappeared.
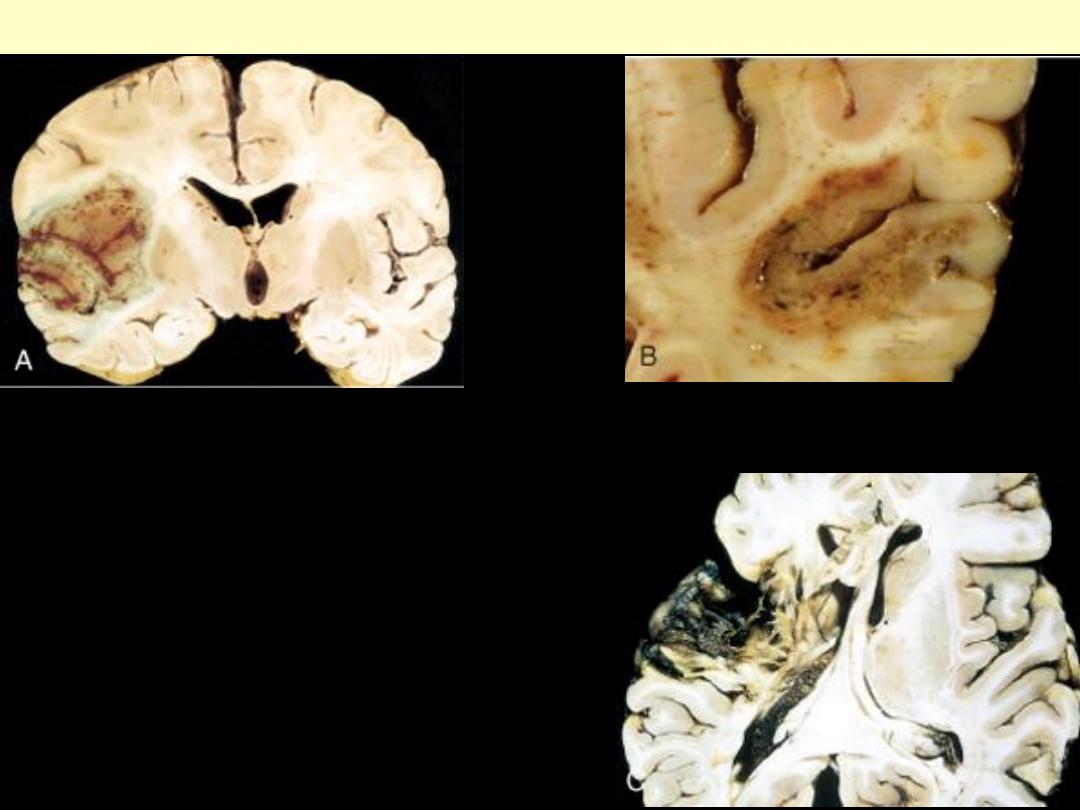
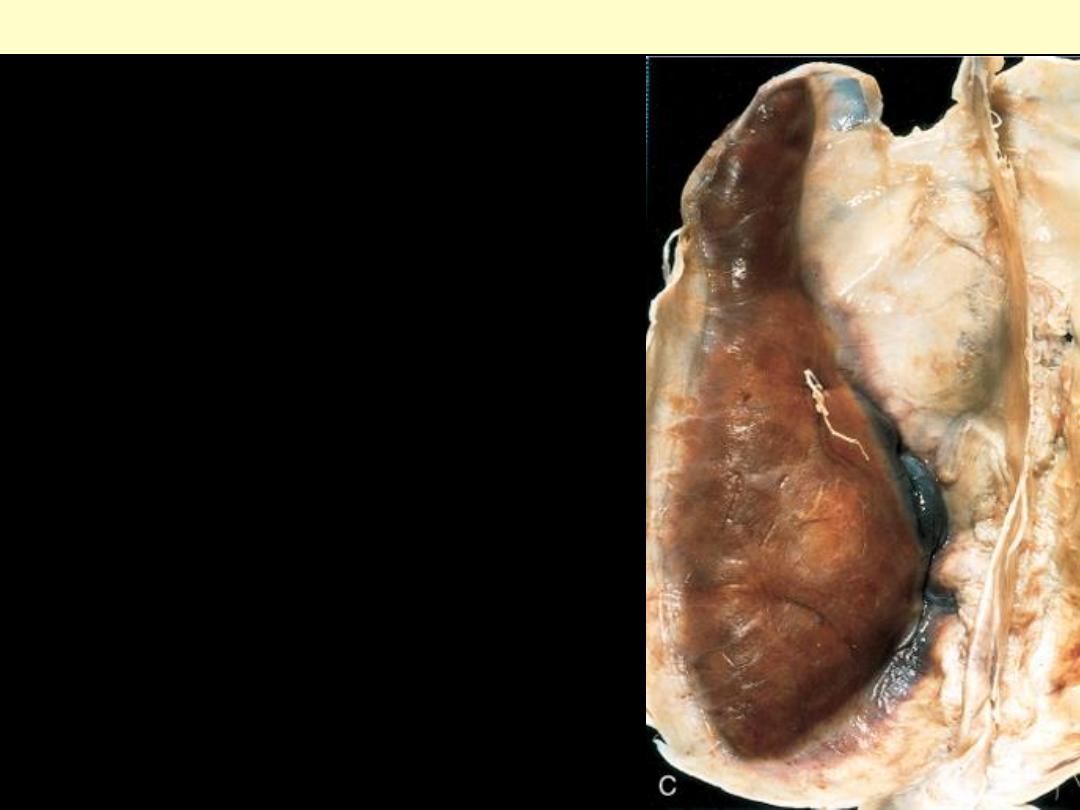
A: Section of the brain showing a
large, discolored, focally hemorrhagic
region in the left middle cerebral
artery distribution (hemorrhagic, or
red, infarction). B: An infarct with
punctate hemorrhages, consistent with
ischemia-reperfusion injury, is present
in the temporal lobe. C, Old cystic
infarct shows destruction of cortex and
surrounding gliosis.
Cerebral infarction
Infarction hemorrhagic brain
A' Sections of the brain showing a large, discolored, focally hemorrhagic region in the left middle
cerebral artery distribution (Hgic, or red, infarction).
Recent infarction in the distribution of the
right middle cerebral artery which could
have been caused by thrombosis. There is
haemorrhage into the anterior portion of the
infarct and the temporal lobe is soft and
swollen, as can be seen by comparing it with
the left temporal lobe.
Cerebral infarction.
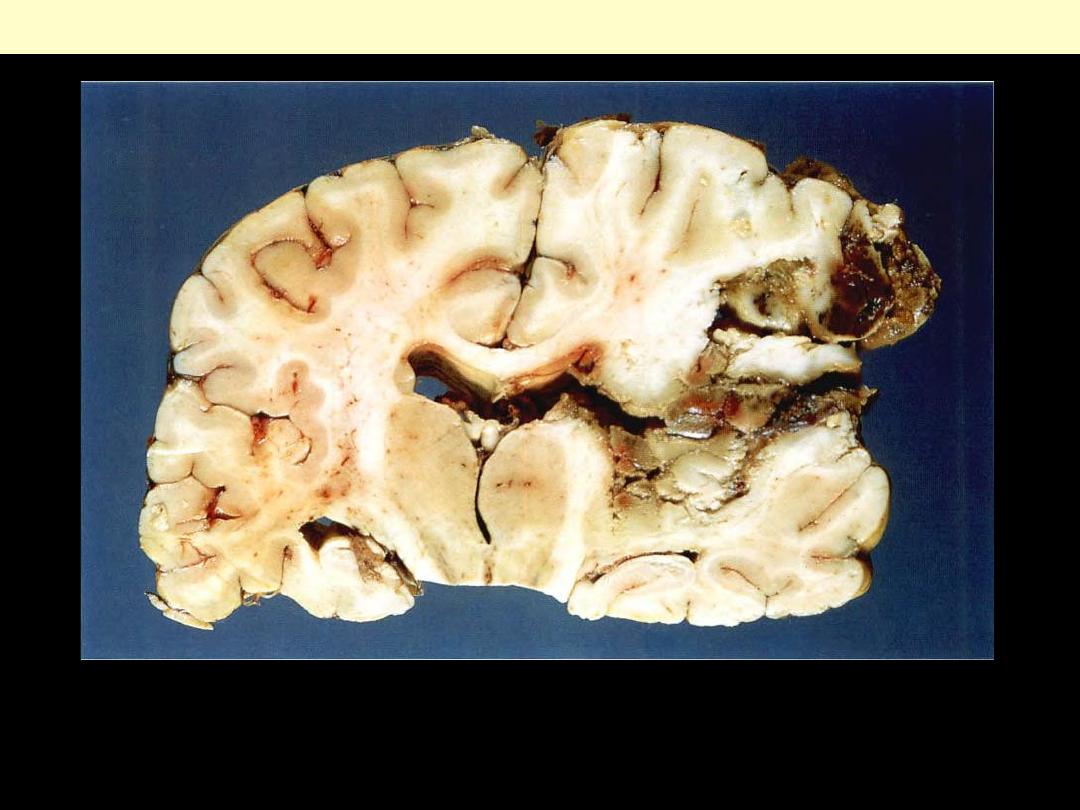
Vertical section of brain showing haemorrhagic infarction in the distribution of the right middle
cerebral artery.
Cerebral infarction
Old infarction in the distribution of the left middle cerebral artery. The necrotic brain substance has
liquefied, leaving a cyst.
Cerebral infarction
By 1 month
- more softening and liquefaction
- development of irregular cavities
By about 6 months
- complete liquefaction represented by a cyst.
Cerebral infarction
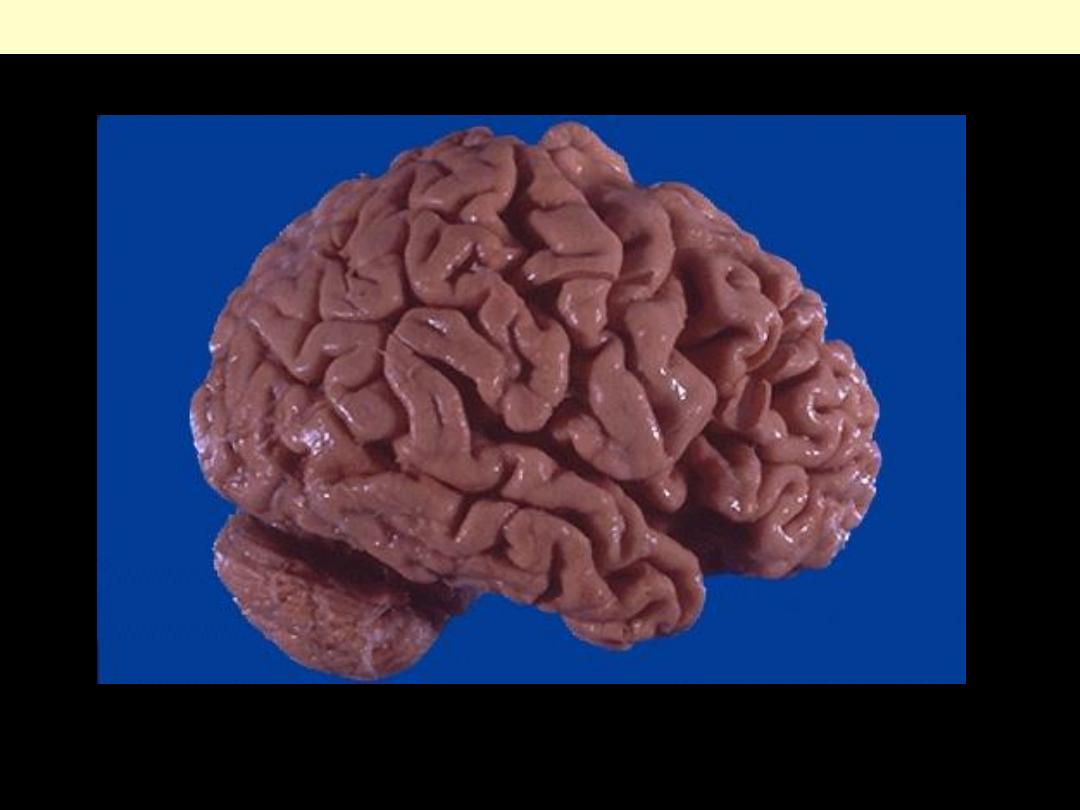
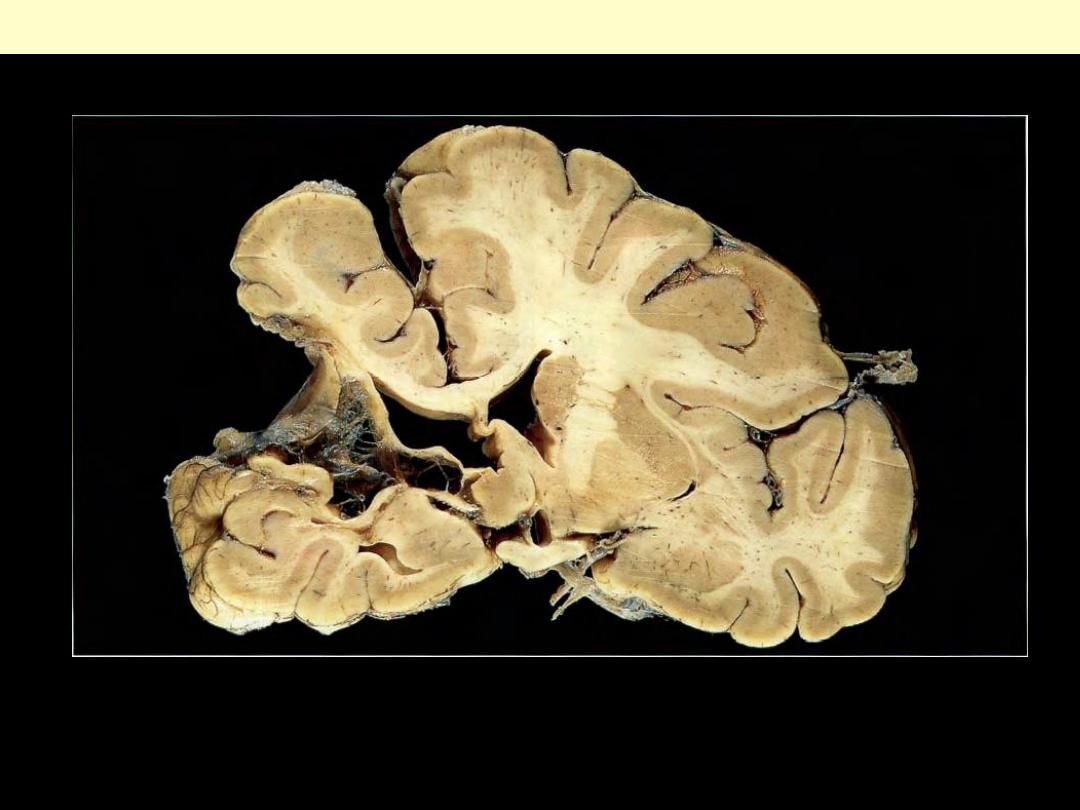
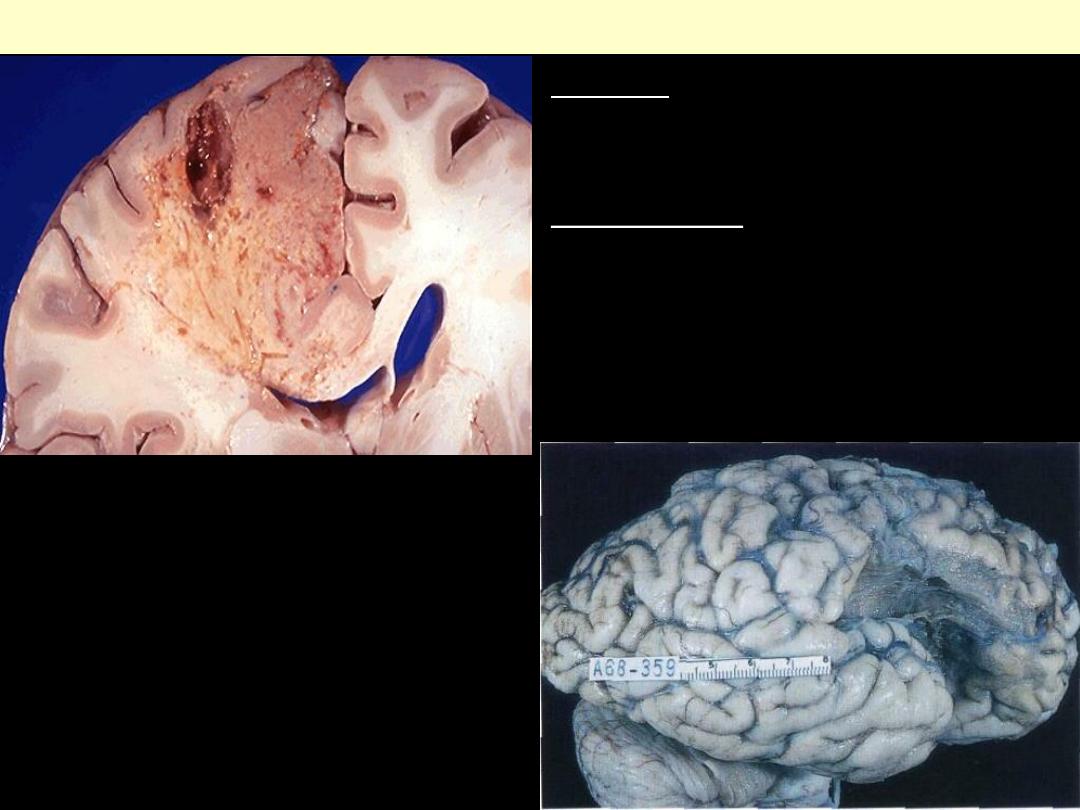
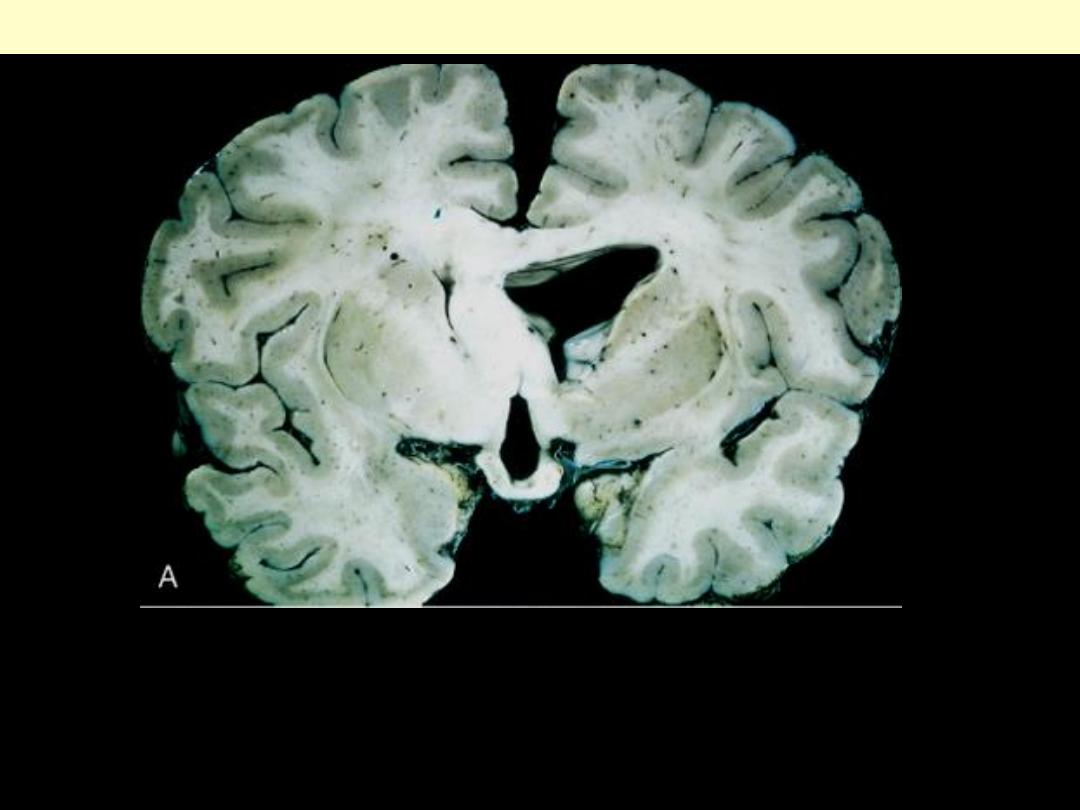
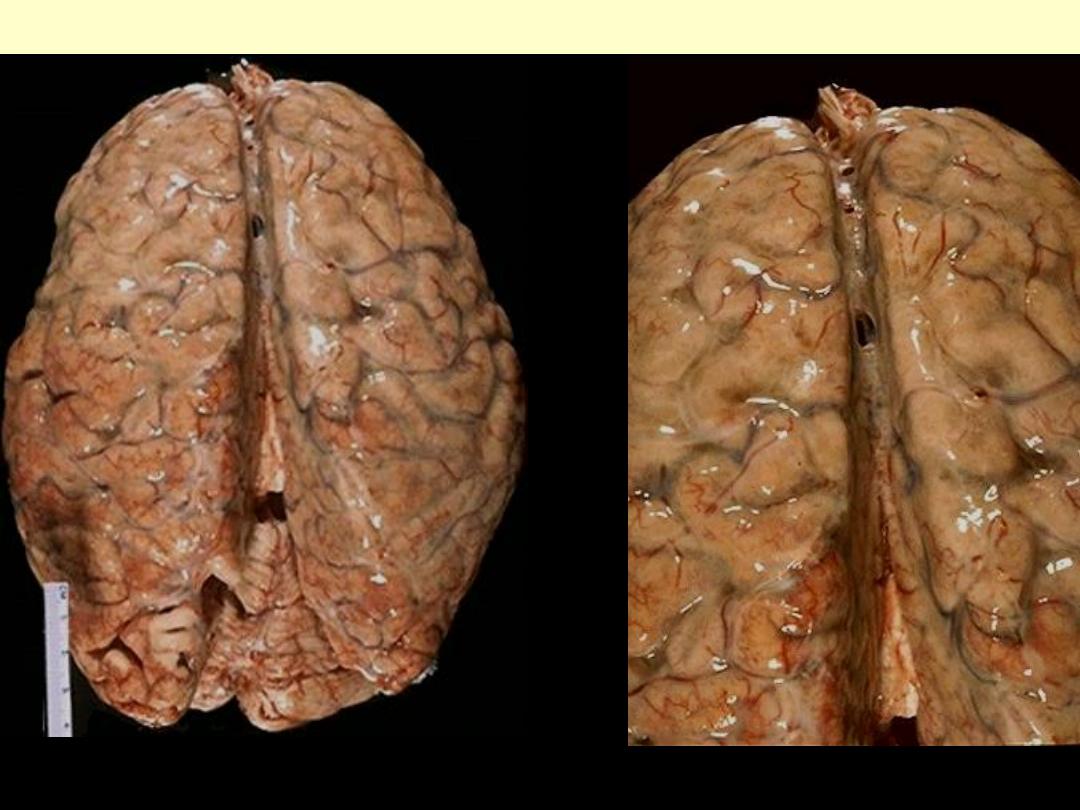
The cerebral atrophy seen here mainly in the frontal and parietal regions is characterized by narrowed
gyri and widened sulci. The atrophy seen here was due to senile dementia of the Alzheimer's type
(Alzheimer's disease).
Alzheimer disease
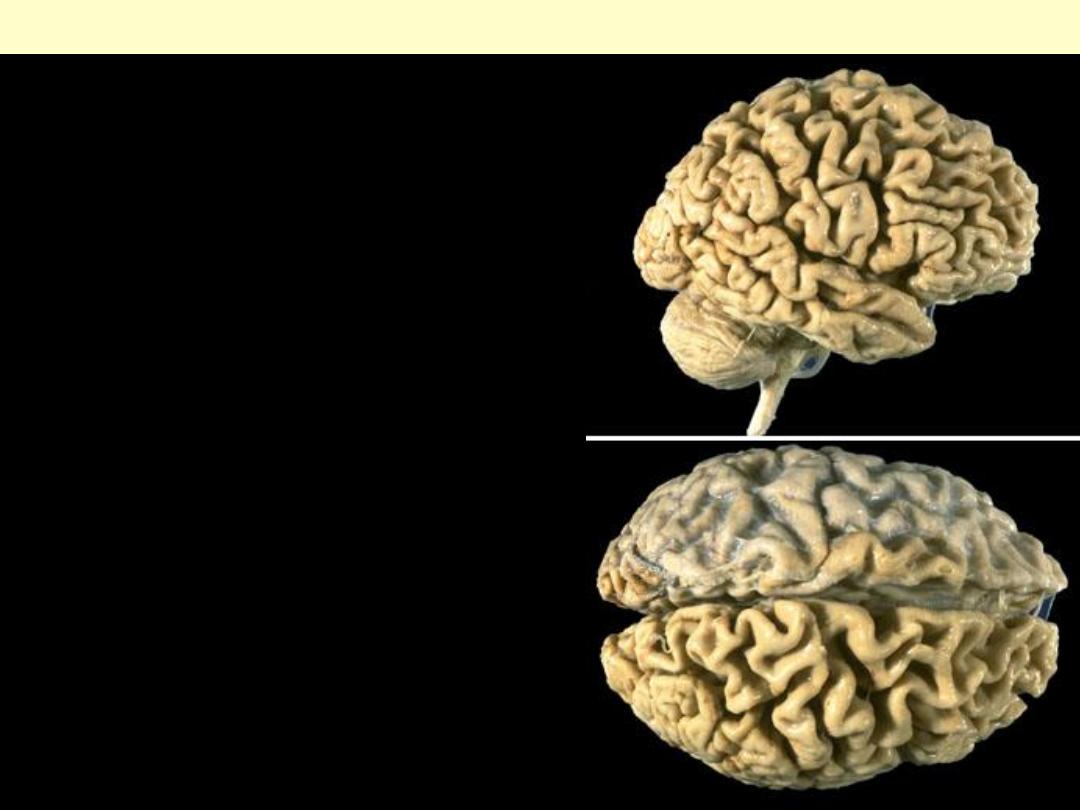
There is marked atrophy
seen superiorly and
laterally, with sparing of the
occipital region.
