Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
INTRA-ABDOMINAL infections result in two major manifestations..
1-early or diffuse infection result in localized or generalized peritonitis.
2-late and localized infection produces. Intra-abdominal and pelvic abscesses.
Learning Objectives
To recognize and understand:
* The clinical features of localized and generalized peritonitis.
* The common causes and complications of peritonitis.
* The principles of surgical management in patients with peritonitis.
* The clinical presentations and treatment of abdominal/pelvic abscesses.
* The clinical presentations of tuberculosis peritonitis.
The Peritoneum:
The peritoneal membrane is conveniently divided into two parts – the visceral
peritoneum surrounding the viscera and the parietal peritoneum lining the other
surfaces of the cavity. The peritoneum had a number of functions.
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Summary box .
Functions of the peritoneum
• Pain perception (parietal peritoneum).
• Visceral lubrication.
• Fluid and particulate absorption.
• Inflammatory and immune responses.
• Fibrinolytic activity.
The parietal portion is richly supplied with nerves and, when irritated, causes
severe pain accurately localized to the affected area. The visceral peritoneum, in
contrast, is poorly supplied with nerves and its irritation causes vague pain that is
usually located to the midline.
The peritoneal cavity is the largest cavity in the body, the surface area of its lining
membrane (2m2 in an adult) being nearly equal to that of the skin. The peritoneal
membrane is composed of flattened polyhedral cells (mesothelium), one layer
thick, resting upon a thin layer of fibroblastic tissue. Beneath the peritoneum,
supported by a small amount of areola tissue, lies a network of lymphatic vessels
and rich plexuses of capillary blood vessels from which all absorption and
exudation must occur. In health, only a few milliliters of peritoneal fluid is found
in the peritoneal cavity. The fluid is pale yellow, somewhat viscid and contains
lymphocytes and other leucocytes; it lubricates the viscera, allowing easy
movement and peristalsis.
In the peritonea space, mobile gas-filled structures float upwards, as does free air
(„gas‟). In the erect position, when free fluid is present in the peritoneal cavity,
pressure is reduced in the upper abdomen compared with the lower abdomen.
When air is introduced, it rises, allowing all of the abdominal contents to sink.
During expiration, intra-abdominal pressure is reduced and peritoneal fluid, aided
by capillary attraction, travels in an upward direction towards the diaphragm.
Experimental evidence shows that particulate matter and bacteria are absorbed
within a few minutes into the lymphatic network through a number of „pores‟
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
within the diaphragmatic peritoneum. This upward movement of peritoneal fluids
is responsible for the occurrence of many subphrenic abscesses.
The peritoneum has the capacity to absorb large volumes of fluid: this ability is
used during peritoneal dialysis in the treatment of renal failure. But the peritoneum
can also produce an inflammatory exudates when injured.
Summary box .
CAUSES OF PERITONIAL INFLAMMATORY EXUDATE..
• Bacterial infection, e.g. appendicitis, tuberculosis.
• Chemical injury, e.g. bile peritonitis.
• Ischemic injury e.g. strangulated bowel, vascular occlusion.
• Direct trauma, e.g. operation.
• Allergic reaction, e.g. starch peritonitis.
When a visceral perforation occurs, the free fluid that spills into the peritoneal
cavity runs downwards, largely directed by the normal peritoneal attachments. For
example, spillage from a perforated duodenal ulcer may run down the right
parabolic gutter.
When parietal peritoneal defects are created, healing occurs not from the edges but
by the development of new mesothelial cells throughout the surface of the defect.
In this way, large defects heal as rapidly as small defects.
Acute Peritonitis
Most cases of peritonitis are caused by an invasion of the peritoneal cavity by
bacteria, so that when the term “peritonitis” is used without qualification,
bacterial peritonitis is implied. Bacterial peritonitis is usually polymicrobial, both
aerobic and anaerobic organisms being present. The exception is primary
peritonitis (“spontaneous” peritonitis), in which a pure infection with
streptococcal, pneumococcal or Haemophilus bacteria occurs.

Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Bacteriology
Bacteria from the gastrointestinal tract
The number of bacteria within the lumen of the gastrointestinal tract is normally
low until the distal small bowel is reached, whereas high concentrations are found
in the colon. However, disease (e.g. obstruction, achlorhydria, diverticulitis) may
increase proximal colonization. The biliary and pancreatic tracts are normally free
from bacteria, although they may be infected in disease, e.g. gallstones. Peritoneal
infection is usually caused by two or more bacterial strains. Gram-negative
bacteria contain end toxins (lip polysaccharides) in their cell walls that have
multiple toxic effects on the host, primarily by causing the release of tumor
necrosis factor (TNF) from host leucocytes. Systemic absorption of end toxin may
produce end toxic shock with hypotension and impaired tissue perfusion. Other
bacteria such as Clostridium wheelchair produce harmful serotoxins.
Bactericides are commonly found in peritonitis. These Gram-negative, non-sporing
organisms, although predominant in the lower intestine, often escape detection
because they are strictly anaerobic and slow to growth on culture media unless
there is an adequate carbon dioxide tension in the anaerobic apparatus (Gillespie).
In many laboratories, the culture is discarded if there is no growth in 48 hours.
