Surgery
UTI
Dr. Ismaeel
Lec. 42
Definitions
Urinary tract infection (UTI) team applied to a variety of clinical conditions
ranging from asymptomatic bacteruria to severe infection of the kidney with
sepsis.
Risk Factors:
female sex; increasing age; low estrogen
states (menopause); pregnancy;
diabetes mellitus;
previous UTI;
elderly;
indwelling catheters;
urolithiasis;
genitourinary malformation;
and voiding dysfunction (including obstruction)
Pyuria: the presence of more than 3 WBCs per high power field in urinalysis.
Sterile pyuria: presence of WBCs(pus) in urinalysis with negative urine culture.
Causes:
1. GU Tuberculosis.
2. Acute papillary necrosis.
Surgery
UTI
Dr. Ismaeel
Lec. 42
3. Ca. in situ
4. Bladder stones
An uncomplicated UTI: UTI occuring in a patient with a structurally and
functionally normal urinary tract.
A complicated UTI: UTI occuring in the presence of an underlying anatomical &
functional abnormality (longer to respond to AB treatmenr & high risk of
recurrence)
Urinary tract infections:
1. Isolated UTI: has an intarval of at least 6 months bet. Infections.
2. Recurrent UTI: Are more than 2 infections in 6 months or 3 within 12
months.
Causes:
1. Reinfection ( by different MO.)
2. Bacterial persistence (same MO. From a focus in the urinary tract).
3. Unresolved infection: failure of initial treatment course to eradicate infection
due to :
a. AB resistance
b. Noncompliance
c. Insufficient AB dose
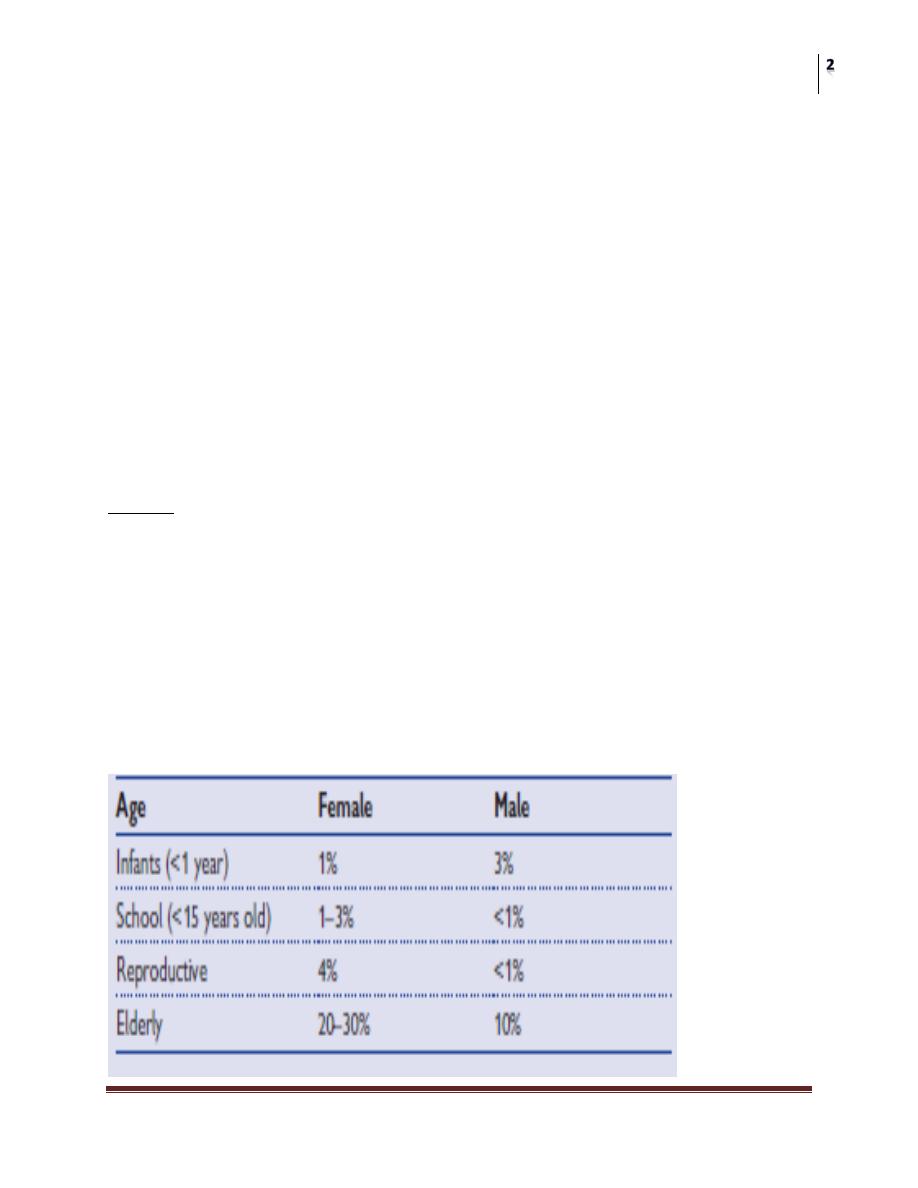
UTI incidence

Surgery
UTI
Dr. Ismaeel
Lec. 42
UTI investigations
Urine dipstick : midstream sample
Urine microscopy :