Alzheimer disease
The cortical atrophy leads to compensatory dilation of the cerebral
ventricles known as "hydrocephalus ex vacuo".
Alzheimer disease
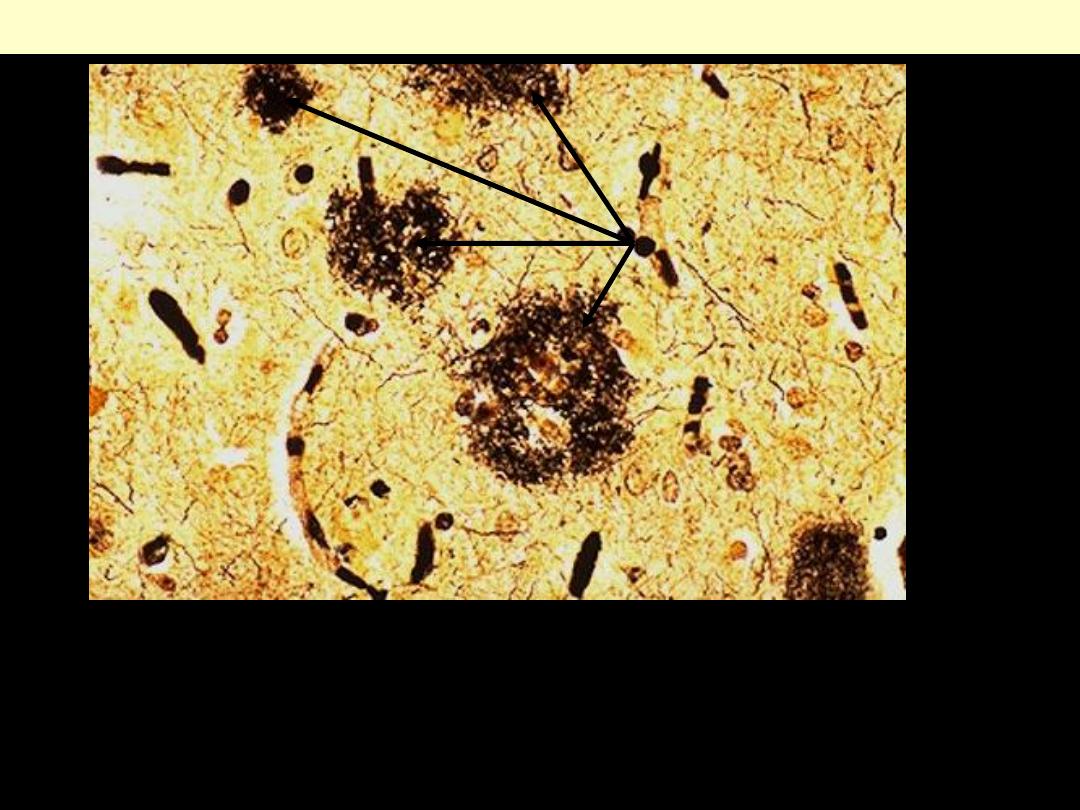
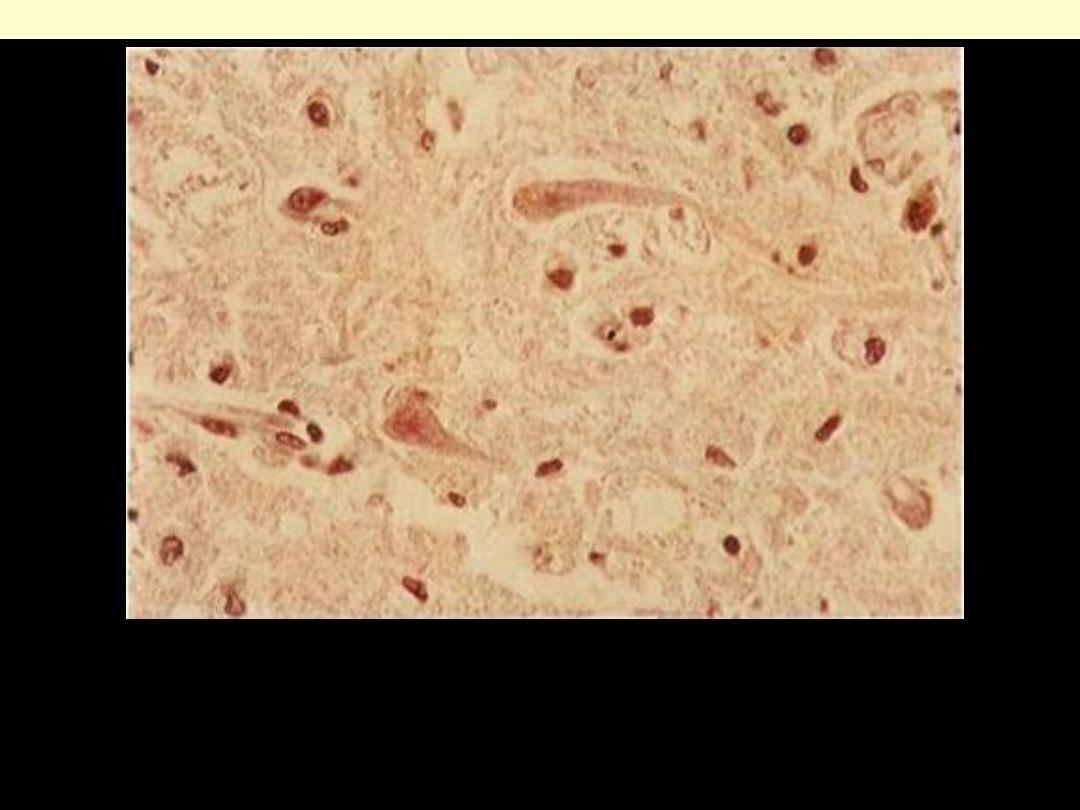
The plaques of Alzheimer disease are seen here with a silver stain
(arrows). Such plaques are most numerous in the cerebral cortex
and hippocampus. This dementia is marked mainly by progressive
memory loss.
Plaques in Alzheimer disease
This is a neurofibrillary
"tangle" of Alzheimer disease.
The tangle appears as long pink
filaments in the cytoplasm.
They are composed of
cytoskeletal intermediate
filaments.
Neurofibrillary tangles of Alzheimer disease
Neurofibrillary tangles of
Alzheimer's disease are also
seen best with a silver stain, as
shown here.
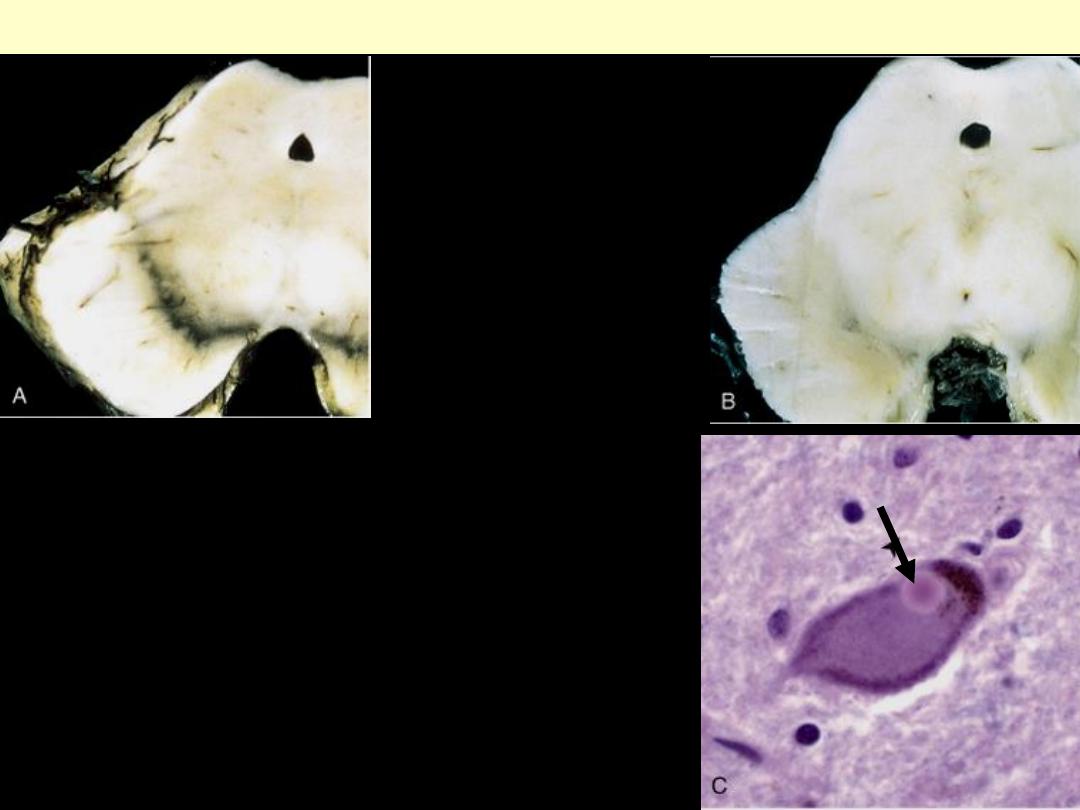
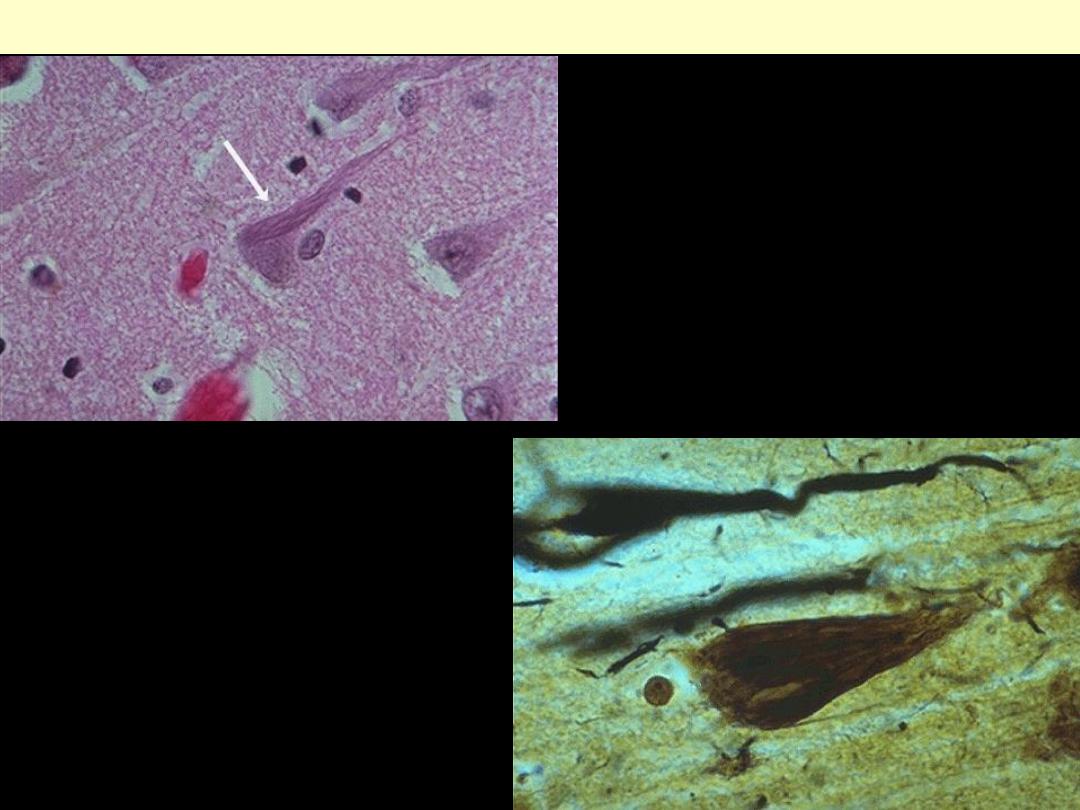
A: Normal substantia nigra.
B: Depigmented substantia nigra
in idiopathic Parkinson disease.
C: Lewy body in a neuron from
the substantia nigra stains pink
(arrow).
Parkinson disease
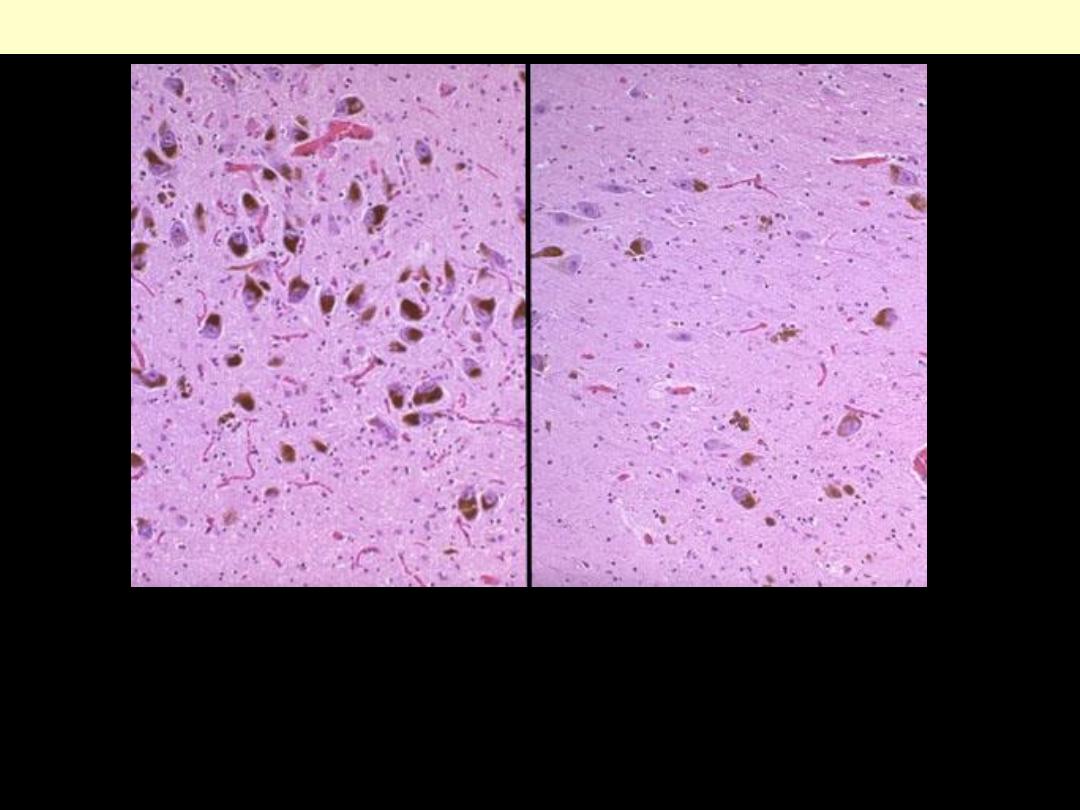
At the left: normal numbers of neurons in the subtantia nigra are
pigmented. At the right: there is loss of neurons and loss of
pigmentation with Parkinson's disease.
Parkinson disease
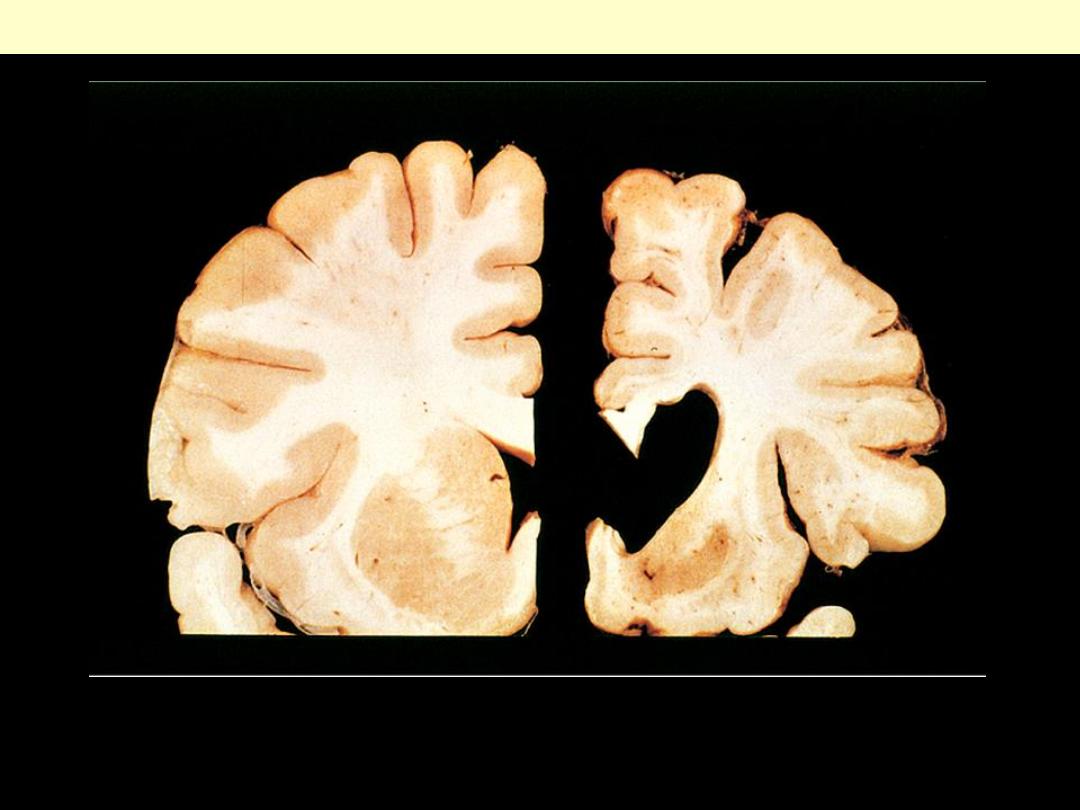
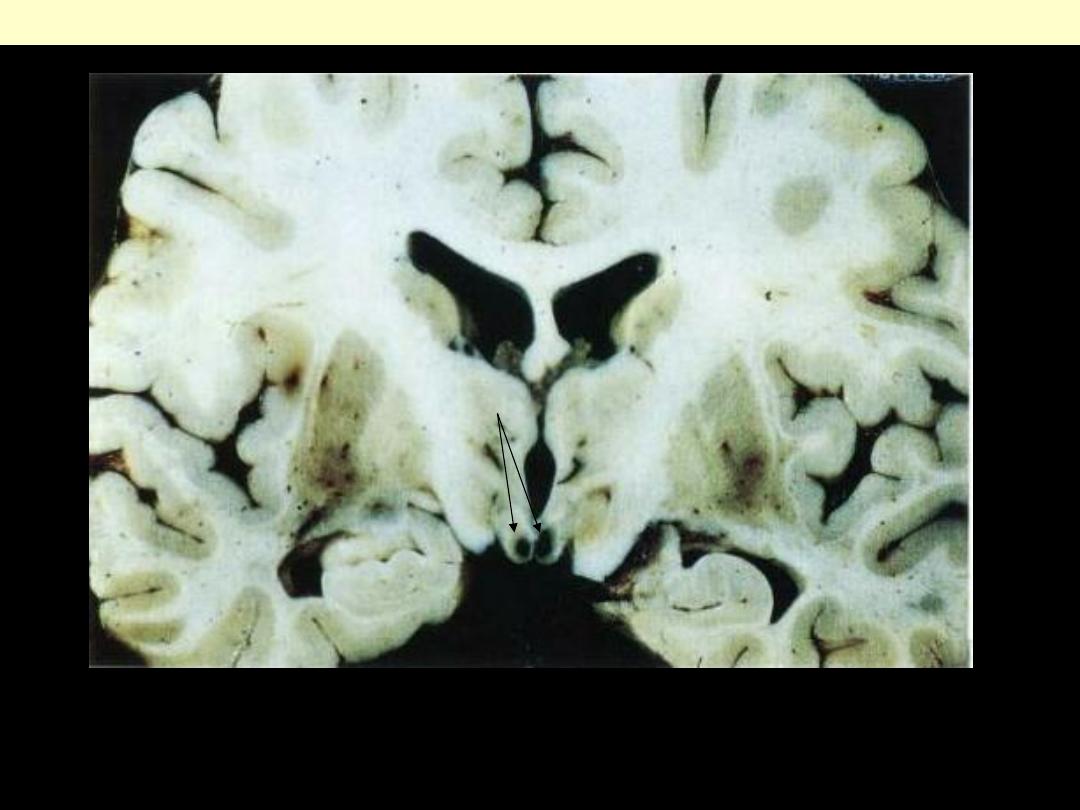
Normal hemisphere on the left compared with the hemisphere with Huntington disease on the right
showing atrophy of the striatum and ventricular dilation.
Huntington disease
This is seen as expanded white matter of the left cerebral hemisphere
and thickened corpus callosum and fornices.
