د. حسين محمد جمعه
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
Management of asymptomaticWolff–Parkinson–White syndrome
Heart 2009Wolff–Parkinson–White syndrome (WPW) is a
frequently encountered electrocardiographicabnormality and an important diagnostic and
therapeutic issue for cardiac specialists. Estimates
of WPW prevalence in the general population are
contingent on the likelihood of asymptomatic
patients having an electrocardiogram (ECG) performed,and range from 0.1–0.2%.
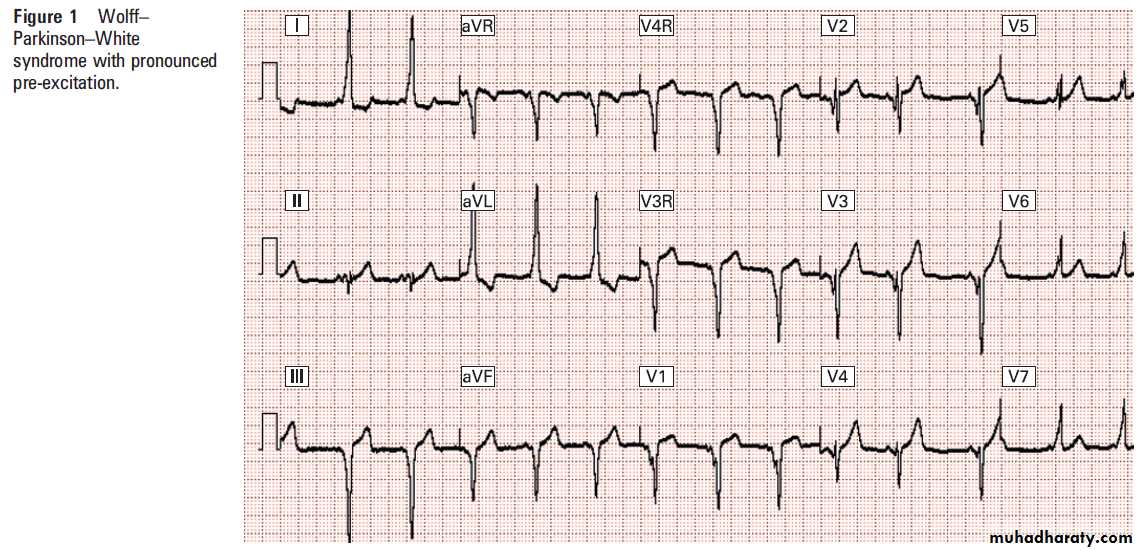
WPW consists of pre-excitation of the QRS (the delta wave) caused by eccentric activation of the ventricular myocardium via an accessory atrioventricular (AV) connection (accessory pathway, historically called the
bundle of Kent) (fig 1). In addition to ventricular
pre-excitation observed in sinus rhythm, the
electrophysiological consequences of this connection
include the paroxysmal occurrence of atrioventricular
reciprocating tachycardia (SVT) and, at considerably lower frequency, the occurrence of rapidly conducted atrial fibrillation, which may result in ventricular fibrillation and death.
AETIOLOGY AND PATHOPHYSIOLOGY
Accessory pathways (APs) by definition traversethe AV groove, and are identified in all anatomical
quadrants of the tricuspid and mitral annuli.
Although WPW is prevalent, pathological demonstration is rare as this myocardial feature is
microscopic and rarely systematically sought in
postmortem study.
Although APs are typically congenital, many well substantiated reports indicate that the clinical aspects of WPW may sometimes
be acquired de novo, typically in patients
who have undergone cardiac surgical procedures.
An increased prevalence of WPW is noted among
patients with Ebstein’s anomaly, in whom APs are
typically anatomically associated with the abnormal tricuspid valve, and often multiple.
Among symptomatic patients, clinical presentation
is typically with palpitations or a sustained
episode of SVT. A bimodal age distribution is
observed: a substantial number of patients present
in the first month of life (in some cases, prenatally),
and a secondary, more diffuse peak through
the school age years.
