A mother's heartache peripartum cardiomyopathy
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
Contents
A case presentation. At each stage of the case, you will be asked how you would manage the situationInformation on the definition, incidence, and diagnosis of peripartum cardiomyopathy
Information on the treatment and prognosis of peripartum cardiomyopathy
Information on spontaneous coronary artery dissection.
•
• A 35 year old Caucasian woman was breastfeeding her baby when she developed chest pain and became breathless. The pain, which was substernal and non-pleuritic, was described as being "sharp, stabbing, and throbbing." It lasted for about an hour and a half, and was not accompanied by a cough or haemoptysis.Ten days previously, this patient had undergone an uneventful elective caesarean section, the pregnancy (her second) having proceeded to term without any complications.
Operative delivery was required because of pelvic deformities from a horseriding accident many years ago. She worked as a chef, smoked 10 cigarettes a day, and was on no medication. She also denied the use of illicit drugs.
When first seen, she looked anxious, and had a heart rate of 105 beats/min. Her temperature, blood pressure, and respiratory rate were all normal.
The jugular venous pressure was raised by 3 cm. She had a third heart sound, a systolic murmur at the lower left sternal edge, and normal breath sounds. There were no marfanoid features or signs of a deep venous thrombosis.
Results of the initial laboratory investigations are shown in table 1.
Table 1 Initial investigations
Haemoglobin: 14.0 g/dl (13.5-18.0 g/dl)WBC: 11.6 x 109/l* (4.0-11.0 x 109/l)
Platelets: 480 x 109/l* (150-400 x 109/l)
INR: 1.02
D-dimer: 0.55 µg/ml* (0-0.23 µg/ml)
Troponin I: 0.65 µg/l* (0 - 0.04 µg/l)
Urea and electrolytes, liver enzymes, and C reactive protein: within reference limits
• The patient's chest x ray revealed a normal cardiac silhouette with distended upper lobe pulmonary veins. The lung fields were clear and there was no pneumothorax.
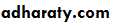
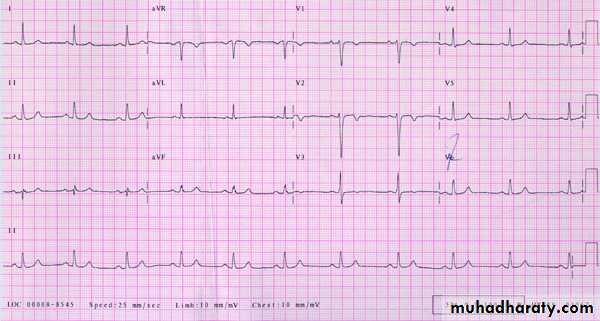
• Figure 1 shows the patient's initial ECG
•
Viral serology, iron studies, serum ACE assay, and autoimmune screens were found to be normal or negative. The patient's serum troponin I concentration, however, continued to rise, eventually reaching a peak of 2.17 µg/l one week after admission.
Although her breathlessness settled on treatment, she remained troubled by intermittent chest pain. The latter was not typical for angina pectoris, in that it was often reproducible by chest wall palpation alone. These symptoms, and the raised troponin readings, were both attributed to her putative cardiomyopathy. She was reassured, and given simple analgesia for symptom control.
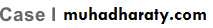
Then, on the sixth day of her stay, a routine ECG (fig 3) showed sudden and dramatic changes when compared to a tracing done 24 hours earlier. The T waves in the chest leads, which were previously inverted, had become upright.
• Figure 3 ECG 2
•
These abrupt ECG changes suggest myocardial ischaemia, and angiography is the only rapid way to arrive at a definitive answer as far as the coronary arteries are concerned.
Learning point
At angiography, a coronary artery dissection may be recognised on the basis of one or more of :The presence of an intimal flap within the lumen
Delayed clearanc e or "hang-up" of contrast .
An unusually narrow coronary artery with atypically smooth vessel walls
Loss of arterial side branches whose origin is cut off by the dissection.
Reflux of contrast back into the coronary sinus on dye injection.