These organisms are resistant to penicillin and streptomycin but sensitive to
metronidazole, clindamycin, lincomycin and cephalosporin compounds. Since the
widespread use of metronidazole (Flagyl), Bacteroides infections have greatly
diminished.
Non- gastrointestinal caused of peritonitis
Pelvic infection via the fallopian tubes is responsible for a high proportion of “non-
gastrointestinal” infections.
Immunodeficient patients, for example those with human immunodeficiency virus
(HIV) infection or those on immunosuppressive treatment, may present with
opportunistic peritoneal infection, e.g. Mycobacterium avium – intracellulare
(MAI).
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Mycobacterium avium – intracellulare (MAI)
(Summary box 58.3).
Summary box .
Bacteria in peritonitis
1-Gastrointestinal source
• Escherichia coli
• Streptococci (aerobic and anaerobic)
• Bacteroides
• Clostridium
• Klebsiella pneumonia
• Staphylococcus
2-Other sources
• Chlamydia
• Gonococcus
• β-Haemolytic streptococci
• Pneumococcus
• Mycobacterium tuberculosis
Route of infection
Infecting organisms may reach the peritoneal cavity via a number of routes
Summary Box.
Paths to peritoneal infection
• Gastrointestinal perforation, e.g. perforated ulcer, diverticular perforation.
• Exogenous contamination, e.g. drains, open surgery, trauma.
• Transmural bacterial translocation (no perforation), e.g. inflammatory bowel
disease, appendicitis, ischaemic bowel.
• Female genital tract infection, e.g. pelvic inflammatory disease.
• Haematogenous spread (rare), e.g. septicaemia.
Even in patients with non-bacterial peritonitis (e.g. acute pancreatitis,
intrapertioneal rupture of the bladder or haemoperitoneum), the peritoneum ofter
becomes infected by transmural spread of organisms from the bowel, and it is not
long (often a matter of hours) before a bacterial peritonitis develops. Most and
many gastric perforations are also sterile at first; intestinal perforations are

Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
usually infected from the beginning. The proportion of anaerobic to aerobic
organisms increase with passage of time. Mortality reflects:
• The degree and duration of peritoneal contamination;
• The age of the patient
• The general health of the patient;
• The nature of the underlying cause.
Localised peritonitis
Anatomical, pathological and surgical factors may favour the localization of
peritonitis.
Anatomical
The greater sac of the peritoneum is divided into (1) the subphrenic, spaces (2) the
pelvis and (3) the peritoneal cavity proper. The last is divided into a supracolic and
an infrasonic compartment by the transverse colon and transverse mescaline, which
deters the spread of infection from one to the other. When the supracolic
compartment overflows, as is often the case when a peptic ulcer perforates, it does
so over the colon into the infrasonic compartment or by way of the right parabolic
gutter to the right iliac fosse and hence to the pelvis.
Pathological
The clinical course is determined in part by the manner in which adhesions form
around the affected organ. Inflamed peritoneum loses its glistening appearance and
becomes reddened and velvety. Flakes of fibrin appear and cause loops of intestine
to become adherent to one another and to the parietals. There is an outpouring of
serous inflammatory exudates rich in leucocytes and plasma proteins that soon
becomes turbid; if localization occurs, the turbid fluid becomes frank pus.
Peristalsis is retarded in affected bowel and this helps to prevent distribution of the
infection. The greater momentum, by enveloping and becoming adherent to
inflamed structures, often forms a substantial barrier to the spread of infection.
Surgical
Drains are frequently placed during operation to assist localization (and exit) of
intra-abdominal collections: their value is disputed. They may act as conduits for
exogenous infection.
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Diffuse peritonitis
A number of factors may favor the development of diffuce peritonitis:
• Speed of peritoneal contamination is a prime factor. If an inflamed appendix . or
other hollow viscus perforates before localization has taken place, there is a gush
of contents into the peritoneal cavity, which may spread over a large area almost
instantaneously. Perforation proximal to an obstruction or from sudden
anastomotic separation is associated with severe generalised peritonitis and a high
mortality rate.
• Stimulation of peristalsis by the ingestion of food or even water hinders
localisation. Violent peristalsis occasioned by the administration of a purgative or
an enema may cause the widespread distribution of an infection that would
otherwise have remained localised.
• The virulence of the infecting organism may be so great as to render the
localisation of infection difficult or impossible.
• Young children have a small omentum, which is less effective in localizing
infection.
• Disruption of localised collections may occur with injudicious handling, e.g.
appendix mass or pericolic abscess.
• Deficient natural resistance (“immune deficiency “) may result from use of drugs
(e.g. steroids), disease {e.g. acquired immune deficiency syndrome (ADIS)} or old
age.
Clinical features
Localised peritonitis
Localised peritonitis is bound up intimately with the causative condition, and the
initial symptoms and signs are those of that condition. When the peritoneum
becomes inflamed, the temperature, and especially the pulse rate, rise. Abdominal
pain increase and usually there is associated vomiting. The most important sign is
guarding and rigidity of the abdominal wall over the area of the abdomen that is
involved, with a positive ”release” sign (rebound tenderness). If inflammation
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
arises under the diaphragm, shoulder tip (“phernic”) pain may be felt. In cases of
pelvic peritonitis arising from an inflamed appendix in the pelvic position or from
salpingitis, the abdominal signs are often slight; there may be deep tenderness of
one or both lower quadrants alone, but a rectal or vaginal examination reveals
marked tenderness of the pelvic peritoneum. With appropriate treatment, localised
peritonitis usually resolves; in about 20% of cases, an abscess follows.
