Tuberculosis: new insights in diagnosis and management
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
"Tuberculosis affects 9 million people a year across the world and it kills 2 million of these people. In the UK prevalence rates have been steadily increasing for almost 20 years and the most recent figures suggest an unexpectedly sharp increase. It is a disease of increasing importance in the UK and we should know how to recognise and treat it."
Figure 1. Pulmonary tuberculosis in a 48 year old man. Soft shadowing is shown in both upper lobes with cavitation on the right. This picture is characteristic of tuberculosis in an HIV negative person.
A number of studies have shown that smoking increases the risk of tuberculosis two- to fivefold. A study in India showed that tuberculosis is the most common cause of death in smokers. This is probably due to suppression of alveolar macrophages by substances in the cigarette smoke.
Body build is known to influence the likelihood of tuberculosis. Being tall and thin may increase the risk by 50%. Being short and overweight may decrease risk by about a third. The reasons for this are not clear but may be because Mycobacterium tuberculosis causes infection in the upper lobes where blood perfusion is least. In a tall, thin person this trend may be accentuated. George Orwell is an example of a tall, thin smoker who had tuberculosis.
Figure 2. George Orwell was tall and thin and a smoker. He died from tuberculosis.
In the older half of the UK population, men outnumber women by three to one in notifications for tuberculosis. It is possible that genetic factors in women are protective. Other evidence suggests that any sex difference may be due to differing smoking patterns.Learning bite
For the treatment of patients with latent tuberculosis you can give:6 months of isoniazid or
3 months of isoniazid and rifampicin
Laryngeal tuberculosis
usually a late complication of pulmonary tuberculosis that has not been treated for many weeks. It is usually preceded by several weeks of cough, malaise, and weight loss. The diagnosis can be made by direct laryngoscopy. Sputum smears are likely to be heavily positive (so a diagnosis of tuberculosis can be made from sputum smear examination). The patient may also report pain on swallowing due to tuberculous pharyngitis.Primary tuberculosis
Rarely in primary tuberculosis the mediastinal glands can enlarge so much that the left recurrent laryngeal nerve is compromised, resulting in hoarseness: but this is unlikely. The chest x ray will usually show left hilar gland enlargement and laryngoscopy will detect a paralysed left vocal chord.The sputum is likely to be negative for acid fast bacilli. Occasionally the gland expands in a posterior direction rather than laterally and will be detected only on a lateral chest x ray.
Figure 3. Sputum smeared for acid fast bacilli.
Figure 4. M tuberculosis being cultured on a Lowenstein-Jensen slope.
Primary tuberculosis is likely to be subclinical with no symptoms even in the presence of greatly enlarged lymph nodes. In children aged 5 to 11 years tuberculosis can be a seemingly innocuous illness with only mild symptoms.Gastric washings are the best way of obtaining specimens for microbiology in small children. Even bronchoscopy does not improve the yield of culture confirmed disease. From notification data in the UK, only 22% of children notified as having tuberculosis have disease that is confirmed on culture.
• There are no absolute rules about the contents of the cerebrospinal fluid in tuberculous meningitis, but typically there is low glucose and raised protein. White cells may be few or absent. If they are present then lymphocytes usually predominate.
• Acid fast bacilli are seen only on smear in patients with advanced tuberculous meningitis.
• Even culture may be negative in some patients (in such patients specific treatment seems to provide an empirical diagnosis). The place of polymerase chain reaction in diagnosis is not yet clear.
If treatment is started before progression to stage 2 or 3 the outlook is usually good. However, a small percentage of patients, even those in stage 1, may have a severe debilitating stroke or may die months into treatment.
Stage 1 tuberculous meningitis is characterised by the typical symptoms of meningitis; headache, neck stiffness, and photophobia
Stage 2 is defined by an alteration of consciousness or the presence of one or more cranial nerve lesions
Stage 3 is characterised by coma
The prognosis is strongly related to the stage at which treatment is started.