1. Bacterial count more than 100000 CFU/ml
2. >3 WBC/HPF,,,
3. Gram stain
4. Large numbers of squamous epithelial cells- sample is contaminated.
Urine culture and collection (Urine culture is the gold standard for the
diagnosis of a bacterial UTI.).
Further investigation ((plain abdominal film, CT, ultrasound)).
functional studies (uroflow, post void residual urine determination,
urodynamics studies)
Urinalysis give us a provisional diagnosis of UTIs and urine culture give us
the definitive diagnosis of UTIs
Urinary tract infection:
microbiology
Most UTIs are caused by fecal-derived bacteria that are facultative
anaerobes (i.e., they can grow under both anaerobic and nonanaerobic
conditions).
Uncomplicated UTI(E coli 85%,50%).
Complicated UTI ( E. coli 50%).
Most of UTIs caused by a single bacterial species.
Route of infection
Ascending ((vast majority)).
Hematogenous( TB ).
Infection via lymphatics(rare)
Direct extention from adjacent organs eg intraperitoneal abscesses or
vesicointestinal fistula.
Surgery
UTI
Dr. Ismaeel
Lec. 42
Pathogenesis:
Factors increasing bacterial virulence
Adhesion factors (pili):by these pili the bacteria can adhere to the urothelium
and causing UTIs.
P pili
Type 1 pili
Avoidance of host defense mechanisms:
(An extracellular capsule, Toxins, Enzyme production)
Host defenses
Factors protecting against UTI are the following:
• Mechanical flushing effect of urine through the urinary tract (i.e., antegrade flow
of urine)
• A mucopolysaccharide coating of the bladder (Tamm–Horsfall protein, glucose
amino glycan [GAG layer]) helps prevent bacterial adherence.
• Low urine pH and high osmolarity reduce bacterial growth.
• Urinary immunoglobulin (IgA) inhibits bacterial adherence.
Normal flora in females in the periurethral area (lactobacillus).
Urinary tract infection: treatment
The aim is to eliminate bacterial growth from the urine.
Antimicrobial drug therapy
Management of women with recurrent UTIs from reinfection:
Screening tests (KUB radiograph, renal ultrasound, CT scan, flexible
cystoscopy) to evaluate for a potential source of bacterial persistence.
Mx:
1- Avoidance of spermicides used with the diaphragm or on condoms
(nonoxynol-9).
2- Estrogen replacement therapy.
3- Low-dose antibiotic prophylaxis (trimethoprim, nitrofurantoin, low-dose
cephalexin, and the fluoroquinolones ).

Surgery
UTI
Dr. Ismaeel
Lec. 42
Alternative therapies:
1- Natural yogurt.
2- Cranberry juice.
Post-intercourse antibiotic prophylaxis.
Self-start therapy.
Management of men and women with recurrent UTIs due to
bacterial persistence
Investigations
These are directed at identifying the potential causes of bacterial persistence:
1- KUB.
2-Renal ultrasound.
3-Bladder ultrasound.
4-IVP or CT urogram.
5-Flexible cystoscopy.
Treatment::
Treatment depends on the functional or anatomical abnormality identified as the
cause of the bacterial persistence.
KIDNEY INFECTIONS:
Acute pyelonephritis
Definition: inflammation of the kidney and renal pelvis and it is diagnosis is
usually clinical.
Presentation:
1. fever(temp > 38.5 c)
2. Rigor
3. Renal angle tenderness
4. Lower UTI Symptoms (freq, urgency...)
5. Neonatal presentation.
Differential diagnosis:
1. Cholecystitis
2. Pancreatitis
Surgery
UTI
Dr. Ismaeel
Lec. 42
3. Diverticulitis
4. appendicitis
Risk factors:
VUR.
UT obstraction.
Stones.
Neurogenic bladder.
