Surgery
Intestinal obstruction
Dr. Tariq Al-Aubaidi
Lec. 10
Intestinal obstruction is a common surgical emergency and because of its serious
nature it demand early diagnosis and treatment. It may classify in to two types:
1. Dynamic: here there is peristalsis working against an obstructing agent,
which may be in the lumen such as bolus of incompletely digested material,
faeces.
Gall stones, in the wall such as inflammatory or malignant stricture,
or outside the wall as in hernias adhesions, volvulus or intussusceptions.
2. Adynamic: in this condition peristalsis ceases and no true propulsive wave
occur as in paralytic ileus or mesenteric vascular occlusion.
Dynamic obstruction:
is classified clinically in to three types:
1. Acute obstruction: favoring the small gut with central abdominal pain,
early vomiting central abdominal distension and constipation.
2. Chronic obstruction: favoring the large bowel severe abdominal colic at
first and absolute constipation and distension later.
3. Acute-on-chronic: which spread from the large bowel to involve the small
intestine gives early pain and constipation followed by general distension
and vomiting.
Pathology:
1.
The intestine above the point of obstruction: have a vigorous peristalsis to
overcome obstruction, the peristalsis continue for a period from 48hours to
several days. If obstruction is not relived the peristalsis becomes less and

Surgery
Intestinal obstruction
Dr. Tariq Al-Aubaidi
Lec. 10
less with increasing distension finally peristalsis ceases and obstructed
intestine becomes flaccid and paralyzed.
2.
The intestine below the point of obstruction: has normal peristalsis and
absorption from it continue for 203 hours following the obstruction until the
residue of its contents has been passed onwards. Then the empty intestine
becomes immobile, contracted and pale and so it remains until the
obstruction has been overcomes or death ensues.
3.
Distension: this occurs proximal to obstruction and begins immediately after
the obstruction occurs. The cause of distension is two folds
(a) Gas: compose of swallowed air (80%), diffusion from blood to bowel lumen
(22%) and the product of digestion and bacterial activity (10%). When the
oxygen and carbon dioxide has been absorbed in to blood stream the resultant
mixture is made up of nitrogen 90% and hydrogen sulfide.
(b) fluid: this made up by various digestive juices about 8000ml|24hours, above
pylorus 4000ml, saliva1500ml, gastric juices2500ml and below pylorus
4000ml, bile and pancreatic 1000ml, succus entericus 3000ml. the absorption of
gut is retarded and excretion of water and electrolyte in the lumen persist and
even be increased and the loss usually by vomiting, defective of absorption and
sequestrations in lumen of the bowel. Toxins appear in the peritoneal cavity
only when the viability of the bowel wall is affected by cutting its blood supply
(strangulation). These are endotoxins of gram negative bacilli leads to septic
shock and death if not relieved.
Strangulation:
of the bowel occurs when it trapped by a hernia or a band or
involved in a volvulus or intussusceptions in such way that its blood supply is
progressively interfered with. It is a very dangerous condition and demands early
treatment before gangrene of the bowel arises. Mesenteric vascular occlusion alone
gives rise to gangrene without mechanical obstruction. The onset of gangrene first
compression of the veins causes the strangulated bowel. When venous return is
completely occluded the color changes from the purple to black. As time passed,
increased edema at the point of obstruction the arterial supply is in danger, the
peritoneal coat loses its glistening appearance, the mucous membrane becomes
ulcerated and moist gangrene is imminent.
Surgery
Intestinal obstruction
Dr. Tariq Al-Aubaidi
Lec. 10
Clinical features of acute intestinal obstruction: there are four important
symptoms and signs, pain, vomiting distension and constipation.
(1) Abdominal pain is the 1
st
symptom it commences suddenly and often without
warning it becomes increasingly severe then passes off gradually only to returns to
interval of a few minutes. These attacks of intestinal colic which last from 3-5
minutes, spread all over the abdomen but are localized mainly at umbilicus. In
between attacks the patient is often quite free from the pain. Recurring attacks of
severe abdominal pain are a leading feature of all varsities of acute intestinal
obstruction with the exception of paralytic ileus.
(2) Vomiting: when the jejunum is a mechanically obstructed, vomiting occurs
with 1
st
and each succeeding attack of pain. In the much more common obstruction
of the ileum the patient may vomit once, following which there is an interval of
several hours during which time the attacks of pain occur without vomiting.
Ultimately copious, forcible, repeated vomiting sets in. as acute intestinal
obstruction progress the character of the vomitus alters. Initially it contains partly
digested food, next it consists entirely of yellow or green from regurgitation of bile
finally it is faeculent.
(3) Distention: in early cases of obstruction of the small intestine, abdominal
distension often slight or even absent. Centrally placed distension is present in
fully established cases of obstruction of ileum. Visible peristalsis may be present,
borborygmi are sometime loud enough to be heard by unaided ear, more often
auscultation is necessary. The sound of turbulent peristalsis coinciding with an
attack of colic is valuable evidence of intestinal obstruction. In all cases of
suspected intestinal obstruction it is essential to examine the common hernia sites.
