Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Surgical anatomy:
The name ‘pancreas’ is derived from the Greek ‘pan’ (all) and ‘kreas’(flesh).
Weight 80 g situated retroperitoneally.
head=30 per cent of the gland
body and tail 70 per cent of gland
The superior mesenteric vein joins the splenic vein to form the portal vein
behind the neck of the pancreas near its upper border.
80—90 per cent of the pancreatic mass is composed of exocrine tissue.
Islet of Langerhans cells consist of differing cell types:
75 per cent are B cells (producing insulin),
20 per cent A cells (producing glucagon),
Remainders are D cells (producing somatostatin) and a small number of
pancreatic polypeptide cells.

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Surgical physiology:
In response to a meal, the pancreas secretes digestive enzymes in an alkaline
(pH 8.4) bicarbonate-rich fluid.
The hormone secretin which is released from the duodenal mucosa evokes a
bicarbonate-rich fluid.
Cholecystokinin-pancreozymin (CCK) is released from the duodenal mucosa
in response to food: CCK produces no increase in the volume of secretion,
but is responsible for enzyme secretion.
Vagal stimulation increases volume.
Investigations:
1. pancreatic damage
Measurement of amylase is the most widely used test of pancreatic damage.
The serum amylase rises within a few hours of pancreatic damage and declines
over the next 4—8 days. A markedly elevated serum level is highly suspicious
of acute pancreatitis.
2. pancreatic function:
Measuring bicarbonate and enzymes produced in the pancreatic juice.
Indirect Lundh test produced by the ingestion of a test meal
Direct stimulated by injection of a hormone secretin and CCK can be
administered intravenously to produce both bicarbonate and enzyme
stimulation.
Chronic pancreatitis cannot be diagnosed until over 70 per cent of the
gland has been destroyed or there is obstruction to the duct.
So these tests have been largely abandoned.
The more practical test is the nitroblue tetrazolium—para-aminobenzoic
acid (NBT PABA) tests in which the recovery in the urine of PABA is
measured after oral administration.
A simpler test now available is one which measures faecal elastase levels.
Absence indicates chronic pancreatitis and is specific.
3. Morphological abnormality of the parenchyma and duct system.
Ultrasonography
Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Computerized tomography (CT),
Magnetic resonance imaging (MRI)
Endoscopic retrograde cholangiopancreatography (ERCP).
Ultrasonography
bile duct dilated
presence or absence of a mass in the pancreas
the coexistence of gallstones or gross disease within the liver such as metastases
Computerized tomography
Pancreatic carcinomas of 1—2 cm in size can usually be demonstrated
A specific pancreatic protocol should be followed using a spiral CT scanner.
Following rapid injection of intravenous contrast, scanning is performed at 5-
mm intervals in the arterial phase and 10-mm intervals during the venous phase.
Prior to injection of contrast an unenhanced CT scan is essential to determine
the presence of calcification within the pancreas and gall bladder.
The stomach and duodenum should be outlined with water and distended to
define the duodenal loop.
CT-Scan preferred technique for defining Endocrine tumours.
CT scanning is also of value in the therapeutic setting to drain cysts or
abscesses, or to guide percutaneous biopsies.
Magnetic resonance imaging
Magnetic resonance pancreatography and cholangiography may well replace
diagnostic endoscopic pancreatography and cholangiography.
Endoscopic retrograde cholangiopancreatography
Changes seen in chronic pancreatitis include:
pancreatic duct strictures,
dilatation of the main pancreatic duct with stones ,
abnormalities of pancreatic duct side branches,
communication of the pancreatic duct with cysts
Bile-duct strictures.
Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
In pancreatic carcinoma, the main pancreatic duct may be narrowed or
completely obstructed at the site of the tumor with dilatation upstream but with
a normal duct system downstream. This, in conjunction with bile-duct
obstruction or a stricture, results in the so-called ‘double duct sign’.
Collection of bile or pancreatic juice at endoscopy and brushing of these ducts
can yield cells which confirm the suspected diagnosis of carcinoma
Plain X-ray
A chest X-ray should never be forgotten as it may show a complication of
pancreatic disease.
A plain X-ray before contrast studies is essential to delineat calcification.
Pancreatitis
Acute pancreatitis
Definition: acute condition presenting with abdominal pain and usually associated
with raised pancreatic enzyme levels in the blood or urine as a result of
inflammatory disease of the pancreases.
The mechanism of damage in pancreatitis is auto-digestion of the gland by its own
enzymes.
Incidence
Acute pancreatitis accounts for 3 per cent of all cases of abdominal pain
admitted to hospital.
About one-third of patients die in the early phase of an attack from multiple
organ failure,
Deaths occurring after the first week of onset are due to infective complications.
Aetiology
The two major causes of acute pancreatitis are:
biliary calculi, 50—70 per cent of patients,
and alcohol, 25 per cent of patients,.

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
rare causes:
After biliary or gastric surgery especially after billrith 2 partial gastrectomy, if
pancreatic duct is injured orduodenal loop obstruction producing high duodenal
pressure.
After trauma as blow to pancreas.
