Hypospadius
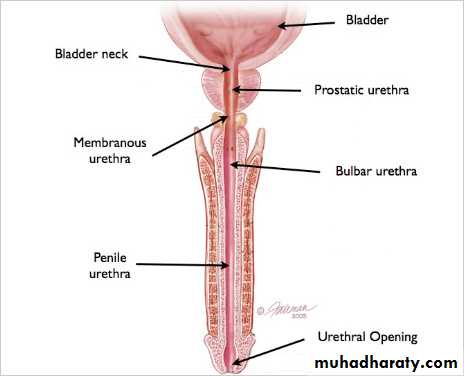
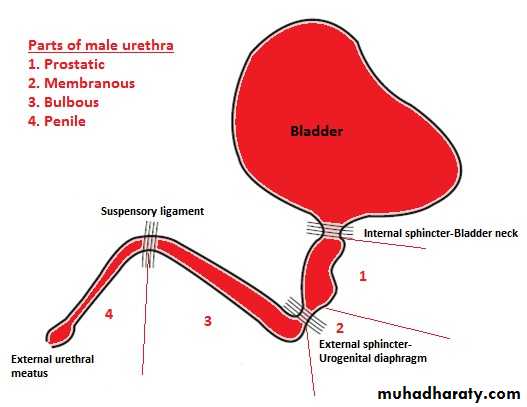
Urethral Disorder in MalesAnatomy of Male Urethra
What is Hypospadius??
What is Hypospadius
• It is the most common congenital malformation of the urethra
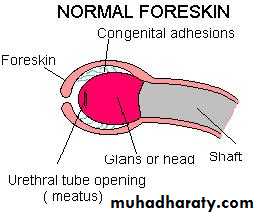
• It’s incidence is about 1 in 200-300 boys• In which the external urethral meatus opens on the ventral aspect of the penis or on perineum
• The foreskin may be absent on ventral aspect of the penis & excessive on dorsal aspect
• Hooded foreskin
Classification of Male Hypospadius
Classification of Male Hypospadius
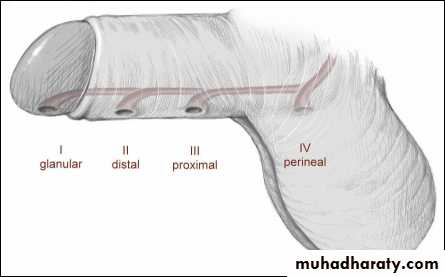
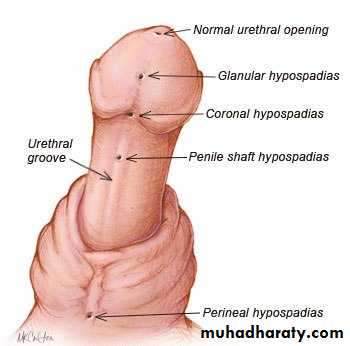
Classification of Male HypospadiusHypospadias can be classified according to the anatomical location of the urethral meatus .
Anterior (or distal)—glandular, coronal, and subcoronal (~50%)
Middle—distal penile, midshaft, and proximal penile (~30%)
Posterior (or proximal)—penoscrotal, scrotal, and perineal (~20%)
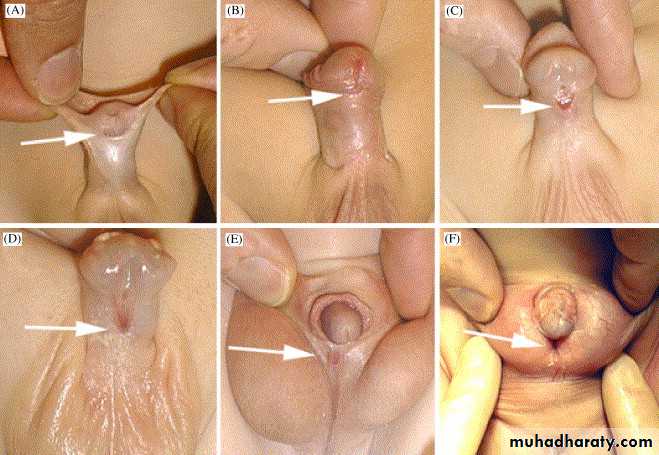
• Low vaginal ectopia of external urethral opening
• High vaginal ectopia of external urethral opening• Vescicovaginal (fusion of bladdar neck with vagina)
• Ectopia in urogenital sinus
(Female hypospadius is rare )
Classification of female hypospadius
Why Hypospadius Occur
• Cosmotic problem• Abnormal urinary stream on micturation
• Defect in erection
• Severe hypospadius associated with chordee….
