Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Aims of this lecture:
By the end of this lecture you are supposed to know:
and urological terms
-genital organs
Evaluation by:
Symptoms:
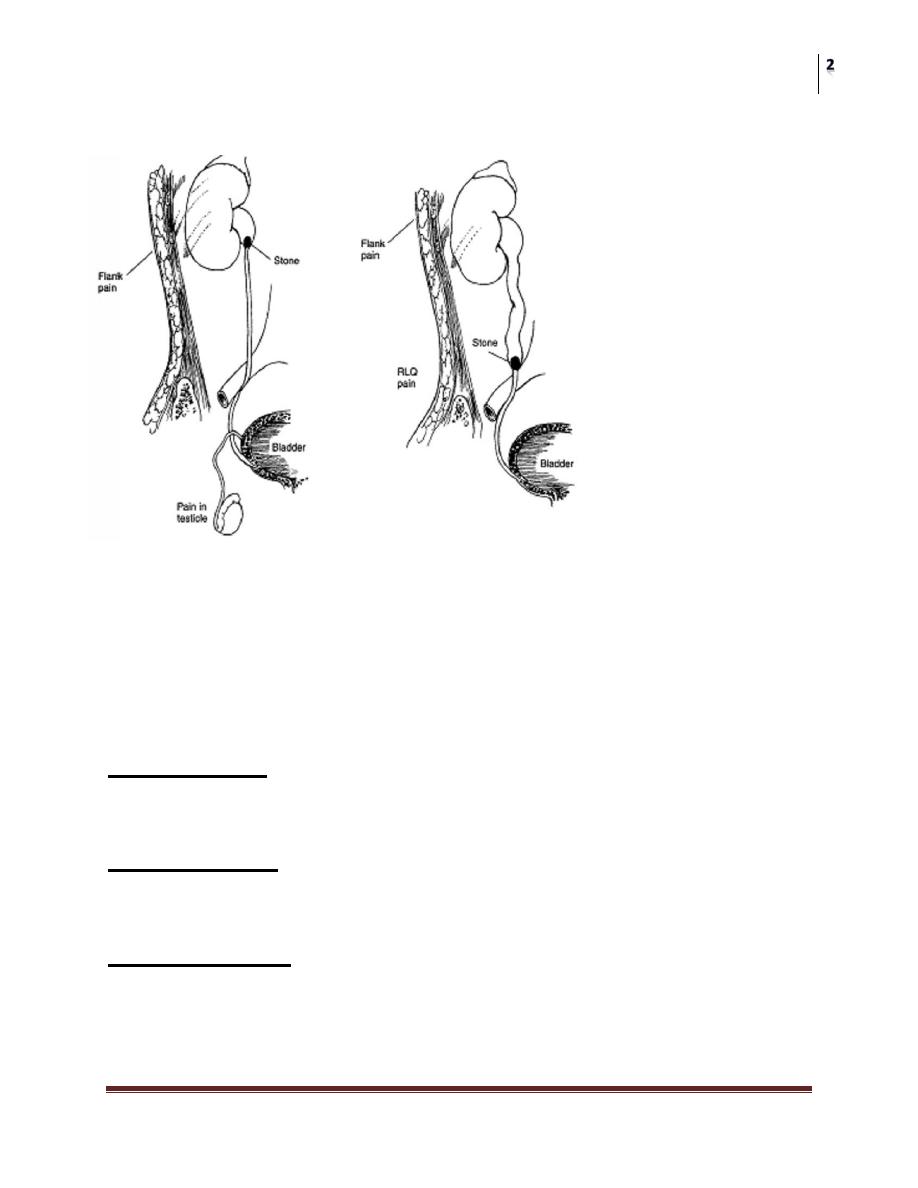
Flank pain/Loin pain/ renal pain
Dull pain
Colicky pain
Associated GI symptoms
Location
◦ Costo-vertebral angle
◦ Loin to groin.
DDx:
Passage of a stone
Clot or tumor colic
Uretero-pelvic junction obstruction.
Infection
Other less common causes: renal cystic disease.
Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Radiation:
Non urological causes
Vascular: aortic aneurysm
Medical: Pneumonia/pleurisy, MI
Musculoskeletal.
Gynecological and obstetric : Ectopic pregnancy
Gastrointestinal: Acute appendicitis
Neurological/spinal /Vertebral: spinal nerve root irritation.
Vesical Pain:
Vesical pain is usually produced either by overdistention of the bladder or by
inflammation. It should be related to the act of micturition
Prostatic Pain:
Prostatic pain is usually secondary to inflammation with secondary edema and
distention of the prostatic capsule.
Testicular Pain.