Astrocytoma (Low-grade)

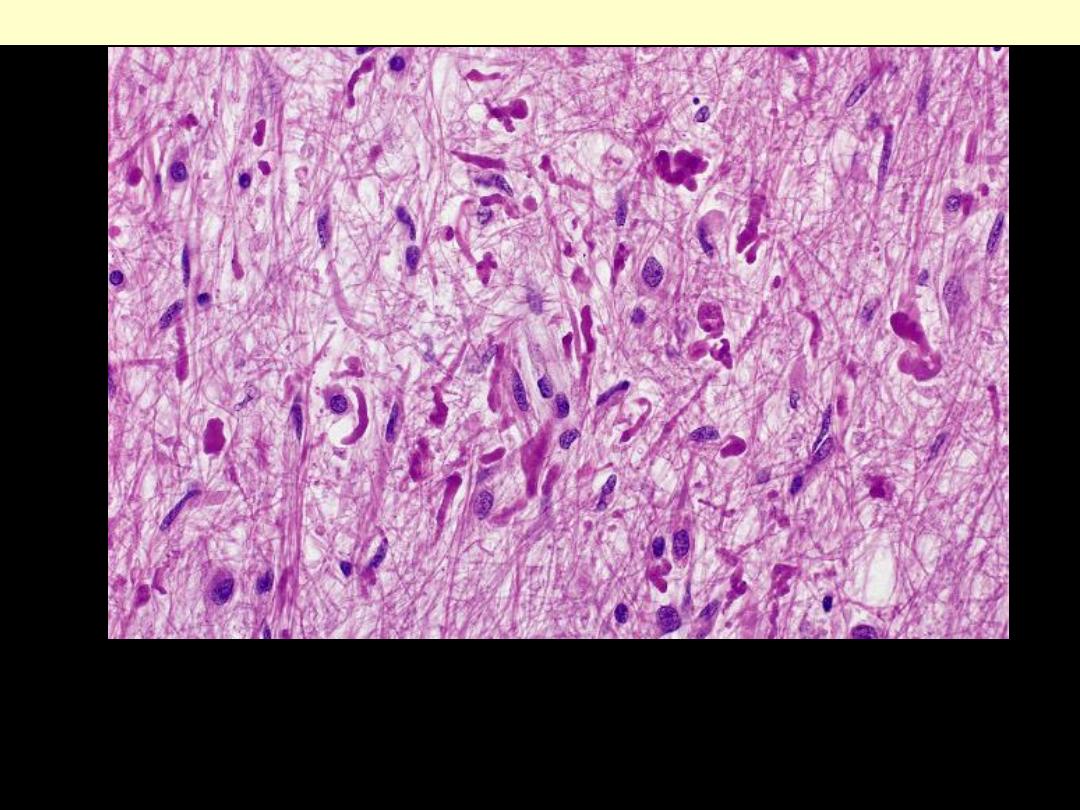
Insidious permeation of brain tissue is typical of the fibrillary astrocytoma as illustrated in this
anterior temporal lobectomy specimen. The gyrus at right maintains a clearly demarcated cortical
ribbon over its digitate white matter. Moving to the left, there is diffuse gyral expansion and effacement
of these landmarks, reflecting tumoral infiltration. No discrete mass is formed, and, as is characteristic
of low-grade examples, there is no evident hemorrhage or necrosis
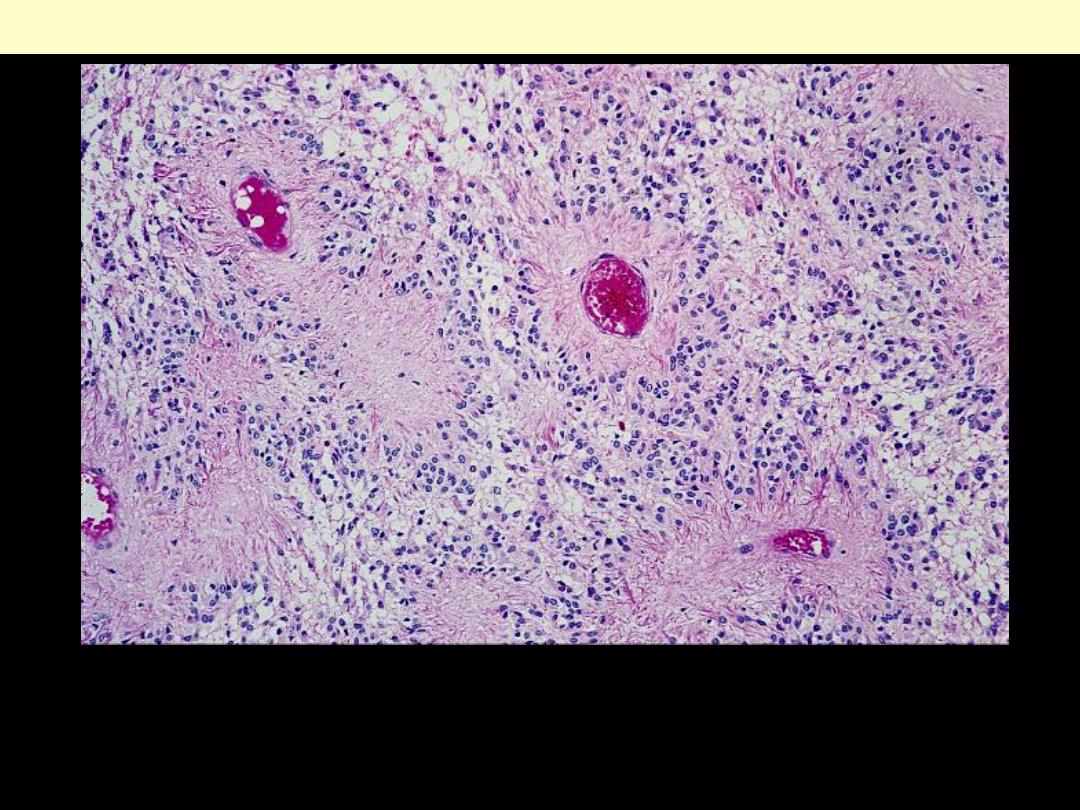
Diffusely infiltrating astrocytoma cerebrum
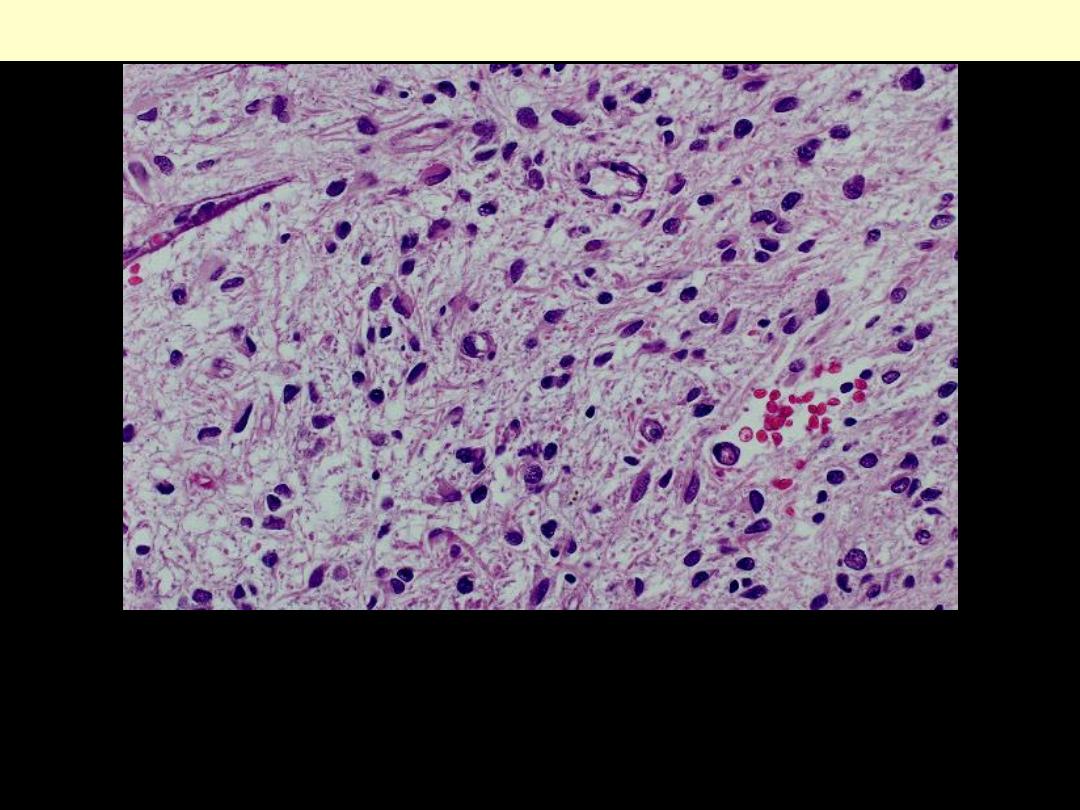
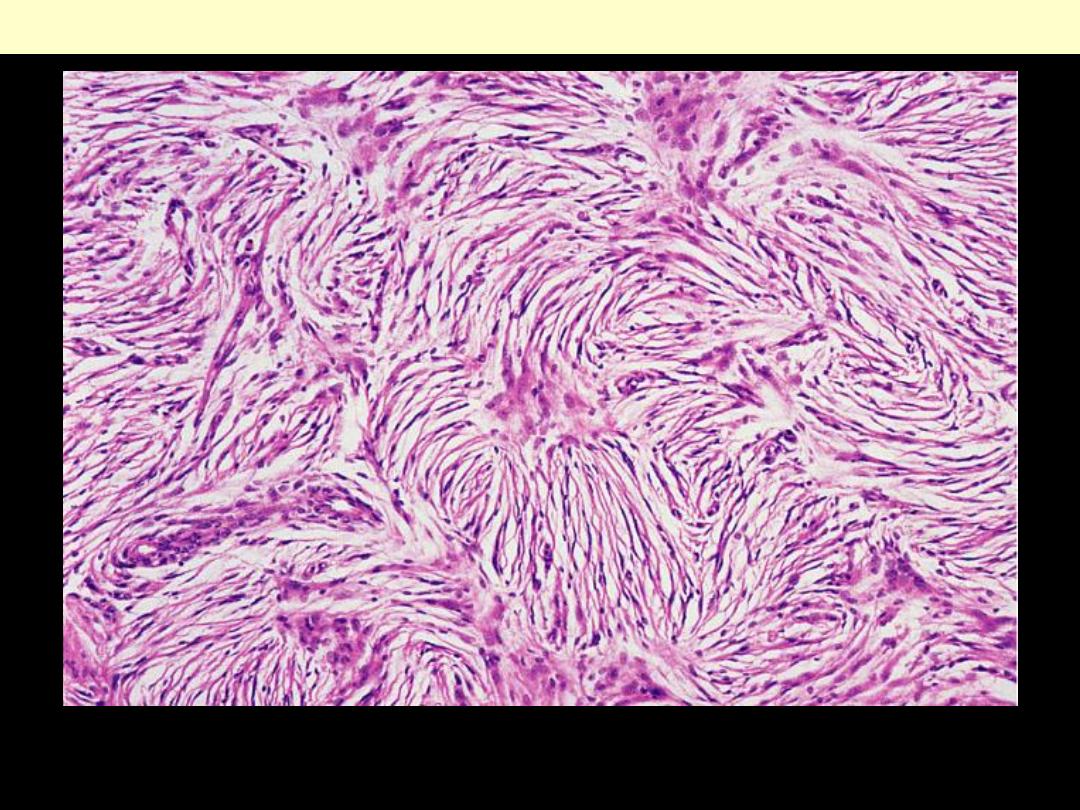
Proliferation of fibrillary astrocytes with rich fibrillary background.
There is little pleomrphism and only modest hyperchromasia.
Absence of mitoses is supportive There is no necrosis or vascular
endothelial hyperplasia.
Diffusely infiltrating astrocytoma
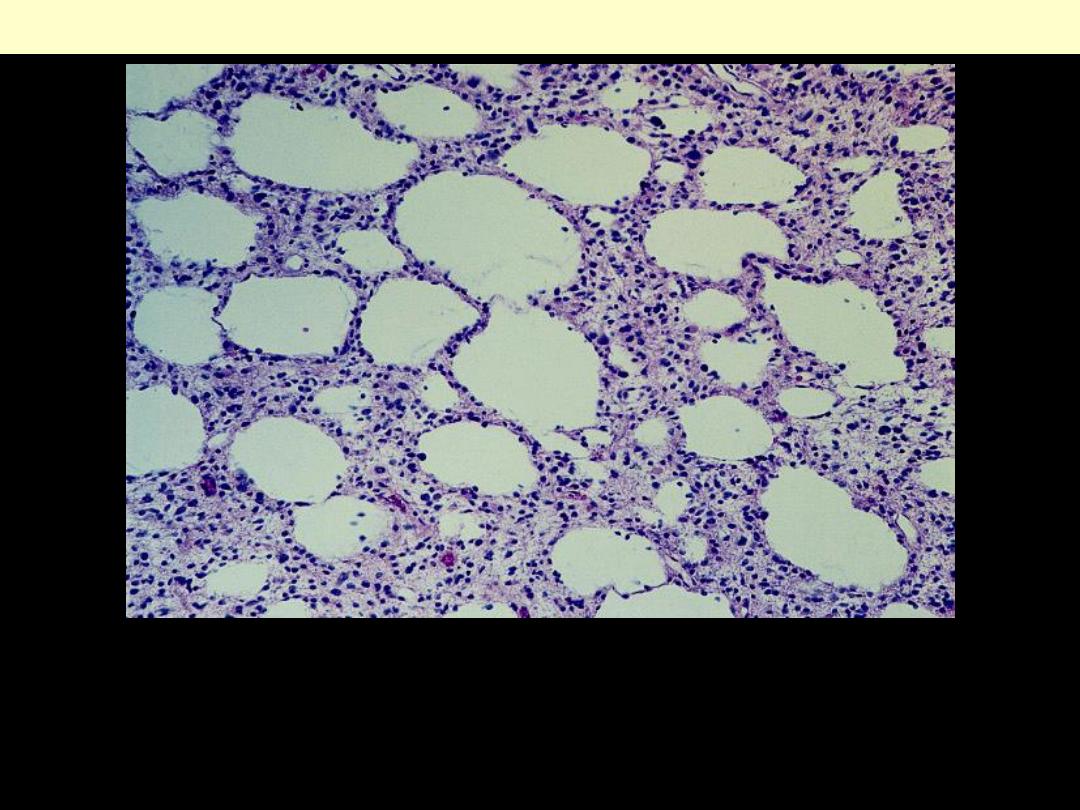
Microcystic change is a particularly conspicuous feature of some
low-grade astrocytomas. This does not occur in reactive gliosis.
Diffusely infiltrating astrocytoma; microcystic change
This is appearing as a
necrotic, hemorrhagic,
infiltrating mass.
Glioblastoma multiforme
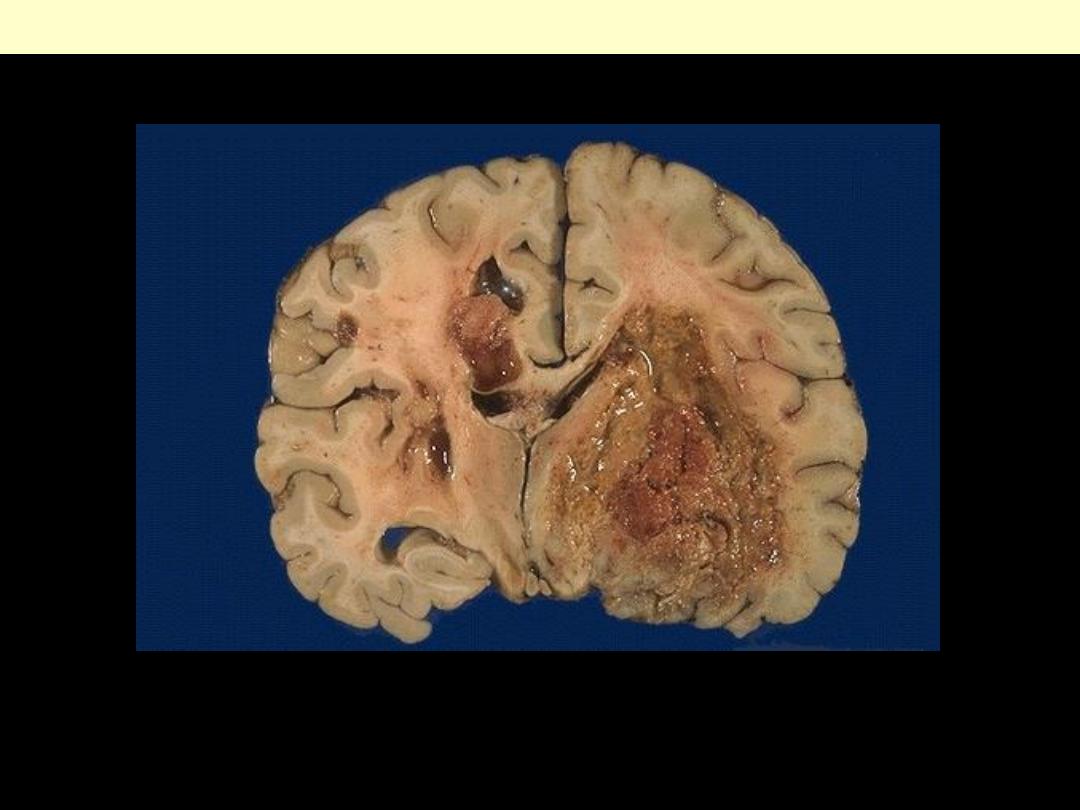
This is the worst possible form of glioma--a glioblastoma multiforme. These neoplasms are quite vascular with
prominent areas of necrosis and hemorrhage. Note how this one has crossed the midline to the opposite hemisphere.
Glioblastoma multiforme cerecrum coronal section
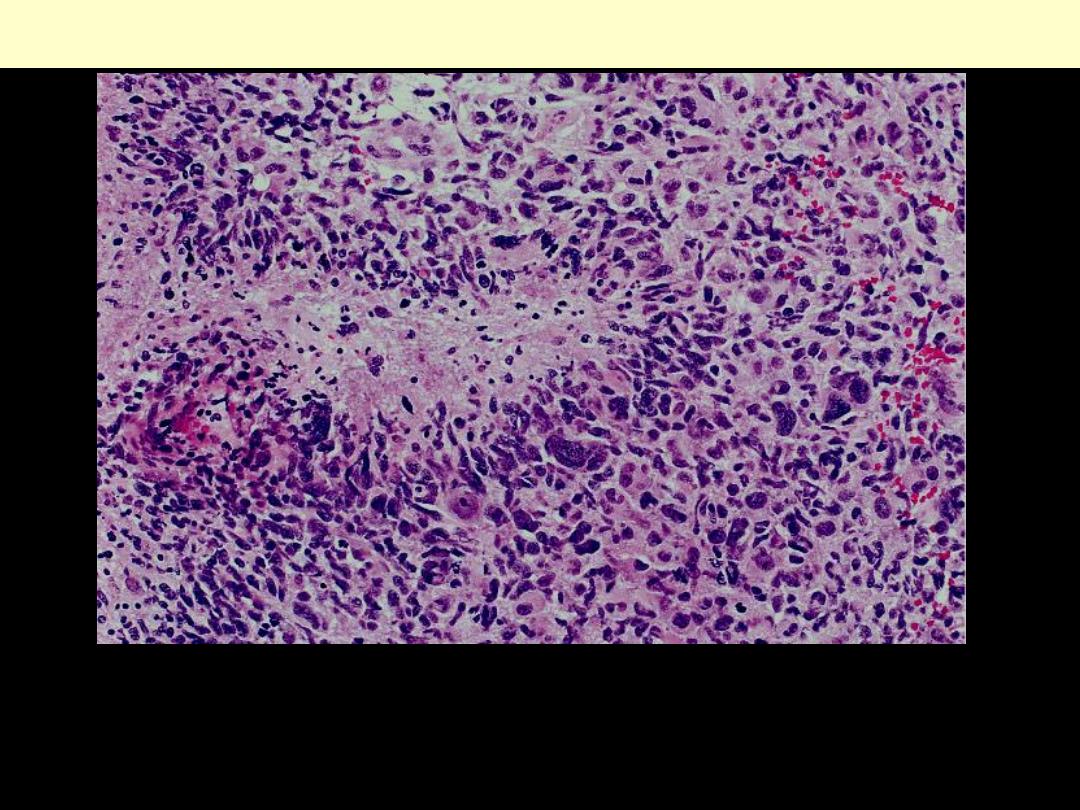
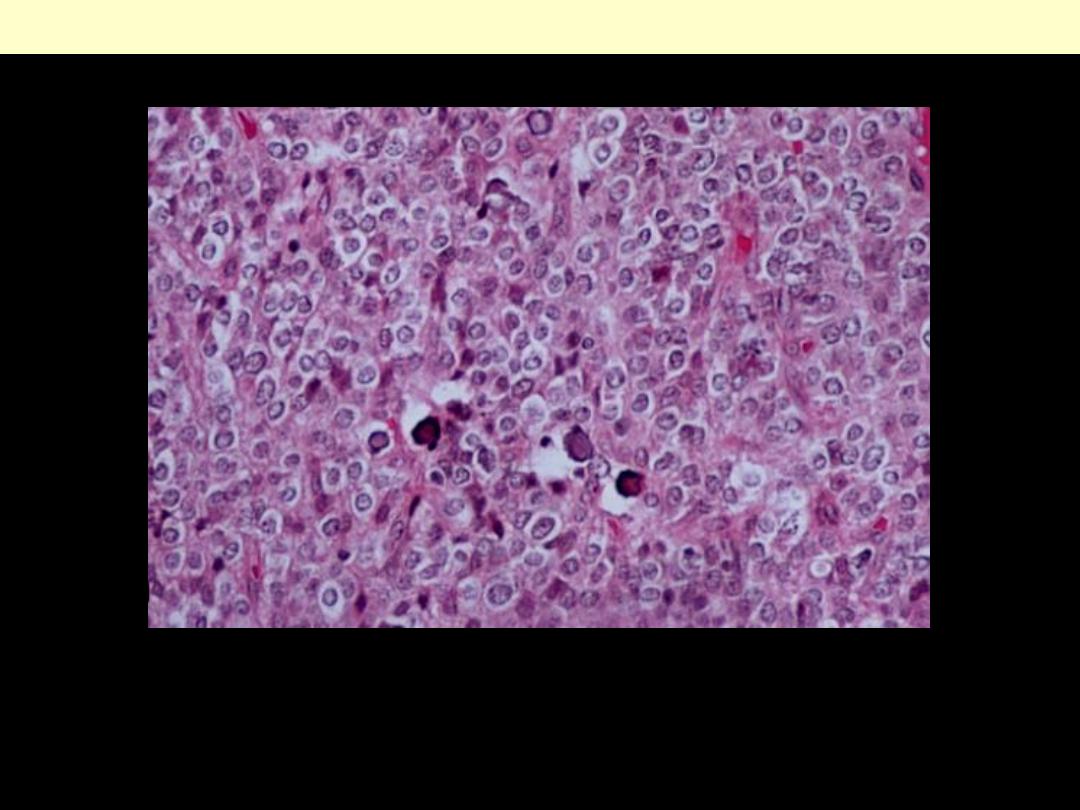
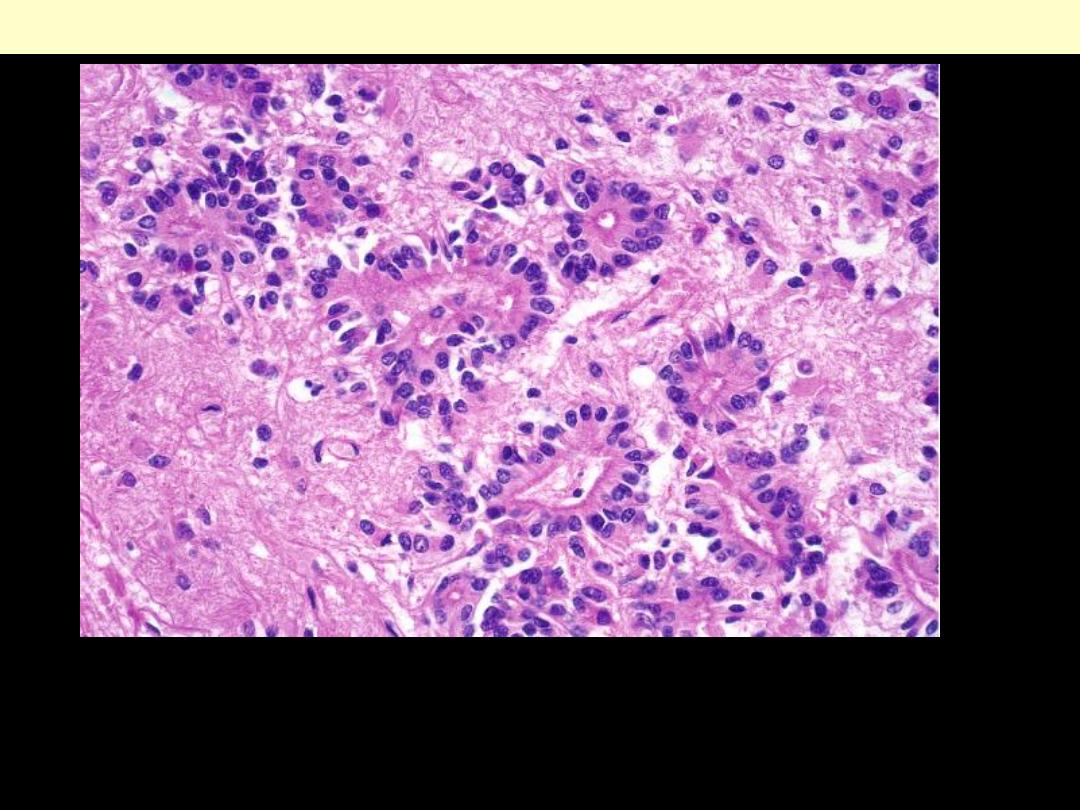
Dense cellularity, striking pleomorphism, and zones of coagulative
necrosis lined by "palisading" tumor cells characterize the
prototypical glioblastoma.
Glioblastoma multiforme: Necrosis
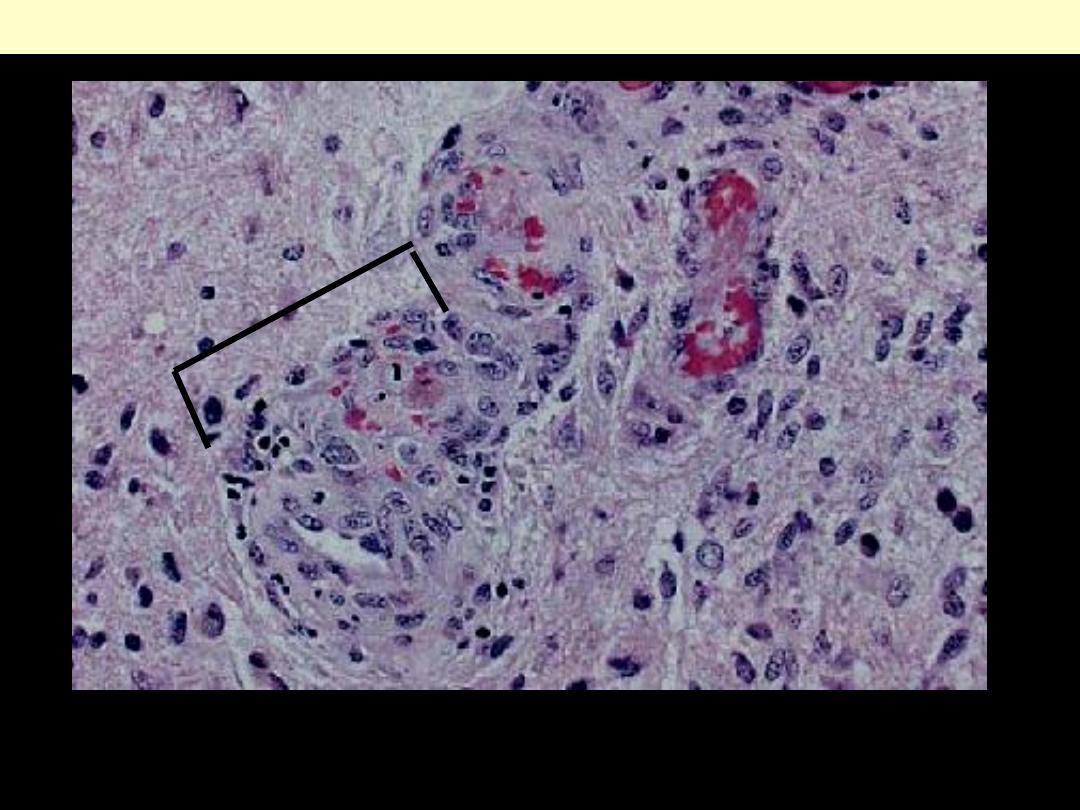
Note the complex, "glomeruloid" quality of the microvascular proliferation. Astrocytic elements are
seen at Rt.