Problems Caused by Hypospadius
Does hypospadius associated with any other anomalies
Isolated hypospadius Associated with :- - undescended testes - inguinal hernia-predispose to urinary tract infection&stone
• Urethroscopy & cystoscopy (to assess normal development of internal male sexual organs )
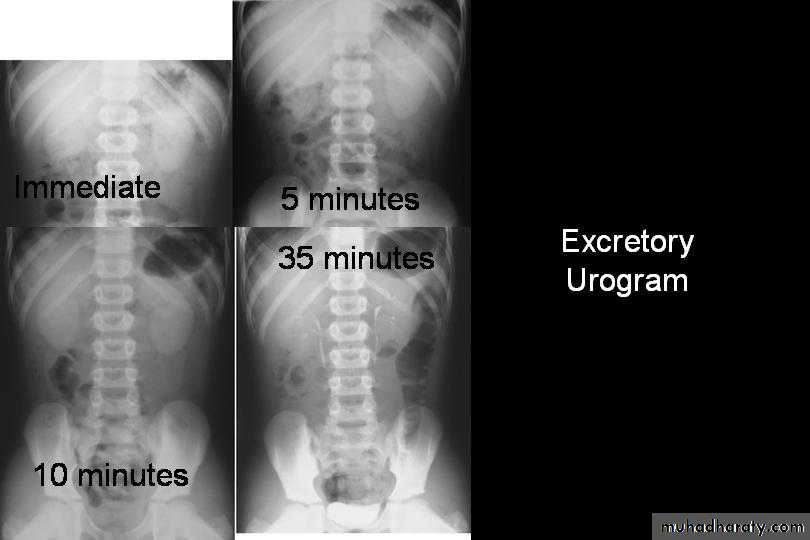
• Excretory urography
• Karyotyping (to establish the genetic sex )
Investigation in child has hypospadius:-
Circumcision must be avoided in infants with hypospadius , because the foreskin is often required for later reconstructive surgery
Surgical Correction of Hypospadius
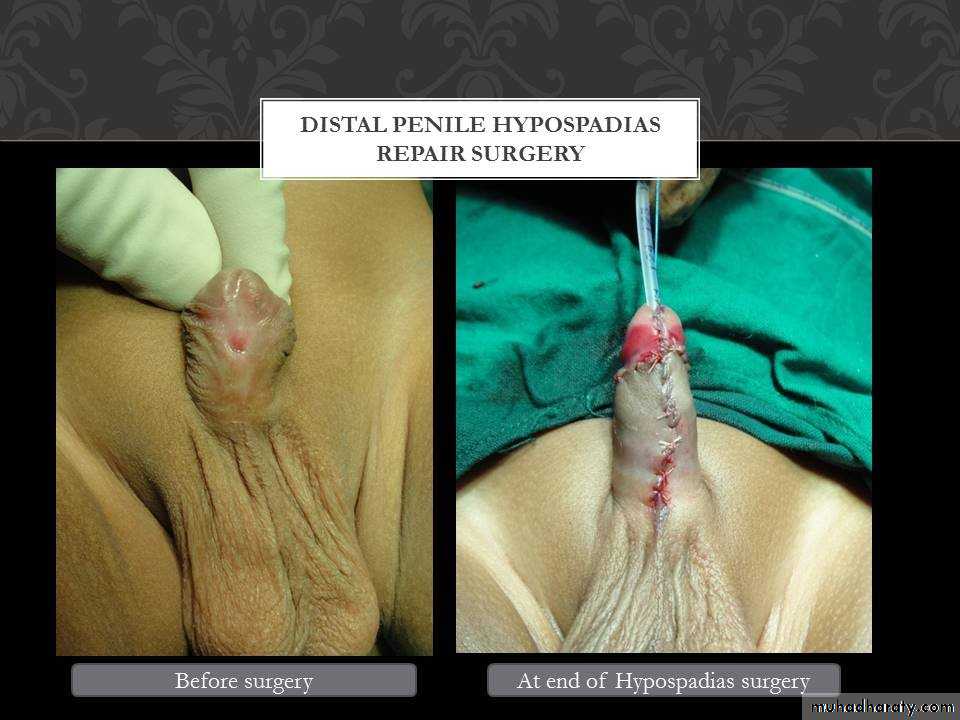
• MAGPI (meatal advancment glansplasty )
• GAP (glans approximation procedure)• Primery tubularization
• Tuburlarized incised plate urethroplasty
-:Anterior hypospadius
• Urethral plate preservation
• Transverse tubularized island flap• Two-stage hypospadius repair
(first stege:correction of penile chordee & transfer of dorsal foreskin to the ventral aspect of the penis)
(second stage:urethroplasty is done 6 months later)