Spontaneous coronary dissection has an association with aortic dissection, particularly in the context of pregnancy. Further imaging of the aorta is therefore indicated. This can be done by contrast enhanced computed tomography, magnetic resonance imaging, or transoesophageal echocardiography.
Although coronary stenting has a role in the treatment of this condition, it is not mandatory in all cases. Conservative medical treatment or even urgent coronary artery bypass graft surgery may be preferable in some situations. The precise treatment employed depends on the individual circumstance, and is influenced by both the location and the extent of the dissection. Spontaneous coronary artery dissection is rare.
Spontaneous coronary artery dissection
uncommon cause of coronary artery occlusion that may result in myocardial infarction or sudden death.Spontaneous coronary artery dissection has a predilection for women in the third or fourth decade of life who are in the puerperal period or the last trimester of an otherwise normal pregnancy. Very often, these women have no risk factors for atherosclerosis. It is estimated that
15% of all intrapartum myocardial infarctions are caused by spontaneous coronary artery dissection.
Coronary artery dissection may also occur in the context of Marfan's syndrome, Ehlers-Danlos syndrome, alpha1-antitrypsin deficiency, severe exercise or retching, cocaine abuse, chest trauma, and during coronary interventions.
In the latter situations, however, the arterial dissection is not strictly "spontaneous."
Relatively little is known about the disease mechanisms that underlie spontaneous coronary artery dissection. Why this condition has a tendency to occur in the peripartum period is also unclear. Based on the frequently reported observation of a periadventitial eosinophilic infiltrate at the site of the dissection, it has been proposed that eosinophils may play apathogenic role in this disease.
Patients who survive the initial onslaught of spontaneous coronary artery dissection typically present with an acute coronary syndrome. Aside from ECG changes and a rise in cardiac troponins, segmental wall motion abnormalities may be seen at echocardiography. Coronary angiography, however, is the key investigation that will secure the diagnosis.
Other imaging modalities like multi-slice CT scanning and transoesophageal Echocardiography may also highlight the presence of an intimal flap within the proximal coronary arteries. The left anterior descending artery appears to be the most frequently affected vessel, followed, in order, by the right coronary artery, circumflex vessel, and the left main stem. Simultaneous multivessel involvement is well described.
As illustrated by this case report, women with spontaneous coronary artery dissection tend to dissect their left coronary arteries. In contrast, the right coronary artery tends to be the site of dissection in men. The reason for this dichotomy is unknown. Spontaneous coronary artery dissection may be associated with an aortic root or arch dissection. Furthermore, coronary dissection may recur in a different location weeks or months after the index event.
In the absence of randomised controlled data comparing the various therapeutic modalities, there is currently no consensus as to how patients with spontaneous coronary artery dissection ought to be managed.
Treatment is therefore tailored to the individual. The options are:
Conservative management with aspirin and/or heparin, nitrates, beta blockers, and ACE inhibitors, particularly if symptoms have settled and there is no evidence of ongoing ischaemia, either at rest or on exertion.
The use of thrombolytic treatment in spontaneous coronary artery dissection is controversial. Although it may lyse the blood clot within the false lumen (and thereby improve blood flow down the true lumen), it may equally expand the haematoma and aggravate the dissection.
Lately, glycoprotein IIb/IIIa inhibitors have also been used to treat spontaneous coronary artery dissection .
Emergency percutaneous coronary intervention with stent insertion
Emergency bypass grafting, particularly if there is left main stem or three vessel dissection and haemodynamic instability.The prognosis of spontaneous coronary artery dissection is variable and probably related to the site and number of vessels involved, and the extent of myocardial damage. It is reported that more than half of patients with spontaneous coronary artery dissection die suddenly.
However, those who live through the acute episode have a good prognosis: the 30 month survival rate is approximately 80%, regardless of the treatment received.
Cardiac troponin I is not affected by a normal pregnancy, prolonged labour, or operative delivery
D-dimer values rise continuously during the course of a normal pregnancy, so much so that it often exceeds the cut off limit for the control (non-pregnant) population by the time the woman is in her third trimester. During the 40th week of a normal pregnancy, for example, values as high as 1 µg/ml may be obtained.