Glioblastoma multiforme: vascular endothelial hyperplasia
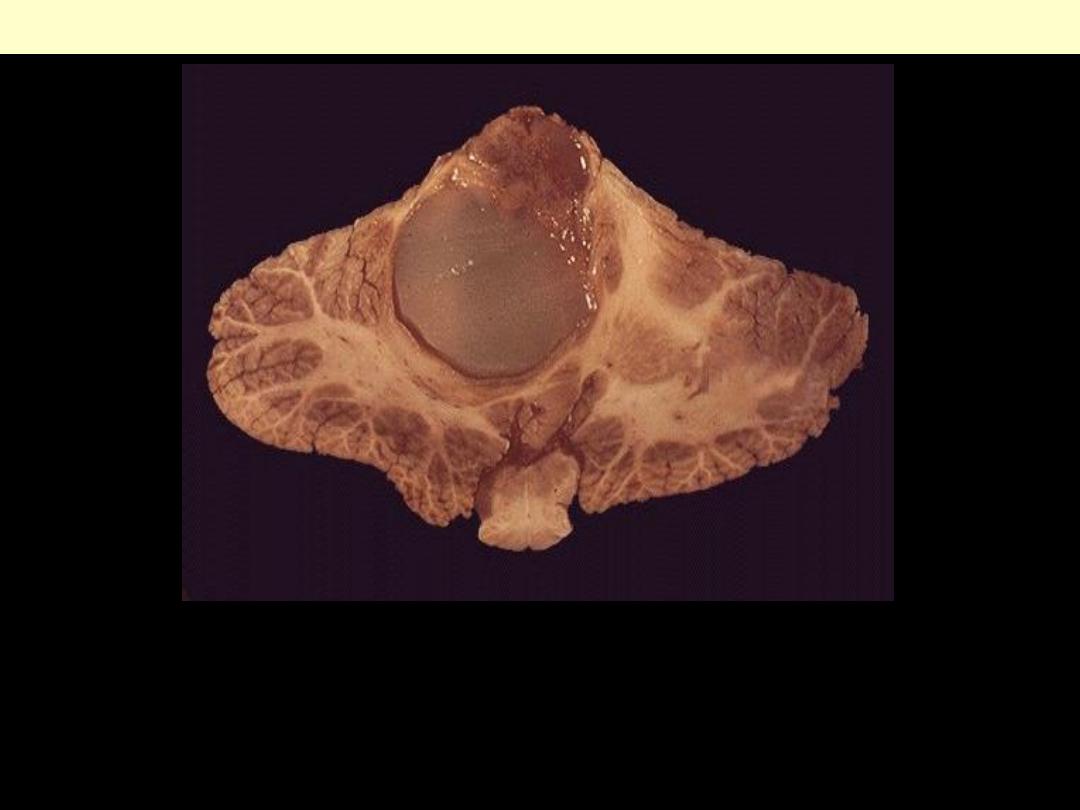
Pilocytic astrocytoma
This is a cystic tumor of the cerebellum in a child. Most childhood
brain tumors arise below the tentorium, which is the reverse of the
adult. Gliomas in children, therefore, are most common in the
posterior fossa. They are often cystic.
Pilocytic astrocytoma. vermiform Rosenthal fibers lie among the
otherwise delicate and hair-like cytoplasmic processes for which the
pilocytic astrocytoma is named.
Pilocytic astrocytoma
Pilocytic astrocytoma smear
Pilocytic astrocytoma showing uniform and long bipolar stout processes.
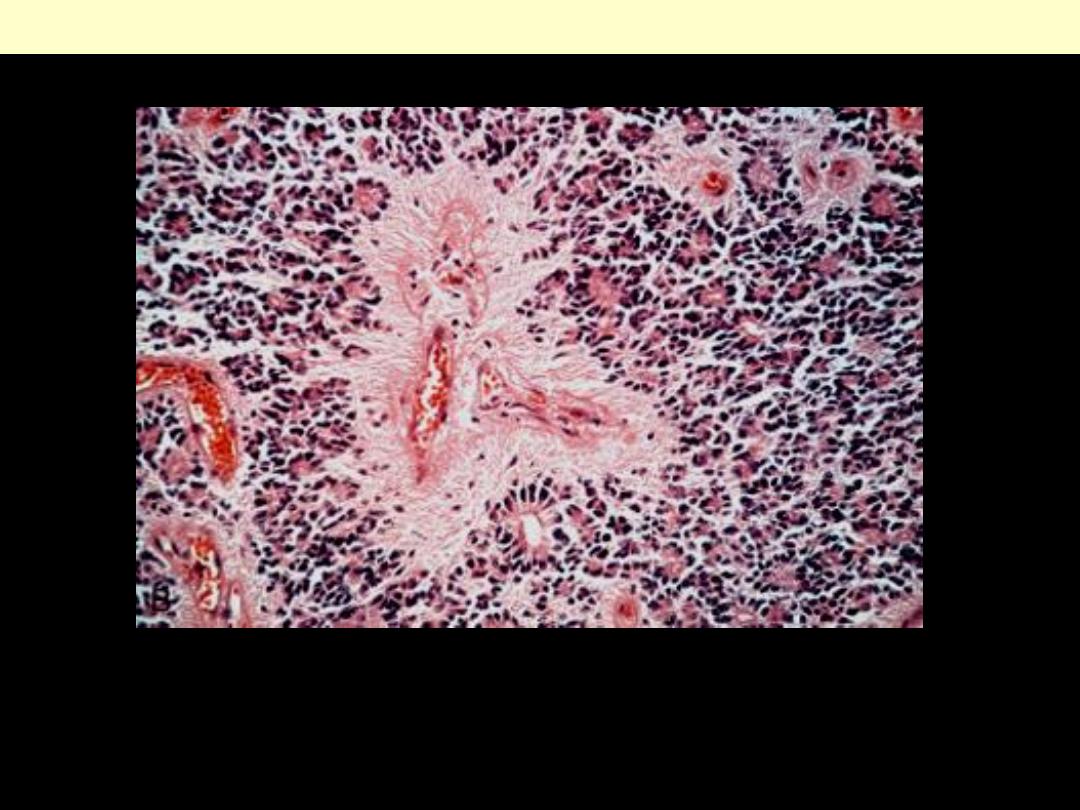
Oligodendroglioma
Oligodendrogliomas: are infiltrative gelatinous, gray tumors.
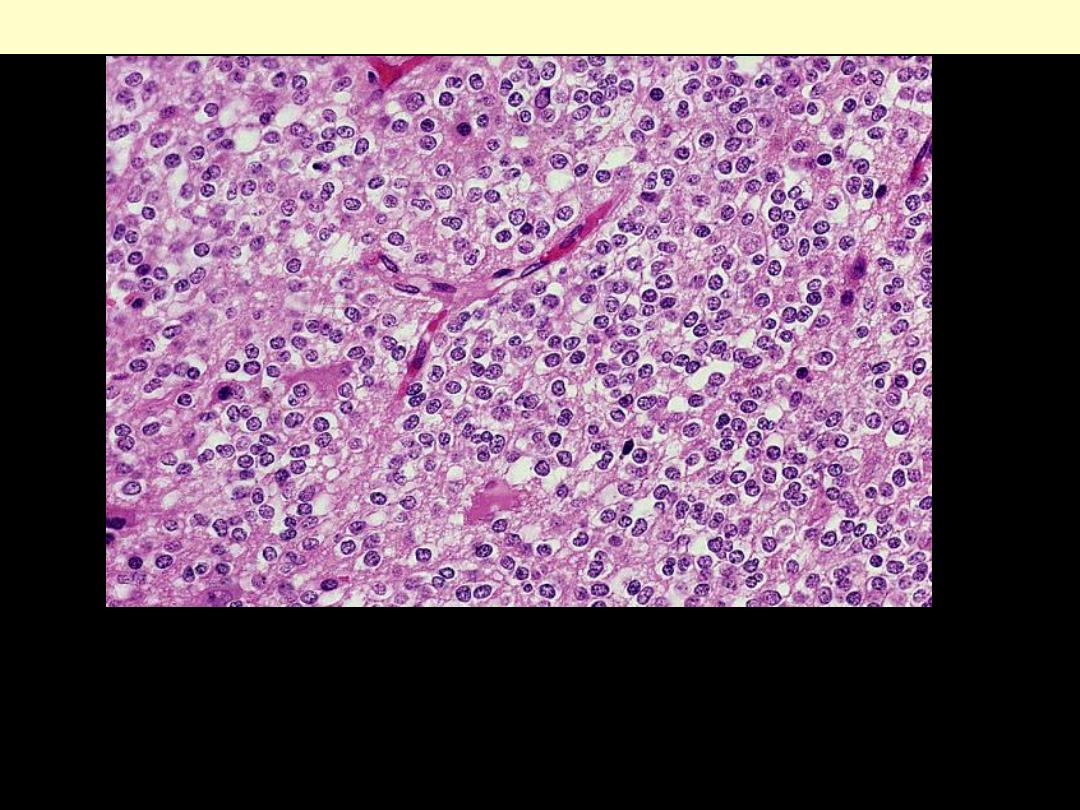
Sheets of uniform, small, round nuclei and clear perinuclear halos
(artefacts of delayed fixation) typify well-differentiated
oligodendrogliomas. Note the delicate network of anastomosing
capillaries.
Oligodendroglioma
Oligodendroglioma composed mainly of cells with round or oval nuclei surrounded by moderate
amounts of clear cytoplasm. There is usually a fine meshwork of capillaries and there are small foci of
calcification.
Oligodendroglioma
Ependymoma
These tumors may arise in both the intracranial compartment and the
spine. Intracranial tumors typically originate from a ventricular surface,
as in the case of this large lesion arising in the fourth
ventricle. It is anchored to the floor of the ventricle.
Ependymoma
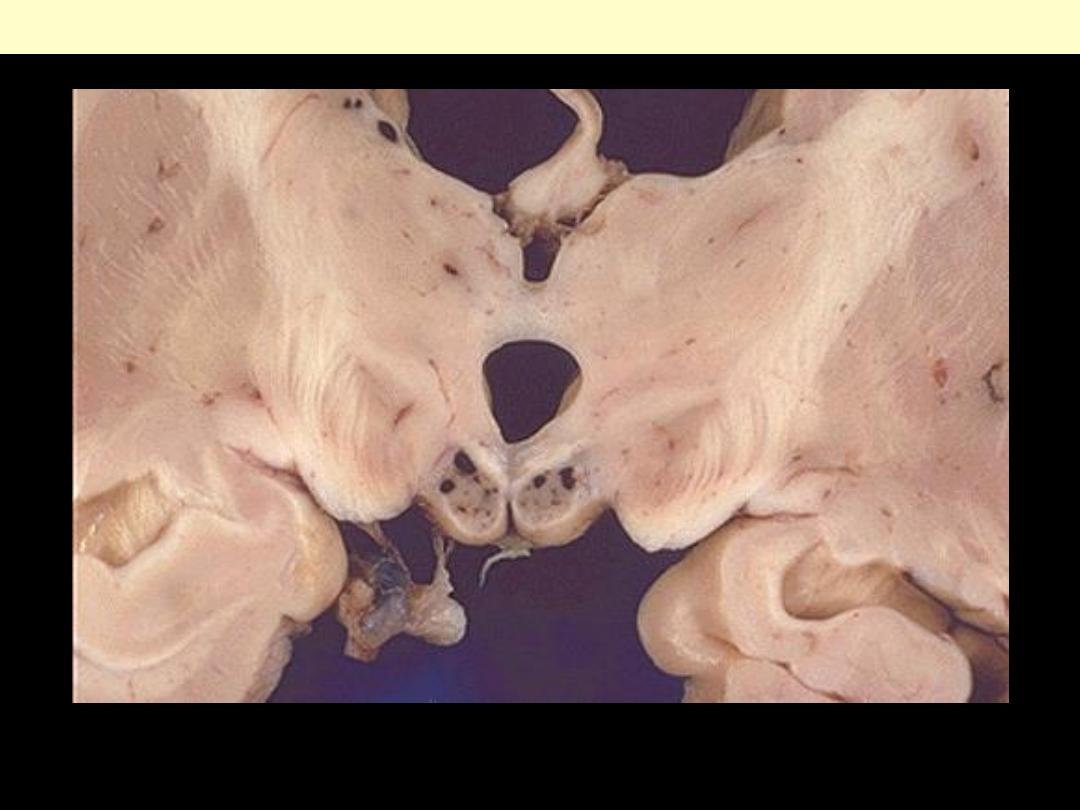
This horizontal section of the
brain reveals a large
ependymoma of the fourth
ventricle.
Ependymoma involving lateral V
Ependymoma
The cytoplasmic processes of ependymal tumor cells condense about
blood vessels to form pseudorosettes.
Ependymoma-Fibrillary pseudorosettes
The true ependymal rosette contains a well-defined central lumen.
Clustered ciliary basal bodies (“blepharoplasts”) are responsible for
the enhanced, granular staining of tumor cell apices.
Ependymoma- rosettes
Tumor cells form rosettes & pseudorosettes.
Ependymoma
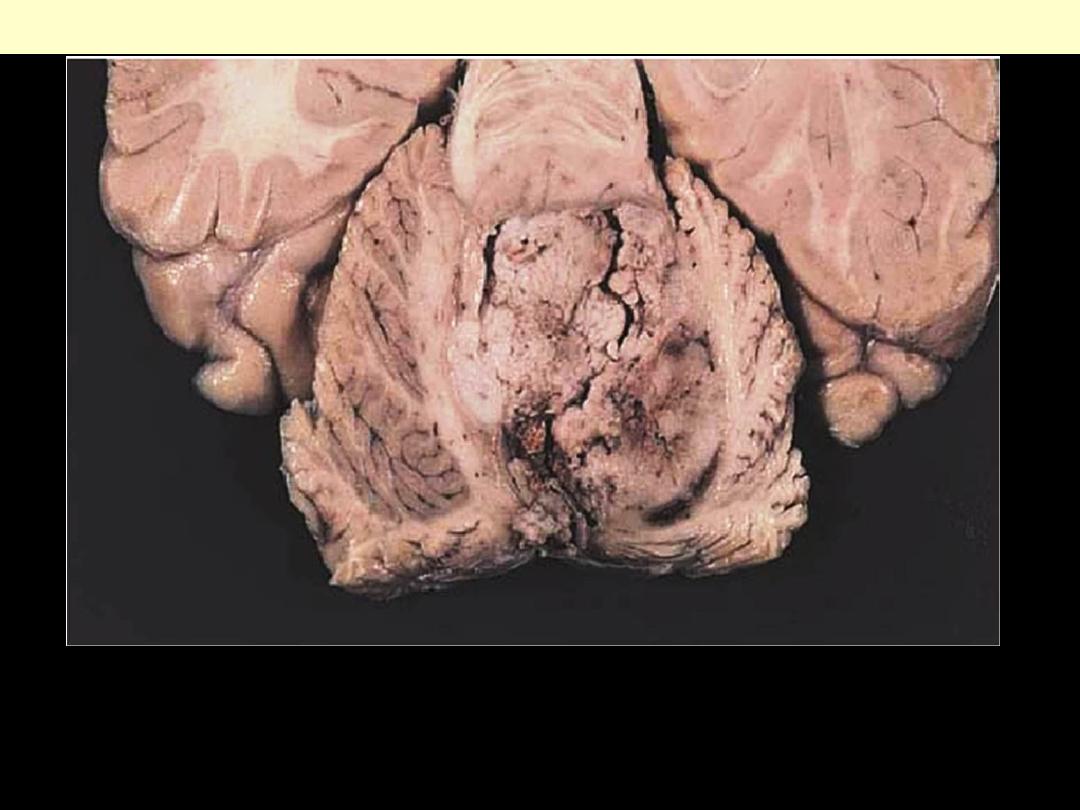
Cerebellar Medulloblastoma
The tumor arises in the cerebellar vermis and (as it commonly does)
come to fill the fourth ventricle. It is well circumscribed, gray, and
friable
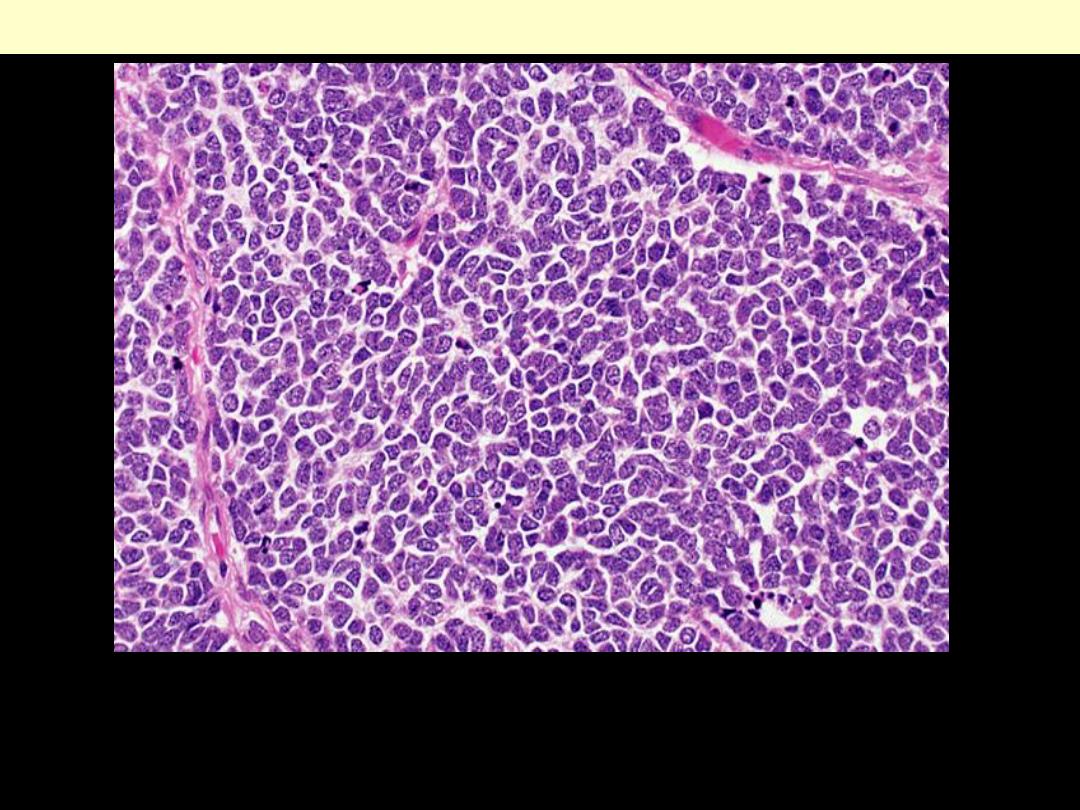
This is a highly cellular neoplasm composed of small,
undifferentiated-looking cells with little cytoplasm and
hyperchromatic nuclei.
Medulloblastoma
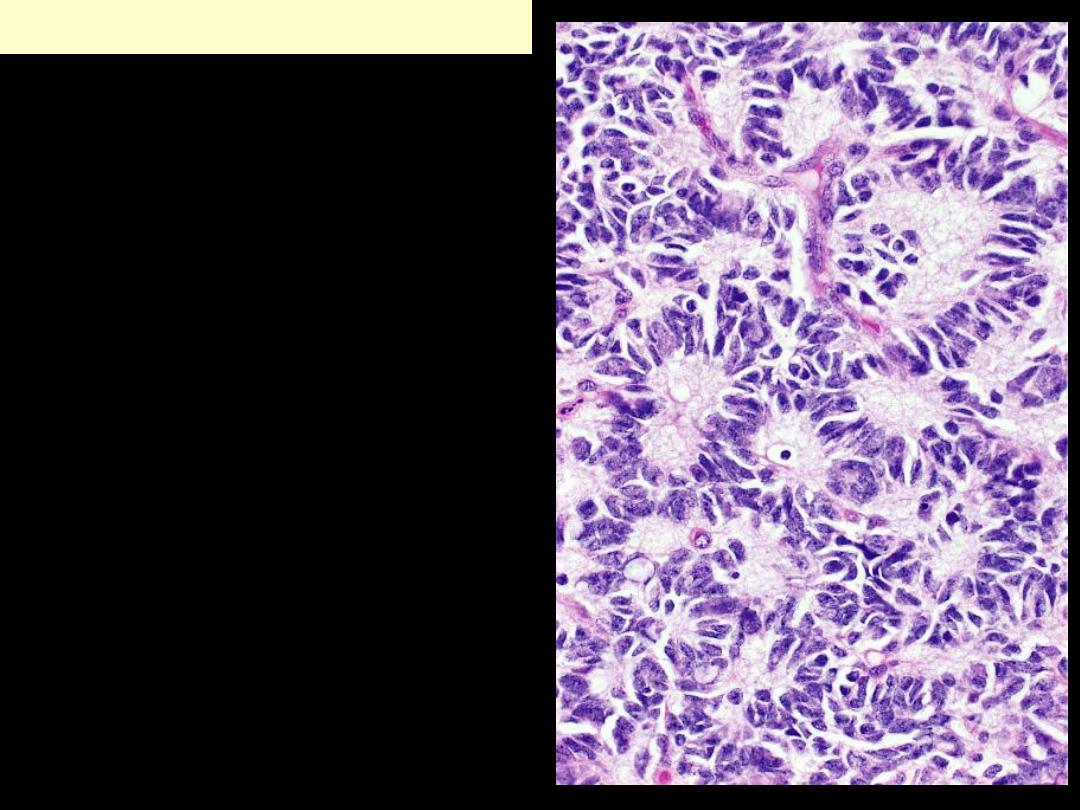
Homer Wright rosettes consist of
tumor cell nuclei disposed in
circular fashion about tangled
cytoplasmic processes. These
structures are indicative of
differentiation along neuronal
lines.
Medulloblastoma
Parasagittal multilobular meningioma attached to the dura with
compression of underlying brain.
Meningioma
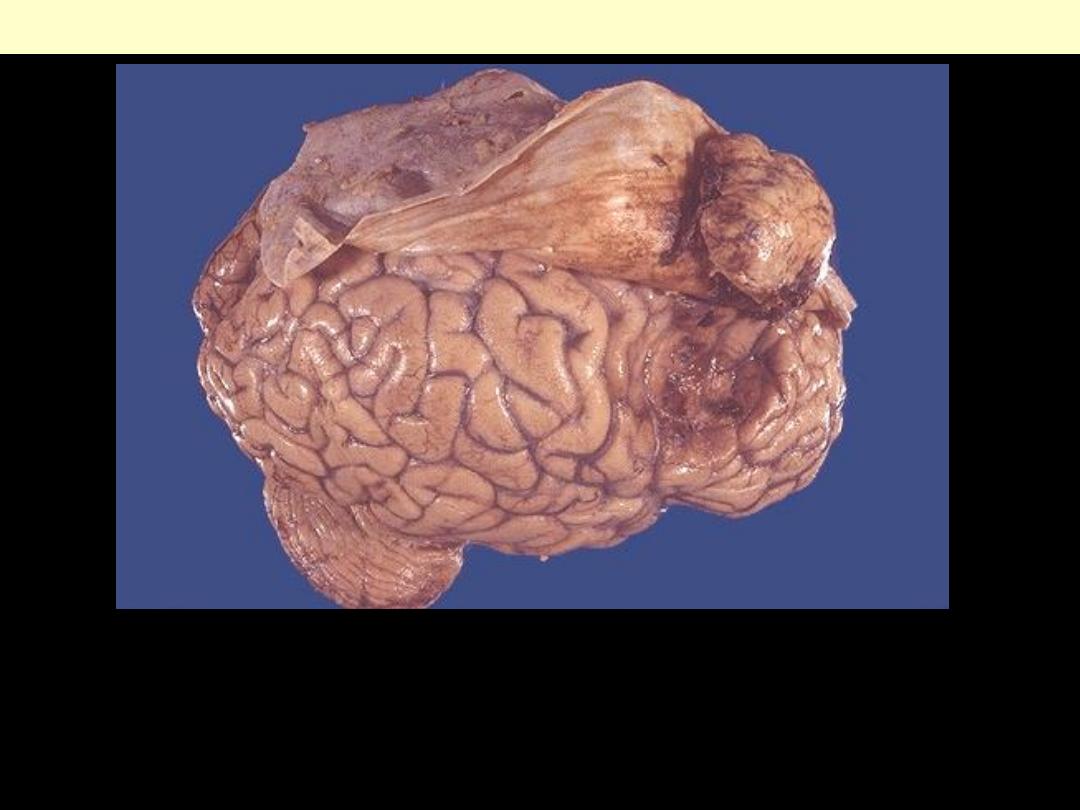
The tumor is roughly spherical, circumscribed reddish-yellow & firm. It is located
beneath the dura next to the falx cerebri. This superior parasagittal location, in
vicinity of superior sagittal sinus, is quite common. Note how this meningioma has
compressed the underlying cerebral hemisphere. Rarely, meningiomas can be
more aggressive and invade.