DM
Pregnancy.
Catheters.
Pathogenesis and microbiology:
1. 80% E. coli.
2. 20% others; klebsiella,pseudomonas ,strept. Faecalis,S. aureus.
Investigation:
1.urinalysis.
2. urine& blood culture.
3. Complete blood picture.
4. Renal function test.
5. Radiological imaging; IVU, CT scan
Surgery
UTI
Dr. Ismaeel
Lec. 42
Treatment:
1. Depend on severity.
2. Obstruction must be relieved.
3. Hospital addmission.
4. Antibiotic therapy.;
a. Outpatient treatment: oral quinolones eg ciprofloxacin 500 mg /twice daily
OR Trimethoprim for 10-14 days.
b. Hospital patients: parentral AB. Eg ampicillin +gentamycin OR 3
rd
generation cephalosporins, OR IV quinolones , for 10-14 days.
complications:
Pyonephrosis
Perinephric abscess.
perinephric abscess
Extension of infection outside the parenchyma of the kidney in acute
pyelonephritis or from haematogenous spread.
Risk factors:
1. Diabetis.
2. Obstruction of the UT. Eg stone in the ureter.
Clinical feature:
No response to IV antibiotic therapy for acute pyelonephritis.
Investigations:
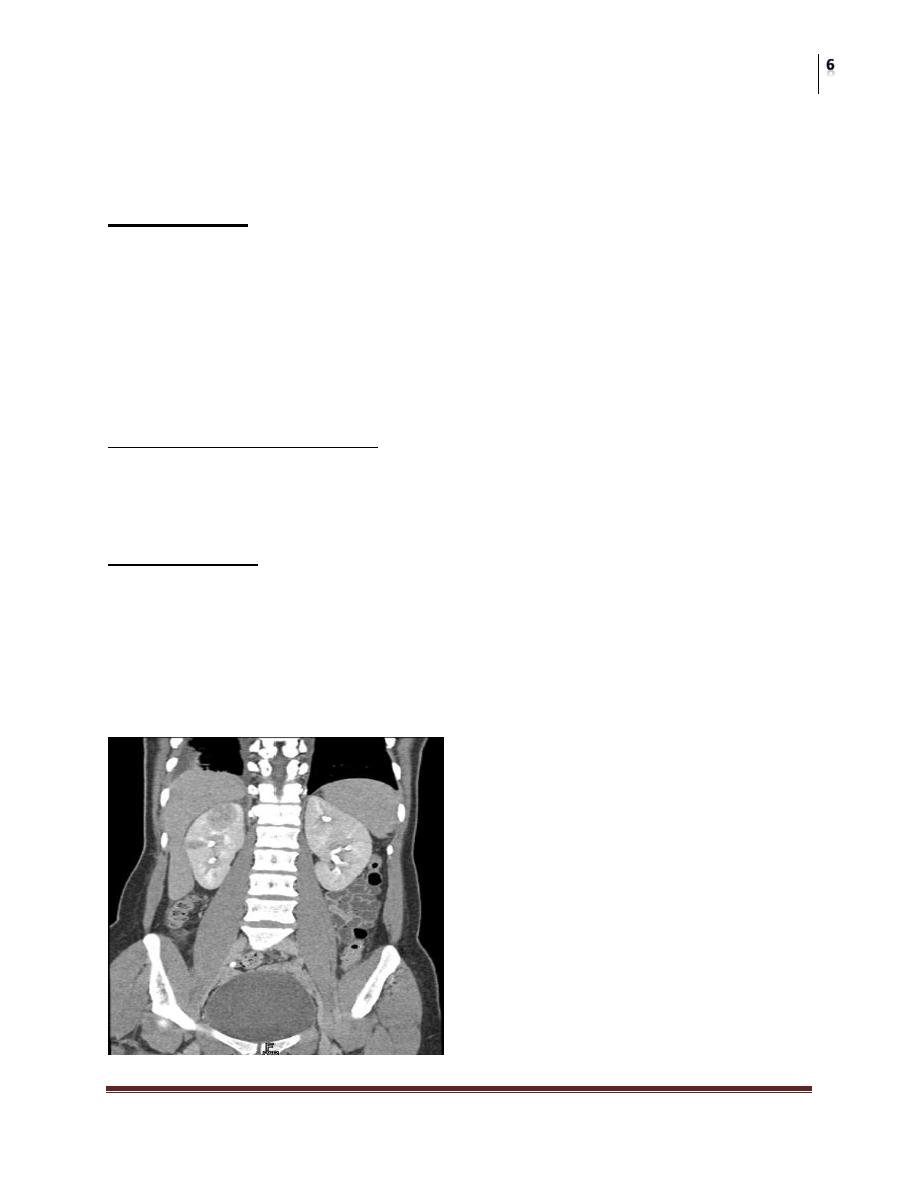
Imaging : US,CT scan
Treatment:
Drainage (percut. Or open) + antibiotic therapy
Nephrectomy.