Prenatal and infantile
presentation of SVT is often associated with signsof congestive heart failure, perhaps due in part to
the relatively prolonged interval between onset and
diagnosis. Although pre-excitation is typically a
persistent phenomenon, it may in some cases be
variably present, even after electrocardiographic
diagnosis of WPW.
Infants with SVT may demonstrate pre-excitation that emerges months or even years after their initial diagnosis of SVT. The
reasons for this variability are poorly understood.
The conduction velocity of the AV node as well as
the refractory period of the APs change with
developmental stage in childhood, factors that
may be expected to affect the degree of preexcitation. (a balance between the speed of AV
conduction and the percentage of the ventricular
myocardium depolarised in advance of the normal
activation sequence).
However, they do not fully explain observations of ‘‘occult pre-excitation’’ or some certain aspects of AP behaviour during AF, and other mechanisms such as concealed retrograde conduction may need to be inferred to explain this phenomenon.
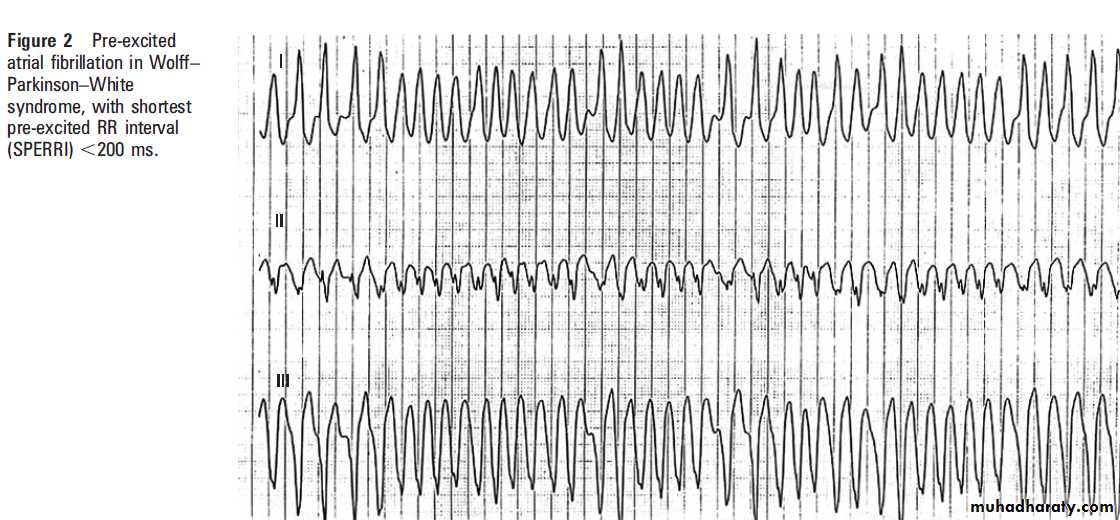
SUDDEN DEATH ASSOCIATED WITH WPW
Although the relationships of the bundle of Kent toboth pre-excitation and reciprocating tachycardia
were proposed soon after WPW was described in
the 1930s, the rapid conduction of atrial fibrillation
via the AP as a mechanism of sudden death in
WPW was not identified until 1971 by Dreifus
(fig 2). A North American population study
suggested that the risk of this severe complication
of WPW is about 3–4% over several decades, and
this is conventionally quoted as an annual risk rate
of ,0.1%/year.
These data were generated in an era which antedated both the widespread use of the ECG for screening of non-specific symptoms
(fewer asymptomatic patients identified) and the
modification of the population by ablation (longer
periods to observe natural history). More recently,
a long term follow-up of military personnel with
WPW reported a mortality rate of 0.02%/year.
Two additional studies comprising more than 4000
additional years of patient follow-up present
estimated mortality rates between these two.
In the aggregate, these studies suggest a consensus
estimate of 0.05%/year. However, a widely noted
report from Italy has also presented a WPW patient
group that was prospectively followed for 3 years,
and which recorded a severe event rate (defined as
death or potentially lethal arrhythmia recorded on
monitoring) that was 10 times higher—,0.5%/year.