Meningioma
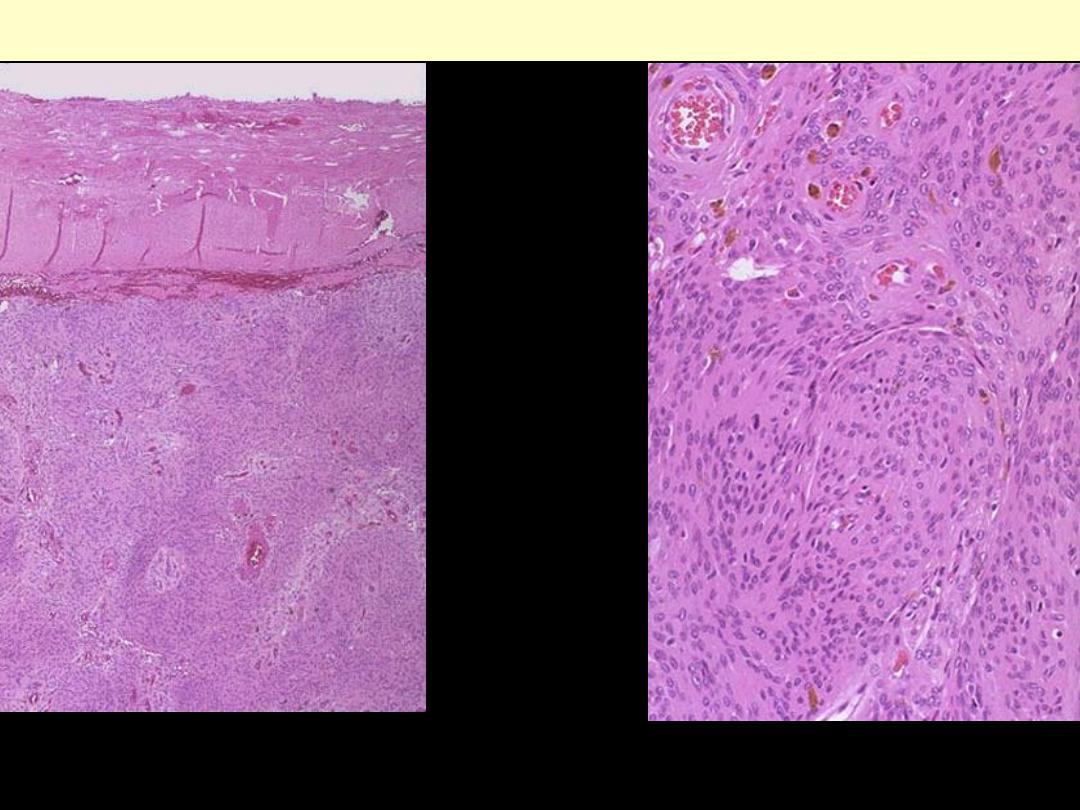
This is the microscopic appearance of a meningioma at low magnification. Note the dense pink
connective tissue dura at the top. The cells of the meningioma have abundant pink cytoplasm.
B. At medium power, there is characteristic whorled nests of cells.
Syncytial meningiomas
At high magnification, this meningioma has plump pink cells. A small amount of brown granular
hemosiderin is present.
Syncytial meningioma
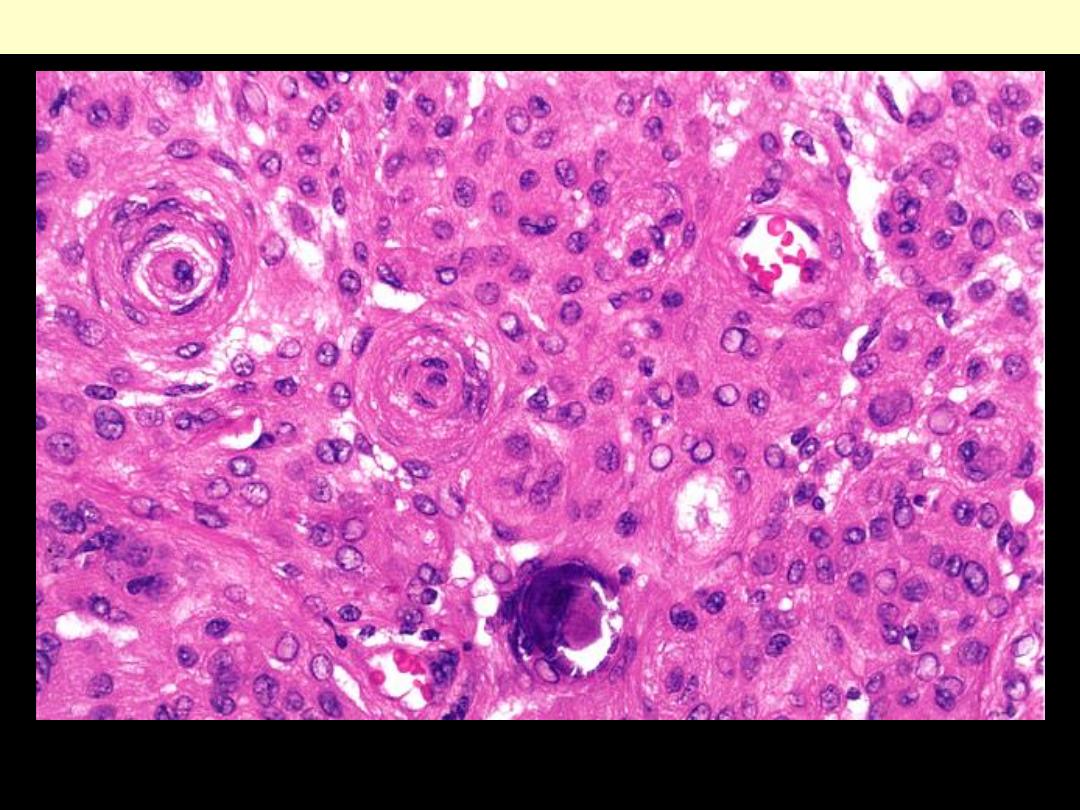
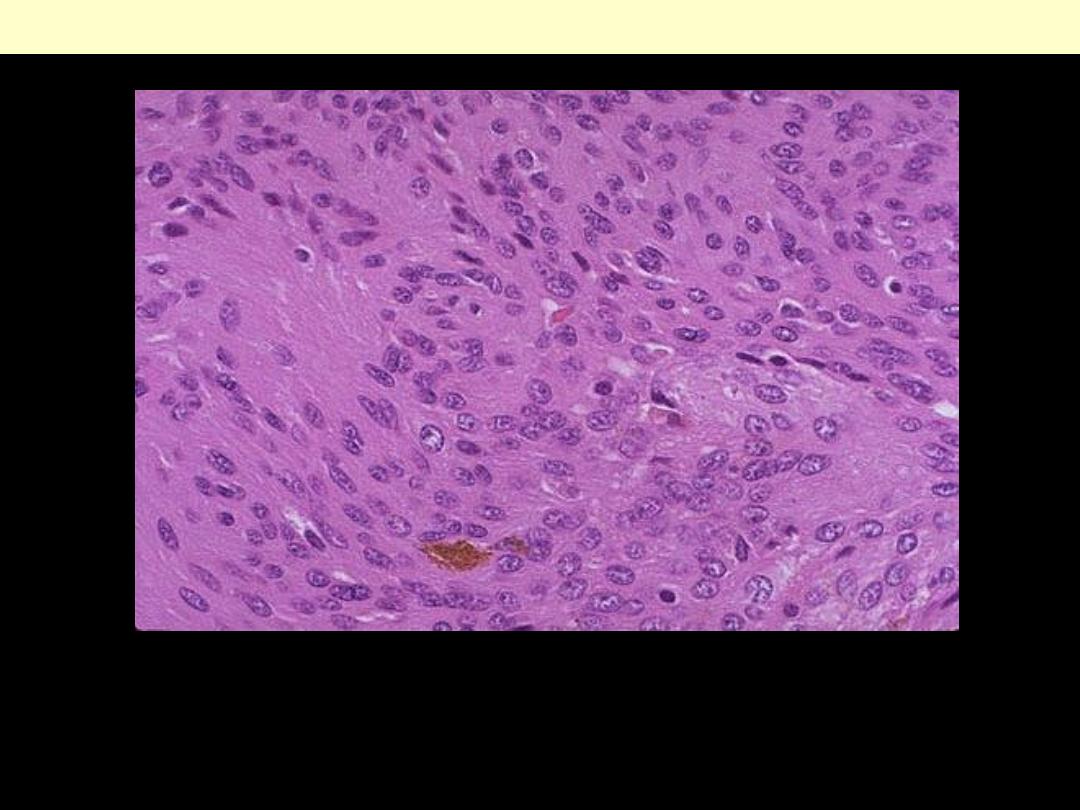
Meningioma. Indistinct cytoplasmic boundaries, nuclear clearing (“pseudoinclusions”), cellular whorls,
and a psammoma body are all apparent in this view of syncytial meningioma.
Syncytial meningioma with psammoma bodies
Meningioma. Cellular spindling and a fascicular or storiform architecture are evidenced by
meningiomas of “fibroblastic” type.
Fibroblastic meningioma

d
Psammomatous meningioma
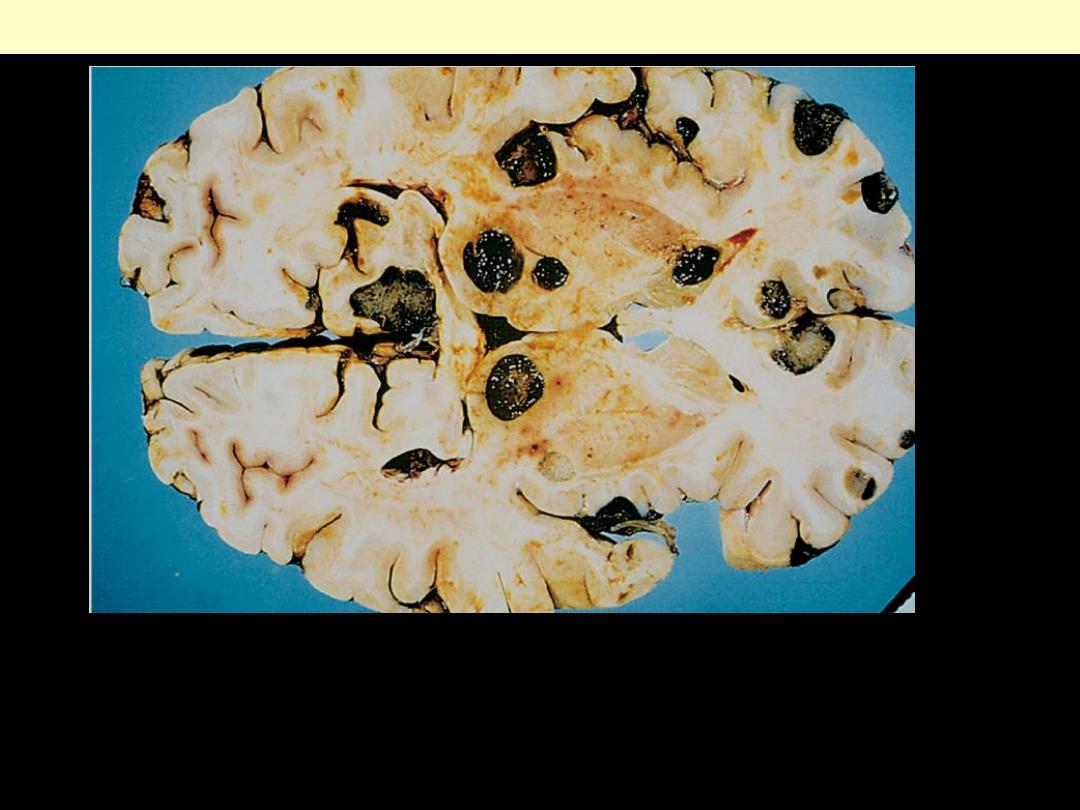
Metastatic lesions are distinguished grossly from most primary CNS
tumors by their multicentricity and well-demarcated margins. The
dark pigment in the tumor nodules in this case is characteristic of
most malignant melanomas.
Metastatic melanoma
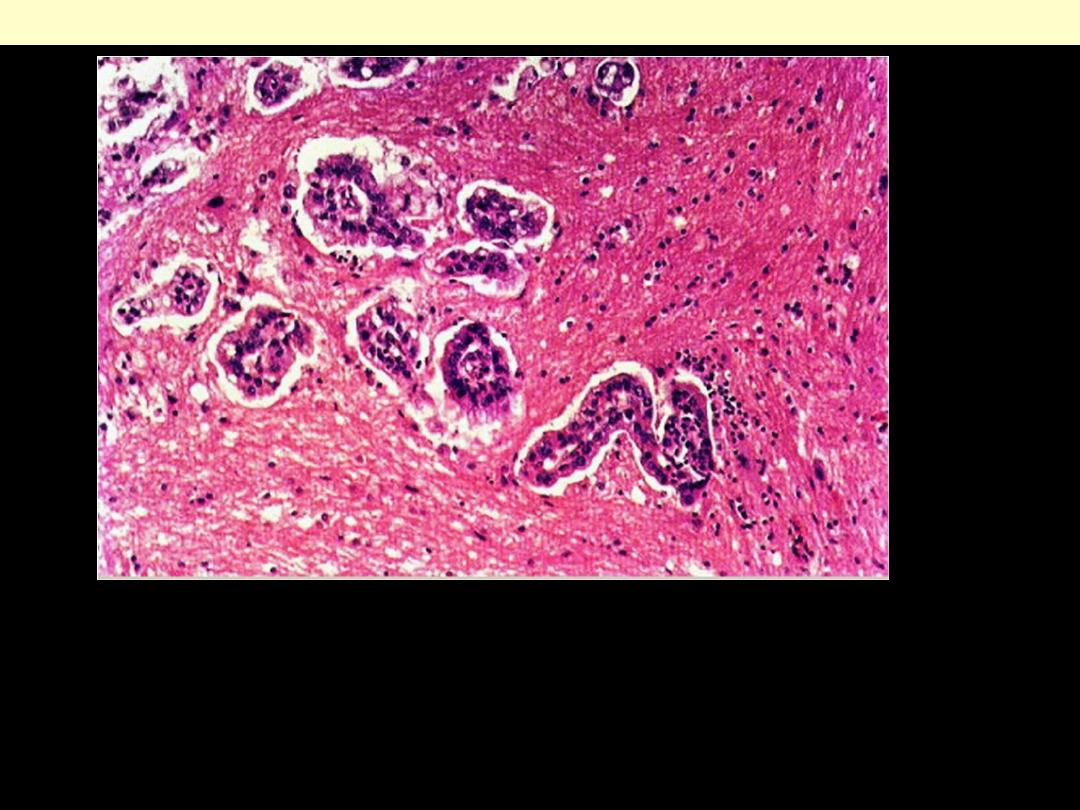
Metastatic breast carcinoma CNS
Tumor cells are invading the white matter. They form papillary structures,
with a central core of vascular connective tissue and an outer layer of
large cuboidal or columnar cells. Secondary tumors tend to have a
histological structure similar to that of the primary and the primary in this
case was a papillary adenocarcinoma of breast.
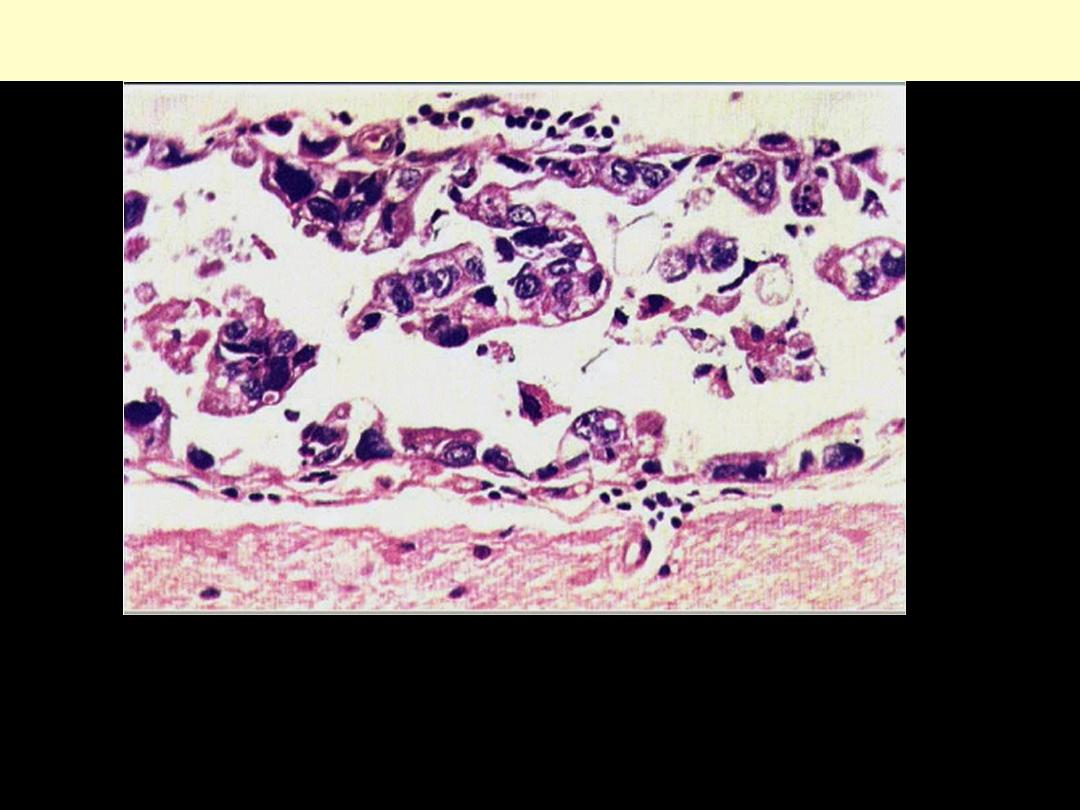
Metastatic bronchial ca brain
Sometimes the metastatic tumour is confined to the leptomeninges, the malignant
cells growing in the subarachnoid space. The cerebral cortex covered with the pia
mater is at the bottom, and the arachnoid membrane at the top. In the
subarachnoid space tumor cells are growing freely. They are very pleomorphic.
The primary was a carcinoma of bronchus.
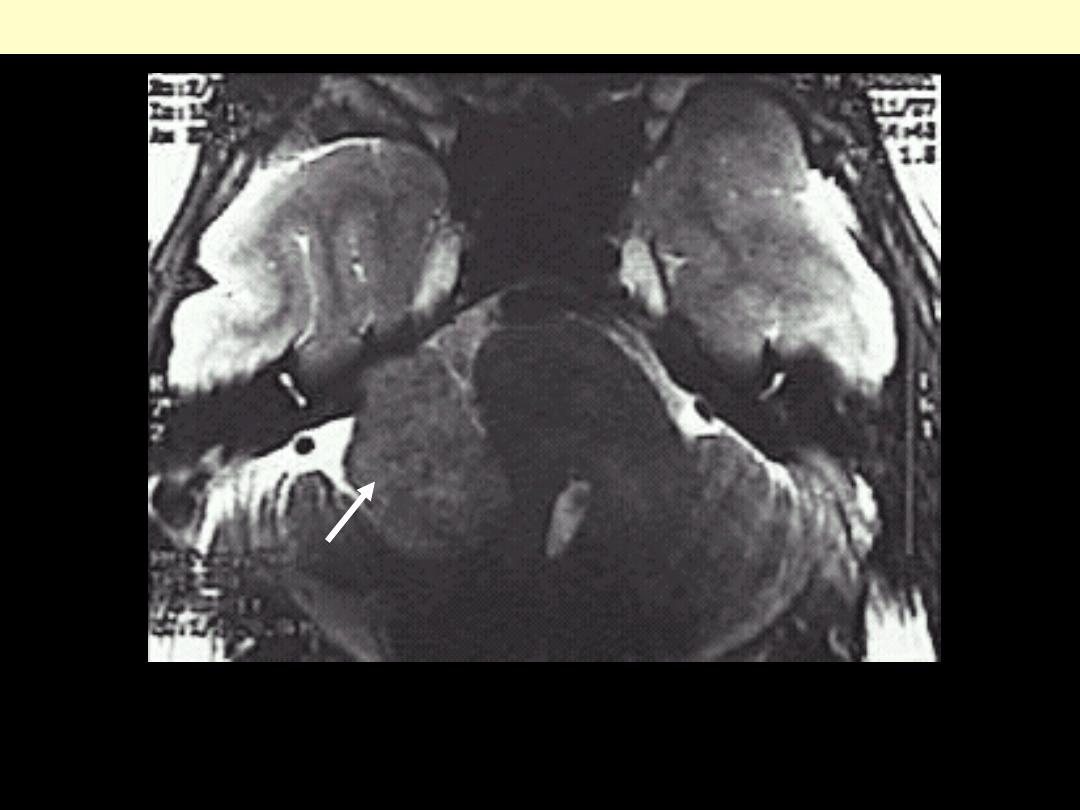
This magnetic resonance imaging (MRI) scan in transverse view demonstrates a mass impinging upon
the cerebellum from the cerebellopontine angle. This is a schwannoma, also known as an acoustic
neuroma because it arises from the eighth nerve.
Schwannoma
Schwannoma
The mass lesion here is arising in
the acoustic (eighth cranial)
nerve at the cerebellopontine
angle
.
Patients may present with
hearing loss.

The cut surface of a schwannoma is similar to that of many
mesenchymal neoplasms, with a "fish flesh" soft tan appearance.
Schwannoma
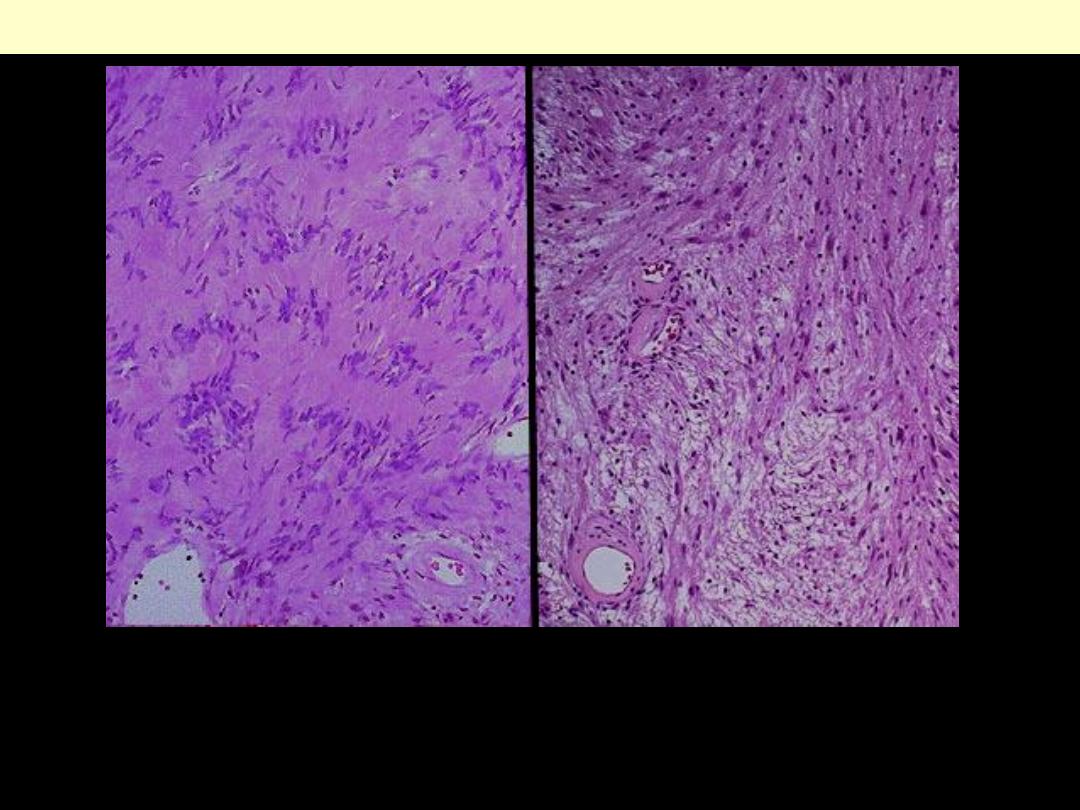
Schwannoma
Schwannoma: Note the more cellular pattern on the left with
palisading nuclei surrounding pink areas (Verocay bodies). On the
right has a looser stroma, fewer cells, and myxoid change.
