The Era of Hips & Waists
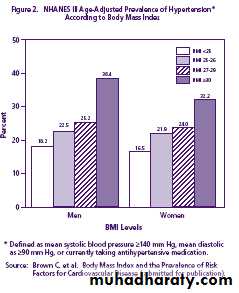
Hypertension in Metabolic syndrome
Common risk factors for chronic diseasesDeaths from 4 chronic diseases
Deaths from all other causes50% of all deaths
3 risk factors
Tobacco
Poor dietLack of exercice
4 chronic diseases
Cancer
Type 2 diabetesChronic respiratory disease
Cardiovascular
Oxford Health Alliance 2003
Obesity, Type 2 Diabetes, Hypertension or Dyslipidemia
Relative riskWaist circumference (cm)
Adapted from Lee ZSK et al. Obes Rev 2002; 3: 173-82 andKo GT et al. Int J Obes Relat Metab Disord 1997; 21: 995-1001
0
History of MS
1923 - Kylin first to describe the clustering of hypertension, hyperglycemia, hyperuricemia1936 - Himsworth first reported Insulin insensitivity in diabetics
1965 - Yalow and Berson developed insulin assay and correlated insulin levels & glucose lowering effects in resistant and non-resistant individuals
1988 - Reaven in his Banting lecture at the ADA meeting coined the term Syndrome X and brought into focus the clustering of features of Metabolic Syndrome
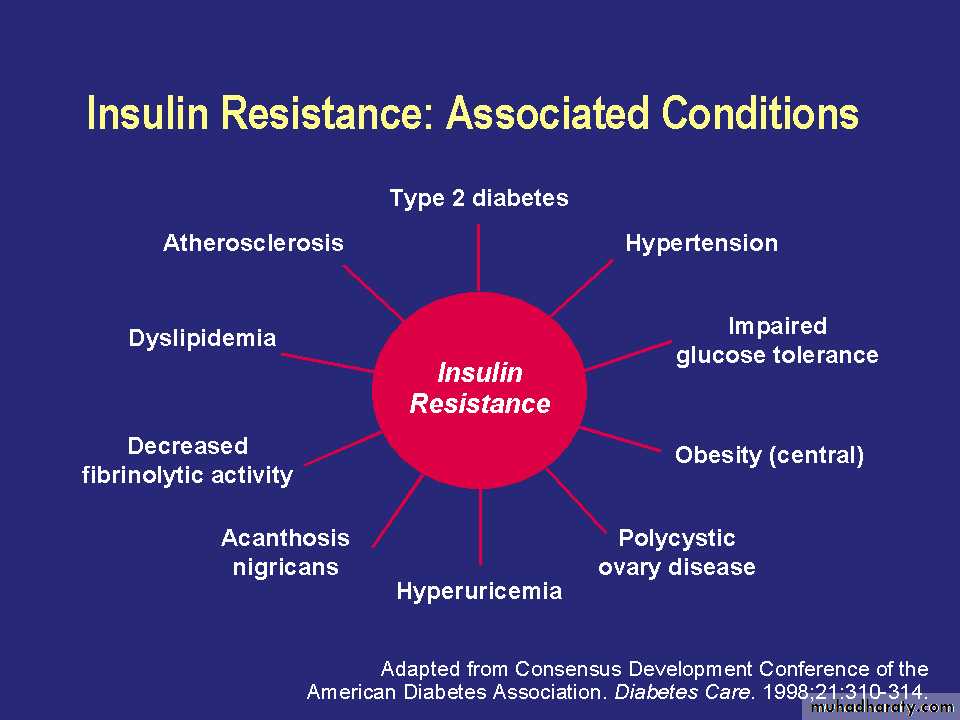
Reaven now prefers the name, Insulin-Resistance Syndrome - feels insulin resistance is the common denominator for Metabolic Syndrome
Metabolic Syndrome
Etiology – not fully elucidatedInsulin Resistance
Acquired causes
• Overweight and central (visceral) obesity
• Physical inactivity, aging, ethnicity
• High CHO diets (>60%)
Proinflammatory state, hormones
Poly Genic causes
INSULIN RESISTANCE - MECHANISMS
Pre receptor ( abnormal insulin or insulin
antibodies)
Receptor ( decreased receptor number or affinity)
Postreceptor (abnormal signal transduction and phosphorylation)
Glucose transporter ( decreased GLUT 4 molecule)
INSULIN RESISTANCE & HYPERTENSION
More than 50 % of hypertensives are found to be Insulin Resistant and Hyperinsulinemic.IR and Hyperinsulinemia have been
documented to be present even in leanHypertensives who are not Diabetic
MS Clustering of Components:
Hypertension: BP. > 140/90Dyslipidemia: TG > 150 mg/ dL ( 1.7 mmol/L )
HDL- C < 35 mg/ dL (0.9 mmol/L)
Obesity (central): BMI > 30 kg/M2
Waist girth > 94 cm (37 inch)
Waist/Hip ratio > 0.9
Impaired Glucose Handling: IR , IGT or DM
FPG > 110 mg/dL (6.1mmol/L)
2hr.PG >200 mg/dL(11.1mmol/L)
Microalbuninuria (WHO)
Necessary Criteria to Make Diagnosis
WHO:
Impaired G handling + 2 other criteria.
