Chronic kidney disease: an update on diagnosis and management
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
What is chronic kidney disease stage 3 to 5?
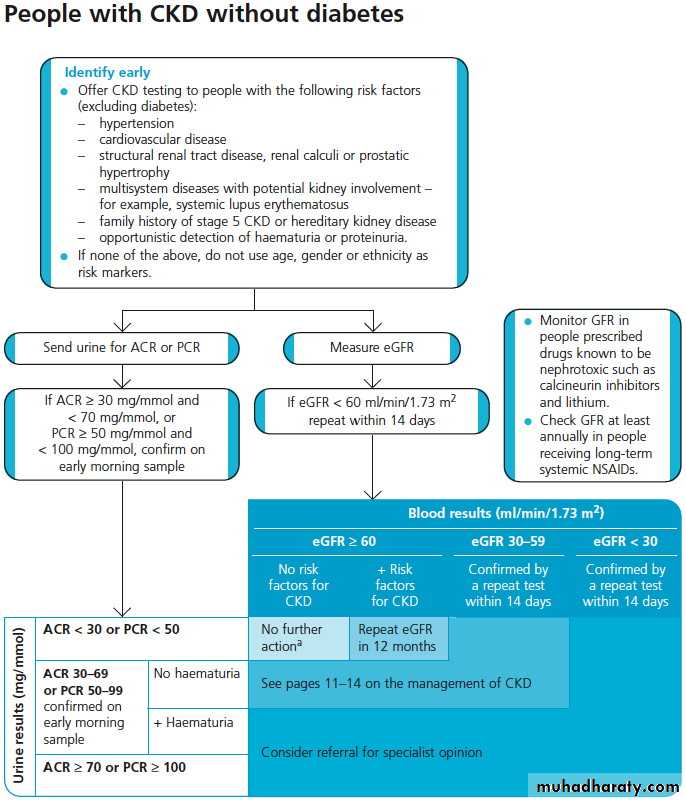
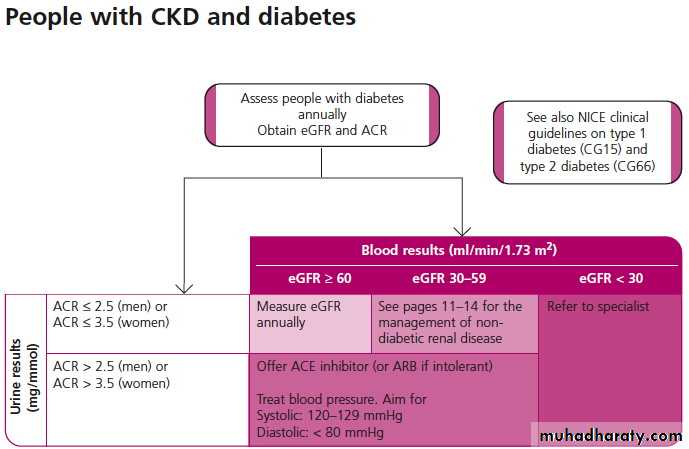
Patients with chronic kidney disease stage 3 to 5 have a moderate to severe decrease in their renal function. This means they have an eGFR less than 60 ml/min/1.73 m2 (for more than three months).How do I know what the eGFR is?
Most laboratories now report the eGFR along with creatinine using a validated equation. Note that this provides a reliable estimate in most patients, but underestimates GFR in African-Caribbean patients and in those with large muscle bulk, and overestimates it in those with low muscle mass (for example in very elderly people, and people who have had an amputation).It is important to remember that the eGFR is valid only if renal function is stable. You should also be aware that it is not valid in children or pregnant women.
How are stages 3 to 5 defined?
Stage 3 is a moderate decrease in GFR (30-59 ml/min/1.73 m2)
Stage 4 is a severe decrease in GFR (15-29 ml/min/1.73 m2)
Stage 5 is established chronic renal failure (<15 ml/min/1.73 m2)
Initial management
Practices can receive up to six points by recording the percentage of patients on the chronic kidney disease register whose notes have a record of blood pressure in the previous 15 months.Ongoing management
Practices can receive up to 11 points by achieving a blood pressure of 140/85 mm Hg or less in 70% of patients with chronic kidney disease.Practices can receive up to nine points by treating patients on the chronic kidney disease register with hypertension and proteinuria with an angiotensin converting enzyme inhibitor (ACE-I) or angiotensin receptor blocker (ARB) (unless a contraindication or side effects is recorded), in 80% of cases.