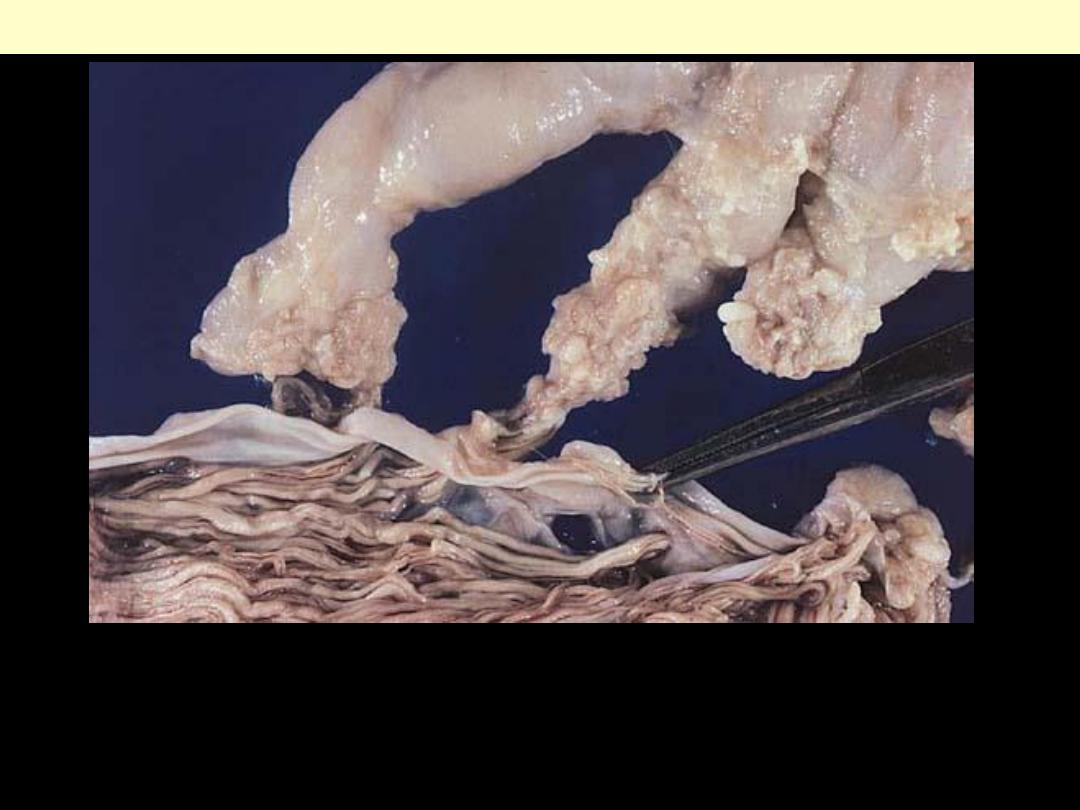
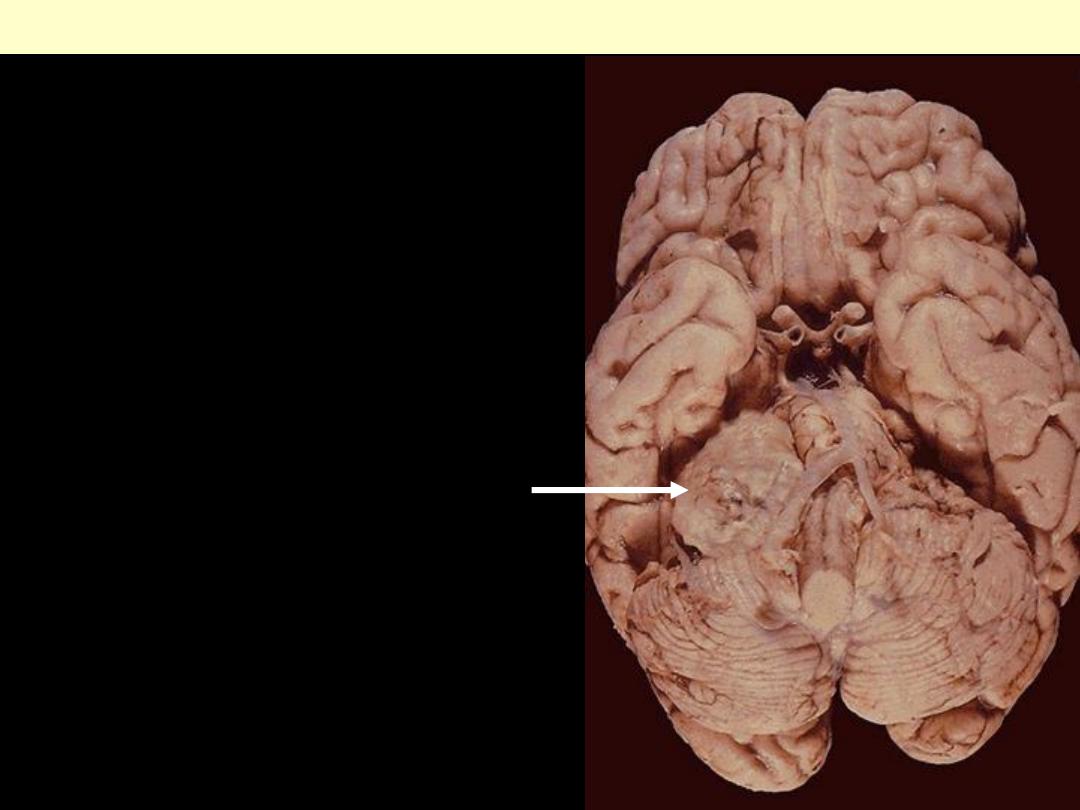
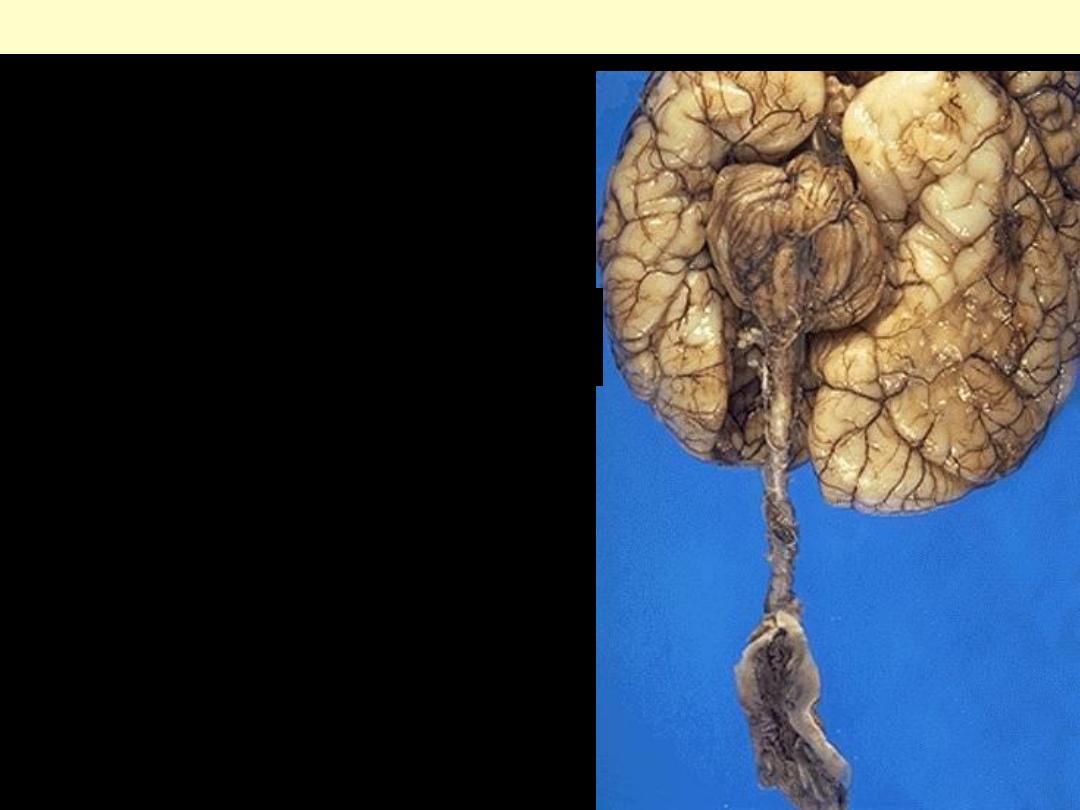
Neurofibromas of the spinal nerve roots are principally encountered in the
setting of type 1 neurofibromatosis (classic von Recklinghausen disease).
Multiple spinal roots of this afflicted patient exhibit plexiform
neurofibromatous expansion. Normal cauda equina are present at bottom.
Plexiform neurofibroma
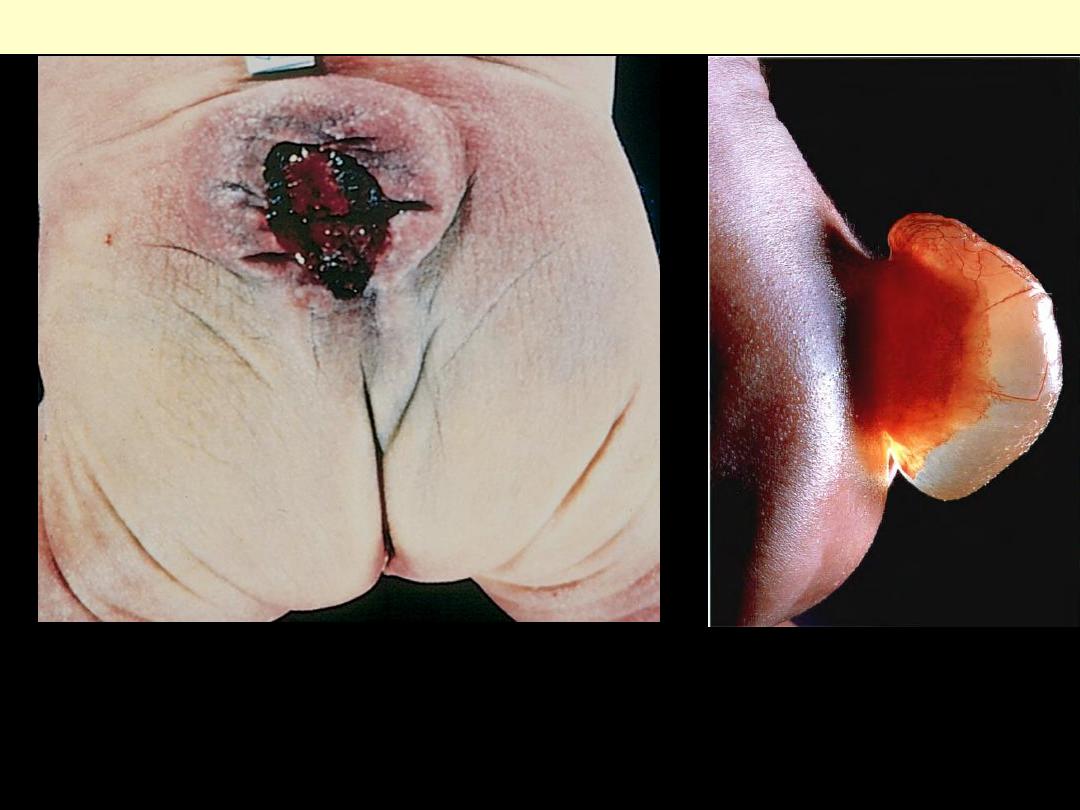
These defects occur because the caudal neural tube fails to close properly. In
meningomyelocele, both the meninges and spinal cord parenchyma are included in
the cystlike structure visible just above the buttocks. Because such lesions expose
the CNS to the outside environment, infection is a common complication.
Myelomeningocele
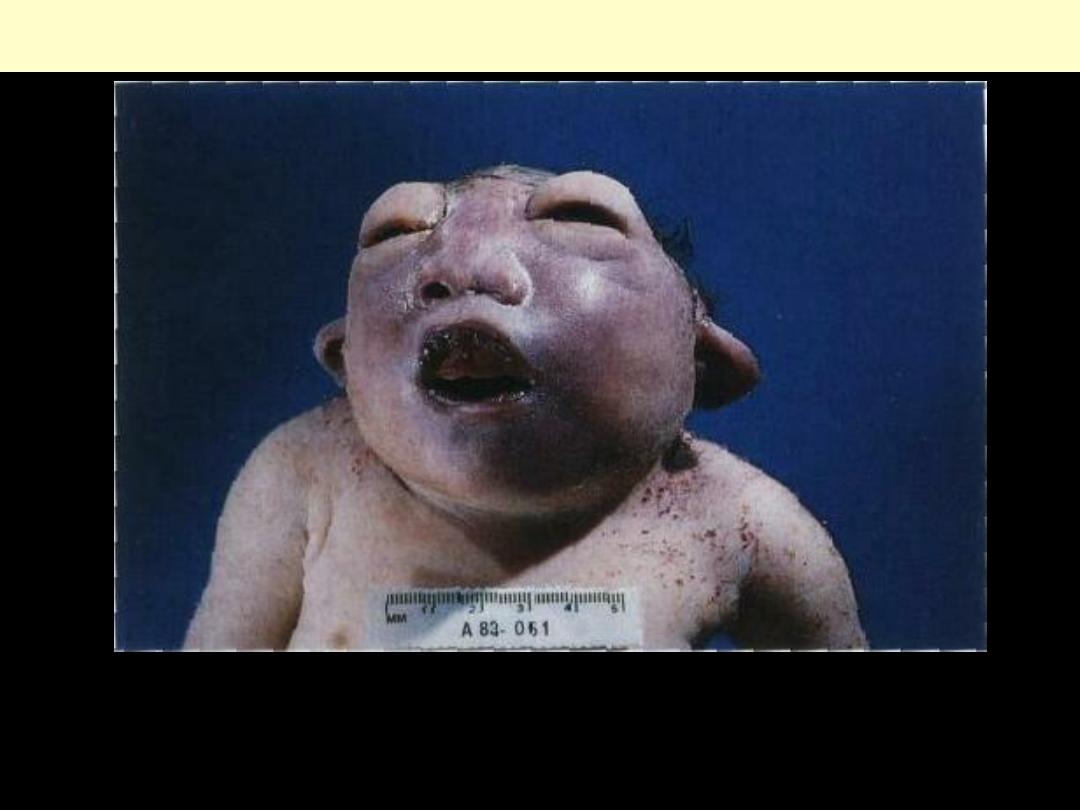
Anencephaly
This is the most common and most severe of cranial neural tube defects. The
orbital bones are of nearly normal size, despite absence of the brain and cranial
bones, resulting in a froglike facial appearance.
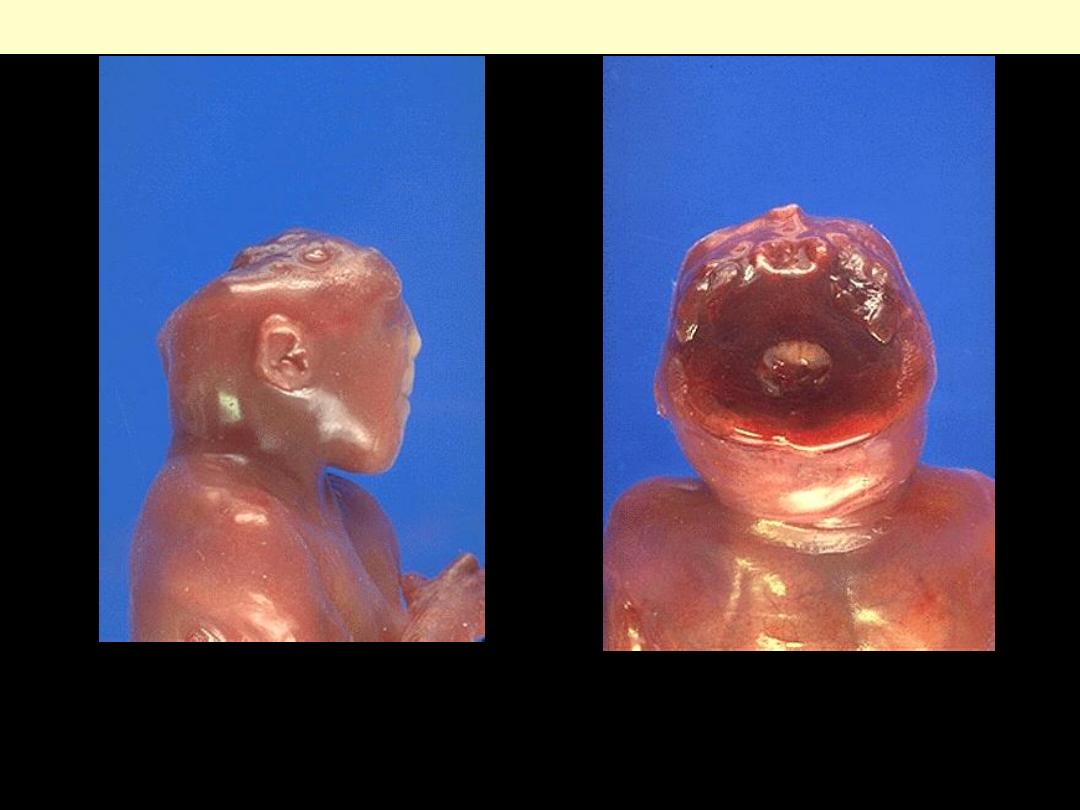
Anencephaly is absence of the fetal cranial vault. Exposure of
cerebral tissue to amniotic fluid precludes brain development. The
absence of the fetal cranial vault in anencephaly is shown here.
Anencephaly
Encephalocele
A well-developed cortical mantle characterizes this neurosurgical
specimen from the occipital region of a newborn.
Arnold chiari malformation
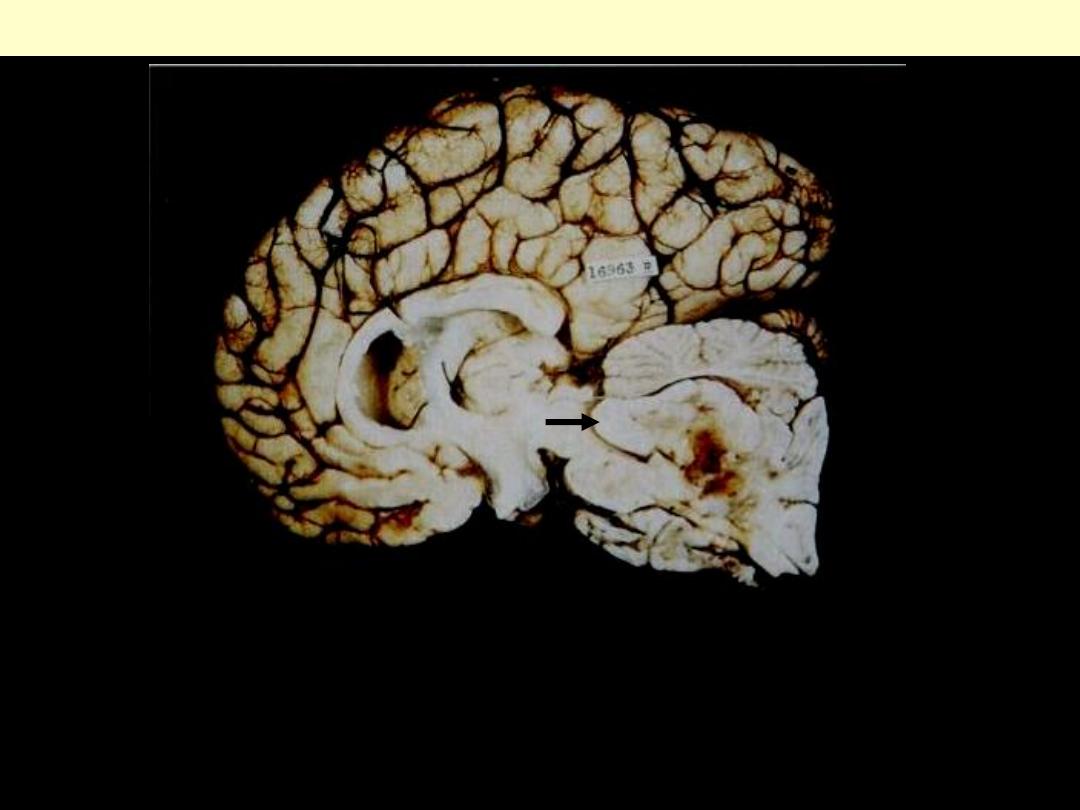
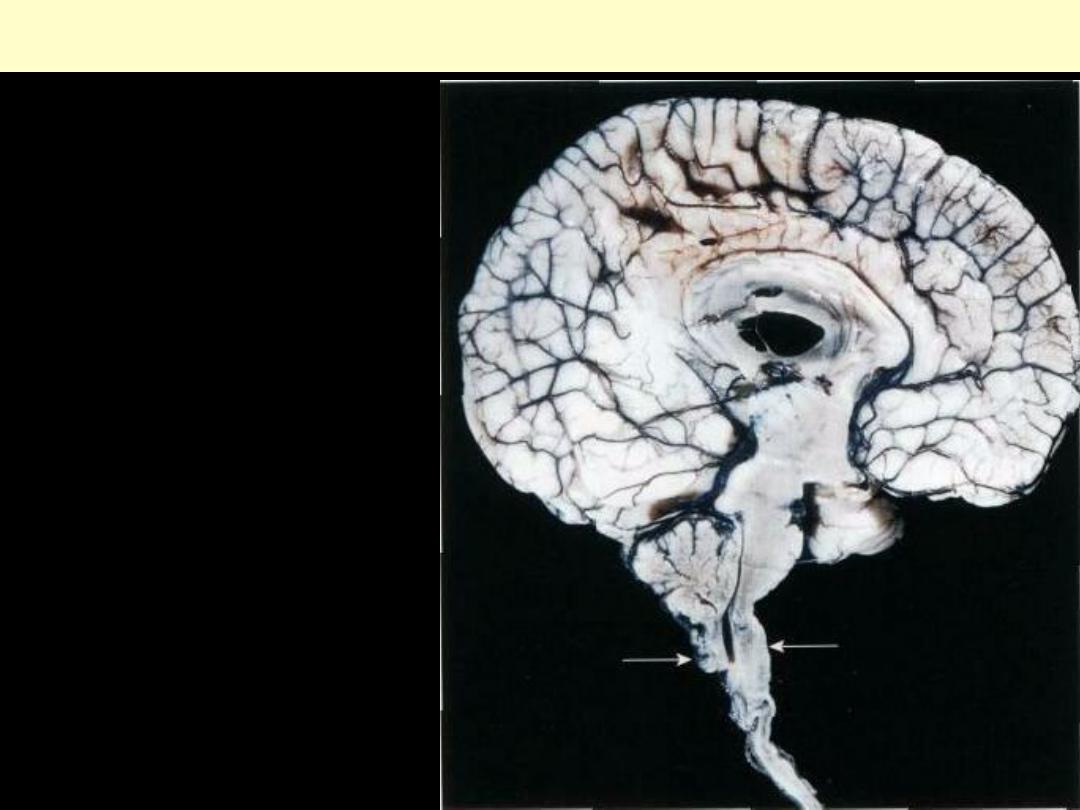
Midsagittal section showing small
posterior fossa contents, downward
displacement of the cerebellar vermis,
and deformity of the medulla
(arrowsindicate the approximate level of
the foramen magnum).
An Arnold-Chiari malformation occurs when there is
elongation and flattening of the cerebellum and medulla
with protrusion down a large conical foramen magnum.
Arnold-Chiari malformation
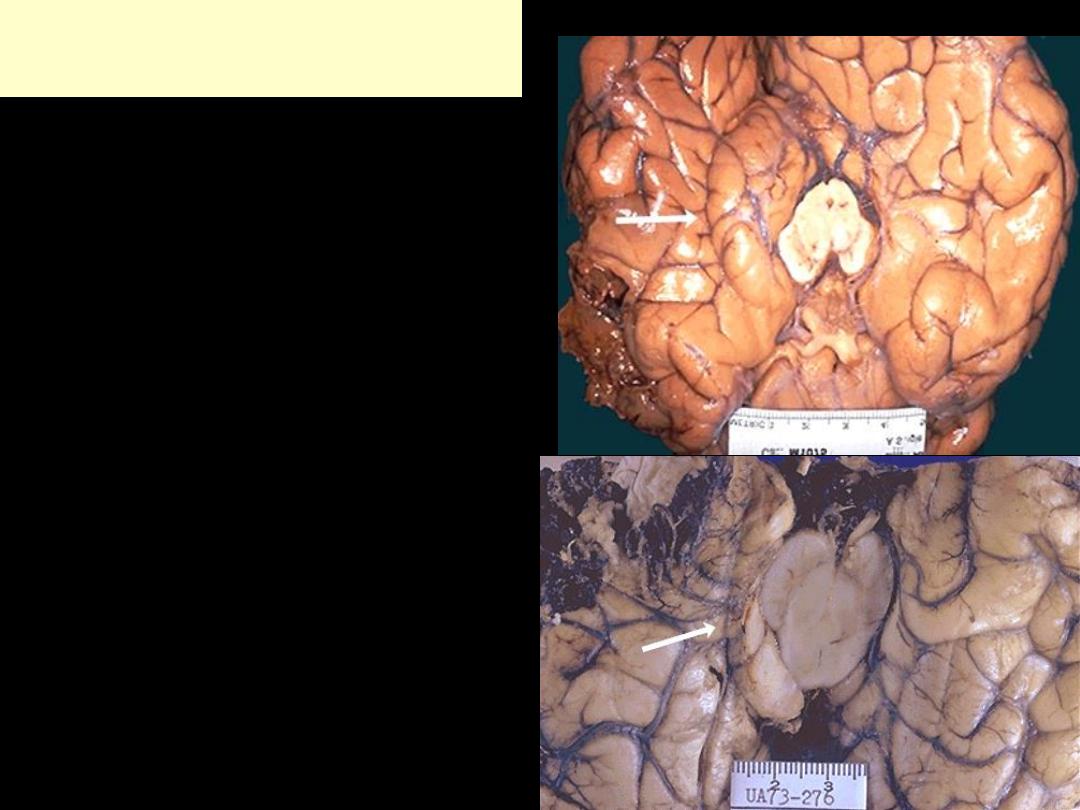
A: Acute contusions are present
in both temporal lobes, with
areas of hemorrhage and tissue
disruption.
