Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
Gall stones (cholelithiasis):
Gall stones are the most common biliary pathology. It is estimated that gall stones
are present in 10-15% of adult population in USA.
They are asymptomatic in majority (more than 80%) .
approximately 1-2% of asymptomatic patients will
develop symptoms requiring cholecystectomy per year
, making this operation one of the most common
operations performed by general surgeons.
Aetilogy of gall stones: gall stones can be divided in to three main types
cholesterol, pigment (brown/black) or mixed stones. In western countries 80% are
cholesterol or mixed stones, whereas in Asia, 80% are pigment stones. Cholesterol
or mixed stones contain 51-99% pure cholesterol plus an admixture of calcium
salts, bile acids, bile pigments and phospholipids. Cholesterol which is insoluble in
water is secreted from canalicular membrane in phospholipid vesicles. Whether
cholesterol remains in solution depends on concentration of phospholipids and bile
salts in bile and the type of phospholipids and bile acids. Micelles formed by
phospholipid hold cholesterol in a stable thermodynamic state. When the bile
supersaturated with cholesterol or bile acid concentrations are low, unstable
unilaminar phospholipid vesicles form, from which cholesterol crystals may
nucleate and stone may form. The process of gall stones formation is complex.
Obesity, high calorie diets and certain medications can increase the secretion of

Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
cholesterol and supersaturate the bile, increasing lethogenicity of bile. Nucleation
of cholesterol monohyderate crystals from multilaminar vesicles is the crucial step
in gall stone formation. Abnormal emptying of the gall bladder may promote the
aggregation of nucleated cholesterol crystals, hence removing gall a stone without
removing the gall bladder inevitably leads to gall stones recurrence. Pigment
stones are the name used for stones containing less than 30% cholesterol. There
were two types black and brown. Black stones are largely composed of insoluble
bilirubin pigment polymer mixed with calcium phosphate and calcium bicarbonate.
Overall, 20-30% of stones are black. The incidence rise with age. Black stones
accompany hemolysis, usually hereditary spherocytosis or sickle cell disease. It
can accompany liver cirrhosis. Brown pigment stones contain calcium bilirubinate,
calcium palmitate and calcium srearate, as well as cholesterol. Brown stones are
rare in the gall bladder. They form in the bile ducts and are related to the bile stasis
and infected bile. Bacteria can form deconjugated bilirubin which is insoluble and
leads to stone formation. Brown pigments are also associated with the presence of
foreign bodies within the bile ducts as endoprosthesis (stents) or parasite such as
clonorchis sinensis and ascaris lumbricodes. Pigment stones are mostly small, and
multiple. Cholesterol stones comprising 6% consist entirely of cholesterol and are
often solitary (cholesterol solitaire). Mixed stones from 90% of gall stones and the
mixture formed from calcium phosphate, calcium carbonate, calcium palmitate and
proteins. Usually they are multiple and often they are faceted.
Incidence of gall stones: Fat, Fertile, Flatulence, Female of Fifty or Forty and Fair
is the classical sufferer from symptomatic gall stone. This is useful in clinical
memorandum, it should be tempered with the knowledge that cholelithiasis occurs
in both sexes, quite often at much earlier age even childhood and is more common
in old age.
Clinical features: patients typically complain of right upper quadrant or epigastric
pain, which may radiate to the back. This may be described as colicky but more
often is dull and constant. Other symptoms include dyspepsia, flatulence, food
intolerance particularly to fat and some alteration in bowel frequency. Biliary colic
is typically present in 10-25% of patients. This is described as severe right upper
quadrant pain that ebbs and flows associated with nausea and vomiting. Pain may
radiate to the chest. This pain is usually severe and may last for minutes or even

Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
several hours. Frequently the pain starts during the night waking the patient. Minor
episodes of the same discomfort may occur intermittently during the day.
Dyspeptic symptoms may coexist and be worse after such attack. As the pain
resolves the patient is able to eat and drink again, often only to suffer further
episodes. It is of interest that the patient may have several episodes of this nature
over a period of a few weeks and then no more trouble for some months. When
symptoms do not resolve but progress to continued pain with fever and
leucocytosis, the diagnosis of acute cholecystitis should be considered.
Differential diagnosis: (1) common----appendicitis, perforated peptic ulcer, acute
pancreatitis. (2) Uncommon----acute pyelonephritis, myocardial infarction,
pneumonia.