Scrotal pain may be either primary or referred. Primary pain arises from
within the scrotum and is usually secondary to acute epididymitis or torsion
of the testis or testicular appendices.
Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Chronic scrotal pain is usually related to noninflammatory conditions such
as a hydrocele or a varicocele, and the pain is generally characterized as a
dull, heavy sensation that does not radiate.
Scrotal pain
Pathology within the scrotum
Epididymitis, orchitis, epididymo-orchitis Torsion of the testicles,Torsion of
testicular appendages.
Testicular tumor (usually painless)
Referred pain
Ureteric colic
Inguinal hernia
Nerve root irritation or entrapment (ilioinguinal or genitofemoral).
Hematuria
Hematuria is the presence of blood in the urine.
Macroscopic (gross) hematuria is visible to the naked eye.
Microscopic or dipstick hematuria is when blood is identified by urine
microscopy or dipstick testing.
Microscopic hematuria
Is generally defined as 3 or more red blood cells (RBCs) per high-power
field on a centrifuged specimen confirmed on 2 of 3 properly collected
specimens.
Sometimes in females up to 5 RBC’s are considered normal.
Causes
Surgical (urological)
Cancer. described by PPP
Stones (urolithiasis).
Infection.
Inflammation.
Trauma (blunt and penetrating).
Renal cystic disease: e.g., medullary sponge kidney.
Congenital abnormalities: vesicoureteric reflux.
Prostatic: benign prostatic hyperplasia (BPH).
Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Medical (nephrological)
Systemic
Urological investigation of hematuria
Involves
Urine culture (if symptoms suggest urinary infection),
Urine cytology.
Upper tract imaging
Diagnostic cystoscopy?
If radiological investigation demonstrates a lesion suggesting a urothelial
carcinoma.
Asymptomatic Microscopic Hematuria recommends cystoscopy in all high
risk patients.
What is the best upper tract imaging study for the evaluation of hematuria?
US can detect masses, stones, or obstruction.
IVP is the traditional modality for urinary tract imaging.
CT is considered as the GOLD STANDARD modality for the evaluation of
urinary stones, renal masses, and renal infections.
Magnetic resonance imaging (MRI) is limited in the initial evaluation of
hematuria.
Retrograde pyelography (RPG) it is now considered of historical value in the
era of CT and MRI
Lower urinary tract symptoms (LUTS)
The classic prostatic symptoms of :
hesitancy, poor flow, frequency, urgency, nocturia, and terminal dribbling have in
the past been termed prostatism or simply BPH symptoms.
The new terminology (LUTS) is useful because it reminds the urologist to
consider possible alternative causes of symptoms, which may have
absolutely nothing to do with prostatic obstruction.
Overactive bladder
Is a newly defined symptom complex during which patients experience
urgency with or without urge incontinence, usually accompanied by
frequency and/or nocturia.

Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Lower Urinary Tract Symptoms
A. Irritative Symptoms
Frequency: Urinary frequency is due either to increased urinary output
(polyuria) or to decreased bladder capacity (anatomical of functional)
Nocturnia : is nocturnal frequency .
Dysuria: is painful urination.
Urgency: difficulty to inhibit desire to urinate
B-Obstructive Symptoms
Decreased force of urination.
Urinary hesitancy.
Intermittency.
Post voids dribbling.
Straining.
Incontinence
Urinary incontinence; is the involuntary loss of urine.
Types:
◦ Continuous Incontinence.
◦ Stress Incontinence.
◦ Urgency Incontinence.
◦ Overflow Urinary Incontinence.
◦ Mixed urinary incontinence (MUI).
Complete Urine Analysis
Urine analysis is a simple, non-invasive and cheap laboratory test that
rapidly provides valuable information about the urinary tract and other body
systems.
Complete urine analysis should be performed, even if one component part
shows no abnormalities.
Concurrent serum or plasma biochemical analysis is often required to gain
maximum benefit from urine analysis.
History
Method of collection
exam
intestinal conduit drainage bag is
NOT valid
Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
In men: clean the external meatus, discard the first 20mls, and collect the next
(MID-STREAM CLEAN CATCH)
In women:
Clean the vulva and urethral meatus, separate labia, and take the (MID-STREAM
CLEAN CATCH)
If satisfactory sample cannot be obtained, DO NOT hesitate to use a catheter
In children: use plastic bags (not suitable for bacteriology), in females do not
hesitate to use a catheter.
suprapubic aspiration is needed for culture.
Timing
A freshly voided specimen a few hours after a meal or genital examination
that is examined within one hour is the best.
Ideally the first morning sample is the best
Casts are particularly vulnerable to disintegration and will only be detected
if fresh urine is examined very soon after collection.