B: Remote contusions are
present on the inferior frontal
surface of this brain, with a
yellow color.
Cerebral trauma
A
B
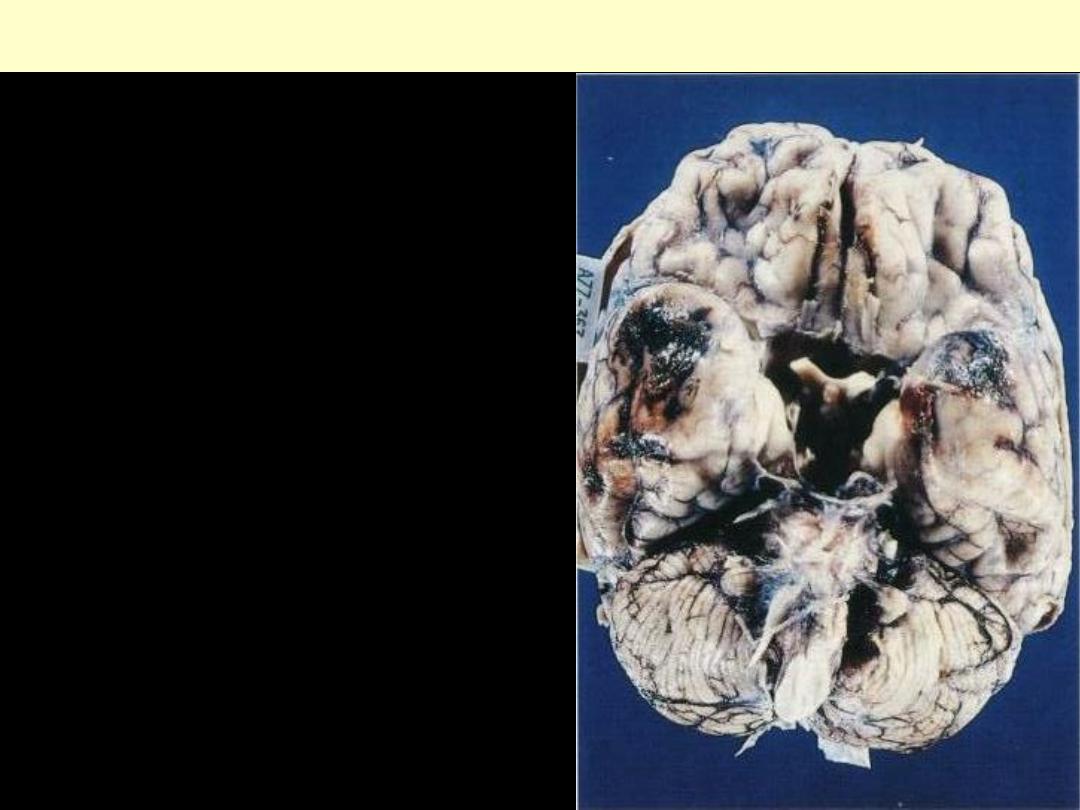
Cerebral contusions
The temporal poles are discolored by areas of
hemorrhage. Such lesions represent "bruises" of the
surface of the brain caused by violent contact
between the delicate brain parenchyma and the hard
inner surface of the skull.
A thick layer of yellow
purulent suppurative
exudate covers the brain
stem and cerebellum, and
thickens the leptomeninges
Pyogenic meningitis
The yellow-tan clouding of the meninges seen here is due to an exudate from acute bacterial
meningitis; it obscures the sulci.
Acute bacterial meningitis
Clouding of the meninges seen here is due to an yellow purulent
exudate from acute bacterial meningitis; it obscures the sulci. The
cerebrospinal fluid (CSF) in such cases typically has a low glucose,
high protein, and many PMN's. A gram stain should be done to
identify organisms.
Acute bacterial meningitis
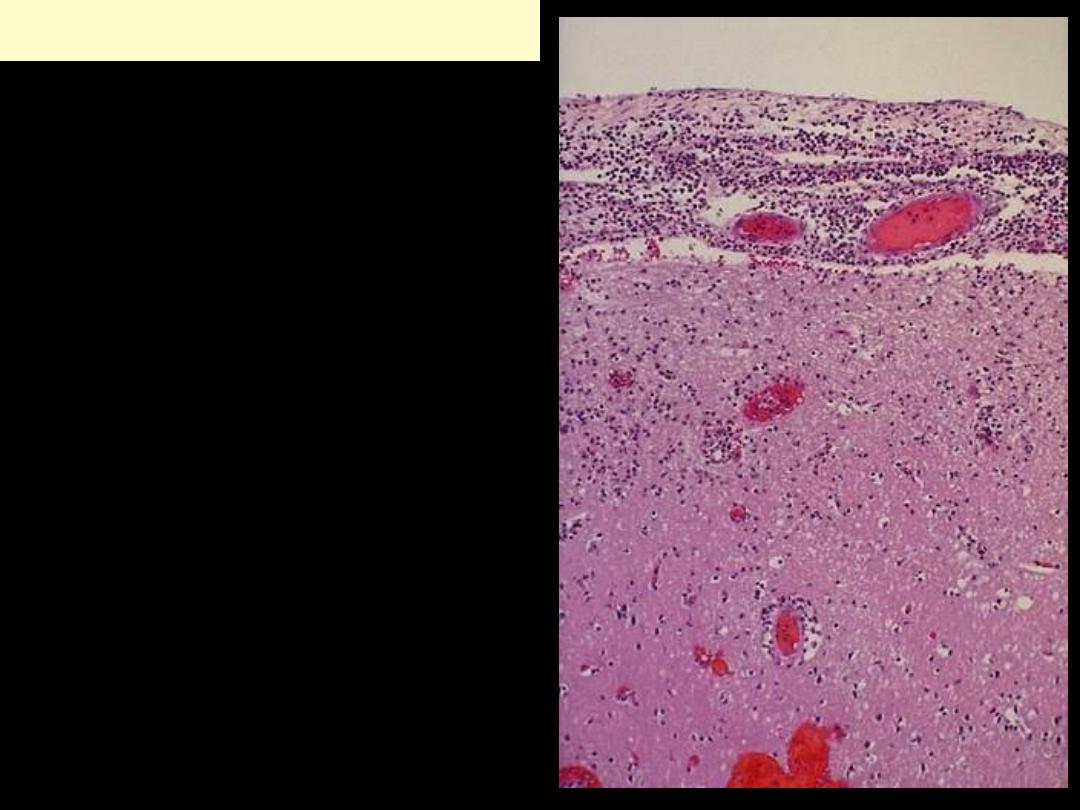
A neutrophilic exudate is seen
involving the meninges above,
with prominent dilated vessels.
There is edema and focal
inflammation (extending down
via the Virchow-Robin space) in
the cortex below. This acute
meningitis is typical for
bacterial infection
.
The edema
can lead to herniation and
death. Resolution of infection
may be followed by adhesive
arachnoiditis with obliteration
of subarachnoid space leading
to obstructive hydrocephalus.
Acute bacterial meningitis
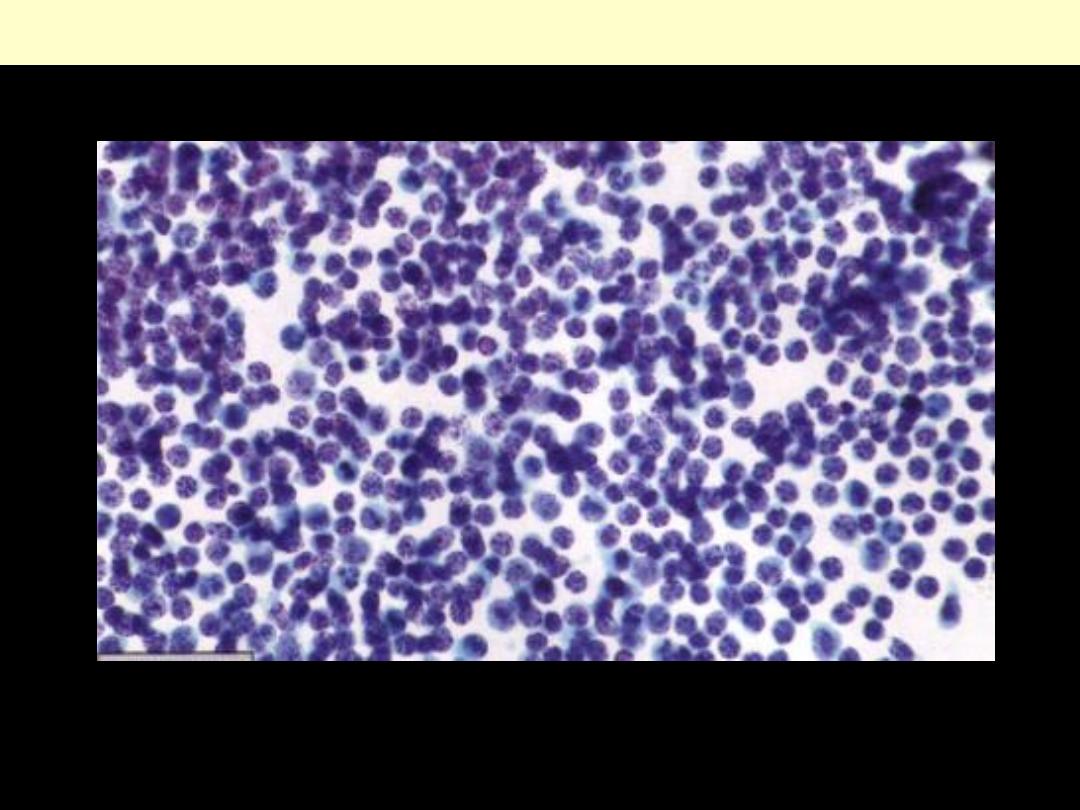
Viral Meningitis CSF
Polymorphic population of lymphocytes
Abscesses in the frontal white matter (arrows): discrete lesions with
central liquefactive necrosis and a surrounding zone of hyperemia
Brain abscess
There is a liquefactive center with yellow pus surrounded by a thin wall
*
.
Cerebral abscess
Brain abscess
Brain abscess that is sharply demarcated, indicating that it has been
present for some time. Purulent exudate is visible in the center of the
abscess.
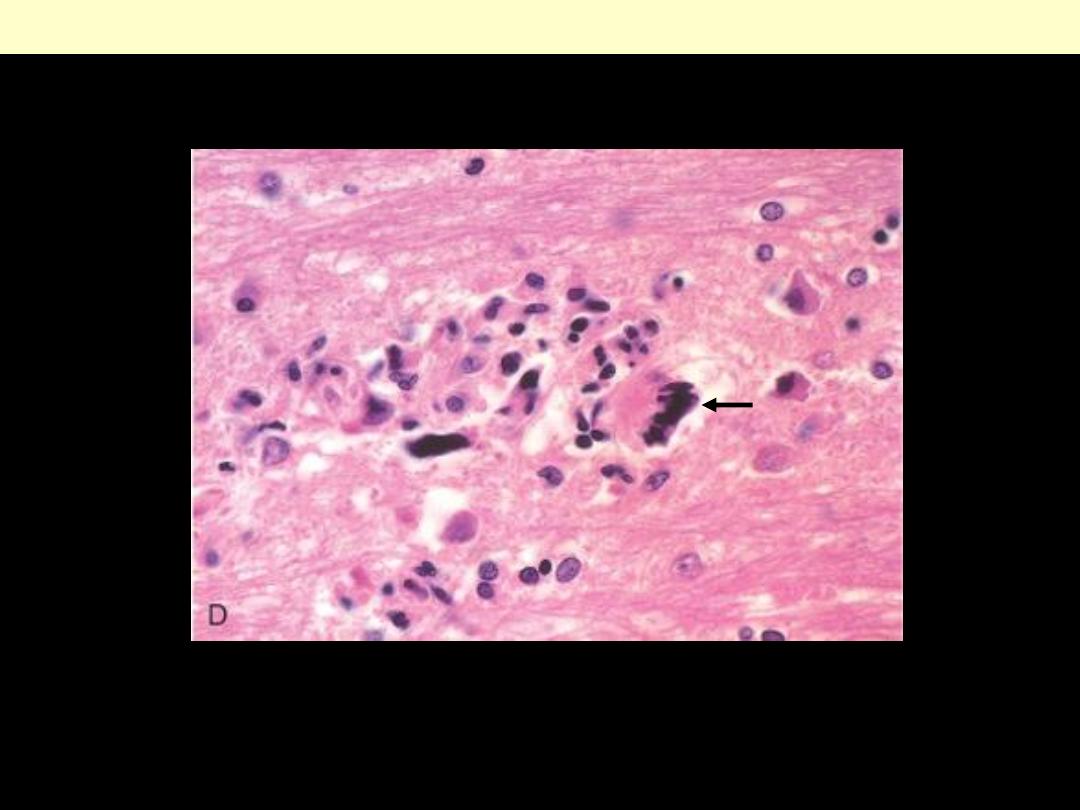
The lesion's purulent contents (Rt.) are separated from neighboring
white matter by a granulation tissue-like zone of angioblastic and
fibroblastic activity.
Brain abscess
There is marked necrosis of the right temporal lobe, and petechial
haemorrhages and early necrosis in the left temporal lobe. This
distribution is characteristic of herpes simplex encephalitis.
Herpes encephalitis
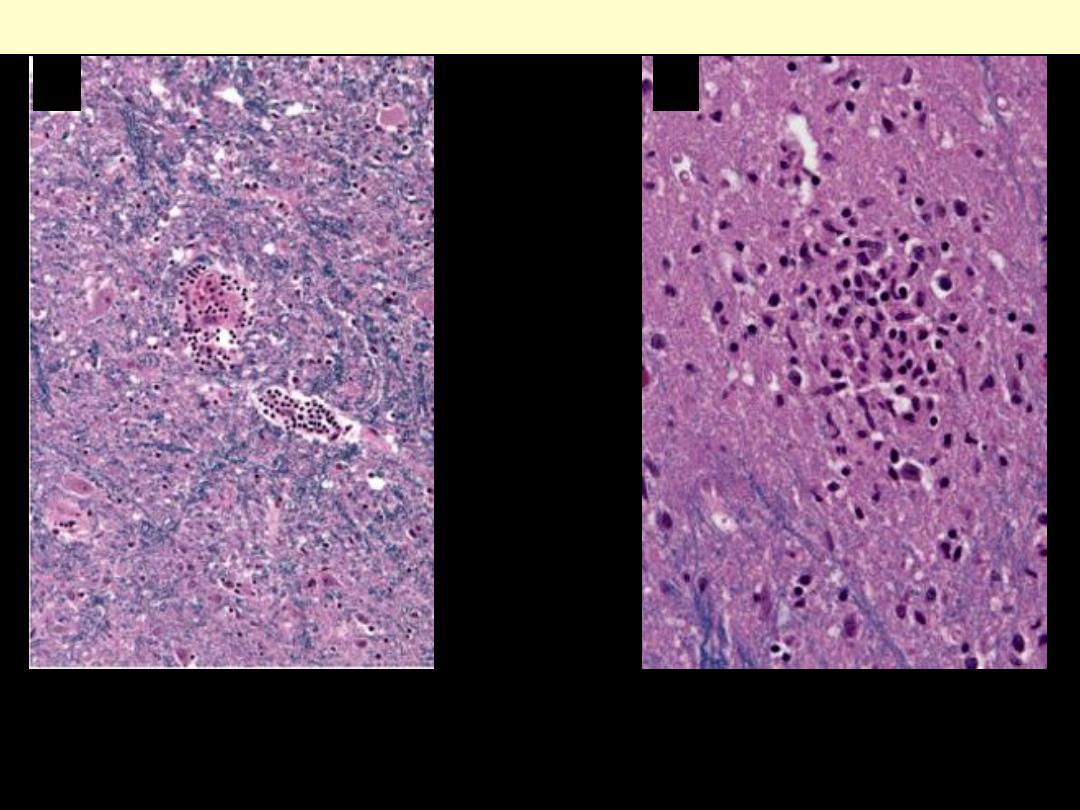
Characteristic findings of viral meningitis include perivascular cuffs
of lymphocytes (A) and microglial nodules (B).
Viral infections
A
B
Note the microglial nodule and multinucleated giant cell (arrow).
HIV encephalitis
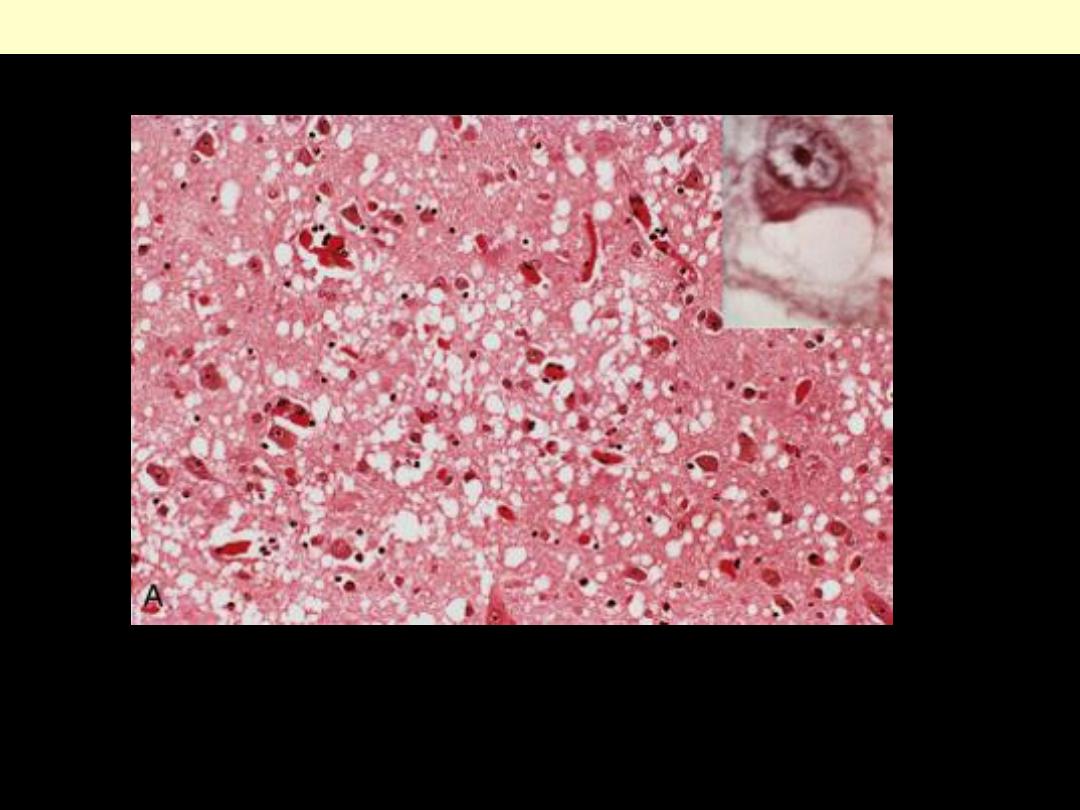
In this prion disease there is spongiform change in the cerebral cortex. Inset, High magnification of
neuron with vacuoles
Creutzfeldt-Jakob disease (CJD)
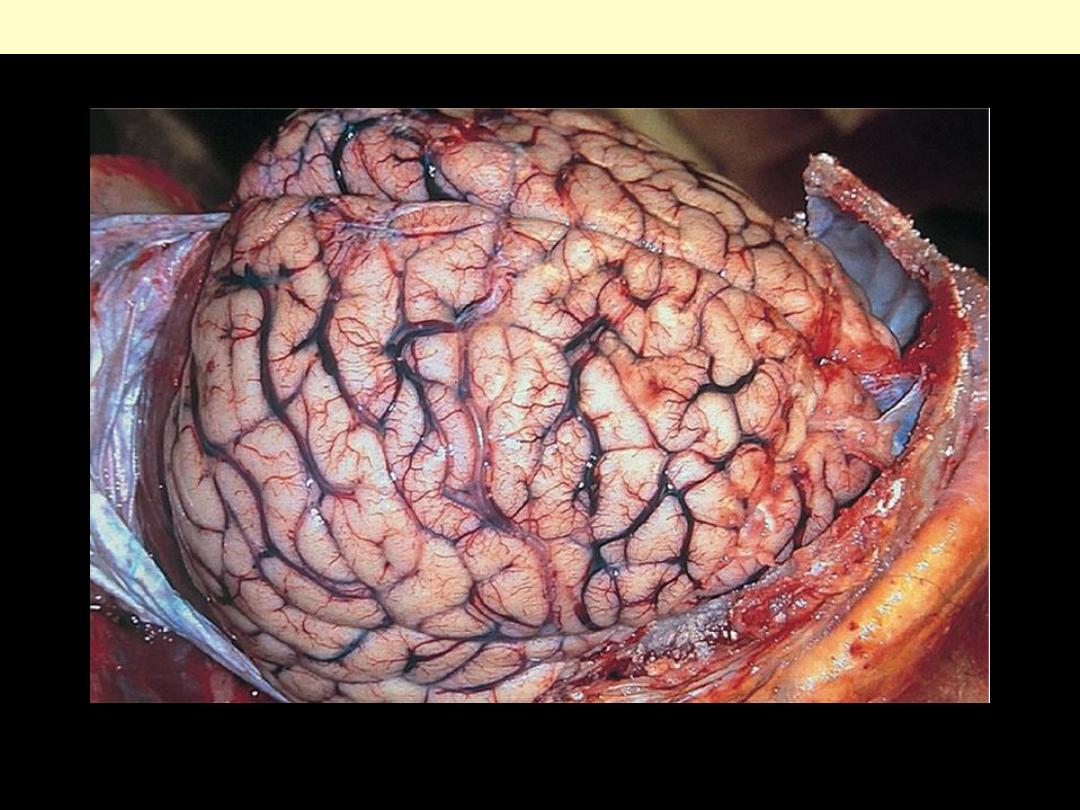
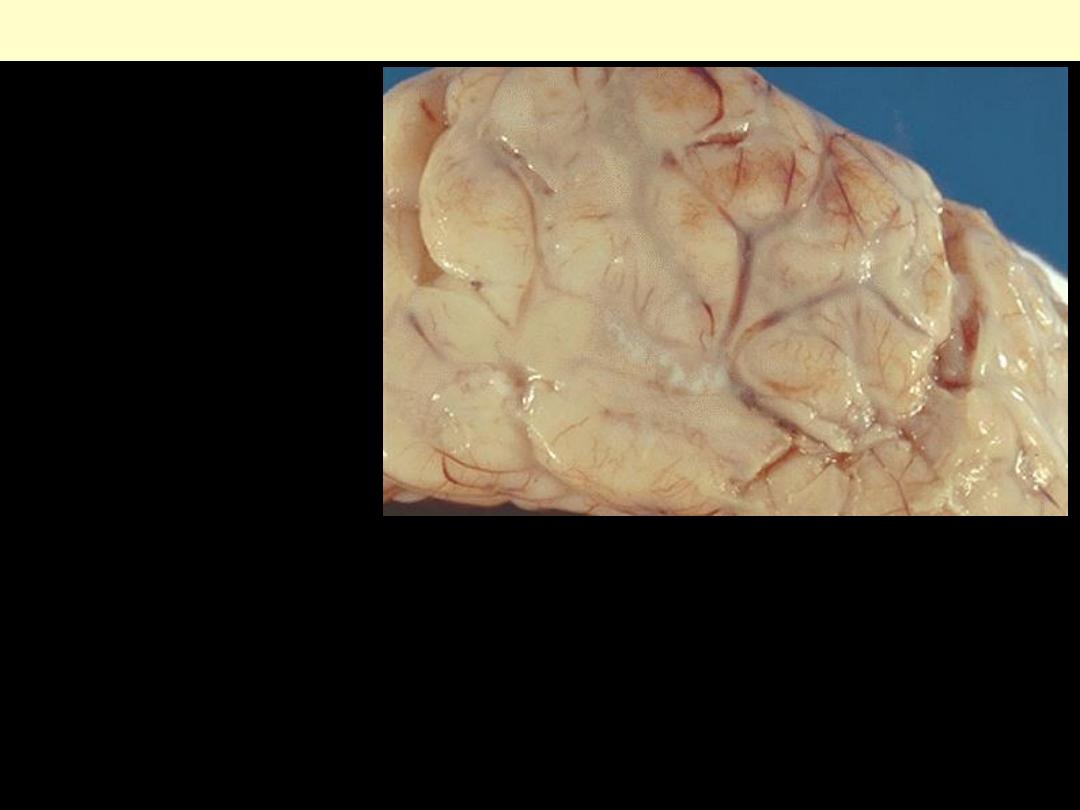
The surfaces of the gyri are flattened as a result of compression of the expanding brain by the dura
mater and inner surface of the skull. The sulci are very narrow. Such changes are associated with a
dangerous increase in intracranial pressure.