Posterior hypospadius :-
Complication of surgical correction of hypospadius
• Bleeding &hematoma
• Wound infection• Penile &scrotal edema
• Flap necrosis
• Urethral stent related problem (block; slipping)
Early complication
• Scarring
• Fistula• Urethral stricture
• Urethral diverticula
Late complication
Pediatric Urology Posterior urethral valve
Posterior urethral valve
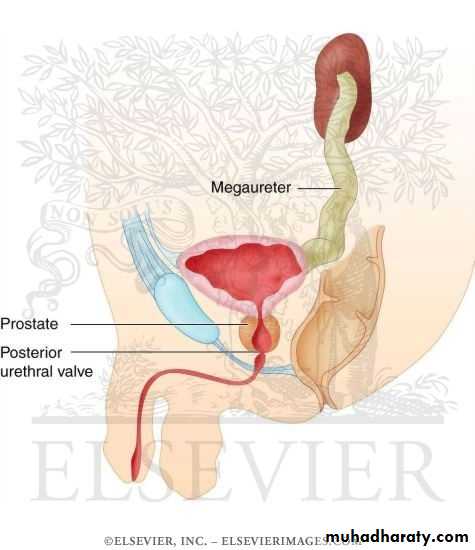
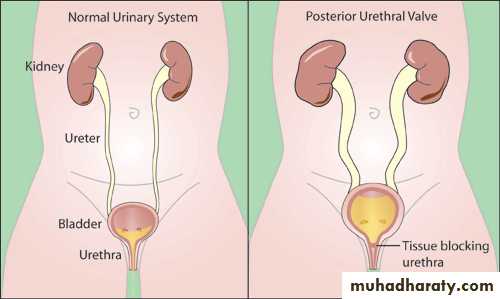
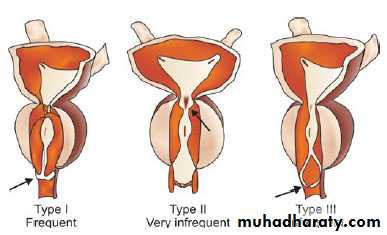
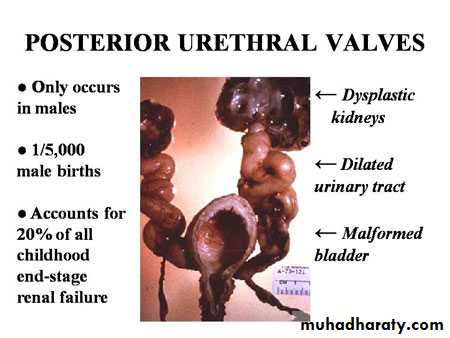
A posterior urethral valve is an obstructing membrane in the posterior male urethra as a result of abnormal embryological development and it is the most common cause of bladder outlet obstruction in male neonate.The embryological abnormality giving rise to posterior urethral valves is thought to represent either an anomalous insertion of the mesonephric duct into the uro-genital sinus, preventing normal migration of these ducts and their anterior fusion or a consequence of an abnormality of the cloacal membrane.