Definition, incidence, and diagnosis of peripartum cardiomyopathy
Is an uncommon and potentially life threatening condition that presents as heart failure in thelast month of pregnancy or within five months of delivery. It is a diagnosis of exclusion, made only in the absence of an identifiable cause for the heart failure and in the absence of heart disease before the last month of pregnancy.
The diagnosis must be supported by objective evidence of new left ventricular systolic dysfunction, demonstrated, for example, by echocardiographic criteria (ejection fraction <45% or fractional shortening <30%).
In the West, peripartum cardiomyopathy is estimated to afflict between 1 in every 3000 to 1 in every 4000 live births. The incidence is higher in Africa.
Risk factors for peripartum cardiomyopathy include multiparity,
advanced maternal age,
twin or multifetal pregnancy,
prolonged tocolysis,
pre-eclampsia, and
gestational hypertension.
Peripartum cardiomyopathy has a predilection for Afro-Caribbean women.
Even though the cardiomyopathy is described as "peripartum," most women present in the postpartum period, primarily within four months of delivery; only a small minority (less than 15%) are identified antepartum
The patient's aortic root and proximal aorta appeared normal on a contrast enhanced CT.
After weighing up the various aspects of her condition (the lack of ischaemic cardiac symptoms, the absence of further ECG changes, a falling troponin concentration, and the presence of feeding collaterals to her blocked left anterior descending artery), the decision was eventually taken to manage this patient's coronary dissection conservatively. Aspirin was added.On day 11, an echocardiogram revealed substantial improvement to both the size and the function of her left ventricle. Only a modest degree of anterioapical and apicolateral hypokinesia was seen. At a treadmill test just before discharge (day 20), she managed to complete nine minutes of the Bruce protocol, stopping because of fatigue. Although her blood pressure response to exercise was blunted, there were no ECG changes to suggest inducible cardiac ischaemia.
In outpatients a month later, she reported excellent physical recovery, and was essentially asymptomatic. Her ECG (fig 4), which bore the stigmata of an old anterior infarction, also showed nascent R waves in the septolateral leads.
Figure 4 ECG 3
In addition, near normal wall motion was observed when the infarct related segments of her heart were examined with ultrasound. The left ventricular ejection fraction was calculated at 52%.Establishing a diagnosis of spontaneous coronary artery dissection requires a high degree of clinical suspicion. The relative rarity of the condition and its tendency to occur in the puerperal period means that it may be confused with peripartum cardiomyopathy, atherosclerotic myocardial infarction, or even pulmonary embolism, all of which overlap to a greater or lesser extent in their presentation.
This point is illustrated in the case recounted above. With hindsight, the presence of subtle segmental wall motion abnormalities on echocardiography should perhaps have prompted us to arrange early coronary angiography, to exclude coronary artery disease. Among other learning points therefore, this report highlights the potential dangers of diagnostic parsimony (see Occam's razor below), particularly when dealing with the postpartum patient with cardiac symptoms.
The aetiology of peripartum cardiomyopathy remains speculative. Possible causative factors for the condition include myocarditis, immune dysregulation during pregnancy, genetic susceptibility, an abnormal response to the increased haemodynamic stresses of late gestation, and the influence of pregnancy hormones and proinflammatory cytokines.
Although widely suspected, there is currently no convincing evidence of a causative link between cardiotrophic viruses and peripartum cardiomyopathy.
Occam's razor
"Pluralitas non est ponenda sine necessitate"Named after William of Ockham, a controversial 14th century theologian, Occam's razor refers to a well known philosophical principle - the parsimony of explanations. Translated from its original Latin form, the principle states: "Plurality must not be posited without necessity." In modern parlance, this roughly means: "Keep it simple."
Occam's razor is widely applied in scientific thinking, and is also adopted in clinical medicine, when one best explanation is used to account for a given combination of symptoms and signs. Although an important intellectual tool, the razor should not be wielded rigidly, because many illnesses turn out to be more complicated than expected.
William was born in 1285, in the village of Ockham in Surrey, England. He joined the Franciscan order in his youth, and then studied and taught theology at Oxford. His career in England did not get very far, however, for he was later expelled from the university, and then excommunicated from the church, for expounding heretical views on Catholic teaching. William fled to Germany, where he was granted asylum by Ludwig IV of Bavaria. There, he continued writing against the papacy, generating a series of treatises on the power of the Pope and civil governance. He is thought to have died in 1349, in a convent in Munich, a victim of the Black Death.