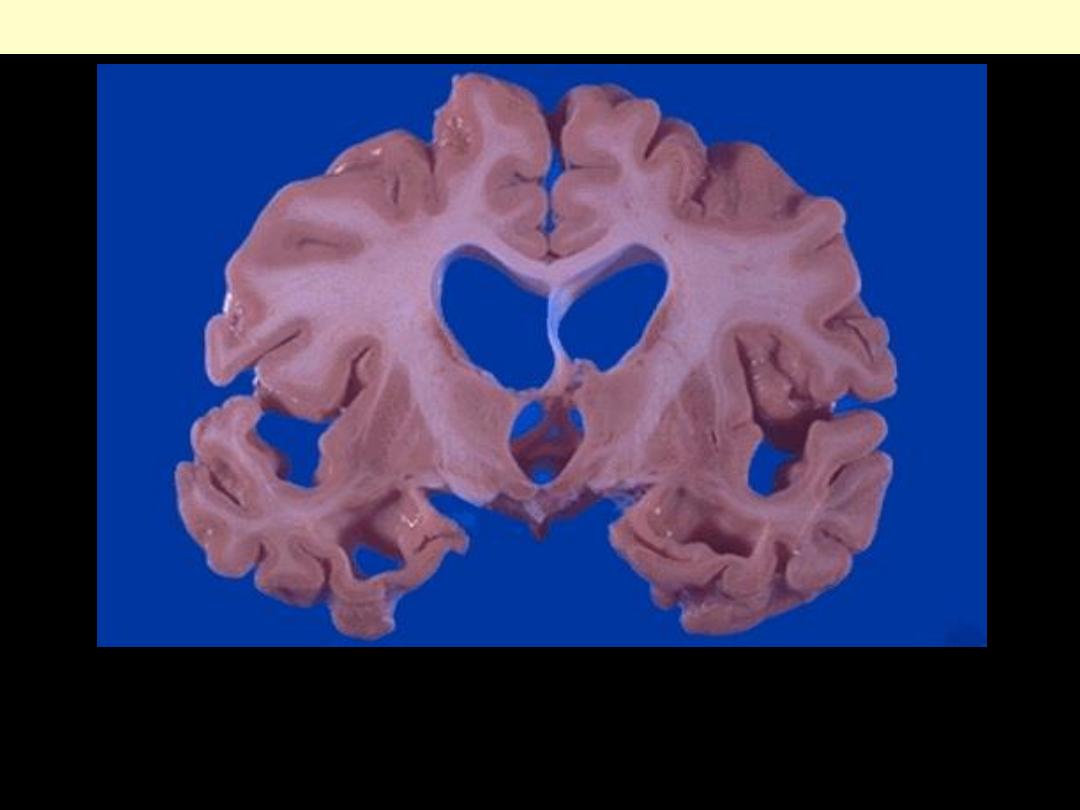
Cerebral edema
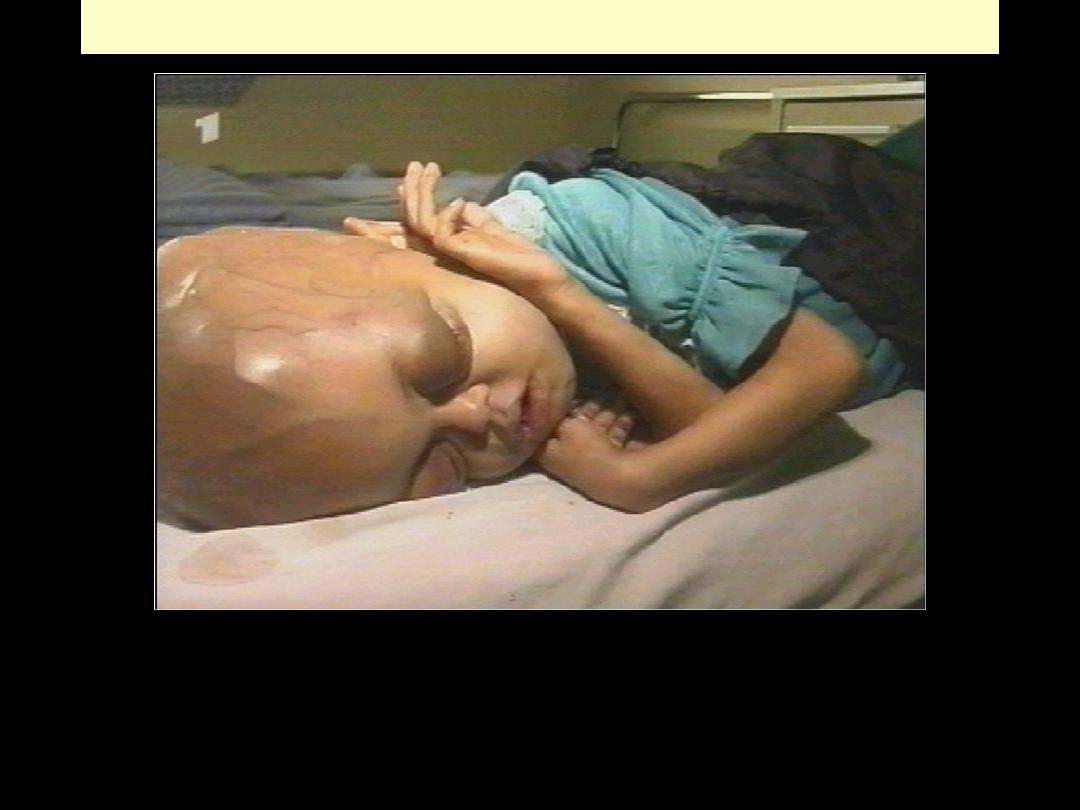
Hydrocephalus
When hydrocephalus develops in infancy before closure of the cranial sutures, there is enlargement of
the head
Hydrocephalus
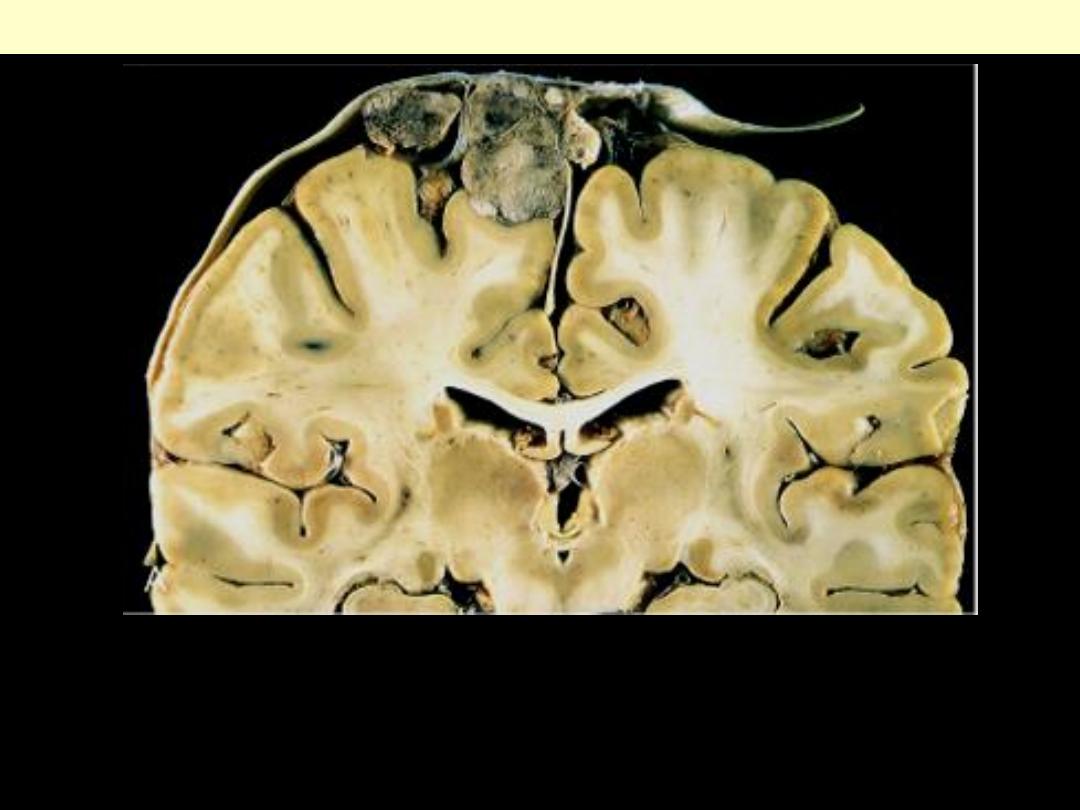
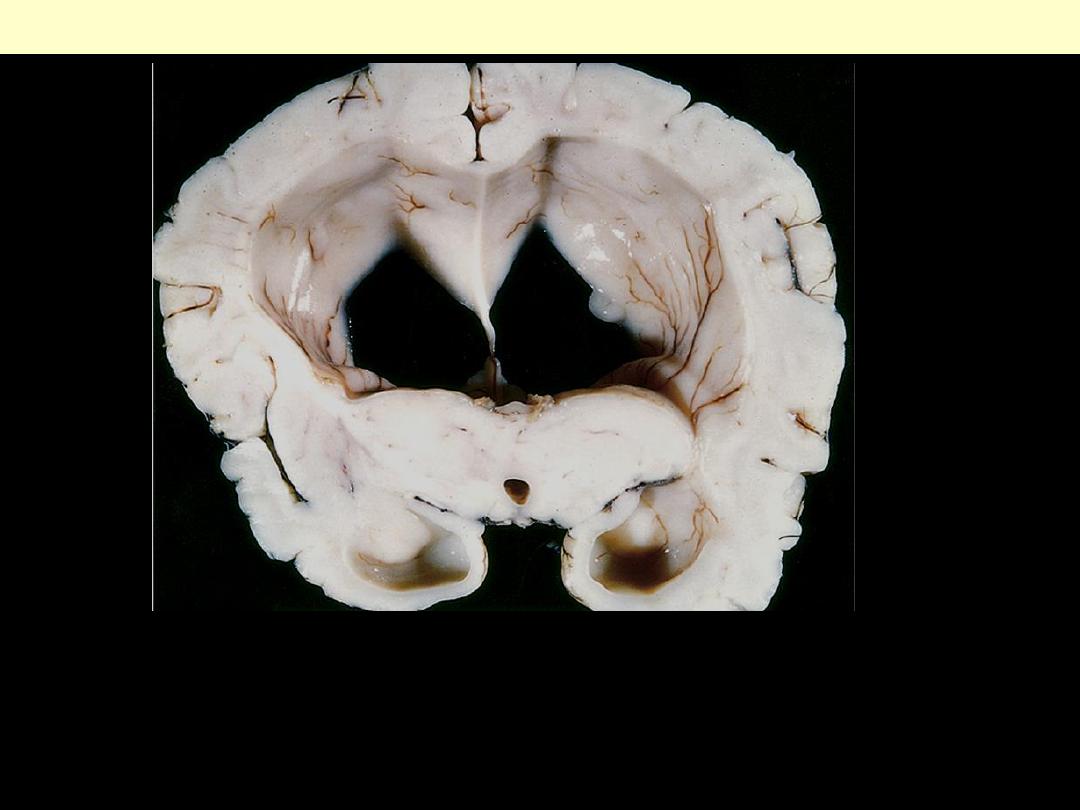
Obstruction of the flow of cerebrospinal fluid has caused the
ventricles to expand, with a resultant increase in intracranial
pressure. Dilated lateral ventricles seen in a coronal section through
the mid-thalamus.
Hydrocephalus
Hydrocephalus. Obstruction of the flow of cerebrospinal fluid has caused the ventricles to expand, with
a resultant increase in intracranial pressure. Obstructive hydrocephalus must be distinguished from
hydrocephalus ex-vacuo, in which the ventricles expand to compensate for a loss of brain parenchyma.
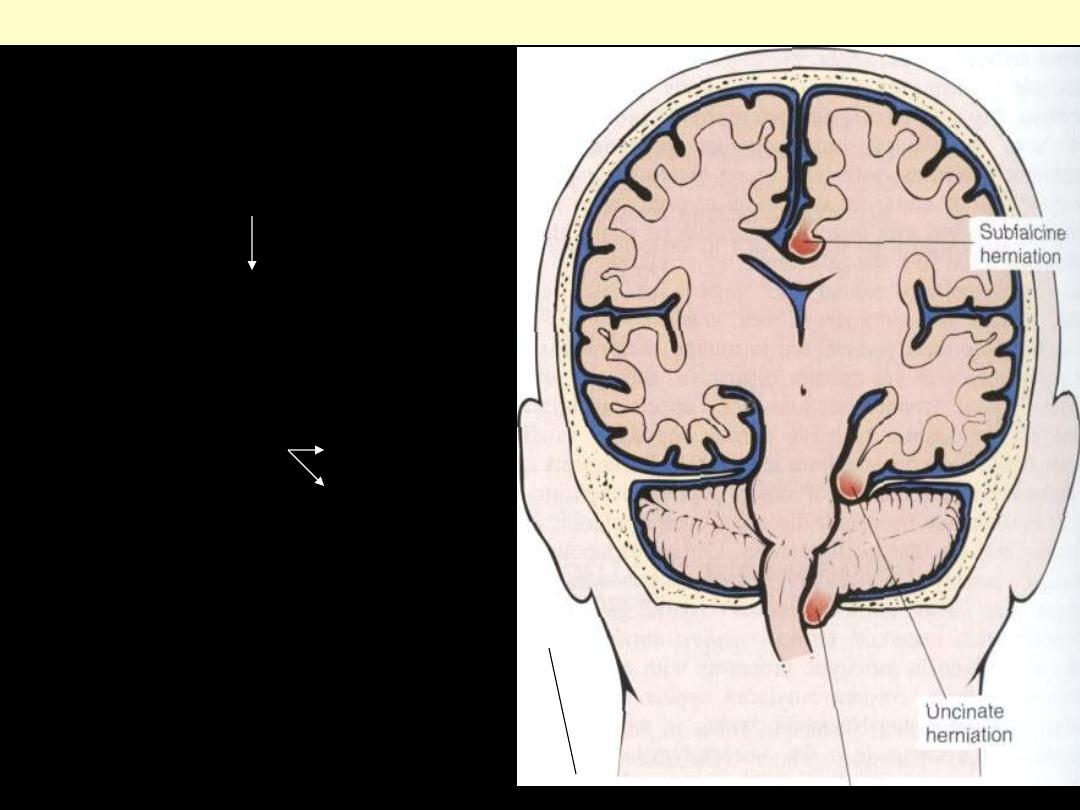
Patterns of brain herniation
Tonsillar herniation
Uncal gyral herniation
III C nerve
post C artery
Cingulate gyrus herniation
AC artery
Cerebel tonsil through F. magnum: fatal
Brain stem herniation fatal (Duret
Hge)
Another example of uncal
herniation.
Swelling of the left cerebral
hemisphere has produced a shift
with herniation of the uncus of
the hippocampus through the
tentorium, leading to the groove
seen at the white arrow.
Cerebrum, uncal herniation
complicating brain edema
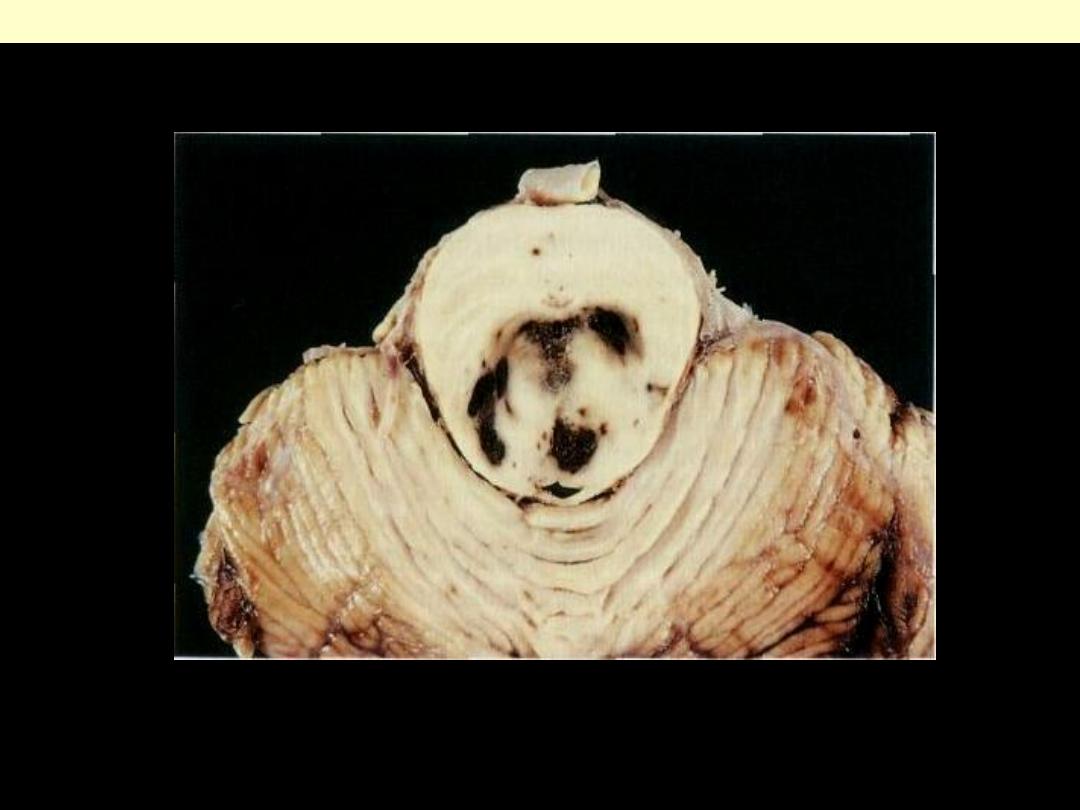
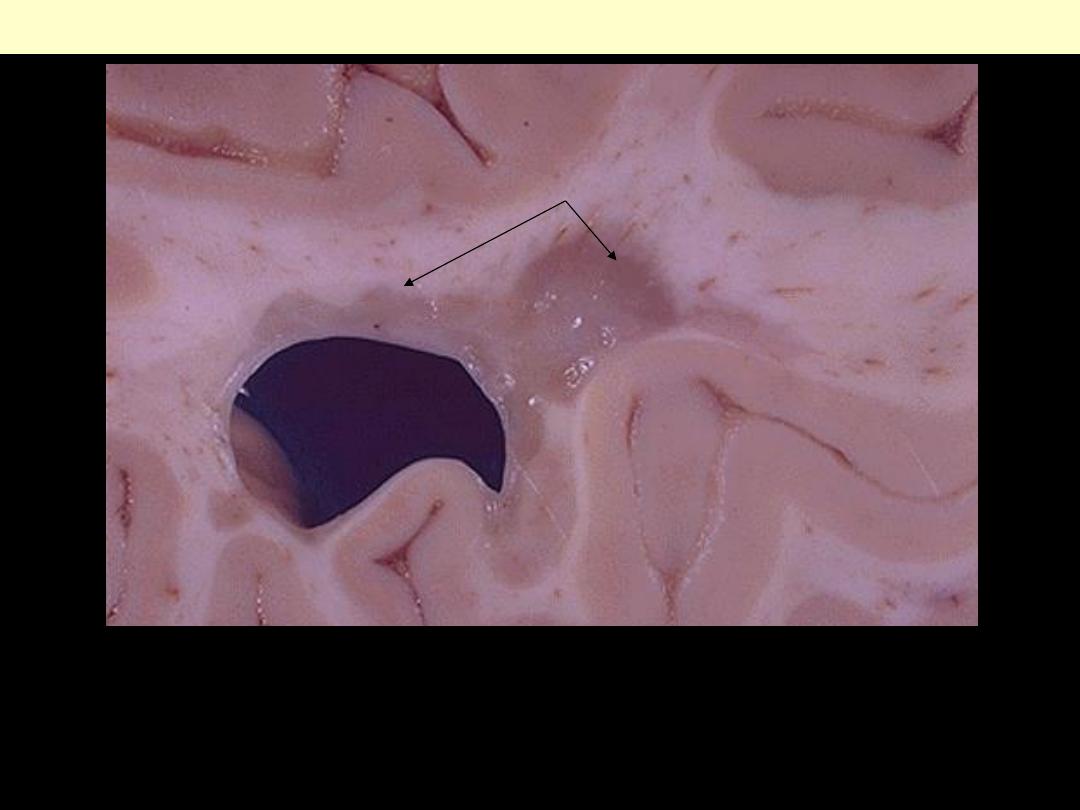
Duret hemorrhage
Progression of transtentorial herniation is often accompanied by hemorrhagic lesions in the midbrain
and pons, termed Duret hemorrhages
Progression of transtentorial herniation is often accompanied by
hemorrhagic lesions in the midbrain and pons, termed Duret hemorrhages.
As mass effect displaces the brain downwards, there is disruption of the
vessels that enter the pons along the midline, leading to hemorrhage.
Duret hemorrhage
Multiple sclerosis
The typical plaque is a well-demarcated, firm, gray-pink lesion. The
periventricular white matter is a common site for these lesions,
although they may occur in any part of the brain or spinal cord.
Seen here in white matter is a "plaque" of demyelination. The
plaque has a grey-tan appearance. Such plaques are typical for
multiple sclerosis (MS
).
Multiple sclerosis
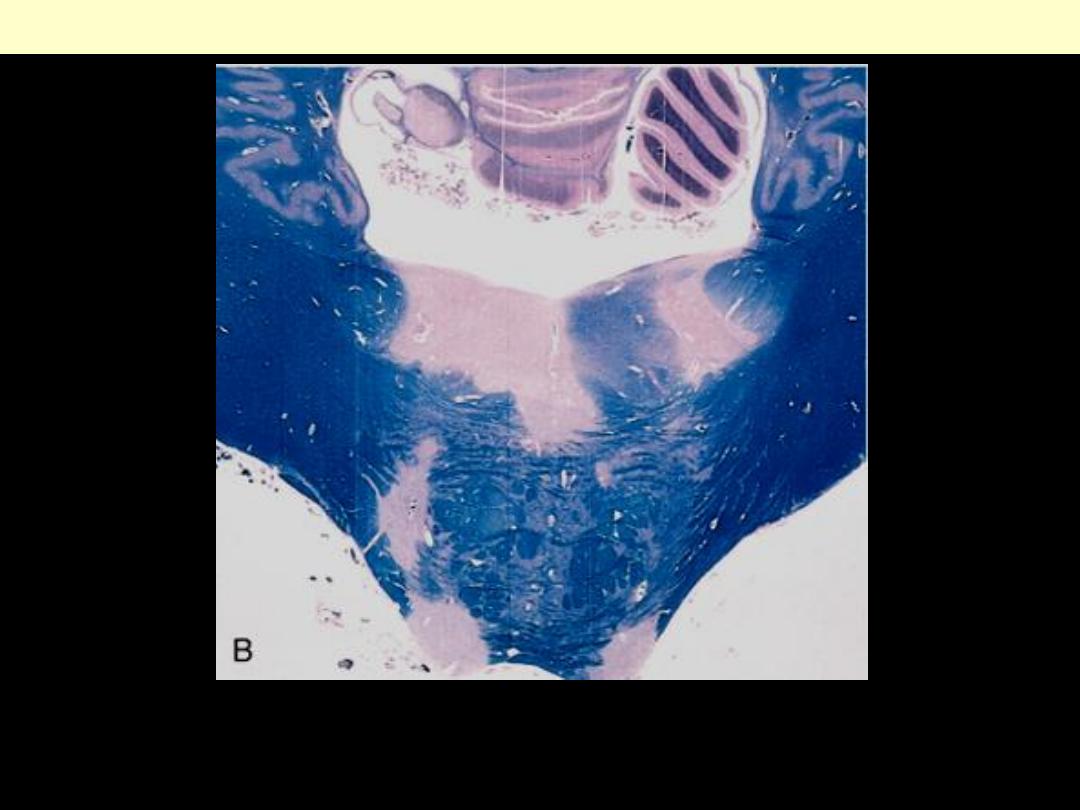
Unstained regions of demyelination (MS plaques) around the fourth
ventricle.
Multiple sclerosis
The arteriolar sclerosis that results from chronic hypertension leads to small
lacunar infarcts, or "lacunes", one of which is seen here in the pons.
Microscopically a lacunar infarct shows a cystic space from the resolved
liquefactive necrosis. Such lesions are most common in basal ganglia, deep white
matter, and brain stem.
Lacunar infarct Pons
Wernicke encephalopathy
Wernicke encephalopathy. Thiamine deficiency in the central nervous system is associated with the
development of hcmorrhagic gray matter lesions, depicted here in the mamillary bodies of the
hypothalamus.
The small petechial hemorrhages in the mammillary bodies seen here are characteristic for Wernicke's
disease, another complication of chronic alcoholism with thiamine deficiency.
Wernicke encephalopathy