Infrequently, localised peritonitis becomes diffuse. Conversely, in favourable
circumstances, diffuse peritonitis can become localised, most frequently in the
pelvis or at multiple sites within the abdominal cavity.
Diffuse (generalised) peritonitis
Diffuse (generalised) peritonitis may present in differing ways dependent on the
duration of infection.
Early
Abdominal pain is severe and made worse by moving or breathing. It is first
experienced at the site of the original lesion and spreads outwards from this point.
Vomiting may occur. The patient usually lies still. Tenderness and rigidity on
palpation are found typically when the peritonitis affects the anterior abdominal
wall. Abdominal tenderness and rigidity are diminished or absent if the anterior
wall is unaffected, as in pelvic peritonitis or, rarely, peritonitis in the lesser sac.
Patients with pelvic peritonitis may complain of urinary symptoms; they are tender
on rectal or vaginal examination. Infrequent bowel sounds may still be heard for a
few hours but they cease with the onset of paralytic ileus. The pluse rises
progressively but, if the peritoneum is deluged with irritant fluid, there is a sudden
rise. The temperature changes are variable and can be subnormal.
Late
If resolution or localisation of generalised peritonitis does not occur, the abdomen
remains silent and increasingly distends.
Circulatory failure ensues, with cold, clammy extremities, sunken eyes, dry tongue,
thread (irregular) pulse and drawn and anxious face (Hippocratic fancies; The
patient finally lapses into unconsciousness. With early diagnosis and adequate
treatment, this condition is rarely seen in modern surgical practice.
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Summary box .
Clinical features in peritonitis
• Abdominal pain, worse on movement.
• Guarding/rigidity of abdominal wall.
•Pain/tenderness on rectal/ vaginal examination (pelvic peritonitis).
• Pyrexia (may be absent).
• Raised pulse rate.
• Absent or reduced bowel sounds.
• “Septic shock” {systemic inflammatory response syndrome (SIRS) in later
stages.
Diagnostic aids
Investigations may elucidate a doubtful diagnosis, but the importance of a careful
history and repeated examination must not be forgotten.
• A radiograph of the abdomen may confirm the presence of dilated gas-filled
loops of bowel (consistent with a paralytic ileus) or show free gas, although the
latter is best shown on an erect chest radiograph. If the patient is too ill for an
“erect” film to demonstrate free air under the diaphragm, a lateral decubitus film is
just as useful, showing gas beneath the abdominal wall.
• Serum amylase estimation may establish the diagnosis of acute pancreatitis
provided that it is remembered that moderately raised values are frequently found
following other abdominal catastrophes and operations, e.g. perforated duodenal
ulcer.
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
• Ultrasound and computerized tomography (CT) scanning are increasingly used to
identify the cause of peritonitis Such knowledge may influence management
decisions
• Peritoneal diagnostic aspiration may be helpful but is usually unnecessary. Bile-
stained fluid indicates a perforated peptic ulcer or gall bladder; the presence of pus
indicates bacterial peritonitis. Blood is aspirated in a high proportion of patients
with intraperitoneal bleeding.
Summary box.
Investigations in peritonitis
• Raised white cell count and C-reactive protein are usual.
• Serum amylase >4x normal indicates acute pancreatitis.
• Abdominal radiographs are occasionally helpful.
• Erect chest radiographs may show free peritoneal gas (perforated viscus).
• Ultrasound/CT scanning often diagnostic.
• Peritoneal fluid aspiration (with or without ultrasound guidance) may be helpful.
Treatment
In case of doubt, early surgical intervention is to be preferred to a “wait and see”
policy. This rule is particularly true for previously healthy patients and those with
postoperative peritonitis. Caution is required in patients at high operative risk
because of co morbidity or advanced age.
Treatment consists of:
A- General care of the patient;
B- Specific treatment of the cause;
C- Peritoneal lavage when appropriate.
A-General care of the patient
1- Correction of circulating volume and electrolyte imbalance.
Patients are frequently hypovolaemic with electrolyte disturbances. The plasma
volume must be restored and electrolyte concentrations corrected. Central venous
catheterization and pressure monitoring may be helpful, particularly in patients
with concurrent disease. Plasma protein depletion may also need correction as the

Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
inflamed peritoneum leaks large amounts of protein. If the patient‟s recovery is
delayed for more than 7-10 days, intravenous nutrition is required.
2- Gastrointestinal decompression
A nasogastric tube is passed into the stomach and aspirated. Intermittent aspiration
is maintained until the parplytic ileus has resolved. Measured volumes of water are
allowed by mouth when only small amounts are being aspirated. If the abdomen is
soft and not tender, and bowel sounds return, oral feeding may be progressively
introduced. It is important not to prolong the ileus by missing this stage.
3- Antibiotic therapy
Administration of antibiotics prevents the multiplication of bacteria and the release
of endotoxins. As the infection is usually a mixed one, initial treatment with
parenteral broad-spectrum antibiotics active against aerobic and anaerobic bacteria
should be given.