Distortion of ampulla's of Vater as result of peptic ulcer or ampullary
carcinoma.
As result of generalized disorder as hypercalcaemia, hyperlipidemia, D.M,
prophyria.
Drugs as corticosteroids
Viral infections as mumps.
Autoimmune diseases as polyarteritis nodosa.
Impaired pancreatic blood flows after cardio-pulmonary by –pass and following
hypothermia.
Idiopathic
The importance of aetiology is that removal of the causative factor can avoid
further episodes of pancreatitis. Thus, in a patient who has gallstone pancreatitis,
the gallstones should be removed as soon as the patient is fit to undergo surgery
and, preferably, before discharge from hospital.
Clinical presentation
Pain is usually the cardinal symptom. characteristically develops quickly
The pain is frequently severe or even agonising, it is refractory to the usual
doses of analgesics, and constant in nature and intensity.
Pain is usually experienced first in the epigastrium but may be localised to
either upper quadrant or felt diffusely throughout the abdomen.
There is radiation to the back in about 50 per cent of patients and some
patients may gain relief by sitting or leaning forwards.
Nausea, vomiting and retching are usually marked accompaniments.
Hiccoughs can be troublesome and may be due to gastric distension or
irritation of the diaphragm.

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Acute pancreatitis should be suspected in the patient who:
Develops marked abdominal pain, fever or unexplained shock following
abdominal surgery.
presents with diabetic coma and shock;
Has clinical features suggesting myocardial infarction with abdominal
distension.
On examination
Tachypnea is common,
Tachycardia is usual and hypotension may be present.
The body temperature is often normal or even subnormal, but frequently rises as
inflammation develops.
Mild icterus can be caused by biliary obstruction in gallstone pancreatitis, and
acute swinging pyrexia suggests cholangitis.
Bleeding into the fascial planes can produce blueish discoloration of the flanks
(Grey Turner sign) or umbilicus (Cullen’s sign). Neither sign is pathognomonic
of acute pancreatitis; in fact Cullen’s sign was first described with rupture of an
ectopic pregnancy.
Subcutaneous fat necrosis may produce small red tender nodules on the skin of
the legs.
Abdominal examination may reveal distension due to ileus or, more rarely,
ascites with shifting dullness.
A mass can develop in the epigastrium due to inflammation.
There is usually muscle guarding in the upper abdomen, although marked
rigidity is unusual.
A pleural effusion is present in 10—20 per cent of patients.
Pulmonary oedema and pneumonitis are also described and may give rise to the
differential diagnosis of pneumonia or myocardial infarction.
The patient may be confused and exhibit the signs of metabolic derangement
together with hypoxaemia.
Investigations
A serum amylase four times above normal is indicative of the disease.
Plain abdominal X-ray findings include a generalised or local ileus (sentinel
loop), a colon ‘cut-off’ sign and a renal ‘halo’ sign.
Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Occasional helpful, but nondiagnostic, signs include calcified gallstones and
pancreatic calcification.
A chest X-ray may show a spectrum of changes depending on the disease
severity. A pleural effusion is present in 20 per cent, and in severe cases a
diffuse alveolar interstitial shadowing may suggest an acute respiratory distress
syndrome
Ultrasound scanning The swollen pancreas may be detected but the gland is
poorly visualised in 25—50 per cent of cases. Ultrasound is valuable in
detecting free peritoneal fluid, gallstones, dilatation of the common bile duct
If doubt remains a CT scan should be performed in order to determine the
diagnosis.
Laparotomy. To misdiagnose acute pancreatitis is not uncommon because the
presentation is so variable that even the shrewdest clinician can be mistaken.
The appearances at laparotomy are characteristic.