Summary
Peripartum cardiomyopathy
Diagnostic criteria
Development of cardiac failure in the last month of pregnancy or within five months of delivery
Absence of another identifiable cause for the heart failure.
Absence of heart disease prior to the last month of pregnancy.
Presence of left ventricular systolic dysfunction on echocardiography (fractional shortening <30% and/or ejection fraction <45%)
Epidemiology of peripartum cardiomyopathy
In the West, peripartum cardiomyopathy is thought to occur in between 1 in 3000 and 1 in 4000 live births.The disease has a predilection for Afro-Caribbean women, although all races can be affected.
Recognised risk factors for the condition include:
• Multiparity
• Advanced maternal age
• Twin or multifetal pregnancy
• Delay during delivery
• Pre-eclampsia or gestational hypertension.
Subsequent pregnancy
Following peripartum cardiomyopathy, a woman's ability to tolerate another pregnancy is closely related to the cardiac size and function.If left ventricular impairment persists for one year following the patient's index episode, then the risk of death in a subsequent pregnancy is nearly 20%.
However, if left ventricular function is normal, then her risk of death is probably small,
although there is a significant chance (approximately 20%) of a symptomatic relapse of heart failure and further (possibly permanent) loss of cardiac function.
Spontaneous coronary artery dissection
Is an uncommon cause of myocardial infarction and sudden death.It has a predilection for women in the third or fourth decade of life and also in the puerperal period or the last trimester of pregnancy.
Very often, these women have no risk factors for atherosclerosis.
may occur in patients with:
Marfan’s syndrome
Ehlers-Danlos syndrome
Alpha1-antitrypsin deficiency
Severe exercise or retching
Cocaine abuse
Chest trauma.`
Clinical presentation
Diagnosis of spontaneous coronary artery dissection requires a high degree of clinical suspicionPatients who do not die suddenly typically present with an acute coronary syndrome
There are usually ECG changes and a rise in cardiac troponins, and regional wall motion abnormalities on echocardiography
The diagnosis is confirmed by coronary angiography
The LAD is the most frequently affected vessel, followed, in order, by the right coronary artery, circumflex artery, and the left main stem
Simultaneous multi-vessel involvement is well described.
Women tend to dissect their left coronary arteries. In contrast, the right coronary artery tends to be the site of dissection in men
Spontaneous coronary artery dissection may be associated with an aortic root or arch dissection. Furthermore, arterial dissection may recur in a different coronary location weeks or months after the index event
Angiographic features of coronary artery dissection
• Presence of an intimal flap within the lumen of the artery• Delayed clearance or "hang-up" of contrast in the vessel
• An unusually narrow coronary artery with atypically smooth vessel walls
• Loss of arterial side branches which are cut off by the dissection
• Reflux of contrast back into the coronary sinus on dye injection.
The histological abnormalities in peripartum cardiomyopathy are non-specific, and are similar to other forms of dilated cardiomyopathy. In particular, a degree of myocardial inflammation is often present. The frequency of this finding varies with different reports, but appears to be in excess of 50% in the more recent studies.
Of the 42 patients with peripartum cardiomyopathy that were enrolled into the study by Felker et al, for example, 62% had evidence of myocarditis on endocardial biopsy.
Peripartum cardiomyopathy tends to present relatively acutely, with clinical features that are typical of decompensated heart failure.
Because many women in the final weeks of a normal pregnancy also experience breathlessness, ankle oedema, and fatigue, a degree of suspicion is required in order to identify the rare patients with peripartum cardiomyopathy from this population of women.
Two other well described presenting complaints are chest pain and haemoptysis, either of which may confuse the initial clinical evaluation. In peripartum cardiomyopathy, the ECG may reveal normal sinus rhythm, sinus or ventricular tachycardia, T wave inversion, anteroseptal Q waves, or diffuse and non-specific ST-T changes. Very often, variable degrees of pulmonary congestion and cardiac enlargement are observed on chest x ray.