4- Correction of fluid loss
A fluid balance chart must be started so that daily output by gastric aspiration and
urine is known. Additional losses from the lungs, skin and in faces are estimated,
so that the intake requirements can be calculated and seen to have been
administered. Throughout recovery, the haematocrit and serum electrolytes and
urea must be checked regularly.
5- Analgesia
The patient should be nursed in the sitting-up position and must be relieved of pain
before and after operation. If appropriate expertise is available, epidural infusion
may provide excellent analgesia. Freedom from pain allows early mobilization and
adequate physiotherapy in the postoperative period, which help to prevent basal
pulmonary collapse, deep vein thrombosis and pulmonary embolism.
6- Vital system support
Special measures may be needed for cardiac, pulmonary and renal support,
especially if septic shock is present.
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
B-Specific treatment of the cause
If the cause of peritonitis is amenable to surgery, operation must be carried out as
soon as the patient is fit for anaesthesia. This is usually within a few hours. In
peritonitis caused by pancreatitis or salpingitis, or in cases of primary peritonitis of
streptococcal or pneumococcal origin, non-operative treatment is preferred
provided the diagnosis can be made with confidence.
C-Peritoneal lavage
In operations for general peritonitis it is essential that, after the cause has been
dealt with, the whole peritoneal cavity is explored with the sucker and, if
necessary, mopped dry until all seropurulent exudates is removed. The use of a
large volume of saline (1-2 litters) containing dissolved antibiotic (e.g.
tetracycline) has been shown to be effective (Matheson) .
Summary box.
Management of peritonitis
General care of patient:
• Correction of fluid and electrolyte imbalance.
• Insertion of nasogastric drainage tube.
• Broad – spectrum antibiotic therapy.
• Analgesia.
• Vital system support.
Operative treatment of cause when appropriate with peritoneal debridement/lavage.
Prognosis and complications
With modern treatment, diffuse peritonitis carries a mortality rate of about 10%.
The systemic and local complications are shown in Summary boxes.
Summary boxes .
Systemic complications of peritonitis
• Bacteraemic/endotoxic shock.
• Bronchopneumonia/ respiratory failure.
• Renal failure.
• Bone marrow suppression.
• Multisystem failure.
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Summary boxes .
Abdominal complications of peritonitis
• Adhesional small bowel obstruction.
• Paralytic ileus.
• Residual or recurrent abscess.
• Portal pyaemia/liver abscess.
Acute intestinal abstruction due to peritoneal adhesions
The usually gives central colicky abdominal pain with evidence of small bowel gas
and fluid levels sometimes confined to the proximal intestine on radiography.
Bowel sounds are increased. It is more common with localised peritonitis. It is
essential to distinguish this from paralytic ileus.
Paralytic ileus
There is usually little pain, and gas-filled loops with fluid levels are seen
distributed throughout the small and large intestine on abdominal imaging. In
paralytic ileus, bowel sounds are reduced or absent.
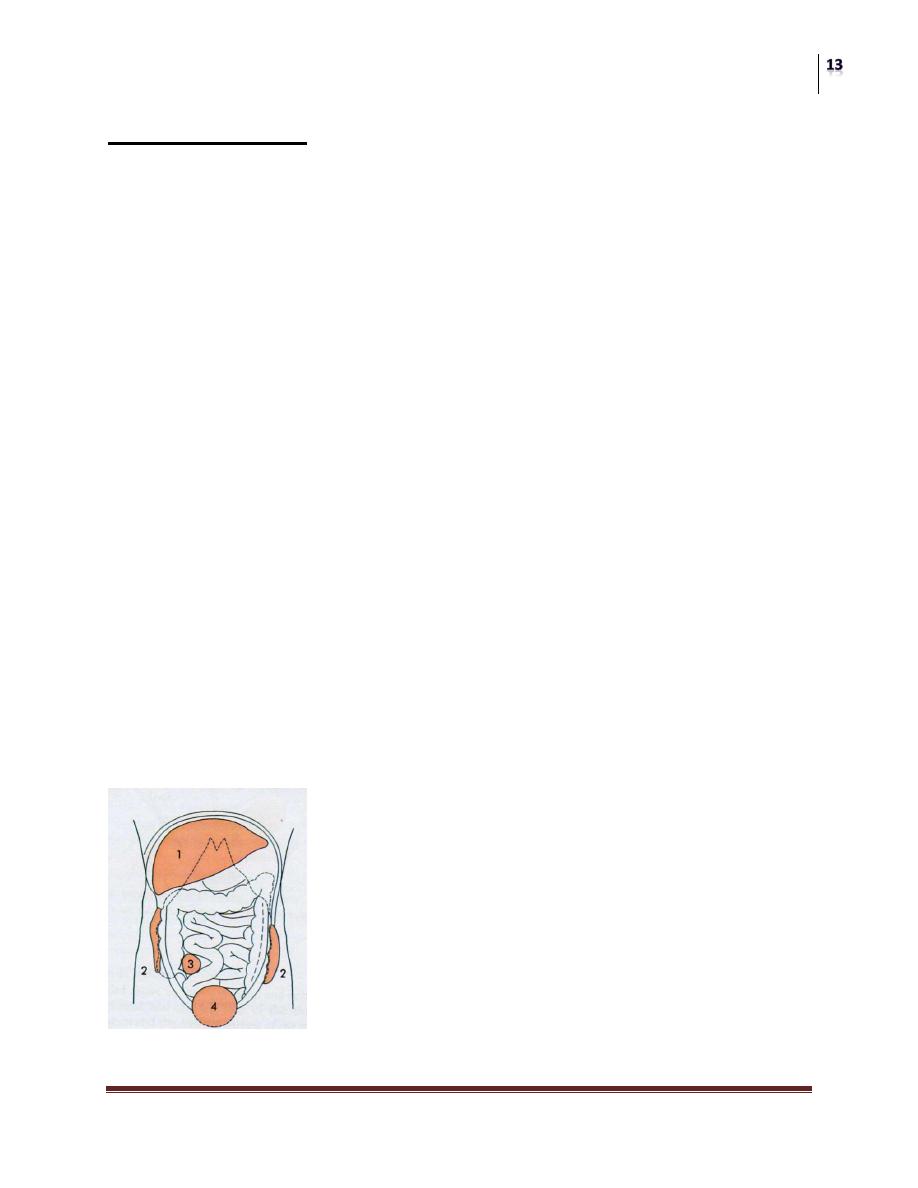
Abdominal and pelvic abscesses
Abscess formation following local or diffuse peritonitis usually accupies one of the
situations shown in The symptoms and signs of a purulent collection may be vague
and consist of nothing more than lassitude, anorexia and malaise; pyrexia (often
low – grade), tachycardia, leucocytosis, raised C-reactive protein and localised
tenderness are also common
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Summary box .