Management:
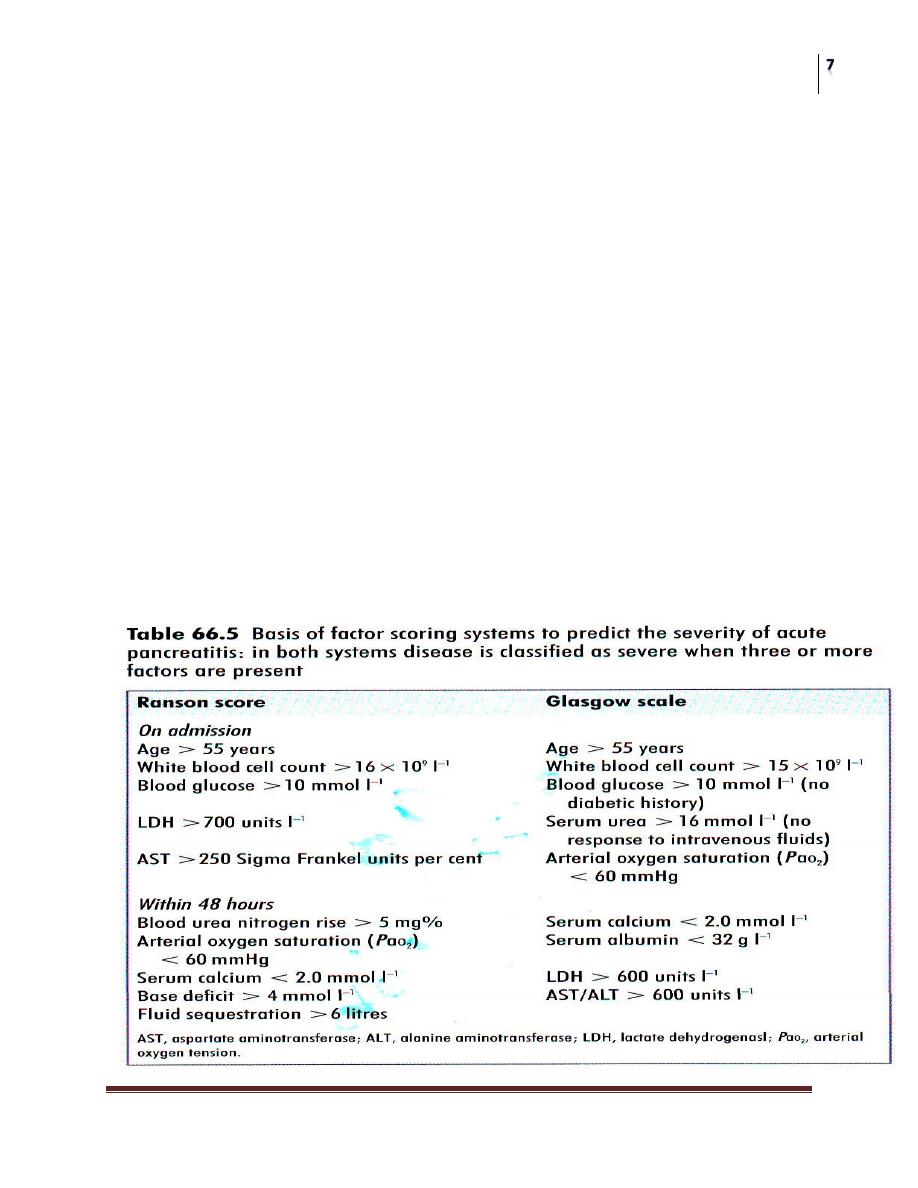
Scoring
Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Mild attack
conservative approach is indicated with
nil by mouth, intravenous fluid administration and
frequent, but noninvasive, observation
Antibiotics are not indicated unless there is evidence of infection.
CT scanning is unnecessary unless there is evidence of deterioration
severe attack
More aggressive approach is required with the patient being admitted to a high-
dependency or an intensive care unit.
The patient is monitored invasively to ensure homeostasis of the cardiovascular,
respiratory and renal systems.
Full resuscitation and strict asepsis should be observed in the placement of all
monitoring lines.
If there is evidence of cardiocirculatory compromise then a Swan—Ganz
catheter should be inserted in order to measure pulmonary artery wedge
pressure, cardiac output and systemic resistance.
Regular arterial blood gas analysis is essential as the onset of hypoxia and
acidosis may be detected late by clinical means alone.
appropriately sedated and adequate analgesics given.
There is some evidence to support the use of prophylactic antibiotics in the
prevention of local and other septic complications. Intravenous cefuroxime or
imipenem is advised.
If gallstones are the aetiology of severe pancreatitis, an urgent ERCP is
indicated to exclude the presence of a stone stuck in the ampulla of Vater mif
there is no improvement in the general condition of the patient within 48 hours.
The presence of cholangitis with abnormal liver function tests is an indication
for urgent endoscopic intervention.
Surgical intervention is only contemplated in the patient who deteriorates
following successful stabilisation. Once the presence of infected necrosis is
suspected and confirmed, an appropriate débridernent may be performed.
Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Complications
General.
1. Shock: due to hypovoleamia as result of gastrointestinal fluid loss,
retroperitoneal and pleural fluid collection may be associated with low Hb, and
electrolyte disturbance. The central venous pressure should be monitored, fluid
replacement, in form of whole blood, plasma expanders and albumin.
2. Pulmonary insufficiency: hypoxia common, due to retroperitoneal haematoma
and edema, elevation of diaphragm, reduced ventilation due to pain, shunting of
blood in the lung, high affinity to oxyhemoglubin. The treatment by O2 and +ve
pressure of ventilation.
3. Colonic stricture: due to scarring of colon and mesocolon at point overlies the
pancreas.
4. Hypocalcaemia: 3-30 %due to fat necrosis and saponification. Also high
calcitonin and low parathyroid hormone may play a role to cause .I.V Ca can be
replaced by if tetany occurred. It is of poor prognosis.
Local
Acute fluid collection.
Occurs early in the course of acute pancreatitis and is located in or near the
pancreas. The wall encompassing the collection is ill defined.
Acute pseudocyst:
A collection of pancreatic juice enclosed in a wall of fibrous or granulation tissue
that arises following an attack of acute pancreatitis Formation of a pseudocyst
requires 4 weeks or more from the onset of acute pancreatitis.
Pancreatic necrosis :
A diffuse or focal area of nonviable parenchyma which is typically associated with
peri pancreatic fat necrosis. The onset of infection results in infected necrosis
which is associated with a trebling of the mortality rate.