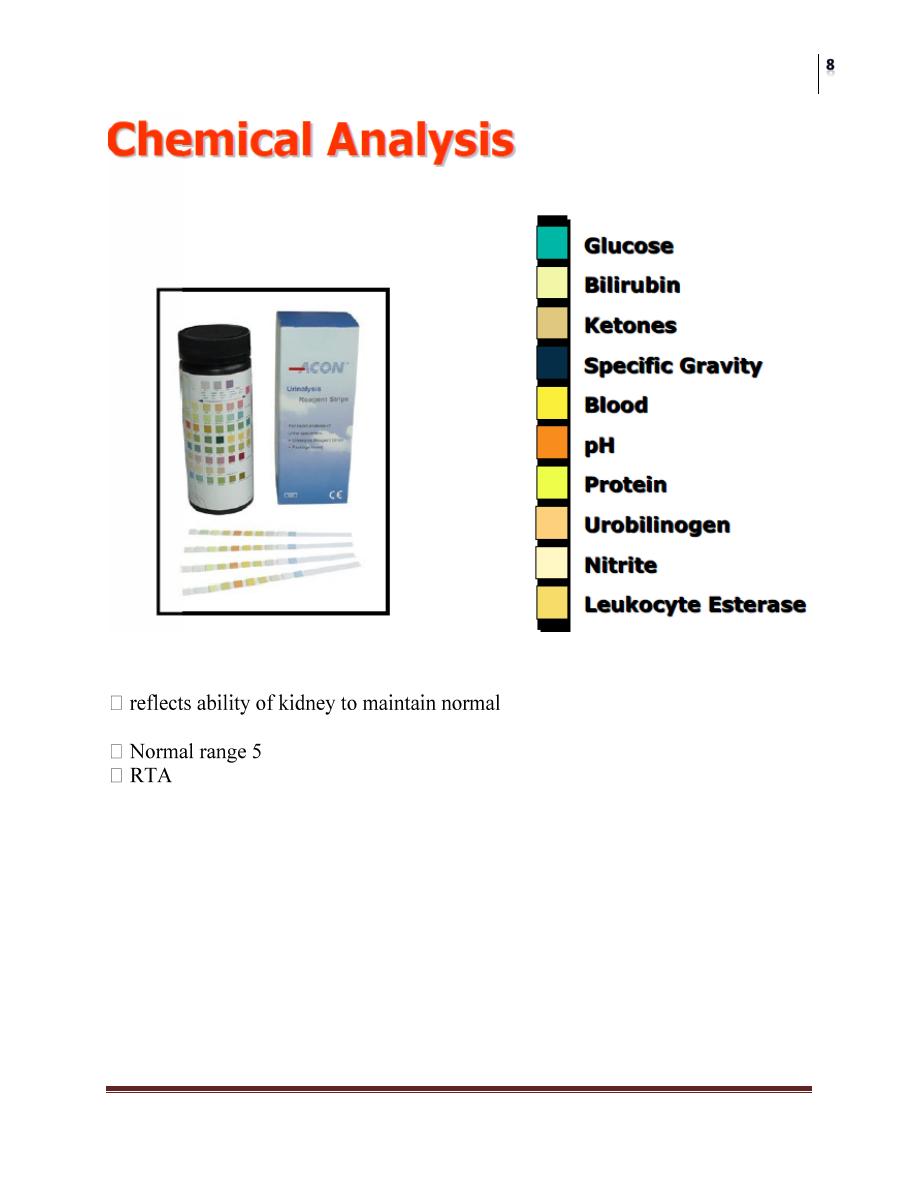
Parts of analysis
− Macroscopic (physical)
− Chemical (Dipstick)
− Microscopic
− Culture
− Cytological
Physical examination
Volume:
(0.5 -2.0 L/day)
Increased volume (Polyuria) > 2.0 L/day: -
Physiological: Excessive water and fluid intake.
Pathological:
Diabetes mellitus.
Diabetes insipidus
Chronic renal failure
Diuretics
Decreased volume (Oliguria) < 0.4 L/day:
Dehydration
Acute renal failure (prerenal, renal, postrenal)
Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
APPEARANCE
Normal fresh urine is clear.
Cloudy (turbid) urine is due to abnormal constituents (pus cells, bacteria,
salt or epithelial cells).
Colored:
− Colorless --- Diluted urine
− Deep Yellow --- Concentrated Urine, Riboflavin
− Yellow-Green --- Bilirubin / Biliverdin
− Red --- Bld / Hg/beets/rifamp/urisept
− Brownish-red --- Acidified Blood (Actute GN)
− Brownish-black --- metHb,Melanin,alkptnuria
− Smoky urine --- acute GN
− Orange urine --- concentrated/carotinoids(vit-A)
Color:
Normally urine is clear, and its color is pale yellow.