Practices can receive up to six points for measuring a urine albumin:creatinine ratio (ACR) or protein:creatinine ratio (PCR) test in the previous 15 months in 70% of patients with chronic kidney disease. (Since in patients without diabetes, proteinuria predicts a risk of progression.)
Limitations of the eGFR
Work through these case studies to learn more about using eGFR and its limitations.Case study 1
A 76 year old man with diabetes presents to the accident and emergency department. He has not attended his GP for reviews for the last five years. Blood tests show an eGFR of 24 ml/min/1.73 m2. Does he have stable chronic kidney disease and, if so, what stage is he at?
Because you do not know his previous eGFR values it is impossible to say whether his renal function is stable. You should assume he has acute renal failure until proved otherwise, although most such patients will not have acute renal failure.
Other reasons to suspect acute renal failure are:
A 50% rise in creatinine
A fall in eGFR of greater than 25%
Oliguria.
But the history is the most important tool for finding out whether a patient has acute or chronic renal failure.
Case study 2
A 45 year old African-Caribbean man has an eGFR of 58 ml/min/1.73 m2. Should you adjust his GFR in view of his African-Caribbean origin?
For patients of African-Caribbean origin you should multiply the eGFR by 1.2, unless the laboratory has already made this adjustment. Assuming it hadn't, you should record his eGFR as 58 x 1.2 = 69.6 ml/min/1.73 m2.
An 82 year old man has an eGFR of 55 ml/min/1.73 m2. Should you adjust his GFR in view of his advanced age?
You should not adjust his GFR or the reference ranges in light of his age. You should use the same criteria in patients from 18 years of age. However, if this man had been emaciated then his eGFR might be an overestimate.
Causes of chronic renal impairment
It is well known that the following conditions are associated with an increased risk of renal impairment:Diabetes
Hypertension
Vascular disease
Heart failure
Smoking
Low socioeconomic status.
But when assessing a patient it is important to think of other causes, such as obstruction to the flow of urine or systemic disease (such as systemic lupus erythematosus).
Case study 3
A 65 year old man has a raised creatinine and a reduced eGFR. He has never reported symptoms of bladder outlet obstruction. Does absence of symptoms exclude bladder outlet obstruction?An association between bladder outlet obstruction and chronic kidney disease has been demonstrated in men who have not reported symptoms. So you should still consider bladder outlet obstruction and specifically enquire about symptoms, and you should examine his abdomen for bladder enlargement.
Case study 4
A 56 year old woman presents with late onset asthma. Her eosinophil count is raised and urinalysis reveals protein 1+ and blood 2+. Creatinine is mildly elevated with an eGFR of 56 ml/min/1.73 m2. What type of problems should you consider?
Vasculitides can cause renal failure, and this pattern raises the possibility of Churg-Strauss syndrome. An anti-neutrophilic cytoplasmic antibody (ANCA) level would be a useful additional investigation.
Case study 5
A 50 year old man has moderate chronic kidney disease. Urinalysis reveals proteinuria 2+. What should you do next? Do you need to do a 24 hour collection of his urine?There is no need to do a 24 hour urinary collection. But you should send a midstream urine sample to the lab to detect a urinary tract infection. You should also send an early morning urine specimen to the lab to confirm proteinuria.
.
A positive test for proteinuria
would be:Urine protein:creatinine ratio >45 mg/mmol
Albumin:creatinine ratio >30 mg/mmol
or urinary protein excretion 0.5 g/24 h or more.
Persistent proteinuria means the patient has had proteinuria on two separate occasions, one or two weeks apart.
You should refer patients with a protein:creatinine ratio >100 mg/mmol to a nephrologist.
You should refer patients with a protein:creatinine ratio >45 mg/mmol who also have microscopic haematuria to a nephrologist.
Learning bite
Finding and treating a remedial cause of chronic kidney disease may occasionally improve renal function. For example, stopping non-steroidal anti-inflammatory drugs (NSAIDs) may improve renal function. But most management is directed towards slowing the rate of progression, and reducing vascular risk.Managing chronic kidney disease
Aimed at reducing the rate of decline in renal function and also at reducing cardiovascular risk.
Monitoring aims to:
Minimise risk factors for cardiovascular disease
Limit progression of kidney disease
Detect complications of renal impairment (such as metabolic bone disease, hyperkalaemia, and anaemia).
Minimising risk factors for cardiovascular disease is important.
Over 10 years a patient with stage 3 chronic kidney disease has a 25% chance of dying of cardiovascular disease, but less than a 5% chance of needing dialysis.