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Pancreatic abscess:
A circumscribed intra-abdominal collection of pus, usually in proximity to the
pancreas containing little or no pancreatic necrosis.
Pancreatic effusion
An encapsulated collection of fluid arising as a consequence of acute pancreatitis,
typically in the pleural cavity.
Pancreatic ascites.
Chronic generalized peritoneal enzyme-rich effusion usually associated with
pancreatic duct disruption.
Pseudoaneurysm.
Pseudoaneurysm is a false aneurysm of a major peripancreatic vessel confined as a
clot by the surrounding tissues and often associated with infection. Recurrent
bleeding is common, often culminating in fatal haemorrhage.
Management of local complications
If fluid collections cause symptoms or impair function then percutaneous or
transgastric drainage is appropriate.
The only indication for operative intervention in acute pancreatitis is the
presence of an abscess related to necrosis in or around the pancreas.
To determine whether a collection of peripancreatic oedema and fluid is
necrotic and infected, a CT scan should be performed and a needle passed into
the necrotic area under CT guidance, choosing a path that does not traverse
hollow viscera.
If the aspirate is infected and the patient’s condition deteriorating, then a
laparotomy with débridement of the dead tissue around the pancreas is
appropriate.
Because the process is progressive further necrotic tissue may form, and the
abscess cavity can either be drained and flushed (Beget) or repeated
laparotomies performed until there is a clean granulating cavity (Bradley).
Some of these patients are ill for long periods of time. Nutritional support is
essential. During the early phase of disease parenteral nutrition is important and
no advantage has yet been shown for early enteral nutrition.

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
However, once the phase of paralytic ileus has been passed it is appropriate to
commence nasojejunal feeding or feeding via a jejunostomy placed in those
who have undergone laparotomy.
This has the effect of reducing the risk of sepsis from parenteral feeding, and
enteral feeding restores the gut mucosal barrier preventing bacterial
translocation through the damaged mucosa.
Acute pancreatic pseudocysts (PP)
Complicate 5-10% of attacks of acute pancreatitis, and their persistence is often
associated with disruption of the pancreatic duct secondary to pancreatic
necrosis.
Some 30-60% of acute PP may resolve spontaneously,
and a period of
observation is therefore warranted.
Persistent, symptomatic, large (greater than 6 cm), enlarging and complicated
PP are indications for intervention.
Whilst external drainage may be necessary in septic patients with infected PP
and those critically ill,
internal drainage provides optimal management of
persistent symptomatic PP as it avoids an external pancreatic fistula and
considerably reduces the risk of recurrence.
Although internal drainage is traditionally achieved by open surgery, minimally
invasive approaches have gained increasing credibility in recent years and may
include endoscopic trans-mural or trans-papillary options and laparoscopic
approaches
Prognosis of acute pancreatitis
Acute mild episode mortality should be less than 1 per cent while severe attack
20—25 per cent mortality.
Those who have infected necrosis a mortality of up to 50 per cent .
The failure to remove a predisposing factor could lead to a second attack of
pancreatitis, which could be fatal.

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Chronic pancreatitis
• Defined as a continuing inflammatory disease of the pancreas characterized
by irreversible morphological changes typically causing pain and/or
permanent loss of function.
Pathology and aetiology
The pancreas enlarges and becomes hard as a result of fibrosis.
The ducts become distorted and dilated.
Calcified stones may form within the ducts.
The most frequent cause of chronic pancreatitis is high alcohol consumption.
Other causes are pancreatic duct obstruction resulting from stricture formation
after trauma, acute pancreatitis or even occlusion of the duct by pancreatic
cancer.
Hereditary pancreatitis, begins at a young age, is associated with a high
incidence of diabetes mellitus and stone formation is frequent.
The importance of hereditary pancreatitis and pancreatitis occurring at a young
age is that there is an undoubtedly increased risk of the development of
pancreatic cancer, particularly if the patient smokes tobacco heavily.
Clinical features
Pain is the outstanding symptom in the majority of patients.
The site of pain depends to some extent on the main focus of the disease.
If the disease is mainly in the head of the pancreas then epigastric and right
subcostal pain is common, while if it is limited to the left side of the pancreas
then left subcostal and back pain are the presenting manifestations.
Radiation to the shoulder, usually the left shoulder, occurs.
Nausea is common during attacks, and vomiting may occur.
All of the complications of acute pancreatitis can occur with chronic
pancreatitis.
Weight loss is common, in that the patient does not feel like eating because of
pain.

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Loss of exocrine function will occur leading to steatorrhoea which can be
debilitating without supplementation
Loss of endocrine function and the development of diabetes are not uncommon,
and the incidence increases as the disease progresses.
Investigation
Only in the early stages there be a rise in serum amylase
Pancreatic function tests merely confirm the presence of pancreatic
insufficiency or that more than 70 per cent of the gland has been destroyed.
The prime investigation is either an MRI scan or a CT scan which will show the
outline of the gland, the main area of damage and the possibilities for surgical
correction.
An MR cholangiogram will show the presence of biliary obstruction, and an
MR pancreatogram the state of the pancreatic duct.