Classification
PUV and its consequences
1- Renal dysplasia2- Upper tract dilatation
3- VUR
4- UTI 5- Bladder dysfunction
This accounts for 25-30% of pediatric renal transplantation in UK
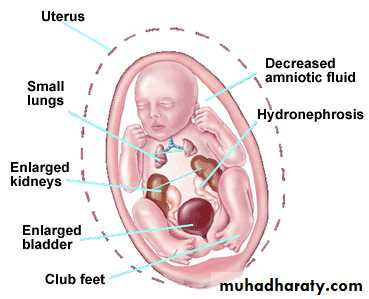
Prenatal Diagnosis
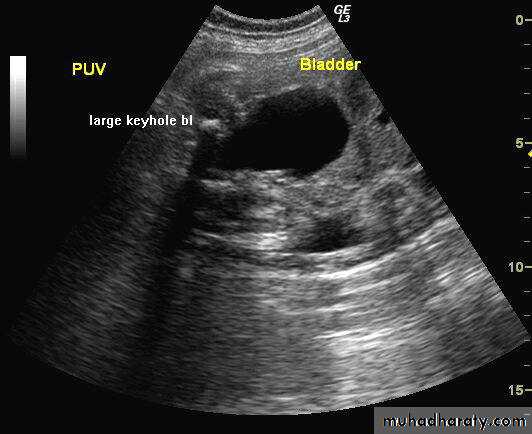
Approximately ½-2/3of boys with PUV will be suspected prenatally. Prenatal findings on ultrasonography in suspected cases may include:
a thick walled bladder, the ‘keyhole’ sign with a dilated bladder and posterior urethra, unilateral or bilateral hydroureteronephrosis, echobright kidneys and oligohydramnios.
Investigation
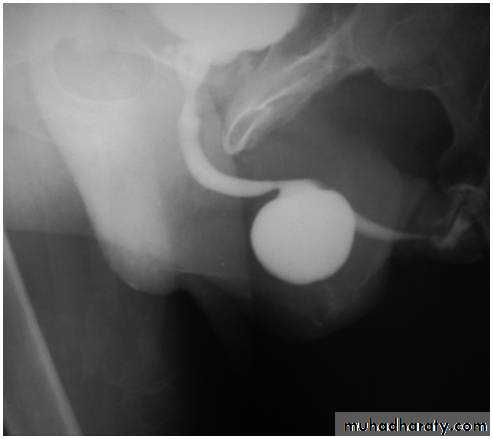
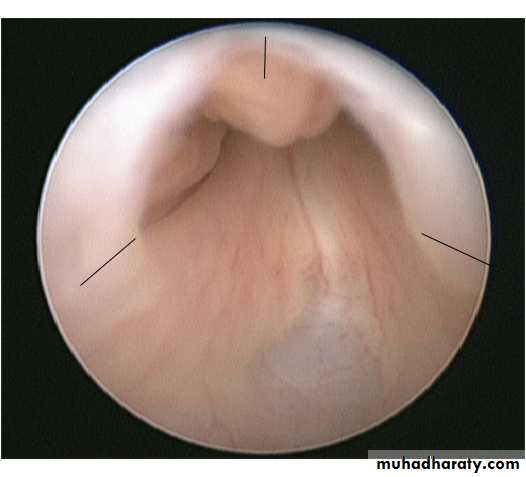
Ultrasound scan of kidneys and bladder.VCUG shows distended and elongated posterior urethra; partially filled anterior urethra; bladder neck hypertrophy; lucencies representing valve leaflets; thick-walled bladder (±diverticuli); incomplete bladder emptying; reflux (50%).