As mentioned, transthoracic echocardiography is required to provide evidence of left ventricular systolic dysfunction, and to rule out other causes of heart failure, such as valvar heart disease. An endocardial biopsy is not strictly required for diagnosis, although some authorities suggest a potential role for immunosuppressive drugs if there is histological evidence of myocarditis.
Although warfarin crosses the placenta and has the potential to cause both an embryopathy (during the first trimester of pregnancy) and fetal bleeding (in late gestation), it may still be used between the 12th and 36th week of a pregnancy - for example, by a woman with a metallic heart valve.
Low molecular weight heparin does not cross the placental barrier.
Note that the prolonged use of heparin during pregnancy may result inmaternal osteopenia,
thrombocytopenia, and
alopecia.
The use of beta blockers during pregnancy is associated with babies that are small for their gestational age. This is not the same as fetal microcephaly.
Whereas angiotensin converting enzyme (ACE) inhibitors should be avoided during pregnancy (because of very serious effects on the fetus), currently available data indicate that only small amounts of these drugs are secreted into breast milk. This makes them relatively safe for use by nursing mothers.
Management of patients with peripartum cardiomyopathy
Drug treatment is currently focused at the support of the patient's cardiac function. In this respect, it is no different from the treatment of other forms of congestive cardiomyopathy.Because of the high incidence of thromboembolic complications in this condition, systemic anticoagulation is recommended.
There may be a role for steroids and immunosuppressive drugs in patients with biopsy evidence of myocarditis who fail to improve after two weeks of standard heart failure therapy. The use of these drugs for this indication, however, is not supported by randomised controlled data.
In those who are acutely unwell, intravenous nitrates and inotropic agents should be considered.
However, a minority will continue to deteriorate despite maximal medical therapy.
The use of balloon pump and left ventricular assist devices or other support devices may help - either alone or as a bridge to cardiac transplantation.
• Outcome
• In earlier reports, the maternal mortality rate of peripartum cardiomyopathy was estimated to be between 25% and 50%.
• Recent data, however, suggest a much better prognosis. In a stringently defined case series of subjects (n=42) who were followed for a median duration of eight and a half years, the incidence of death and the need for cardiac transplantation were found to be 7% each. Most patients improved spontaneously.
•
Survival appears to depend on the recovery of cardiac size and function within six months of delivery. The outlook is poor if left ventricular dysfunction persists six to 12 months after the initial presentation. In this subgroup of patients, the five year mortality rate may be as high as 85%.
Treatment and prognosis of peripartum cardiomyopathy
There are no randomised controlled data to guide the management of peripartum cardiomyopathy, and the condition is currently treated in exactly the same way as other forms of heart failure. Because of the high incidence (up to 50%) of thromboembolic complications in this condition, anticoagulation is also recommended.In general, the drugs that are commonly used in heart failure (including ACE inhibitors) only get into the breast milk in small quantities. It is therefore important, particularly in Africa where peripartum cardiomyopathy is more prevalent, that the infant is not denied breast milk, which may be the only safe nutrition available for the newborn.
A minority (less than 15%) of all cases of peripartum cardiomyopathy will fail to respond to maximal medical treatment, including inotropic support. In these individuals, an intra-aortic balloon pump or a ventricular assist device may be deployed as a bridge to cardiac transplantation. Transplantation in this context is associated with a survival rate that is comparable to those of age matched women undergoing heart transplantation for other reasons.
The role of immunosuppressive (prednisolone and azathioprine) or immunomodulatory (intravenous immunoglobulins) treatment in peripartum cardiomyopathy is unclear.
Studies on this subject have either involved relatively small numbers of patients and were not prospective randomised controls. This last point is important, because most patients with peripartum cardiomyopathy demonstrate spontaneous resolution of left ventricular dysfunction, thereby creating an important confounding factor in studies which are unblinded and have no controls.
Despite these uncertainties, an expert panel on peripartum cardiomyopathy recently concluded that there may be a role for immunosuppressive therapy in patients with definite biopsy evidence of myocarditis who fail to improve after two weeks of standard heart failure treatment.