An ERCP can elucidate the anatomy of the duct and, in conjunction with the
whole organ morphology, determine the type of operation required, if operative
intervention is indicated.
Treatment
A diet low in fat and with no alcohol is advised
Pancreatic enzyme supplementation may reduce the frequency of painful crises.
The use of morphine should be avoided and tobacco smoking stopped.
The role of surgery is in overcoming obstruction and removing mass lesions.
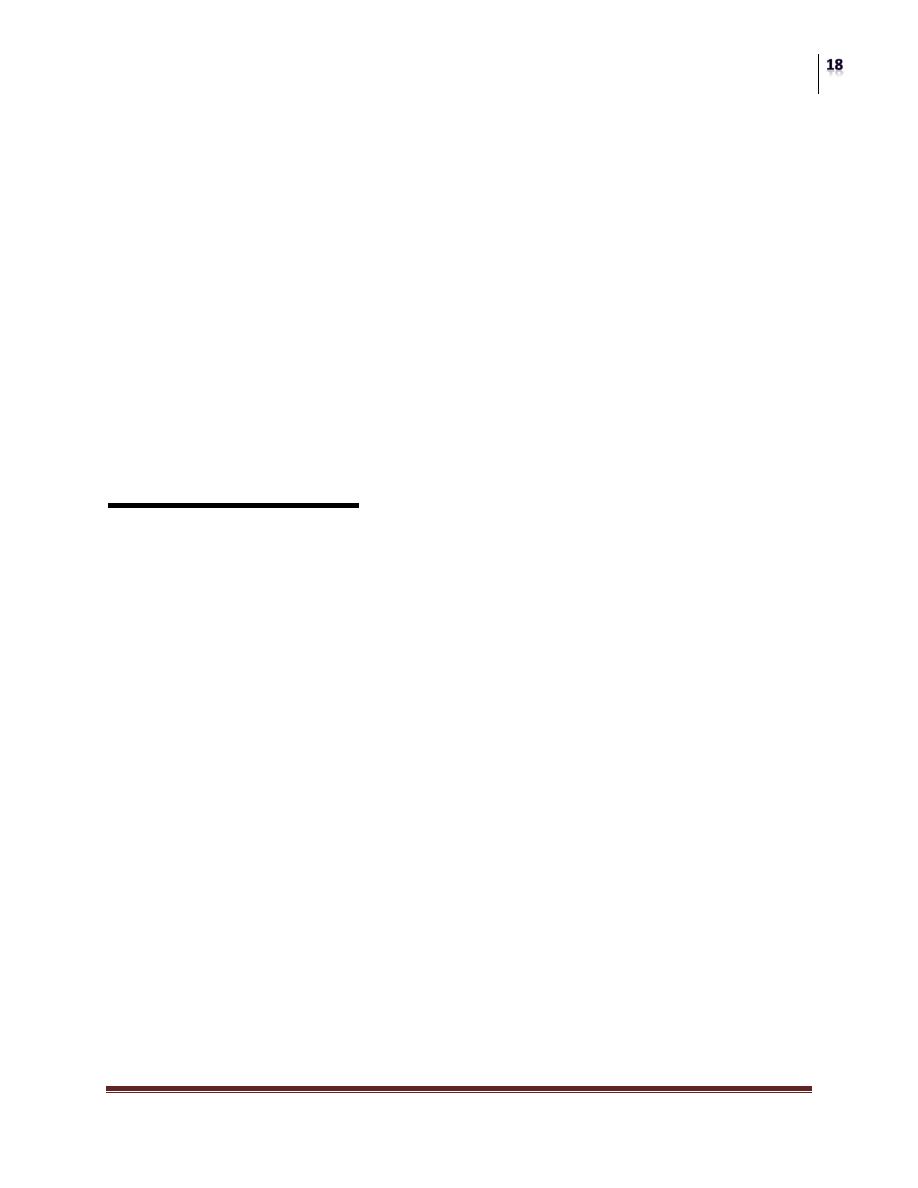
Most patients have a mass in the head of the pancreas, for which a resection of
the head of the pancreas by a pancreatoduodenectomy is appropriate.
If the duct is markedly dilated, then a longitudinal pancreatojejunostomy or
Frey procedure can be of value
The rare patient with disease limited to the tail will be cured by a distal
pancreatectomy.
Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Pancreatic fistula
This usually follows operative trauma to the gland, or may occur as a
complication of acute or chronic pancreatitis.
Management is to define the site of the fistula, the epithelial structure to which
it communicates (e.g. external to skin or internal to bowel), and to correct
metabolic and electrolyte disturbances.
The danger of a pancreatic fistula is that there is digestion of surrounding
structures by activated pancreatic enzymes causing local damage, perforation,
bleeding and digestion of the skin.
Immediate control of the fistula can be obtained by a nil by mouth regime, the
use of octreotide and adequate drainage of the fistula with protection of the
skin.
Frequently the cause is related to obstruction within the pancreatic duct which
can be overcome by the insertion of a stent or catheter endoscopically into the
pancreatic duct, and waiting for closure of the fistula while supporting the
patient by a conservative regime with parenteral nutritional support and good
nursing.