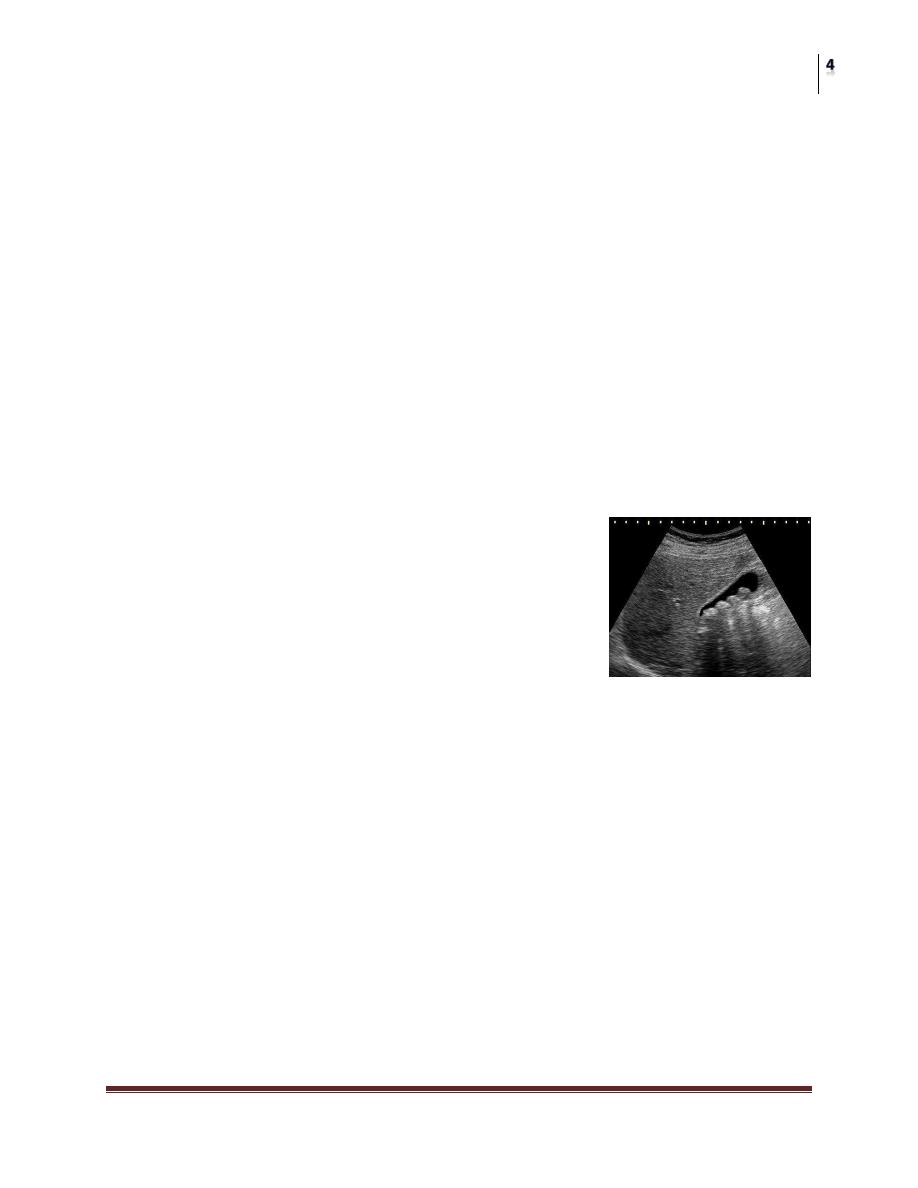
Diagnosis: a diagnosis of gall stones disease is based on the history and physical
examination with confirmatory radiological studies such as ultrasound of abdomen
and scan. In ultrasound study the gall stones have a hypoechoeic shadow and with
acoustic shadow, it demonstrate the biliary duct and show any dilatation in the bile
duct specially common bile duct (up to 10mm consider normal) and the thickness
of the wall of the gall bladder , more than 3mm considered pathological, and any
mass in the pancreas.
Plain abdominal x-ray has a limited value as most of gall stones are radiolucent
(85%) and (15%) are radio-opaque to be seen in plain x-ray.