In earlier reports, the maternal mortality rate in peripartum cardiomyopathy was estimated to be 25-50%, with nearly half of all deaths occurring in the first three months of the postpartum period. More recently, a stringently defined case series of tertiary referral subjects (n = 42) who were followed for a median duration of approximately eight and a half years reported the incidence of death and the need for cardiac transplantation at 7% each.
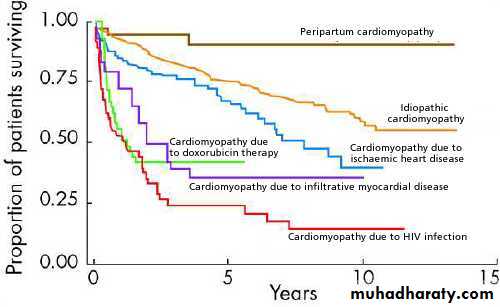
The same group also found that women with peripartum cardiomyopathy had a substantially better prognosis when compared to patients with other forms of heart failure - the five year survival rate of their peripartum cardiomyopathy cohort was 94% (fig 2).
• Figure 2 Adjusted Kaplan-Meier estimates of survival according to the underlying cause of cardiomyopathy.
•
Survival in peripartum cardiomyopathy appears to depend on the recovery of cardiac size and function within six months of delivery. The outlook is poor if left ventricular dysfunction persists 6-12 months after initial presentation. In this group of patients, the five year mortality rate may be as high as 85%. Notably, the presence of myocarditis on endocardial biopsy does not appear to correlate with clinical outcome.
The advisability of further pregnancy for a woman with a history of peripartum cardiomyopathy remains a difficult issue to address, because subsequent pregnancy in this situation is associated with further loss of cardiac function, symptomatic deterioration, and even maternal death. The risk of such outcomes may be stratified according to the patient's ventricular systolic function 12 months after her index episode of heart failure.
In women with persistent ventricular impairment (ejection fraction <50%) following peripartum cardiomyopathy, the risk of death in a subsequent pregnancy is nearly 20%.
If left ventricular function is normal, then the risk of maternal death in the next pregnancy is probably low, although there is a significant chance (approximately 20%) of a symptomatic relapse of heart failure and further (possibly permanent) loss of cardiac contractile function.
Peripartum cardiomyopathy is associated with a five year survival rate that is much better than that of idiopathic dilated cardiomyopathy.
Peripartum cardiomyopathy presents as heart failure in the last month of pregnancy or within five months of delivery.
Biopsy evidence of myocarditis does not carry a worse prognosis.
The diagnostic criteria for peripartum cardiomyopathy are as follows:
• Development of cardiac failure in the last month of pregnancy or within five months of delivery• Absence of another identifiable cause for the heart failure
• Absence of heart disease prior to the last month of pregnancy
• Presence of left ventricular systolic dysfunction on echocardiography (fractional shortening <30% and/or ejection fraction <45%)
The risk of peripartum cardiomyopathy is increased in a twin pregnancy.
Chronic alcohol abuse is not a known risk factor for peripartum cardiomyopathy.
Peripartum cardiomyopathy improves with ACE inhibitors and beta blocking agents in at least 50% of cases.
There is no proved association between peripartum cardiomyopathy and Coxsackie.
Peripartum cardiomyopathy occurs most often in the postpartum period.
Treatment with immunosuppressive drugs has not been proved to improve outcome.
Spontaneous coronary artery dissection has a particular tendency to occur in women who are in the peripartum period.
Spontaneous coronary artery dissection is not associated with Klinefelter's syndrome.
Spontaneous coronary artery dissection is not associated with pre-eclampsia in pregnancy.
Spontaneous coronary artery dissection presents as sudden death in a significant number of sufferers.
It tends to involve the left coronary artery in women and the right coronary artery in men.
D-dimer values rise continuously during the course of a normal pregnancy, so much so that it often exceeds the cut off limit for the control (non-pregnant) population by the time the woman is in her third trimester. During the 40th week of a normal pregnancy, for example, values as high as 1 µg/ml may be obtained.
Cardiac troponin I is not affected by a normal pregnancy, prolonged labour, or operative delivery.