This important, disparate finding requires further exploration and confirmation, as it notably alters the outcome of risk-to-benefit calculations which guide therapy decisions discussed below.Because it is difficult to resolve these numbers, it is also useful to check them against estimates of global sudden death rates in the ‘‘healthy’’ population (0.0013%/year), the fraction of such deaths attributable to WPW in pathological and
clinical studies (2–4%), and an estimated prevalence of the disease in the general population of
1/1000. Utilisation of these statistics yield a
projected mortality rate of 0.03–0.05%/year among
WPW patients, tending to support the lower range
of estimates for mortality presented above.
ASYMPTOMATIC WPW
Symptoms associated with WPW are almost solelydue to the occurrence of transient or sustained
SVT. Frequent and/or severe SVT related symptoms
may themselves prompt many patients to
seek catheter ablation, especially if attempts to
prevent episodes using drugs such as b-blockers
prove unsuccessful.
However, many patients with WPW are completely asymptomatic, and are diagnosed serendipitously at the time of cardiac evaluation proposed for an unrelated indication (for example, evaluation of murmur, chest pain, dizziness, screening for sports participation or before drug prescription).
The proportion of patients with WPW who are truly asymptomatic is unknown, and its estimate is made difficult because of the increasing use of the ECG in general, and particularly for screening young populations (athletes, those receiving certain classes of prescription drugs). Counterbalancing this, there may
often also be a desire of clinicians and patients to
attribute retrospectively remembered episodes of
transient palpitation to WPW after the disease has
been serendipitously diagnosed.
Nonetheless, there seems to be agreement within the literature that
50% or more of patients with WPW are asymptomatic.This also extends to the much smaller number of WPW patients who present with cardiac arrest, 40–50% of whom may have had no symptoms or knowledge of their diagnosis before the event.
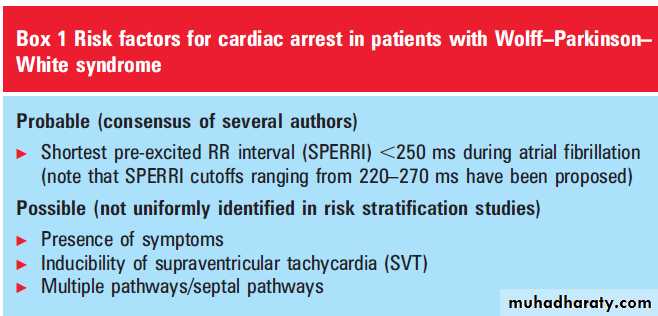
RISK STRATIFICATION IN WPW
Many investigators have sought to identify riskfactors for cardiac arrest in WPW, studying both
clinical and electrophysiological markers (box 1).
Absence of symptoms in WPW patients is not in
itself a marker of low risk for arrest, as the
occurrence of sudden death in these patients is well
documented.
The affirmative (and more difficult to prove) converse of this statement—that symptomatic
and asymptomatic WPW patients have an
equivalent risk of cardiac arrest—has not been
demonstrated. However, several studies reviewed
below suggest that electrophysiological properties of
the two groups may, in some ways, suggest that the
asymptomatic WPW patient may in fact be at
somewhat lower risk for cardiac arrest.
It was demonstrated in early clinical studies that
patients who had suffered the most severe symptomsof tachycardia, particularly cardiac arrest,
have shorter pre-excited RR intervals (SPERRI)
during episodes of atrial fibrillation than those
with more mild symptoms. Those with SPERRI
(220 ms (250 ms in some studies), and/or with
other measurable properties of the AP such as its
effective refractory period and rapid 1:1 conduction
of atrial pacing are thus considered to be ‘‘high
risk’’ for a life threatening event, relative to the
general population with WPW.
Conversely, longer SPERRI and/or longer AP refractory periods identify a lower risk patient subgroup.
This association has been investigated by many
independent observers. Milstein et al compared the
electrophysiological properties of asymptomatic
WPW patients to matched symptomatic controls
and found that asymptomatic patients were at
somewhat decreased risk for short SPERRI.