Carcinoma of the pancreas
The disease is a disease of ageing, with the average age of death in men being
74 years and that in women 79 years.
Affects men and women to the same degree.
Predisposing factors are tobacco smoking and chronic pancreatitis.
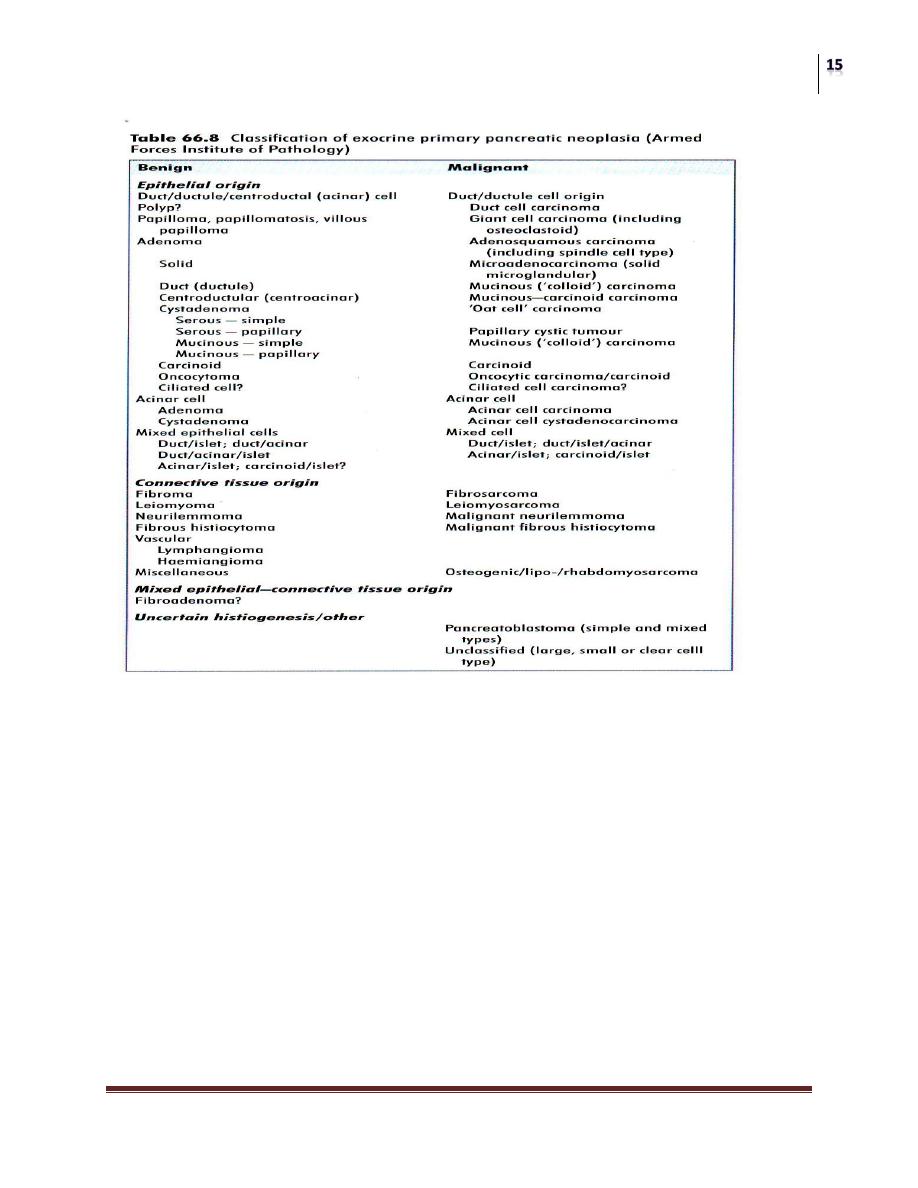
Pathology
85 per cent of cases are duct cell adenocarcinornas
Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Clinical features
The most frequent symptoms are nonspecific, namely epigastric discomfort,
anorexia and weight loss.
Jaundice is the commonest sign and symptom which brings the patient to the
attention of his or her physician. Some 85 per cent of patients present with
this symptom. It is characteristically painless jaundice but may be associated
with nausea and epigastric discomfort.
On examination there is frequently evidence of weight loss, a palpable liver,
a palpable gall bladder and even metastatic lymph nodes in the neck.
Courvoisier first drew attention to the association of an enlarged gall bladder
and a pancreatic tumor in 1890, when he stated that when the common duct

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
is obstructed by a stone dilatation is rare; when the duct is obstructed in
some other way, dilatation is common.
Other signs of intra-abdominal malignancy should be looked for with care,
such as a mass, ascites and tumor deposits in the pelvis.
Investigation
If the patient is jaundiced, the usual blood tests and ultrasound scan should be
performed. This will determine whether or not the bile duct is dilated.
If it is and there is a genuine suspicion of a tumor in the head of the pancreas,
the preferred test is now a contrast enhanced spiral CT scan specific for the
pancreas.