Tuberculous meningitis
Treatment of tuberculous meningitis is the same as for pulmonary tuberculosis
The treatment of tuberculous meningitis involves giving four drugs for two months or until sensitivities are obtained, followed by 10 months of isoniazid and rifampicin. The use of steroids from the start of treatment is also indicated, especially if the patient presents with stage 3 disease.
Surgical intervention for possible tuberculous lymphadenitis often results in a chronically discharging sinus, which can take months to heal and which leaves an unsightly scar. It is best avoided except when an environmental mycobacterium has been isolated (in this circumstance complete excision of the gland should be carried out).
A fine needle aspiration from the wall of the abscess offers the best hope of a positive culture in the presence of sterile pus. A specimen sent for testing with the polymerase chain reaction is unlikely to help because this test is less sensitive than culture.
According to randomised controlled trials treatment for six months is sufficient for tuberculosis at any site except the central nervous system.
You should consider an HIV test
Current guidelines recommend that all patients with tuberculosis should be offered an HIV test. An extrapulmonary site is particularly common in patients with HIV infection.
You should take blood for liver function tests before starting treatment and you should warn patients to stop treatment and seek medical advice if they have nausea or jaundice. Once treatment is started, and provided pretreatment liver function is normal, biochemical monitoring is not required. Patients invariably show some rise in liver enzyme levels on treatment, but an acceptable upper level has not been agreed. It is safest to tell patients to stop treatment and to return to the clinic if nausea or jaundice occurs.
Conversion of sputum from smear and culture positive to negative is the only reliable way of determining the effectiveness of treatment. Weight gain can be a good clinical indication of successful treatment. But symptomatic improvement may be masked by side effects of treatment such as nausea. The chest x ray may improve with treatment but it is a poor indicator because permanent fibrosis and scarring may have occurred before treatment has started.
Nausea and flushing are common side effects of pyrazinamide and probably occur in at least one in five patients. Side effects are more common in elderly people.
If the patient reports nausea you should check liver function to ensure that drug related hepatitis is not occurring. Nausea can often be controlled with antiemetics.
Learning bite
Pyrazinamide can cause hyperuricaemia and attacks of gout.Although rare, optic neuritis is a serious side effect of ethambutol. At doses of 15 mg/kg it is likely to occur only in the elderly. When the drug used to be used at doses of 25 mg/kg the side effect occurred more frequently.
Tb effusion,The best way to confirm the diagnosis is to send a pleural biopsy for histology and culture. Pleural fluid is unlikely to reveal mycobacteria even in culture and pleural biopsy for histology alone is often negative. A combination of pleural biopsy for histology and culture will provide the diagnosis in 80-90% of patients.
HIV reduces the CD4 lymphocyte count and impairs
cell mediated immunity; this means there is no type IV hypersensitivity reaction to tuberculosis infection, which causes the positive tuberculin skin test and lung cavitation.Large numbers of bacteria accumulate in lung cavities with access to the open air via the bronchial tree rendering the patient's sputum smear positive, sometimes heavily so. In contrast in HIV seropositive patients cavitation may not be present, bacteria being retained within body tissues and therefore not expectorated.
The chest x ray in HIV patients may have virtually any appearance. HIV infection may therefore render the patient's tuberculin skin test and sputum smear negative even though the disease may be rampant.
An HIV test with appropriate counselling is now recommended for all patients with tuberculosis.
Although the gamma interferon blood test (particularly the ELISPOT T-Spot.TB test) is more likely than the skin test to be positive in the presence of HIV and tuberculosis infection, it is diagnostic only for infection and not necessarily for active disease.
Rifampicin, the most important antituberculosis agent, reduces serum levels of many antiretrovirals. Latest data suggest that concurrent therapy of HIV and TB may have lower mortality than sequential treatment. Often treatment for tuberculosis alone will raise the CD4 lymphocyte count. Treating tuberculosis and HIV infection together is complex and should be undertaken only by expert multidisciplinary teams.