CT-scan has a value in complicated cases to certain the diagnosis and can visualize
all abdominal organs. In acute phase the patient may have right upper quadrant
tenderness that is exacerbated during inspiration by the examiner's right subcostal
palpation which is called Murphy's sign. A positive sign suggest acute
inflammation and may be associated with leucocytosis and moderately elevated
liver function tests. A mass may be palpable as the omentum walls off inflamed
gall bladder. Fortunately, in the majority of cases this process is limited by the
stone slipping back in to the body of the gall bladder and the contents of the gall
bladder escaping by way of the cystic duct. This achieves adequate drainage of the
gall bladder and enables the inflammation to resolve. If resolution does not occur
an empyema of the gall bladder may result. The wall may become necrotic and
perforate with the development of localized peritonitis. The abscess may then
perforate in to peritoneal cavity with a septic peritonitis however; this is
Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
uncommon, because the gall bladder is usually localized by omentum around the
perforation. A palpable, non-tender gall bladder as in Courvoisier's sign portends a
more sinister diagnosis. This is usually results from a distal common duct
obstruction secondary to peripancreatic malignancy. Rarely, a non tender palpable
gall bladder results from complete obstruction of the cystic duct with reabsorption
of the intraluminal bile salts and secretion of uninfected mucus secreted by the gall
bladder epithelium, leading to mucocele of the gall bladder.
Treatment: most surgeons would suggest that is safe to observe patients with
asymptomatic gall stones, with cholecystectomy only being performed for those
patients who develop symptoms or complications of their gall stones. However,
prophylactic cholecystectomy should be considered in diabetic patients, those with
congenital hemolytic anemia and those due to undergo bariatric surgery for morbid
obesity, as these groups are at risk of complications of gall stones. For patents of
biliary colic or cholecystitis, cholecystectomy is the
treatment of choice in the absence of medical
contraindications. The timing of cholecystectomy in
acute cholecystitis is remaining controversial between
early and delayed surgery with advantages and
disadvantages of each timing of it.
Conservative treatment followed by cholecystectomy:
experience shows that, in 90% of cases, the symptoms of acute cholecystitis
subside with conservative measures. Non operative treatment is based on four
principles:
1- Nil per mouth and intravenous fluids administration. 2- Parentral analgesia in
form of pethidine, morphine or non-steroidal anti-inflammatory drug with or
without antiemetic drugs. 3- Antibiotics intravenously as 3
rd
generation
cephalosporin with metronidazole, those will affect gram negative aerobes. 4-
Subsequent management. When temperature, pulse and other physical signs
show that the inflammation subsiding, oral fluids are reinstated followed by
regular diet. Ultrasound is performed to ensure that no local compilations have
developed, hat he bile duct is of a normal size and that no stones are contained
in the bile duct. Cholecystectomy may be performed on the next available list,
or the patient may be allowed home to return later when the inflammation has
Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
completely resolved. Conservative treatment may be abandoned (stopped) if the
pain and tenderness increase, depending on the status of the patient, operative
intervention and cholecystectomy should be performed. If the patient has a
serious comorbid condition, a percutaneous cholecystostomy can be performed
under ultrasound control, which will rapidly relieve symptoms. A subsequent
cholecystectomy is usually required.
Routine early operation: as noted above, some surgeons advocate urgent
operation as routine measure in case of acute cholecystitis. Provided that the
operation is undertaken within 5-7 days of the onset of the attack, the surgeon is
experienced and excellent operating facilities are available, good results are
achieved. If an early operation is not indicated one should wait approximately 6
weeks for the inflammation to subside before proceeding to operate.
Medical treatment of gall stones has a very limited space of treatment and
should be used in a small radiolucent stones and functioning gall bladder, this
treatment in form of bile acids, chenodeoxycholic and ursodeoxycholic acid
taken orally will dissolve gall stones , it should be taken at least for 6 months
and it might cause diarrhea, so this treatment keep only for unfit patients and for
small retained stoners of biliary tree.
Empyema of the gall bladder:
the gall bladder appears to be filled with
pus. It may be a sequel of acute cholecystitis or the result of a mucocele
becoming infected. The treatment is drainage and then cholecystectomy.
Acalculous cholecystitis:
acute and chronic inflammation of the gall bladder
can occur in the absence of stones and give rise to clinical picture similar to
calculous cholecystitis. Some patients have no specific inflammation of the gall
bladder. Acute acalculous cholecystitis is seen particularly in patients
recovering from major surgery as coronary artery bypass, trauma and burns. In
these patients the diagnosis often missed and the mortality rate is high.
Typhoid gall bladder: acute and mostly chronic cholecystitis occurs and the
patient being a typhoid carrier, excrete the bacteria of salmonella typhi in the
bile. Gall stones may be present, it is debatable whether the stones are
secondary to the salmonella or preexisting stones predispose the gall bladder to
Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
chronic infection. Salmonella can, however, frequently be cultured from these
stones so the surgeon should not give patients their stones after the operation if
there is any suspicion of typhoid.