Surgery
UTI
Dr. Ismaeel
Lec. 42
Pyonephrosis:
Pus accumulate within hydronephrotic,obstructed kidney with subseq. Destruction
of renal tissue and loss of kidney function.
Diabetes, obstruction
Clinical findings:
Fever,chills , flank pain.
Very ill
Investigations:
urinalysis, CBP,RFT…..Imaging :US,
Treatmen:
iv antibiotics + drainage
Nephrectomy.
Surgery
UTI
Dr. Ismaeel
Lec. 42
Other forms of pyelonephritis
Emphysematous pyelonephritis:
This is a rare, severe form of acute pyelonephritis caused by gas-forming
organisms.
Predisposing factors:
Diabetes mellitus, UT obstruction.
Presentations: severe acute pyelonephritis (high fever) fails to respond
within 2-3 days.
Common MO. E. coli, kleb. ,proteus.
Investigations:
KUB: gas over kidney shaddow
US, CT scan (more sensitive)
Treatment :
Control blood suger, relief of obstruction, iv antibiotics, if failed nephrectomy.
Xanthogranulomatous pyelonephritis:
Chronic bacterial infection of the kikney.
Diabetis,UT obstruction.
Severe infection damage kidney
Histologically: foamy lipid-laden histiocytes(xanthoma cell)
DDx : renal cell ca.
Flank pain, fever, rigor , persistance bacteruria & flank mass.
Imaging: CT scan.
Treatment: nephrectomy.
Chronic pyelonephritis
Lower urinary tract infection:
Cystitis is infection and/or inflammation of the bladder.
Presentation:
1. frequent voiding of small volumes,
2. dysuria, urgency, offensive urine,
Surgery
UTI
Dr. Ismaeel
Lec. 42
3. suprapubic pain,
4. hematuria,
5. fever (uncommon),
6. And incontinence.
Investigation:
Dipstick of midstream specimen of urine
Microscopy of midstream specimen of urine (The finding of pyuria and red
blood cells suggests the presence of active infection).
Treatment:
Short course of AB for 3-5 days eg. Trimethprim, ciprofloxacin.
Haemorrhagic cystitis:
Causes:
1. Bacterial cystitis.
2. Non infective cystitis:
radiation cystitis
drug-induced cystitis (e.g., cyclophosphamide treatment)
Urethritis
Urethritis is infl ammation of the urethra.
Urethritis in men is a sexually transmitted disease, which presents with
dysuria and urethral discharge.
Gonococcal urethritis (GU)
GU is caused by the gram-negative diplococcus Neisseria gonorrhoea
(incubation3–10 days)
Commonly associated with concomitant infection with Chlamydia
trachomatis.
Diagnosis is based on cultures from urethral swab
Treatment involves ceftriaxone 125 mg IM in a single dose or cefi xime 400
mg orally in a single dose plus doxycyclin 100 mg twice daily for 10 days.
Surgery
UTI
Dr. Ismaeel
Lec. 42
Nongonococcal urethritis (NGU)
NGU is mainly caused by Chlamydia trachomatis (incubation 1–5 weeks).
Treat with azithromycin, 1 g as a single oral dose; or doxycycline, 100 mg
orally twice a day for 7 days
Transmission to females results in increased risk of :
1. pelvic infl ammatory disease,
2. abdominal pain,
3. ectopic pregnancy,
4. infertility,
5. perinatal infection
Prostatitis:
Prostatitis is infection and/or inflammation of the prostate.
Classification of prostatitis :(National institute of health)
I Acute bacterial prostatitis (ABP)
II Chronic bacterial prostatitis (CBP)
III Chronic pelvic pain syndrome (CPPS)
IIIA Inflammatory CPPS (chronic nonbacterial prostatitis): WBC in expressed
prostatic secretions (EPS), VB3, or semen
IIIB Noninflammatory CPPS (prostatodynia): no WBC in EPS, VB3 or semen
IV Asymptomatic inflammatory prostatitis (histological prostatitis)
Epidemiology:
The most common type of prostatitis is NIH III chronic pelvic pain
syndrome, accounting for 90–95% of cases of prostatitis.