Isotope renal scan (MAG-3, DMSA) assesses renal function.
Videourodynamics allows diagnosis of associated voiding dysfunction.
US : Keyhole sign
VCUG
Treatment
Commence prophylactic antibiotics immediately, check serum electrolytes, and drain the bladder with a pediatric feeding tube. If there is improvement, cystoscopy and transurethral ablation of valve If upper tracts remain dilated with raised creatinine after bladder drainage, a temporary cutaneous vesicostomy is indicated. An alternative is ureterostomy drainage. Valve ablation is performed at a later stage.
Treatment: endoscopic valve ablation
is a high risk procedure reserved for cases with severe oligohydramnios, to try to limit the associated lung underdevelopment, or pulmonary hypoplasia, that is seen at birth in these patients.
Postoperative follow up
A urethral catheter is placed at the end of the procedure and removed 24-48 hours later.The creatinine should be checked following catheter removal and the nappies weighed to document urine output.
Antibiotic prophylaxis and renal supplements should continue until further review.
The complications of primary valve ablation include
1- Bleeding2- incomplete valve resection
3- urethral stricture
4- inadvertent damage to the external sphincter. The choice of technique is dictated by the instruments available, calibre of the neonatal urethra and the size and maturity of the baby.
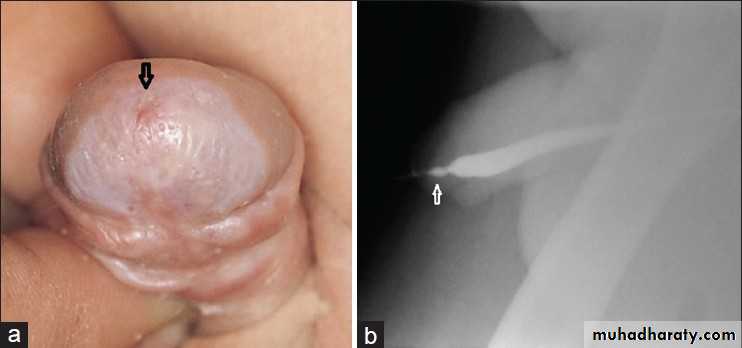
PHIMOSIS
BackgroundAt the end of the first year of life, retraction of the foreskin behind the glanular sulcus is possible in only about 50% of boys.
The phimosis is either primary (physiological), with no sign of scarring, or secondary (pathological), resulting from scarring due to conditions such as balanitis xerotica obliterans.
Phimosis must be distinguished from normal agglutination of the foreskin to the glans, which is a physiological phenomenon.
Treatment
Plastic circumcision (dorsal incision, partial circumcision) carries the potential for recurrence of the phimosis.Associated frenulum breve is corrected by frenulotomy. Meatoplasty is added if necessary.
Paraphimosis
It is characterised by retracted foreskin with the constrictive ring localised at the level of the sulcus.A dorsal incision of the constrictive ring may be required, or circumcision is carried out immediately or in a second session.
MONOSYMPTOMATIC NOCTURNAL ENURESIS
BackgroundEnuresis is incontinence during the night. Any wetting during sleep above the age of five years is enuresis.
It is important to note that there is a single symptom only. Due to an imbalance between night-time urine output and night-time bladder capacity, the bladder can easily become full at night, and thechild will either wake up to empty the bladder or will void during sleep.
Assessment:
Voiding diary or direct questioning including:Voiding habits Weing episodes
Bowel function
Urinalysis
Education
Supportive therapy
Alarm or desmopressin
Consider longer use of desmopression Combination therapies
Imipramine