Cholecystectomy: preparation for operation: an appropriate history is taken, and
the patient's fitness for the procedure is assessed. This includes investigations of
cardiovascular and respiratory systems, and full blood count and biochemical
profile are performed to exclude anemia or abnormal liver function. Blood
coagulation is checked if there is a history of jaundice. The patient is given
prophylactic antibiotics either with premedication or at the time of anesthetic
induction. A second generation cephalosporin or 3
rd
generation is appropriate.
Subcutaneous heparin or antiembolic stockings are prescribed. the patient must
sign a consent form indicate that he or she is fully aware of the procedure being
undertaken, the risks involved and the complications that may occur. Operation
can be done as laparoscopic procedure as it is the procedure f choice while open
procedure can be done in who a laparoscopic approach is not indicated or
conversion from laparoscopic approach is required.
Effect and complications of gall stones: 1- on the gall bladder----Biliary colic,
acute cholecystitis, chronic cholecystitis, empyema of the gall bladder,
mucocele, perforation. 2- in the bile ducts---- Biliary obstruction, acute
cholangitis, acute pancreatitis. 3- in the intestine----intestinal obstruction called
gall stone ileus.
Post cholecystectomy syndrome: in 15% of all cases cholecystectomy fail to
relieve the symptoms for which the operation was performed. The symptoms
are most commonly due to disease of organs other than the biliary tract, such as
hiatus hernia, duodenal ulcer, pancreatitis, diverticulitis or irritable bowel
disease. One should check if there is any stone in bile duct and is missed or if
any damage to common bile duct during operation or long stump of cystic duct.
Stones in the bile ducts: (obstructive jaundice)
Ducts stones may occur many years after cholecystectomy or be related to
development of new pathology such as infection of the biliary tree or infestation
by ascaris lumbrecoids. Any obstruction to the flow of bile can give rise to
stasis with the formation of stones within the duct. The consequence of duct

Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
stones is either obstruction to bile flow or infection. Stones in the bile ducts are
more often associated with infected bile than are stones in the gall bladder.
Symptoms: the patient may be asymptomatic but usually has bouts of pain,
jaundice and fever. The patient is often ill and feels unwell. The term
cholangitis is given to the triad of pain, jaundice and fever, rigor known as
Charcot's triad. Signs: tenderness may be elicited in the epigastrium and the
right hypochondrium. In the jaundiced patient ,it is useful to remember
Courvoisier's law as in obstruction of the common bile duct due to stone,
distension of the gall bladder seldom occurs , the organ is usually already
shriveled(shrinked and contracted) .
In obstruction from other causes, distension of the gall bladder is common by
comparison. Management: it is whether the jaundice is due to liver disease
(hepatocellular), disease within the duct, such as sclerosing cholangitis, or
obstruction of Biliary tree as obstructive jaundice or called surgical jaundice.
Ultrasound scanning, liver function tests, liver biopsy (if the duct are not
dilated), and MRI or ERCP will delineate the nature of the obstruction. The
patient may be ill. Pus may be present with in biliary tree and liver abscess may
develop. Full supportive measures are required with rehydration by a high
intake of glucose to build up the store of liver glycogen, correction of clotting
abnormality and this is usually due to failure to absorb vitamin K as this fat
soluble vitamin requires bile salts for its absorption and these are lacking from
the gut in obstructive jaundice. Vitamin K1 10 mg is given i.m or i.v, blood
cultures are taken and treatment with appropriate broad spectrum antibiotics if
there is any evidence of cholangitis as fever, raised WBC. Patients with
obstructive jaundice particularly if submitted to operation are prone to renal
failure so dehydration must avoided and mannitol i.v should be given prior to
surgery to promote diuresis. Once the patient has been resuscitated, relief of
obstruction is essential. Endoscopic papillotomy is the preferred first technique
with a sphincterotomy by ERCP, removal of stone using Dormia basket or
placement of stent if stone removal is not possible. If this technique fails,
percutaneous transhepatic cholangiography can be performed to provide
drainage and subsequent percutaneous choledochoscopey. Surgery, in form of
choledochotomy (exploration of common bile duct) is now rarely used for this
situation, as most patients can be managed by minimally invasive techniques.
Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
Complications of obstructive jaundice: 1- prolonged obstruction causes
impairment of liver function which in some cases may progress to Biliary
cirrhosis. White bile may be seen in bile ducts at operation. 2- Suppurative
cholangitis as the bile ducts can become fulled with pus. Liver abscesses and
septicemia result. White bile is a condition follows obstruction of a large duct.