Key points
HaemodialysisTo detect and identify proteinuria, use urine albumin:creatinine ratio in preference, as it has greater sensitivity than protein:creatinine ratio for low levels of proteinuria.
For quantification and monitoring of proteinuria, protein:creatinine ratio can be used as an alternative. Urine albumin:creatinine ratio is the recommended method for people with diabetes.
Offer ACE inhibitors or angiotensin-II receptor blockers to non-diabetic people with chronic kidney disease and hypertension and urine albumin:creatinine ratio 30 mg/mmol or more (approximately equivalent to protein:creatinine ratio 50 mg/mmol or more, or urinary protein excretion 0.5 g/24 h or more).
Stage 3 chronic kidney disease should be split into two subcategories defined by:
GFR 45-59 ml/min/1.73 m2 (stage 3A)
GFR 30-44 ml/min/1.73 m2 (stage 3B).
Stages of chronic kidney disease (updated)
Stage*GFR (ml/min/1.73 m2)
Description
1
≥90
Normal or increased GFR, with other evidence of kidney damage
2
60-89
Slight decrease in GFR, with other evidence of kidney damage
3A
45-59
Moderate decrease in GFR, with or without other evidence of kidney damage
3B
30-44
4
15-29
Severe decrease in GFR, with or without other evidence of kidney damage
5
<15
Established renal failure
*Use the suffix (p) to denote the presence of proteinuria when staging CKD (recommendation 1.2.1).
For the purposes of classifying the stages of CKD define proteinuria as urinary urine albumin:creatinine ratio 30 mg/mmol or more, or protein:creatinine ratio 50 mg/mmol or more (approximately equivalent to urinary protein excretion 0.5 g/24 h or more).
In people with a new finding of reduced eGFR, repeat the eGFR within two weeks to exclude causes of acute deterioration of GFR - for example, acute kidney injury or initiation of ACE inhibitor therapy
Define progression as a decline in eGFR of more than 5 ml/min/1.73 m2 within one year, or more than 10 ml/min/1.73 m2 within five years
In people with chronic kidney disease aim to keep the systolic blood pressure below 140 mm Hg (target range 120-139 mm Hg) and the diastolic blood pressure below 90 mm Hg.
In people with chronic kidney disease and diabetes, and also in people with an urine albumin:creatinine ratio 70 mg/mmol or more (approximately equivalent to protein:creatinine ratio 100 mg/mmol or more, or urinary protein excretion 1 g/24 h or more) aim to keep the systolic blood pressure below 130 mm Hg (target range 120-129 mm Hg) and the diastolic blood pressure below 80 mm Hg.
Offer a renal ultrasound to all people with chronic kidney disease who:
• Have progressive chronic kidney disease (eGFR decline more than 5 ml/min/1.73 m2 within one year, or more than 10 ml/min/1.73 m2 within five years)• Have visible or persistent invisible haematuria
• Have symptoms of urinary tract obstruction
• Have a family history of polycystic kidney disease and are aged over 20
• Have stage 4 or 5 chronic kidney disease
• Are considered by a nephrologist to require a renal biopsy.
Advise people with a family history of inherited kidney disease about the implications of an abnormal result before a renal ultrasound scan is arranged for them.
If a patient with chronic kidney disease has anaemia you should first request haematinics to find out the cause - you shouldn't automatically assume that it is anaemia due to chronic kidney disease.
Detecting metabolic bone disease and anaemia
Case study 6You diagnose a 50 year old man with chronic renal failure. His corrected calcium level is 1.9 mmol/l. What should you do?
You should check this man's parathyroid hormone level and his 25-hydroxyvitamin D level. The guidelines state that because he has hypocalcaemia you should also refer him to a nephrologist.
Learning bite
In patients with chronic renal failure you should check calcium and phosphate levels as part of the initial assessment.You should also take a full drug history - the patient may be on nephrotoxic drugs such as lithium.
Case study 7
You check the serum parathyroid hormone level in a patient with moderate chronic kidney disease. The parathyroid hormone level is raised. What should you do?If the parathyroid hormone level is raised you should check the patient's 25-hydroxyvitamin D level. If this is low you should start ergocalciferol or colecalciferol. If the parathyroid hormone remains high despite this treatment you should refer the patient to a specialist.
Case study 8
A 50 year old woman with moderate chronic kidney disease has a haemoglobin level of 10 g/dl. She gets short of breath when walking. What should you do?
You should start by taking a history and examining her to exclude non-renal causes of her anaemia. You should also check her haematinics. You shouldn't automatically assume that the anaemia is due to her chronic kidney disease. If you do not find an alternative cause she will need epoetin. You should aim to achieve a haemoglobin of >11 g/dl but should take into account her levels of physical activity when deciding the target haemoglobin.