The next investigation is that of an endoscopic examination to determine
whether the jaundice can be relieved endoscopically.
If it can, a stent should be inserted through the stricture to relieve the jaundice.
Attention should be paid to the coagulation to ensure that no bleeding occurs
during this process.
If the ERCP shows the characteristic features of a tumor and the CT scan shows
that the tumor is small (less than 4 cm), and confined to the head of the
pancreas without evidence of distant spread or vascular invasion, then the
patient should be considered for operative intervention and their state of general
fitness assessed.
More accurate information can be obtained by endoscopic ultrasound in which
the ultrasound probe on the end of an endoscope is used to obtain images of the
tumor via the duodenum, giving good definition of the tumor and its extent.
Unfortunately, lymphadenopathy is not well shown by this technique, but itis
possible to determine with accuracy whether or not the portal vein is involved.
Management
At the time of presentation, 90—95 per cent of patients are unsuitable for
resection because of either local spread into the superior mesenteric vein, para
aortic or mesenteric lymphadenopathy, or hepatic metastases.
In some patients age precludes major operative intervention. For those patients
who are inoperable palliative treatment should be offered.
Jaundice is relieved by stenting.

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Obstruction of the duodenum occurs in approximately 15 per cent; if this occurs
early in the course of the disease surgical bypass by gastrojejunostomy is
appropriate, but if itis late in the course of the disease then the use of expanding
metal stents inserted endoscopically is preferred as many of these patients have
prolonged delayed gastric emptying following surgery.
If the patient is not a suitable candidate for endoscopic biliary stenting a
percutaneous transhepatic stent can be placed.
In younger patients who may have a better prognosis a laparotomy to assess the
tumor can be appropriate;
If the tumor is proved inoperable a choledochoduodenostomy and gastro-
jejunostomy is the preferred approach, but the simpler cholecystjejunostomy is
more frequently performed.
The disadvantage of the latter technique is that bile must drain through the
cystic duct which is narrow, and if the cystic duct is inserted low into the bile
duct it is vulnerable to occlusion by tumor growth.
Any patient who has palliative treatment should have a biopsy performed to
obtain histological verification.
If operation is undertaken this can be done at the time of the operation, but if no
operative procedure is undertaken a percutaneous trucut biopsy of the tumor
should be performed.
The role of chemotherapy in the management of pancreatic cancer remains ill
defined.
For the duct cell adenocarcinoma, 5-fluorouracil (5FU) or gemcitabine will
produce a remission in 15—25 per cent of patients, whilst the remainder will
have no benefit from the therapy.
Surgical resection
Patients with duct cell cancers which are less than 4 cm in diameter, not
involving the superior mesenteric or portal veins and with no evidence of
multiple enlarged nodes or distant spread should be considered for a resection.
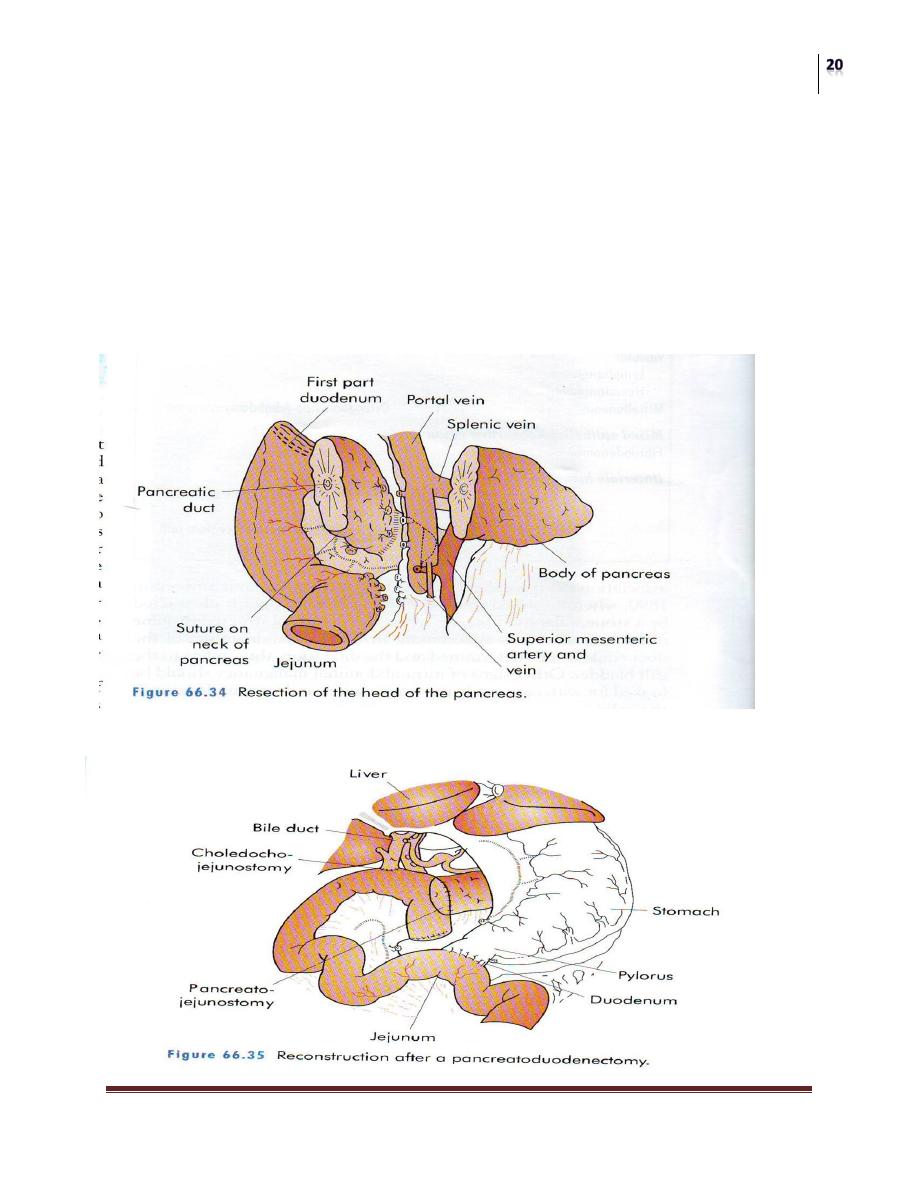
The appropriate resection is that of a pylorus-preserving
pancreatoduodenectomy with a local lymphadenectomy. (wipples procedure).