It is mostly mucus derived from glands lining the ducts.
Stricture of the bile duct: the causes of benign biliary stricture are 1- congenital
as in biliary atresia 2- bile duct injury during surgery as in cholecystectomy,
choledochotomy,
gastrectomy,
hepatic
resection,
transplantation.
3-
inflammatory as stones, cholangitis, parasitic, pancreatitis, sclerosing
cholangitis, radiotherapy. 4- Trauma. 5- Idiopathic.
Investigations: 1- ultrasound to see the size of common duct, stones, growth. 2-
Cholangiography to visualize the bile ducts 3- ERCP. 4- MRCP. 5- PTC. 6- CT
abdomen.
Primary sclerosing cholangitis: primary sclerosing cholangitis is an idiopathic
fibrosing inflammatory condition of the biliary tree that affects both
intrahepatic and extrahepatic ducts. It is of unknown origin, but association with
hypergammaglobulinaemia and elevated markers such as smooth muscles
antibodies and anti-nuclear factor suggests an immunological basis. The
majority of patients are between 30 and 60 years of age. There appears to be
male predominance and strong association with inflammatory bowel disease,
especially ulcerative colitis. Common symptoms include right upper quadrant
discomfort, jaundice, pruritis, fever, fatigue, and weight loss. Liver function
tests reveal increase in alkaline phosphatase, fluctuation in serum bilirubin and
increase in aminotransferase, liver biopsy is helpful to confirm the diagnosis.
The differential diagnosis is with secondary sclerosing and cholangiocarcinoma.
Medical treatment with antibiotics, vitamin K, cholestyramine, steroids and
immunosuppressant as azathioprine is generally unsuccessful. Endoscopic
stenting of dominant strictures and in selected cases, operative resection is
indicated. Liver transplantation is the best option. 5 years survival following
transplantation is more than 80%.
Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
Hydatid diseases in bile ducts: as one major cause of parasitic origin. a large
hydatid cyst may obstruct the hepatic ducts. Sometimes a cyst will rupture in to
the biliary tree and the contents cause obstructive jaundice or cholangitis,
requiring appropriate surgery.
Tumors of bile ducts: it can be benign as papilloma or adenoma or leiomyoma
and it can be malignant as carcinoma which may arise at any point in the biliary
tree, from the common bile duct to small intrahepatic ducts. It is rare tumor as
adenocarcinoma or called cholangiocarcinoma, in elderly age group above 65
years. The risk factors include ulcerative colitis, primary sclerosing cholangitis,
hepatolithiasis, and choledocal cyst. It is a slow tumor invading locally and
metastasis to regional lymph nodes presented with obstructive jaundice and
weight loss and liver might be enlarge and gall bladder might be palpable.
Diagnosis is done by ultrasound and CT scanning. Treatment: palliative
measure through a stenting to relief the obstruction of biliary ducts. Surgical
excision is possible in 5% of the cases. Prognosis is very poor, 90% mortality in
1 year.
Carcinoma of the gall bladder: it is rare disease, but extremely variable by
geographical region and racial/ethnic groups. The highest incidence is in
Chileans, American Indians, and in north India, where it accounts for as much
as 9.1% of all biliary tract disease. In western it accounts for less than 1% . It
occurs usually in elderly patients in their sixties and seventies. The etiology is
not clear and associated with preexisting gall stone disease. Calcification of the
gall bladder is associated with cancer in 10-25% of cases promote the
development of cancer specially typhoid carriers. The majority of cases 90%
are adenocarcinoma and at time of presentation the tumor is usually advanced.
Clinical features: may be asymptomatic at time of diagnosis. If symptoms
appear they are usually indistinguishable from benign gall bladder disease such
as biliary colic, cholecystitis. Jaundice and anorexia are late features. a palpable
mass is late sign. Diagnosis by ultrasound and CT scan. Treatment: occasionally
the diagnosis is made by Histopathological examination of a gall bladder
removed for benign gall stone disease. For early stage disease confined to the
mucosa or muscle of the gall bladder, no further treatment is indicated.
However, for transmural disease, a radical en bloc resection of the gall bladder
Surgery
Gall Bladder Diseases and Obstructive Jaundice
Dr. Tariq Al-Aubaidi
Lec. 15
fossa and surrounding liver along with the regional lymph nodes should be
performed. The disease has a very poor prognosis with the median survival less
than 6 months and 5 year survival of 5%. The value of adjuvant chemotherapy
is unproven.