Clinical features of an abdominal/pelvic abscess
• Malaise
• Sweats with or without rigors.
• Abdominal/pelvic (with or without shoulders tip) pain.
• Anorexia and weight loss.
• Symptoms from local irritation, e.g. hiccoughs (subphrenic), diarrhea and mucus
(pelvic).
• Swinging pyrexia.
• Localised abdominal tenderness/mass.
Later, a palpable mass may develop that should be monitored by marking out its
limits on the abdominal wall and meticulous daily examination. More commonly,
its course is monitored by repeat ultrasound or CT scanning. In most cases, with
the aid of antibiotic treatment, the abscess or mass gradually reduces in size until,
finally, it is undetectable. In others, the abscess fails to resolve or becomes larger,
in which event it must be drained. In many situations, by waiting for a few days the
abscess becomes adherent to the abdominal wall, so that it can be drained without
opening the general peritoneal cavity. If facilities are available, ultrasound or CT
guided drainage may avoid further operation. Open drainage of an intraperitoneal
collection should be carried out by cautious blunt finger exploration to minimize
the risk of an intestinal fistula.
Pelvic abscess
The pelvis is the commonest site of an intraperitoneal abscess because the
vermiform appendix is often pelvic in position and the fallopian tubes are frequent
sites of infection. A pelvic abscess can also occur as a sequel to any case of diffuse
peritonitis and is common after anastomostic leakage following colorectal surgery.
The most characteristic symptoms are diarrhea and the passage of mucus in the
stools. Rectal examination reveals a bulging of the anterior rectal wall, which,
when the abscess is ripe, becomes softly cystic. Left to nature, a proportion of
these abscesses burst into the rectum, after which the patient nearly always
recovers rapidly. If this does not occur, the abscess is definitely pointing into the
rectum, rectal drainage (Fig. 58.6) is employed. If any uncertainty exists, the
presence of pus should be confirmed by ultrasound or CT scanning with needle
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
aspiration if indicated. Laparotomy is almost never necessary. Rectal drainage of a
pelvic abscess is far preferable to suprapubic drainage, which risks exposing the
general peritoneal cavity to infection. Drainage tubes can also be inserted
percutaneously or via the vagina or rectum under ultrasound or CT guidance .
Intraperitoneal abscess
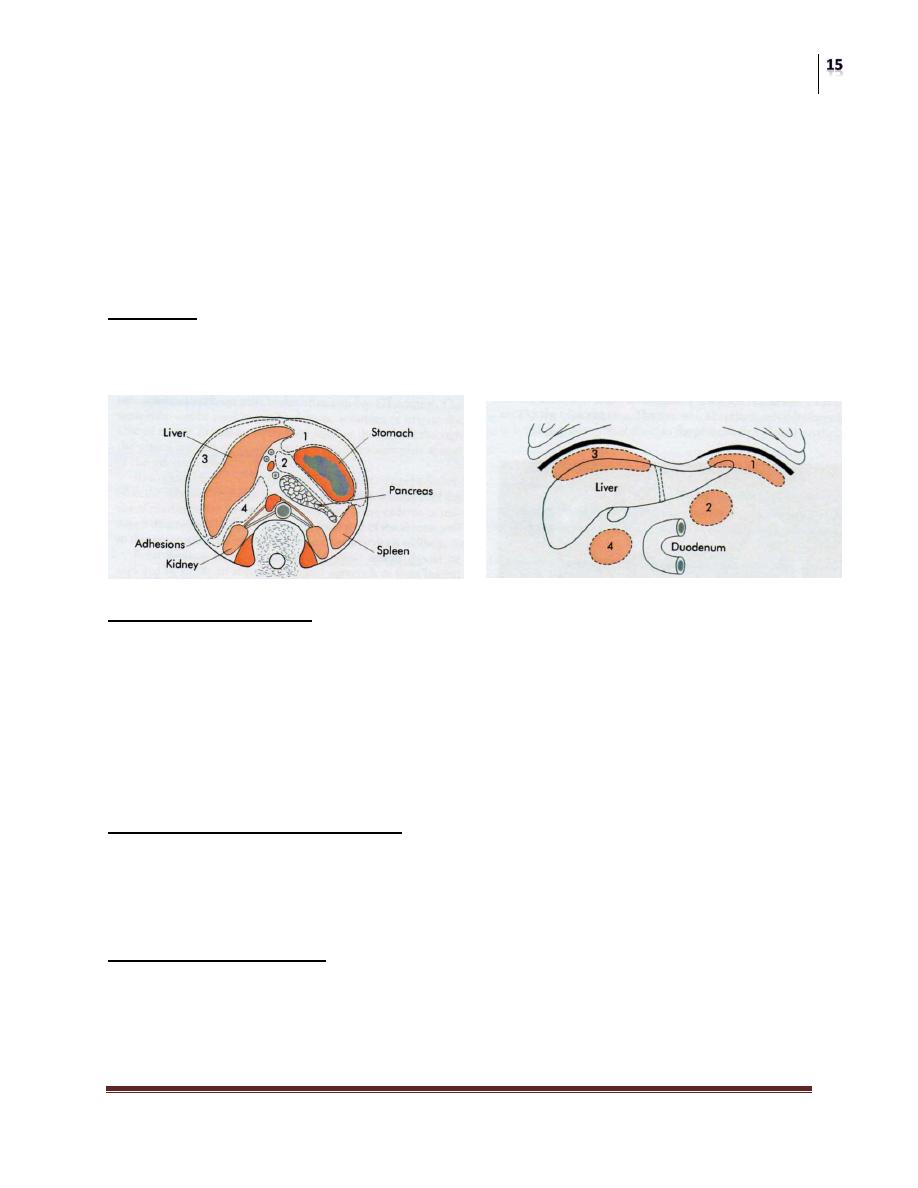
Anatomy
The complicated arrangement of the peritoneum results in the formation of four
intraperitoneal spaces in which pus may collect
Left subphrenic space
This is bound above by the diaphragm and behind by the left triangular ligament
and the left lobe of the liver, the gastrohepatic omentum and the anterior surface of
the stomach. To the right is the falciform ligament and to the left the spleen,
gastosplenic omentum and diaphragm. The common cause of an abscess here is an
operation on the stomach, the tail of the pancreas, the spleen or the splenic flexure
of the colon.
Left subhepatic space/lesser sac
The commonest cause of infection here is complicated acute pancreatitis. In