Odor:
Ammonia-like: Urea-splitting bacteria
Foul, offensive: Old, pus or inflammation
Sweet: Glucose
Fruity: Ketones
Specific gravity
Specific gravity
depends on the concentration of various solutes in the urine. It’s a good
indicator of renal concentrating ability.
1.003 to 1.030
hydrometer
refractometer
dipsticks
Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Urinary pH
hydrogen ion concentration in
plasma & ECF
-8 (average 6)
Protein
Normal urinary proteins
Protein % of Total Daily Maximum
Albumin 40% 60 mg
Tamm-Horsfall 40% 60 mg
Igs 12% 24 mg
Secretory IgA 3% 6 mg
Other 5% 10 mg
TOTAL 100% 150 mg

Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Glucose in urine
Normally no glucose in urine
Methods:
Benedict’s test (detects all reducing subs)
Dip-strips (glucose oxidase-peroxidase) (glucose specific)
Causes of glucosuria
With hyperglycaemia: diabetes, acromegaly, Cushing's disease,
hyperthyroidism, drugs like corticosteroids.
Without hyperglycaemia: renal tubular dysfunction
Hemoglobin:
dip-sticks are +ve in
So once positive, you should document the presence of RBC’s by
microscopy
Other tests:
Abnormal microscopic findings
Per High Power Field (HPF) (400x)
◦ > 3 erythrocytes
◦ > 5 leukocytes
◦ > 10 bacteria
Per Low Power Field (LPF) (200x)
◦ > 3 hyaline casts or > 1 granular cast
◦ > 10 squamous cells (indicative of contamination)
◦ Any other cast (RBCs,WBCs)
Presence of:
◦ Fungal hyphae or yeast, parasite, viral inclusions
◦ Pathological crystals (cystine, leucine, tyrosine)
◦ Large number of uric acid or calcium oxalate crystals
Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Crystals
Calcium oxalate (mono-and di-hydrate)
Calcium phosphate
urate ( amorphus, biurate, uric acid)
cystine
struvite
Drug related (sulphonamides…)
All are normal constituents of urine except struvite and cystine
Other tests on urine
Examination
Urinary tract imaging
Conventional radiographs
Intravenous urography
Ultrasound
CT scan
Nuclear scintigraphy
other contrast studies
Cystography
Urethrography
Regrograde pyelography
Plain radiographs
pre film in IVU
of imaging
-marks for kidneys, ureters, and bladder

Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
EXU
The Intravenous Urogram is the classic routine investigation of
Uroradiology
Technically satisfactory IVU demonstrates clearly and completely both the
renal parenchyma & the collecting system including the calyces, renal
pelvis, ureters and the urinary bladder and gives an indication of their
function
Indications
Suspected renal pathology (stone, mass…)
Hematuria
Complex UTI
Renal colic
Trauma
Contra-indications
Absolute
Relative
Preparation
Explain for the patient
Take consent
Hydration status (may need overhydration)
Bowel prep.
Laxative
Bladder emptying
Metformin
Complications
Allergic
Nephrotoxicity
Access related compl.
Cardio toxicity
Views
prefilm
nephrogram
ureterogram
Full bladder
Post voiding
Added views
Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Renal ultrasound
Basic principles
penetration
Doppler ultrasound :Scrotum CT scan
CT scan
The new standard imaging
Native vs. contrast
Density measured by HU
Stones, masses, trauma
CT
Isotope scanning
Organic molecule of interest is bound to radioactive isotope that emits
gamma rays
99mTc is usually used because of its short half-life of approximately 6 hours
A time-activity curve is recorded and compared to normal curves.
Can measure the split renal function and document the presence and degree
of obstruction.
Main types
Tc-MAG3
Cleared by tubular secretion, no glomerular filteration, well suited for renal
function, diuretic renogram, and plasma flow
Tc-DTPA
Cleared by glomerular filteration, used for renal function evaluation, less useful in
RF
Tc-DMSA
Binds to proximal tubule and retained there, thus images the renal parenchyma
looking for scaring.
Surgery
Evaluation of Urological Patients
Dr. Samir Ali
Lec. 29
Other tests
Cystography
Urethrography
VCUG
Loopography
nephrostography
Retrograde pyelography
MCQ:
What is the most common cause of gross hematuria in a patient older than 50
years of age?
a Renal calculi
b Infection
c Bladder cancer
d Benign prostatic hyperplasia
e Trauma
A common cause of chronic scrotal pain is:
a testicular torsion.
b trauma.
c cryptorchidism.
d hydrocele.
e orchitis.