Also requires microalbuminuria - Albumen/ creatinine ratio >30 mg/gm creatinine
NCEP/ATP III:
Require three or more of the five criteria
IDF(2006):
Abdominal obesity plus two other components: elevated BP, low HDL, elevated TG, or impaired fasting glucoseMeasurement of Waist
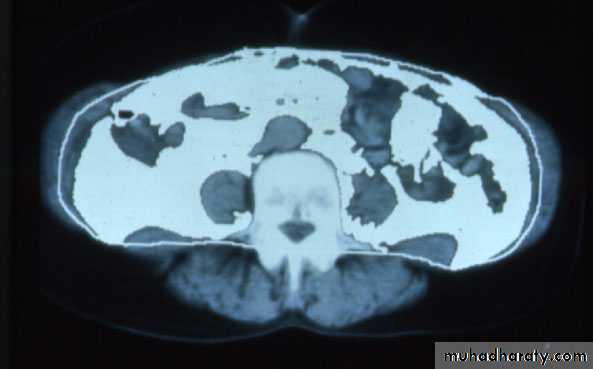
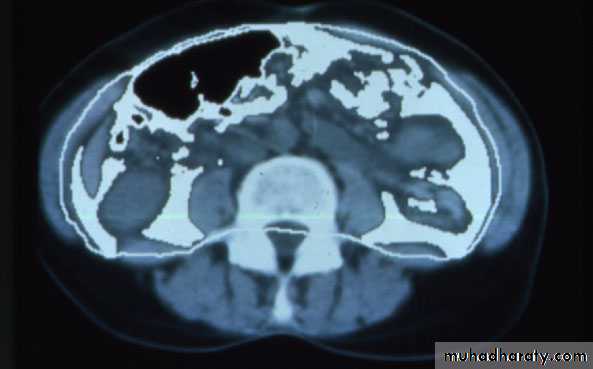
Normal
Visceral AdiposityCourtesy of Wilfred Y. Fujimoto, MD.
Visceral Fat DistributionIDF Waist Circumference
MS2 times increase risk of HT
3 times increase risk of CHD or stroke
5 times increase risk of DM
Chronic liver disease
Increase risk of more than 60 diseases
Resulting Clinical Conditions:
Type 2 diabetesEssential hypertension
Polycystic ovary syndrome (PCOS)
Nonalcoholic fatty liver disease
Sleep apnea
Cardiovascular Disease (MI, PVD, Stroke)
Cancer (Breast, Prostate, Colorectal, Liver)
Hypertension in MS:
IDF:
BP >130/85 or on Rx for previously Dxed hypertension
WHO:
BP >140/90
NCEP ATP III:
BP >130/80
Obesity Effects on Blood Pressure
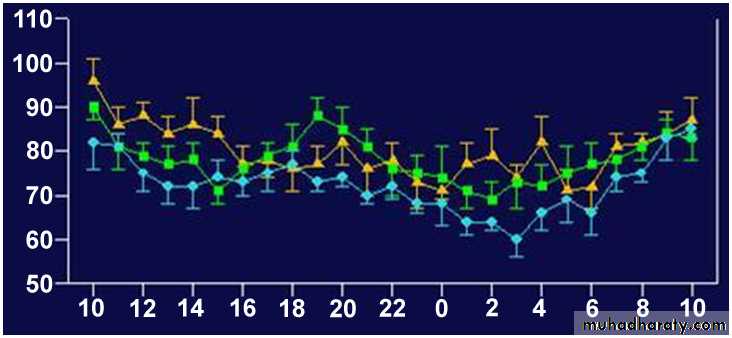
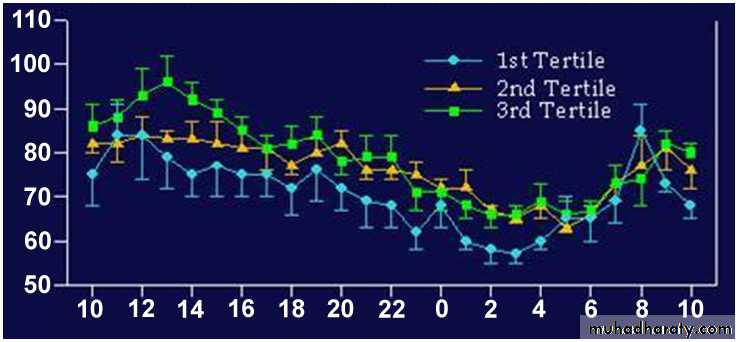
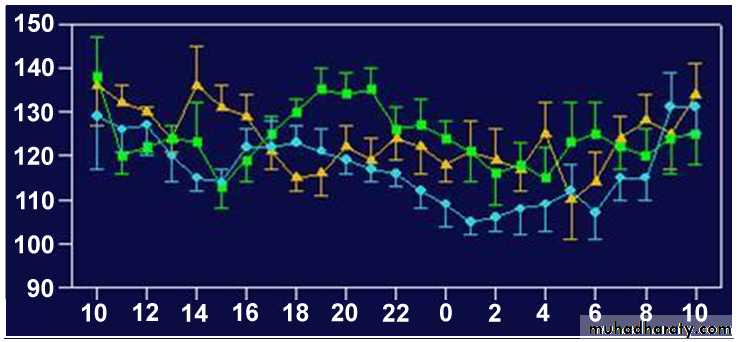
Mean DBP (mmHg)
Clock time (hours)Intra-abdominal (Visceral) Fat Area Tertiles and 24-hour Ambulatory Blood Pressure and Pulse Rate in Chinese Type 2 Diabetic Patients
Clock time (hours)
Mean HR (bpm)
Clock time (hours)
Mean SBP (mmHg)
DBP: diastolic blood pressure
HR: heart rate
SBP: systolic blood pressure
Copyright © 1997 American Diabetes Association
Adapted from Diabetes Care ®, Vol. 20, 1997; 1854-8Reprinted with permission from The American Diabetes Association