practice, a perforated gastric ulcer rarely causes a collection here because the
potential space is obliterated by adhesions.
Right subphrenic space
This space lies between the right lobe of the liver and the diaphragm. It is limited
posteriorly by the anterior layer of the coronary and the right triangular ligaments
and to the left by the falciform ligament. Common causes of abscess here are
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
perforating cholecystitis, a perforated duodenal ulcer, a duodenal cap “blow-out”
following gastrectomy and appendicitis.
Right subhepatic space
This lies transversely beneath the right lobe of the liver in Rutherford Morison‟s
pouch. It is bounded on the right by the right lobe of the liver and the diaphragm.
To the left is situated the foramen of Winslow and below this lies the duodenum.
In front are the liver and the gall bladder and behind are the upper part of the right
kidney and the diaphragm. The space is bounded above by the liver and below by
the transverse colon and hepatic flexure. It is the deepest space of the four and the
commonest site of a subphrenic abscess, which usually arises from appendicitis,
cholecystitis, a perforated duodenal ulcer or following upper abdominal surgery.
Clinical features
The symptoms and signs of subphrenic infection are frequently non-specific and it
is well to remember the aphorism, “pus somewhere, pus nowhere else, under the
diaphragm”.
Symptoms
A common history is that, when some infective focus in the abdominal cavity has
been dealt with, the condition of the patient improves temporarily but, after an
interval of a few days or weeks, symptoms of toxaemia reappear. The condition of
the patient steadily, and often rapidly, deteriorates. Sweating, wasting and
anorexia are present. There is sometimes epigastric fullness and pain, or pain in the
shoulder on the affected side, because of irritation of sensory fibres in the phrenic
nerve, referred along the descending branches of the cervical plexus. Persistent
hiccoughs may be a presenting symptom.
Signs
A swinging pyrexia is usually present. If the abscess is anterior, abdominal
examination will reveal some tenderness, rigidity or even a palpable swelling.
Sometimes the liver is displaced downwards but more often it is fixed by
adhesions. Examination of the chest is important and, in the majority of cases,
collapse of the lung or evidence of basal effusion or even an empyema is found.

Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Investigations
A number of the following investigations may be helpful:
• Blood tests usually show a leucocytosis and raised C-reactive protein.
• A plain radiograph sometimes demonstrates the presence of gas or a pleural
effusion. On screening, the diaphragm is often seen to be elevated (so called
“tented” diaphragm) and its movements impaired.
• Ultrasound or CT scanning is the investingation of choice and permits early
detection of subphrenic collections
• Radiolabelled white cell scanning may occasionally prove helpful when other
imaging techniques have failed.
Differential diagnosis
Pyelonephritis, amoebic abscess, pulmonary collapse and pleural empyema may
give rise to diagnostic difficulty.