Irreducible external hernia may be present although the patient is entirely unaware
of it.
(4) Constipation: in complete intestinal obstruction after the contents of the bowel
below the obstruction has been evacuated there is constipation and usually neither
faeces nor flatus is passed, that is absolute constipation appeared.
(5) Dehydration: repeated vomiting and also loss of the absorptive power by the
distended intestine leads to dehydration and when the patient is 1
st
examined
obvious signs of dehydration, a dry skin and dry tongue and sunken eye may be
Surgery
Intestinal obstruction
Dr. Tariq Al-Aubaidi
Lec. 10
present. The output of the urine is small; it is concentrated and contains a little
chloride. The level urea might be raised.
Chronic obstruction:
this is commonly due to carcinoma or diverticulitis of
the colon. Here constipation appears first may last for days, weeks and finally
becomes absolute when the passage of flatus ceases. Abdominal distension then
occurs, especially in the flanks. As the obstruction occurs in the large bowel, the
caecum becomes ballooned and might be perforated and makes general peritonitis.
Pain accompanies the distension and there are regular bouts of colic usually in the
hypogastrium. It is not uncommon for vomiting to be delayed for 2-3days and
dehydration is very late. On palpation a neoplasm occasionally can be felt in line of
colon , a rectal examination will enable a carcinoma of rectum or mass of impacted
faeces to be felt and it may be possible to feel a neoplasm in then pelvic colon.
Acute-on-chronic obstruction:
this starts with all the features of chronic
obstruction but after a few days ,the pain vomiting and central distension , then
ileocaecal valve is opened and faeculent fluid has passed up via the ileum in to
stomach from which is rapidly vomited.
Strangulation:
it is of the highest importance to distinguish strangulating
from non-strangulating intestinal obstruction, because if the former is not relieved
by urgent operation, gangrene follows quickly. The picture is usually that of an
obstruction together with a degree of shock which is sometimes severe. In
strangulation, the pain so severe and never completely absent and the symptoms
usually commences very suddenly and spasms of intestinal colic recurs 3-4 times
in a minute. Generalized tenderness and rigidity are indicative of early laparatomy
to be performed. Rebound tenderness is very severe over strangulated coil and if
hernia is present usually the lump is tense, tender, irreducible and no cough
impulse and has recently increase in size, these points ar3e most voluble in
diagnosis. Also the vital signs are indicative as increase in pulse rate and decrease
in blood pressure, sign of shock is usually present in strangulation.
Investigations: plain abdominal x-rays taking in standing and lying down position,
multiple air-fluid level inside the coils of intestine usually centrally located in case
of small intestine and peripheral location in large intestine. The small bowel
Surgery
Intestinal obstruction
Dr. Tariq Al-Aubaidi
Lec. 10
distinguish by valvulae conniventes while the large bowel by haustration. In
infants under 2years age a few fluid levels in small intestine are normal
occurrence. In adults two inconstant fluid levels must be regarded physiological,
one on duodenal cap and the other which is more infrequent is with in terminal
ileum. In intestinal obstruction fluid levels appeared later than gas shadows. The
number of fluid levels is proportionate to the degree of obstruction and to the site
of small intestine. In large bowel obstruction a plain film show a large amount of
gas in the caecum and Ba-enema is contraindicated during attack of intestinal
obstruction. Multiple gas filled loops above fluid levels in both small and large
bowel are also seen in paralytic ileus.
Treatment: we start by conservative treatment and this can be relief the
obstruction or it may be preparation of doing operation. It consist of
(1) gastro-duodenal or gastro-intestinal suction drainage by nasogastric tube to
prevent vomiting and to examine the color of fluid and calculate the amount of the
fluid.
(2) Replacement of the fluid as normal saline or ringer solution.
(3) Relief of obstruction by operation.
(4) Antibiotics in form of 3
rd
generation cephalosporin and metronidazole to
prevent complications from sepsis and peritonitis.
(5) Calculate of vital signs of pulse rate, blood pressure, urine output by making a
chart and putting a folly's catheter.
(6) Prepare a blood for transfusion, if needed.
The main indication for early operation after conservative treatment
(1) Obstructed or strangulated external hernia.
(2) Internal intestinal strangulation.