Tuberculosis can pursue a chronic form with decreased appetite leading to weight loss and an inability to regain weight. You should always exclude tuberculosis in patients with suspected anorexia nervosa.
The new guidelines are clear: any person younger than 16 years with a positive tuberculin skin test but normal chest x ray should be given preventive therapy with three months of isoniazid and rifampicin or six months of isoniazid.
Environmental mycobacteria such as M kansasii or M avium are acid fast and infection with them can mimic tuberculosis (but is not tuberculosis)
Gamma interferon blood tests are likely to replace the skin test eventually, but they indicate M tuberculosis infection and not necessarily active disease
HIV infection is by far the strongest risk factor for tuberculosis: it increases risk by about 100-fold.
The next highest risk is jejunal bypass surgery, which increases risk by about 20-fold for reasons we don't understand.
Diabetes and smoking both increase risk by between two- and fivefold (by depressing host immunity).
Being tall and thin increases risk by about 1.3- to 1.5-fold
Children with tuberculosis are often asymptomatic.
Laryngeal tuberculosis arises by direct spread from pulmonary disease; the bacteria are coughed over the larynx and vocal cords. It is secondary to open tuberculosis and therefore likely to be highly infectious. It suggests that the patient has been infectious for some time, perhaps up to several months.
Cervical lymph node tuberculosis usually presents as the only site of disease. It probably results from bacteria tracking in the lymphatic system from the lungs or tonsils from subclinical infection at those sites. The chest x ray is usually normal.
It is dangerous to attribute certain patterns seen on a chest x ray to tuberculosis only. There is a wide differential diagnosis including infection from other causes, bronchogenic carcinoma, and sarcoidosis.
The BCG vaccination usually renders the tuberculin skin test weakly positive: a grade 1 or 2 Heaf test or up to 14 mm on Mantoux testing. But this is by no means the rule; some skin tests may be negative and some strongly positive. The absence of a positive skin test does not mean that the BCG vaccination has not "taken.
The new gamma interferon blood tests will help to distinguish between a skin test rendered positive by BCG vaccination alone and one rendered positive by genuine infection with M tuberculosis because the blood tests use antigens specific to the tuberculosis bacteria and not to the BCG vaccine
The diagnosis of tuberculous meningitis is often difficult. If in doubt you should start treatment because a delay can be catastrophic.
Although evidence is sketchy some studies have shown that steroids reduce complications and deaths, especially if given to patients with stage 3 disease (those in a coma).
At least two months of isoniazid, rifampicin, pyrazinamide, and ethambutol should be followed by 10 months of isoniazid and rifampicin.
There is usually no sure way of knowing when infection with tuberculosis has started but the epidemiology of presentation suggests a time interval of six to 18 months in patients where the time of initial infection can be accurately pinpointed. HIV infection considerably accelerates this process.
The tuberculin skin test is often negative because of reduced type IV hypersensitivity.
Sputum is NOT more likely to be smear positive than in patients without HIV infection. Because HIV reduces CD4 lymphocyte counts, the type IV hypersensitivity (which results in tissue destruction with lung cavitation) is reduced. Therefore, the possibility of large collections of bacteria in cavities to be coughed up is reduced.Because rifampicin reduces the serum levels of most antiretrovirals, treatment of HIV infection is best left until after tuberculosis therapy is complete if possible. Often treatment for tuberculosis alone will raise the CD4 lymphocyte count.
Cure rates of tuberculosis are similar in HIV positive and negative patients, although deaths in the former group may be higher because of opportunist infection with other organisms. Latest data suggest that concurrent therapy of HIV and TB may have lower mortality than sequential treatment.
The characteristic shadowing of post primary tuberculosis can make the diagnosis of tuberculosis appear easy. The shadowing is soft, fluffy, predominantly in the upper lobes, and often with cavitation.