Learning bite
Epoetin increases the risk of hyperkalaemia. This is especially so when it is given in combination with an ACE inhibitor.Assessing cardiovascular risk
Case study 9A 60 year old man with moderate chronic kidney disease says he doesn't want further treatment or monitoring. He says he feels fine and that his condition hasn't harmed him so far. He smokes 10 cigarettes a day. How can you persuade him to take his condition seriously?
Chronic kidney disease stage 3 may progress to more severe renal impairment, but a greater risk is cardiovascular disease.
Chronic kidney disease appears to be an independent risk factor for vascular disease in most (but not all) studies. This means that even when other risk factors (diabetes, hypertension, hyperlipidaemia, and smoking) are accounted for, mild to moderate chronic kidney disease is still associated with a significant increase in cardiovascular mortality.
In patients with established vascular disease or at high risk of vascular disease, renal impairment significantly increases that risk independent of the other risk factors. He would therefore be well advised to:
Stop smoking
Attend for assessment of blood pressure, lipids, and glucose to allow his cardiovascular disease risk to be estimated
Consider therapy to limit risk if the assessment demonstrated this was appropriate.
Although current risk prevention charts underestimate risk in patients with chronic kidney disease, the Renal Association recommends you use the charts to make decisions on primary prevention of vascular disease.
Treatment options
You should consider using aspirin, statins, and ACE inhibitors.
At present there is insufficient evidence to support primary prevention of vascular disease unless you can recommend this based on the vascular risk assessed (without factoring in chronic kidney disease).
Case study 10
A 50 year old man has mild chronic kidney disease. He is anxious to adopt all lifestyle measures possible to stay healthy. How should you advise him? Is it safe for him to exercise? Should he drink alcohol?He should:
Stop smoking. Smoking is a risk factor for progression and stopping smoking can reduce progression of renal disease
Lose weight if he is overweight
Take regular aerobic exercise
Drink fewer than 3 units of alcohol per day (women should drink fewer than 2 units per day).
He takes all these measures and comes back to see you a month later. He had read that chronic kidney disease can affect his heart and wonders whether he should take aspirin. He is not known to have problems with his heart. How should you advise him?
You should estimate his 10 year risk of cardiovascular disease based on conventional charts. If it is greater than 20% you should consider prescribing aspirin.
Next he asks you whether he should take a statin. What should you advise?
Once again you should estimate his 10 year risk of cardiovascular disease based on conventional risk charts. If it is greater than 20% you should consider prescribing a statin.There is evidence that statins and ACE inhibitors are as effective in high risk patients with chronic kidney disease as in high risk patients without chronic kidney disease. The Renal Association recommends you offer primary prevention (statins and aspirin) if the 10 year cardiovascular disease risk reaches 20%.
The Renal Association recommends you offer primary prevention (statins and aspirin) if the 10 year cardiovascular disease risk reaches 20%.
Learning bite
If you do start patients with renal failure on a statin, you should remember that renal failure increases the risk of statin induced myositis. Untreated hypothyroidism also increases the risk of statin induced myositis.
Case study 11
A 59 year old woman has a moderate decrease in her GFR. Her blood pressure is 150/90 mm Hg. She does not have diabetes. Would she benefit from having her blood pressure lowered?Yes she would. Aggressive control of hypertension can reduce the rate of deterioration of renal function. The effect is most marked in people with proteinuria.8 9 The Renal Association recommends you follow the British Hypertension Society guidelines: a threshold for diagnosis of 140/90 mm Hg and a target of 130/80 mm Hg.10 Lowering blood pressure preserves renal function regardless of whether the patient has diabetes.
Low blood pressure is hard to achieve in older people and in people with diabetes and chronic kidney disease. But it is important. In patients with chronic kidney disease you should aim to reduce the blood pressure to 130/80 mm Hg (or to 127/75 mm Hg in patients with proteinuria).
Systolic pressures between 129 mm Hg and 110 mm Hg are associated with a decreased risk of progression of kidney disease.
ACE inhibitors and angiotensin receptor blockers are most effective for preventing further loss of kidney function in patients with chronic kidney disease.
Their effect is most marked in patients with proteinuria but they may be effective even in the absence of proteinuria. They would certainly be first choice in patients with established ischaemic heart disease or with cerebrovascular disease or diabetes.
Non-dihydropyridine calcium blockers should be considered in those intolerant of ACE inhibitors and angiotensin receptor blockers.