Treatment
The clinical course of suspected case is monitored, and blood tests and imaging
investigations are carried out at suitable intervals. If suppuration seems probable,
intervention is indicated. If skilled help is available it is usually possible to insert a
percutaneous drainage tube under ultrasound or CT control. The same tube can be
used to instill antibiotic solutions or irrigate the abscess cavity. To pass an
aspirating needle at the bedside through the pleura and diaphragm invites
potentially catastrophic spread of the infection into the pleural cavity.
If an operative approach is necessary and a swelling can be detected in the
subcostal region or in the loin, an incision is made over the site of masimum
tenderness or over any area where oedema or reness is discovered. The parietes
usually form part of the abscess wall so that contamination of the general
peritoneal cavity is unlikely.
If no swelling is apparent, the subphrenic spaces should be explored by either an
anterior subcostal approach or from behind after removal of the outer part of the
12th rib according to the position of the abscess on imaging. When the posterior
approach, the pleura must not be opened and, after the fibers of the diaphragm
have been separated, a finger is inserted beneath the diaphragm so as to explore the
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
adjacent area. The aim with all techniques of drainage is to avoid dissemination of
pus into the peritoneal or pleural cavities.
When the cavity is reached, all of the fibrinous loculi must be broken down with
the finger and one or two drainage tubes must be fully inserted. These drains are
withdrawn gradually during the next 10 days and the closure of the cavity is
checked by sonograms or scanning. Appropriate antibiotics are also given.
Special forms of peritonitis
Postoperative
The patient is ill with raised pulse and peripheral circulatory failure. Following an
anastigmatic dehiscence, the general condition of a patient is usually more serious
than if the patient had suffered leakage from a perforated peptic ulcer with no
preceding operation. Local symptoms and signs are less definite. Abdominal pain
may not be prominent and is often difficult to assess because of normal wound
pain and postoperative analgesia. The patient‟s deterioration may be attributed
wrongly to cardiopulmonary collapse, which is usually concomitant.
Peritonitis follows abdominal operations more frequently than is realized. The
principles of treatment do not differ from those of peritonitis of other origin.
Antibiotic therapy alone is inadequate; no antibiotic can stay the onslaught of
bacterial peritonitis caused by leakage from a suture line, which must be dealt with
by operation.
In patients on treatment with steroids
Pain is frequently slight or absent. Physical signs similarly vague and misleading.
In children
The diagnosis can be more diffuclt, particularly in the preschool child. Physical
signs should be elicited by a gentle, patient and sympathetic approach.
In patients with dementia
Such patients can be fractious and unable to give a reliable history. Abdominal
tenderness is usually well localised, but guarding and rigidity are less marked
because the abdominal muscles are often thin and weak.
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Bile peritonitis
Unless there is reason to suspect that the biliary tract was damaged during
operation, it is improbable that bile as a cause of peritonitis will be thought of until
the abdomen has been opened. The common causes of bile peritonitis are shown in
Summary box.
Summary box .
Causes of bile peritonitis
• Perforated cholecysitits.
• Post cholecystectomy:
Cystic duct stump leakage
Leakage from an accessory duct in the gall bladder bed Bile duct injury
T-tube drain dislodgement (or tract rupture on removal)
• Following other operations/ procedures:
Leaking duodenal stump post gastrectomy
Leaking biliary – enteric anastomosis
Leakage around percutaneous placed biliary drains
• Following liver trauma
Unless the bile has extravasated slowly and the collection becomes shut off from
the general peritoneal cavity, there are signs of diffuse peritonitis. After a few
hours a tinge of jaundice is not unusual. Laparotomy (or laparoscopy) should be
undertaken with evacuation of the bile and peritoneal lavage. The source of bile
leakage should be identified. A leaking gall bladder is excised or a cystic duct
ligated. An injury to the bile duct may simply be drained or alternatively intubated;
later, reconstructive operation is often required. Infected bile is more lethal than
sterile bile. A “blown” duodenal stump should be drained as it is too oedematous to
repair, but sometimes it can be covered by a jejunal patch. The patient is often
jaundiced from absorption of peritoneal bile, but the surgeon must ensure that the
abdomen is not closed until any obstruction to a major bile duct has been either
excluded or relieved. Bile leaks after cholecystectomy or liver trauma may be dealt
with by percutaneous (ultrasound – guided) drainage and endoscopic biliary
stenting to reduce bile duct pressure. The drain is removed when dry and the stent
at 4-6 weeks.
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Meconium peritonitis
Pneumococcal peritonitis
Primary pneumococcal peritonitis may complicate nephritic syndrome or cirrhosis
in children. Otherwise healthy children, particularly girls between 3 and 9 years of
age, may also be affected, and it is likely that the route of infection is sometimes
via the vagina and fallopian tubes. At other times, and always in males, the
infection is blood-borne and secondary to respiratory tract or middle ear disease.
The prevalence of pneumococcal peritonitis has declined greatly and the condition
is now rare.
Clinical features
The onset is sudden and the earliest symptom is pain localised to the lower half of
the abdomen. The temperature is raised to 39 0 C or more and there is usually
frequent vomiting. After 24-48 hours, profuse diarrhoea is characteristic. There is
usually increased frequency of micturition. The last two symptoms are caused by
severe pelvic peritonitis. On examination, abdominal rigidity is usually bilateral
but is less than in most cases of acute appendicitis with peritonitis.