Metabolic variables in white coat (WC) and sustained (SUST) borderline hypertension Tecumseh study
Julius et al., Hypertension 16, 1990. Tecumseh
NORMAL WC SUST
N=621N=28
N=34
n.s.
p<.00126
22
18
14
Insulin Level
10
p<.001
Hypertension is a very prominent feature of the metabolic syndrome, present in up to 85% of patients.Metabolic Syndrome & Hypertension
Randomized prospective study in Italy with >1700 people with HTN (mean 155/95) & no CVD, followed for a mean of 4 yearsDuring follow up, 162 pts developed CV events, a total of 593 pts had metabolic syndrome using NCEP guidelines
Those with MS had an almost double CV event rate 3.23 vs 1.76per 100pt years.
Insulin Resistance and Hypertension Mechanisms
HyperinsulinemiaProduces renal sodium retention.
Stimulates Sympathetic Nervous activity
Vascular smooth muscle hypertrophy (mitogenic action of insulin)
cytokines and other lipokines
Augmentation of the pressor and
aldosterone response to angiotensin II
Endothelial dysfunction and decreased production of NO
Results of current long term outcome studies support the hemodynamic concept of insulin
resistance in hypertension
HYPOTHESIS
If in addition to cardiovascular responses, the metabolic responses were also decreased in hypertension, the patient’s ability to dissipate calories would be diminished and they would gain more weight.BP Control - How Important?
MRFIT and Framingham Heart Studies:Conclusively proved the increased risk of CVD with long-term sustained hypertension
Demonstrated a 10 year risk of cardiovascular disease in treated patients vs non-treated patients to be 0.40.