But pulmonary tuberculosis can present with virtually any radiographic pattern (especially in the presence of HIV infection). So a chest x ray cannot definitively confirm the diagnosis of tuberculosis.
A sputum smear test
In about 50% of patients with pulmonary tuberculosis the sputum smear test will be negative. This is because over 10 000 bacteria per ml of sputum are needed to give a positive smear. Increasingly in the white population of the UK a positive smear results from an environmental mycobacterium such as M kansasii or M avium, not M tuberculosis. So a sputum smear test cannot definitively confirm the diagnosis of tuberculosis.Culture of a specimen growing M tuberculosis complex
Only a positive culture definitely confirms tuberculosis. The use of liquid media has sped up this process from many weeks to two to three weeks. Enhanced surveillance has shown that as many as 30% of patients treated for pulmonary tuberculosis are culture negative.A positive tuberculin skin test confirmed by a positive gamma interferon blood test
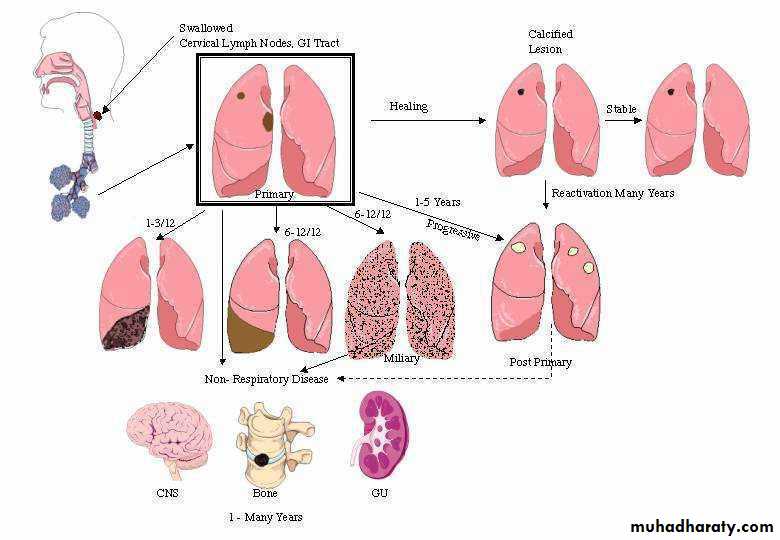
Guidelines from the National Institute for Health and Clinical Excellence (NICE) advise that a positive tuberculin skin test should be followed by a positive gamma interferon blood test (if available) to confirm the presence of tuberculosis infection. But these tests demonstrate only the presence of infection with M tuberculosis, not necessarily active disease.Figure 5. A diagram of the pathophysiology of tuberculosis. Infection usually enters the lungs where a primary complex is formed (square box). Subsequently, healing usually occurs leaving a fleck of calcification (top line). Primary disease may proceed directly to lobar collapse (left of middle line), pleural effusion (left centre), and miliary disease (right centre) or may progress directly to post primary disease with cavitation (right of middle line). Alternatively, healed disease may reactivate to post primary disease (top to middle line). Sometimes disease may spread to extrapulmonary sites such as brain, bone, or the genitourinary system (bottom line). Approximate times from primary infection to presentation are shown with each diagram. Timing will be dramatically shortened by HIV coinfection.
Figure 5. A diagram of the pathophysiology of tuberculosis. Infection usually enters the lungs where a primary complex is formed (square box). Subsequently, healing usually occurs leaving a fleck of calcification (top line). Primary disease may proceed directly to lobar collapse (left of middle line), pleural effusion (left centre), and miliary disease (right centre) or may progress directly to post primary disease with cavitation (right of middle line). Alternatively, healed disease may reactivate to post primary disease (top to middle line). Sometimes disease may spread to extrapulmonary sites such as brain, bone, or the genitourinary system (bottom line). Approximate times from primary infection to presentation are shown with each diagram. Timing will be dramatically shortened by HIV coinfection.