Differential diagnosis
A leucocytosis of 30 000µ 1-1 (30 X 109 1-1) or more with approximately 90%
polymorphs suggests pneumococcal peritonitis rather than appendicitis. Even so, it
is often impossible to exclude perforated appendicitis. The other condition that can
be difficult to differentiate from primary pneumococcal peritonitis in its early stage
is basal pneumonia. An unduly high respiratory rate and the absence of abdominal
rigidity are the most important signs supporting the diagnosis of pneumonia, which
is usually confirmed by a chest radiograph.
Treatment
After starting antibiotic therapy and correcting dehydration and electrolyte
imbalance, early surgery is required unless spontaneous infection of pre-existing
ascites is strongly suspected, in which case a diagnostic peritoneal tap is useful.
Laparotomy or laparoscopy may be used. Should the exudates be odourless and
sticky, the diagnosis of pneumococcal peritonitis practically certain, but it is
essential to careful exploration to exclude other pathology. Assuming that no other

Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
cause for the peritonitis is discovered, some of the exudates is aspirated and sent to
the laboratory for microscopy, culture and sensitivity tests. Thorough peritoneal
lavage is carried out and the incision closed. Antibiotic and fluid replacement
therapy are continued. Nasogastric suction drainage is essential. Recovery is usual.
Other organisms are known to cause some cases of primary pneumococcal
peritonitis, the peritoneal in children, including Haemophilus, other streptococci
and a few Gram – negative bacteria. Underlying pathology ( including an
intravaginal foreign body in girls) must always be excluded before primary
peritonitis can be diagnosed with certainty.
Idiopathic streptococcal and staphylococcal peritonitis in adults
Idiopathic streptococcal and staphylococcal peritonitis in adults is fortunately rare.
In streptococcal peritonitis, the peritoneal exudates is odourless and thin, contains
some flecks of fibrin and may be blood- stained. In these circumstances pus is
removed by suction, the abdomen closed with drainage and non-operative
treatment of peritonitis performed. The use of intravaginal tampons has led to an
increased incidence of Staphylococcus aureus infections: these can be associated
with “toxic shock syndrome” and disseminated intravascular coagulopathy.
Familial Mediterranean fever (periodic peritonitis)
Familial Mediterranean fever (periodic peritonitis) is characterized by abdominal
pain and tenderness, mild pyrexia, polymorphonuclear leucocytosis and,
occasionally, pain in the thorax and joints. The duration of an attack is 24-72
hours, when it is followed by complete remission, but exacerbations recur at
regular intervals. Most of the patients have undergone appendicectomy in
childhood. This disease, often familial, is limited principally to Arab. Armenian
and Jewish populations; other races are occasionally affected. Mutations in the
MEFV (Mediterranean fever) gene appear to cause the disease. This gene produces
a protein called pyrin, which is expressed mostly in neutrophils but whose exact
function is not known.
Usually, children are affected but it is not rare for the disease to make its first
appearance in early adult life, with cases in women outnumbering those in men by
two one. Exceptionally the disease becomes manifest in patients over 40 years of
age. At operation, which may be necessary to exclude other cases but should be
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
avoided if possible, the peritoneum – particularly in the vicinity of the spleen the
gall bladder- is inflamed. There is no evidence that the interior of these organs is
abnormal. Colchincine therapy is used during attacks and to prevent recurrent
attacks.
Starch peritonitis
Like talc, starch powder has found disfavor as a surgical glove lubricant. In a few
starch-sensitive
Tuberculous Peritonitis
Acute tuberculous peritonitis
Tuberculous peritonitis sometimes has an onset that so closely resembles acute
peritonitis that the abdomen is opened. Straw-coloured fluid escapes and tubercles
are seen scattered over the peritoneum and greater omentum. Early tubercles are
grayish and translucent. They soon undergo caseation and appear white or yellow
and are then less difficult to distinguish from carcinoma. Occasionally, they appear
like patchy fat necrosis. On opening the abdomen and finding tuberculous
peritonitis, the fluid is evacuated, some being retained for bacteriological studies.
A portion of the diseased omentum is removed for histological confirmation of the
diagnosis and the wound closed without drainage.
Chronic tuberculous peritonitis
The condition presents with abdominal pain (90% of cases), fever (60%), loss of
weight (60%), ascites (60%), night sweats (37%) and abdominal mass (26%)
(Summary box).
Summary box .
Tuberculous peritonitis
• Acute and chronic forms.
• Abdominal pain, sweats, malaise and weight loss are frequent.
• Caseating peritoneal nodules are common – distinguish from metastatic
carcinoma and fat necrosis of pancreatitis.
• Ascites common, may be loculated.
• Intestinal obstruction may respond to anti-tuberculous treatment without surgery.
Surgery
Acute Peritonitis and Intra-Abdominal Abscesses
Dr. Basim Rassam
Lec. 18
Origin of the infection
Infection originates from:
• tuberculous mesenteric lymph nodes;
• tuberculosis of the ileocaecal region;
• a tuberculous pyosalpinx;
•blood-borne infection from pulmonary tuberculosis, usually the “military” but
occasionally the “cavitating” form.