The operation can now be performed safely with a mortality of 3—5 per cent.
Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Endocrine tumors of the pancreas
Tumors of these endocrine cells comprise 1 per cent of all pancreatic tumors.
Pathology
The actual islet cell lesion may be one of the following: (1) generalised
hyperplasia; (2) discrete adenoma; (3) generalised adenomatosis; and (4)
carcinoma.
As part of the multiple endocrine neoplasia syndromes they may be associated
with tumours in other endocrine glands, especially the anterior pituitary, the
parathyroids and the adrenal cortex.
The commonest of these is the insulinoma.
Insulinoma
Clinical features
Attacks are always associated with hypoglycaemia and occur at irregular
intervals, often with progressively increasing frequency and severity.
The symptoms include epigastric discomfort, nervousness, ‘feeling unwell’,
sweating, dizziness, episodes of inarticulate speech and uncoordinated
movements and, in extreme cases, fits indistinguishable from epilepsy.
Diagnosis
Diagnosis is made by the three criteria described by Whipple which consists of
the signs and symptoms of hypoglycaemia, serum levels of less than 2.8
mmol/litre and the prompt relief of symptoms by the administration of glucose.
The hypoglycaemia should be documented and associated with inappropriate
levels of serum insulin (greater than 6 micro units/dl).
Once the diagnosis has been made, the next step is to localise the tumour.
The prime investigation is that of a high-quality CT scan of the pancreas with
rapid injection (5—7 ml/second) of intravenous contrast.
The diagnosis of the characteristic ‘blush’ noted at the site of the tumour can be
confirmed by endoscopic ultrasound.

Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Treatment
The only curative treatment is EXCISION of the tumor.
Appropriate intravenous therapy with glucose and insulin is started
preoperatively to maintain the blood sugar between 5 and 8 mmol/litre.
The tumor is located usually with ease. Occasionally, the tumor cannot be
palpated and then intraoperative ultrasound will invariably localise the tumor if
present. Enucleation is the procedure of choice.
Resection is rarely necessary unless the tumor is adjacent to the main duct in
the head of the pancreas or there are multiple tumors in close proximity.
The operative mortality rate is 1 per cent and the symptoms should be relieved
in more than 95per cent of patients.
Zollinger—Ellison syndrome
The diagnosis should be suspected when peptic ulcer disease occurs at a very
young age, there is virulent peptic ulcer disease, peptic ulcer disease occurs in
unusual sites such as the jejunum, there is a marginal ulcer, unexplained
diarrhoea, coexistent parathyroid disease or a family history of endocrinopathy.
The diagnosis of Zollinger—Ellison syndrome is confirmed by the
demonstration of hypergastrinaemia and concurrent gastric hyperacidity.
Location and localization
In 1984 Stabile et a!. described the ‘gastrinoma triangle’ (confluence of the
cystic duct and common bile duct superiorly, junction of the second and third
parts of the duodenum inferiorly, and the junction of the neck and body of the
pancreas medially) and suggested that 80—90 per cent of gastrinomas would be
found within this triangle. This is, indeed, the case.
A high percentage of tumors will be found in the duodenal wall and these are
often quite small (4—6 mm).
As 50—60 per cent of patients with the Zollinger—Ellison syndrome have
malignant tumors careful investigation should be performed preoperatively to
exclude metastatic disease.
If there is no metastatic disease exploration should be undertaken.
Surgery
Pancreas
Dr. Muayad Abass Fadhel
Lec. 20
Treatment
If the tumour is localised then resection of the tumour should be undertaken.
Unfortunately, the surgical cure rate is only 30 per cent.
Nevertheless, if a single tumour is found and excised the patient is cured.
If other problems coexist, the patient can be managed medically with
omeprazole and octreotide.
Total gastrectomy is advised only if medical therapy fails.