(3) Acute or acute on chronic obstruction and the most urgent is intestinal
strangulation. Relief of obstruction by operation through repair of obstructed
hernia or lysis of peritoneal adhesions. If the bowel is hugely distended should be
evacuated by aspiration and suction and then relief the obstruction. If there is
strangulation and gangrene seen, a loop of gangrenous bowel should be resected
and anastomosis done. Viable bowel should be distinguished from non-viable by:
Surgery
Intestinal obstruction
Dr. Tariq Al-Aubaidi
Lec. 10
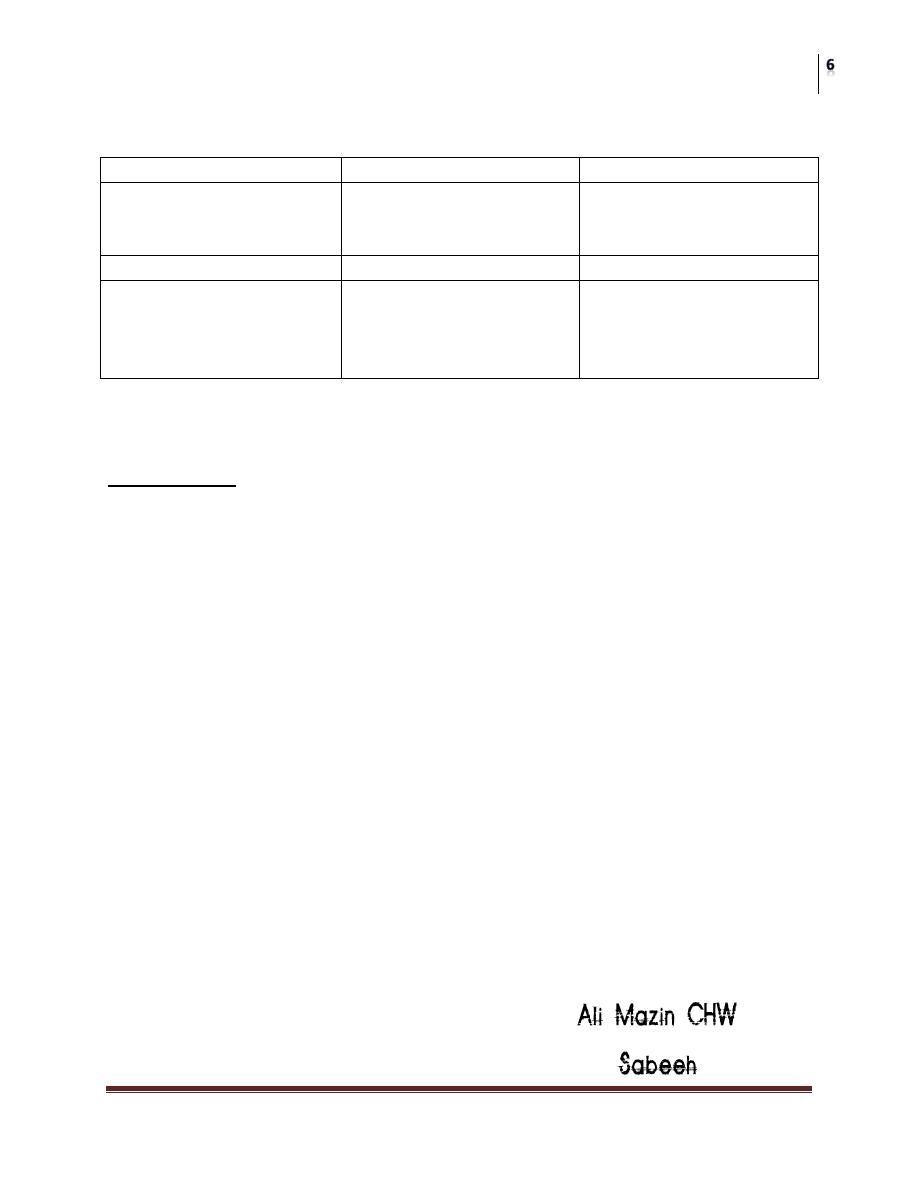
Intestine
viable
Non-viable
circulation
Dark color becomes
lighter, mesentry bleed if
pricked
Dark color remains, no
bleeding if mesentry
pricked.
peritoneum
shiny
Dull and lusterless
Intestinal musculature
Firm, pressure rings may
or may not disappear,
peristalsis may be
observed.
Flabby, thin, and friable,
pressure rings persist, no
peristalsis.
Paralytic ileus: this has already been defined as a state in which the intestine fails
to transmit peristaltic waves and is due to failure of neuromuscular mechanism.
This result in collection of fluid and gas in the intestine with resulting distention,
vomiting, absent bowel sound and failure to pass flatus.
Causes: (1) postoperative: some degree of ileus either local or general may follow
any abdominal operation. The intestinal mobility and absorption commonly returns
to normal in about sixteen hours. (2) Infective: peristalsis ceases as normal
response to prevent dissemination but afterwards bacterial toxins prevent normal
activity of nerve plexus. (3) Reflex: in case of spine, ribs fractures, retroperitoneal
hemorrhage or application of plaster jacket. (4) Uremia (5) hypokalemia.
Clinical features (1) there has been no passage of flatus. (2) There are no returns
of bowel sound on auscultation. (3) Abdominal distension more marked.
Management: (1) primary cause must be removed as hypokalaemia, uremia.
(2)normal bowel activity will be returned if distension is relieved by nasogastric
tube as decompression. (3) Morphine or pethedine in small doses are well proved.
(4) Close attention to and electrolyte balance by giving parenteral fluid and
potassium. (5) Peristaltic stimulants have no place in treatment. The object is to
rest the bowel not to stimulate it.