40% reduction in stroke with control of HTN
therapy
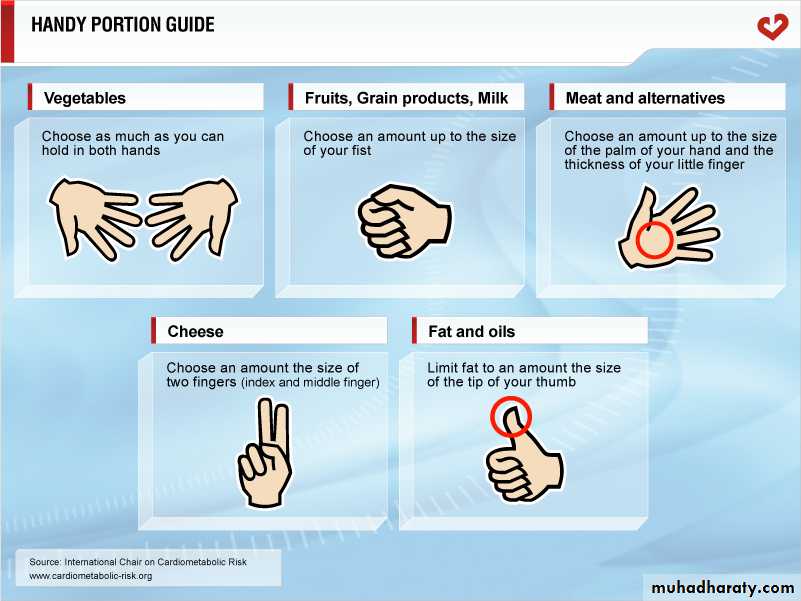
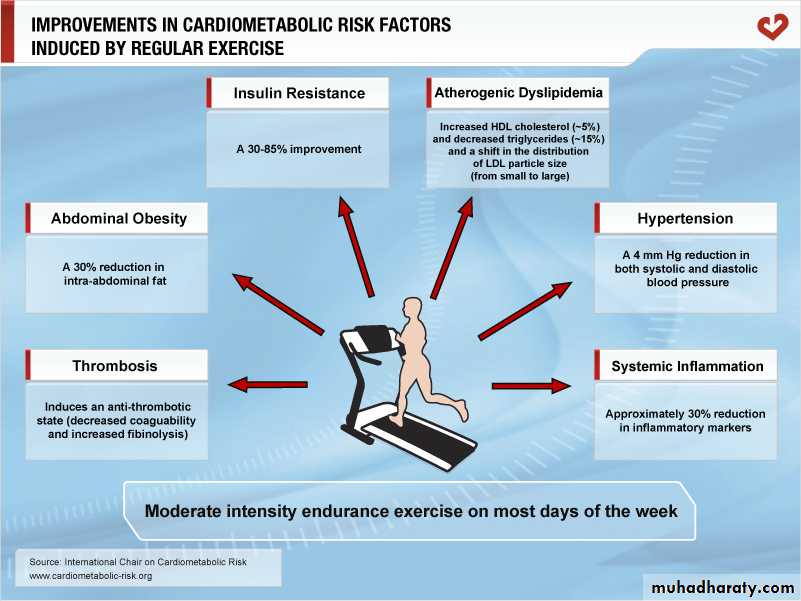
a multi-target approach based on the assessment of the overall cardiovascular risk should be applied;A-non-pharmacological therapy; sodium restriction, alcohol and calorie restriction, smoking cessation, weight reduction, and increase physical activity.
Antihypertensive Medications:
Angiotensin -converting Enzyme Inhibitors (ACEI)Angiotensin II Receptor (ARB) Blockers
Combination with Thiazides, Calcium Channel Blockers, Cardioselective Beta Blockers
Target BP: <130/80
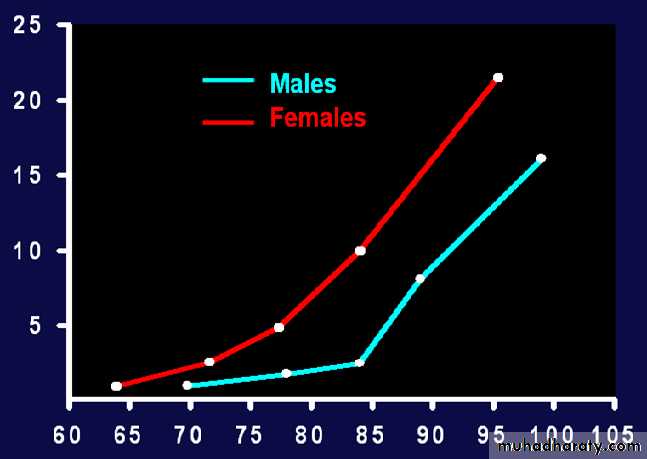
Fit vs. Fat: Can you be both?
Overweight and obese people who are fit are less likely to die prematurely than unfit people who are lean (Lee, CD, et al., Am J Clin Nutr 1999; 69:373-380)Highly Fit men with 2 or 3 risk factors had about the same mortality risk as Low Fit men with no risk (Blair, SN, et al., JAMA 1996; 276: 205-210)
Low Fitness is as significant a risk factor for premature death as smoking, high blood pressure, diabetes, and high blood cholesterol, regardless of weight ( Barlow et al., Int J Obes Metab Disord, 19(suppl 4):41, 1995 and Wei et al., JAMA, 282: 1547, 1999)
-For preventive purposes