Acute and chronic bacterial prostatitis (NIH I and II) each makes up another
2–5% of cases.
Pathogenesis:
The tissues surrounding the prostatic acini become infi ltrated with
inflammatory cells (lymphocytes).

Surgery
UTI
Dr. Ismaeel
Lec. 42
The most common infective agents are gram negative Enterobacteriaceae
(Escherichia coli, Pseudomonas aeruginosa,Klebsiella, Serratia, Enterobacter
aerogenes).
From 5% to 10% of infections are caused by gram-positive bacteria
(Staphylococcus aureus and saprophyticus, Streptococcus faecalis).
Risk factors:
UTI;
acute epididymitis;
urethral catheters;
transurethral surgery;
intraprostatic ductal refl ux;
phimosis;
prostatic stones (corpora amylacea that can provide a nidus of infection for
chronic prostatitis).
Segmented urine cultures:
Also known as the Meares-Stamey or 4-glass test, segmented urine cultures are
useful in the:
1. Clinical evaluation of prostatitis syndromes and
2. Allow the localization bacteria to a specifi c part of the urinary tract by sampling
different parts of the urinary stream, with or without prostatic massage (which
produces EPS).
• VB1—first 10 mL of urine voided. Positive culture indicates urethritis or
prostatitis.
• VB2—midstream urine. Positive culture indicates cystitis.
• VB3—first 10 mL of urine voided following prostatic massage. Positive
culture indicates bacterial prostatitis.
• EPS—Positive culture indicates bacterial prostatitis.
Acute bacterial prostatitis
Acute bacterial prostatitis (NIH I) is infection of the prostate associated with
lower urinary tract infection and generalized sepsis.
Surgery
UTI
Dr. Ismaeel
Lec. 42
E. coli is the most common cause; Pseudomonas, Serratia, Klebsiella, and
enterococci are less common causes.
Clinical features:
Acute onset of fevers, chills, nausea and vomiting;
perineal and suprapubic pain;
irritative urinary symptoms (urinary frequency, urgency, and dysuria); and
obstructive urinary symptoms (hesitancy, strangury, intermittent stream or
urinary retention) are the hallmarks.
Signs of systemic toxicity (fever, tachycardia, hypotension) may be present.
Suprapubic tenderness and a palpable bladder will be present if there is
urinary retention.
On digital rectal examination, the prostate is extremely tender and
aggressive manipulation of the prostate is to be discouraged.
Treatment
If the patient is not systemically ill, use an oral quinolone such as ciprofl
oxacin 500 mg bid for at least 3 weeks.
For a patient who is ill, use IV gentamicin with a third-generation
cephalosporin or ampicillin, pain relief, anti-infl ammatory medications, and
relief of retention if present.
Complications:
1. Chronic prostatitis.
2. Prostatic abscess.
Chronic bacterial prostatitis:
NIH II classification of chronic bacterial prostatitis typically presents with
history of documented recurrent UTI.
E coli is responsible for 75–80% of cases, with enterococci and other gram-
negative aerobes responsible.
Chronic episodes of genitourinary pain and voiding dysfunction may be a
feature.
Surgery
UTI
Dr. Ismaeel
Lec. 42
DRE may show a tender, enlarged, and boggy prostate, or it may be entirely
normal.
Treatment:
An empiric trial of antibiotics is used if the evaluation suggests chronic
bacterial prostatitis and is administered long term (4–6 weeks).
Alfa blockers.
Surgical treatment: TURP.
Transurethral micro wave thermotherapy.
Other prostate infections
Prostatic abscess
Failure of acute bacterial prostatitis to respond to an appropriate antibiotic
treatment regimen (i.e., persistent symptoms and fever while on antibiotic
therapy) suggests the development of a prostatic abscess.
A transrectal ultrasound or CT scan (if the former proves too painful) is the
best way of diagnosing a prostatic abscess.
This may be drained by a transurethral incision.
Granulomatous prostatitis
This is a very uncommon form of prostatitis
Causes:
Most often it is idiopathic.
bacterial, viral, or fungal infection,
systemic granulomatous diseases,
the use of BCG to treat bladder cancer.
Clinical features:
Patients can present as with bacterial prostatitis.
Rectal examination is similar to prostate cancer (hard, indurated, nodular).
The diagnosis is usually made after prostate biopsy to rule out cancer.
Treatment:
Some patients respond to antibiotic therapy and temporary bladder drainage.
With histological evidence of eosinophilic granulomatous prostatitis,
steroids may be useful.
TURP may be necessary if there is no response to treatment and the patient
has bladder outlet obstruction.