Case study 13
A 56 year old woman starts on lisinopril because she has chronic kidney disease. Her creatinine was 160 µmol/l before she started and it is now 200 µmol/l. What should you do?You should repeat the creatinine and check her potassium level. If it is still raised you should seek a specialist opinion on whether to continue the ACE inhibitor or investigate for renal artery stenosis. You should do this if the creatinine rises by more than 20% or the eGFR falls by more than 15%.
Learning bite
The Renal Association recommends monitoring every six months in patients with stage 3 chronic kidney disease.You should consider renal artery stenosis in patients with:
• Continuing hypertension despite taking three or more antihypertensive drugs
• Hypertension and unexplained hypokalaemia
• Recurrent episodes of flash pulmonary oedema (pulmonary oedema despite normal left ventricular function)
• A rising creatinine if they:
Have widespread atherosclerosis or
Are taking an ACE inhibitor.
A 57 year old man has moderate chronic kidney disease. He wonders whether it is safe to have the influenza vaccine. What should you advise?
You should advise him to have annual vaccination against influenza and also to have pneumococcal vaccination.
Patients with an eGFR of between 15 and 29 ml/min/1.73 m2 need an urgent referral (or a routine referral if the patient is known to be stable)
Patients with an eGFR of between 30 and 59 ml/min/1.73 m2 need a routine referral if they have:
A progressive fall in GFR
Microscopic haematuria (once urological causes have been excluded)
Unexplained anaemia or abnormal biochemistry
Suspected systemic illness
Blood pressure that is uncontrolled on three drugs.
You are worried that by following the guidelines your referral rates will rise dramatically. Should you refer everyone with chronic renal disease stages 4 and 5 to a specialist?
Some terminally ill patients will develop renal failure as part of a terminal event. These people will not need a referral. Referral will also be clearly inappropriate for some other patients.
Although anaemia in chronic kidney disease can be due to relative erythropoietin deficiency the possibility of blood loss, unconnected with his renal problems, needs to be investigated first. Monitoring his haemoglobin is not enough; you need to find out why he is anaemic.
You should first request ferritin and iron studies to investigate the cause of his anaemia. He may need erythropoietin if you exclude other causes of his anaemia.
The Renal Association recommends monitoring every six months in patients with stage 3 chronic kidney disease
Measure serum calcium, phosphate, and PTH concentrations in people
with stage 4 or 5 chronic kidney disease (GFR less than < 30 ml/min/1.73 m2).The routine measurement of calcium, phosphate, parathyroid hormone (PTH), and vitamin D levels in people with stage 1, 2, 3A, or 3B chronic kidney disease is not recommended.
When vitamin D supplementation is indicated in people with chronic kidney disease offer:
Cholecalciferol or ergocalciferol to people with stage 1, 2, 3A, or 3B chronic kidney disease1-alpha-hydroxycholecalciferol (alfacalcidol)
or 1,25-dihydroxycholecalciferol (calcitriol) to people with stage 4 or 5.Monitor serum calcium and phosphate concentrations in people receiving
1-alpha-hydroxycholecalciferol or1,25-dihydroxycholecalciferol supplementation.
Learning bite
Offer bisphosphonates if indicated for the prevention and treatment of osteoporosis in people with stage 1, 2, 3A, or 3B chronic kidney disease.
You should encourage people with chronic kidney disease to take exercise, achieve a healthy weight, and stop smoking.
An appropriately trained professional should discuss the risks and benefits of dietary protein restriction, with particular reference to slowing down the progression of disease versus protein-calorie malnutrition, and supervision to ensure malnutrition is prevented. Offer dietary advice to concerning potassium, phosphate, protein, calorie, and salt intake when indicated.
Learning bite - statins and antiplatelet drugs
The use of statin therapy for the primary prevention of cardiovascular disease in people with chronic kidney disease should not differ from its use in people without chronic kidney disease and should be based on existing risk tables for people with and without diabetes. It should be understood that the Framingham risk tables significantly underestimate risk in people with chronic kidney disease.Offer statins to people with chronic kidney disease for the secondary prevention of cardiovascular disease irrespective of baseline lipid values.
Offer antiplatelet drugs to people with chronic kidney disease for the secondary prevention of cardiovascular disease.
Chronic kidney disease is not a contraindication to the use of low dose aspirin but clinicians should be aware of the increased risk of minor bleeding in people with chronic kidney disease given multiple antiplatelet drugs.
There is insufficient evidence to recommend the routine use of drugs to lower uric acid in people with chronic kidney disease who have asymptomatic hyperuricaemia