Bromberg et al performed electrophysiological
evaluation of 60 variably symptomatic childrenwith WPW and showed that short pre-excited RR
intervals were found in 35% of patients with SVT
as their symptom, in 74% presenting with syncope,
and in 100% of those who had a cardiac arrest; the
overall incidence of low SPERRI was 53%.
The severity of presentation was not associated with other clinical features of disease that might be used to predict risk.
They concluded that presence of aSPERRI determined to be ,220 ms was associated with an approximately threefold increase in risk of cardiac arrest, compared to the general WPW
population. Dubin et al studied 119 children with
WPW, divided into asymptomatic patients, those
with SVT, and those with syncope.
They found no difference between these groups with respect to SPERRI ,270 ms, inducibility of SVT, the presence of multiple pathways and pathway location.
Thus, the absence of symptoms did not predict
the findings of intracardiac risk stratification, and
therefore does not obviate need for testing. This
finding intuitively corresponds to the observation
made above that a significant fraction of patients
experiencing cardiac arrest are asymptomatic
before the event.
Less invasive risk stratification techniques have
been proposed and studied in varying degrees asproxy measures which can be used to obviate the
need for intracardiac electrophysiology study
(EPS).
These include the use of Holter monitoring
and exercise testing, to determine whether preexcitation disappears at high physiological heart rates.
Loss of pre-excitation on graded exercise testing generally predicts longer AP effective refractory periods, and this is also assumed to be true for physiological sinus tachycardias recorded
on ambulatory ECG monitoring. Thus, these tests
are sensitive to those at risk, but relatively nonspecific and of low positive predictive value.
Although a formal SPERRI or pathway refractory
period is not determined, the patient is considered
‘‘safe’’ in these cases, and more invasive study deferred.
Bershader et al reviewed 88 patients who underwent exercise testing and subsequent intracardiac EPS and found that, although loss of preexcitation on exercise was associated with longer average AP refractoriness, only 15% of patients had that finding, and among them many had pathways that were ultimately considered to be of ‘‘intermediate’’ risk.
Oesophageal pacing has also been used to probe
pathway behaviour. It is often possible to induceatrial fibrillation for formal assessment of SPERRI
using this technique, and it has been shown that
intracardiac and transoesophageal assessment of
AP refractory period is well correlated. It must be
born in mind, however, that induction of arrhythmia
by this technique also carries the same
intrinsic risks as those induced in intracardiac
EPS, and ventricular fibrillation during oesophageal
study has been reported.
It has also been suggested with less unanimity
that other clinical associations may be importantand useful markers: the nature and severity of
clinical presentation, the presence of multiple pathways and an anatomical location of the AP in the right anteroseptal AV groove, and the
inducibility of any SVT (including both AV
reciprocating tachycardia and atrial fibrillation)
on electrophysiological study.
Identifying areduced and reliable set of risk factors from these different studies is complicated by the fact that some are likely to be electrophysiologically associated.
TREATMENT FOR WPW
In the past two decades, the technique of catheterablation (predominantly using radiofrequency
energy) has been widely and successfully applied
to the treatment of WPW.
During the early development of this curative technique, patients most severely affected by symptoms of WPW—those who had experienced an aborted. cardiac arrest, or who had frequent, disabling and/or drug refractory episodes of SVT—were selected for
ablation.
However, as the technique has matured and become more widely available, it has been
increasingly applied to patients who are minimallysymptomatic or asymptomatic.
It is established that effective catheter ablation
of the AP in WPW eliminates pre-excitation of the
ECG as well as the occurrence of AV reciprocating
tachycardia. Although more difficult to prove in
clinical study (due to the low frequency of the
observed event), effective ablation also appears to
eliminate the excess risk of cardiac arrest attributed to the disease.
This finding is of particular importance, because sudden cardiac arrest (SCA) risk is the only indication for therapy in asymptomatic patients, and there is no indication that it can be reduced by antiarrhythmic drug treatment,which may be useful for some patients with
symptomatic SVT.
Interestingly, ablation also appears to reduce the elevated propensity of many WPW patients to the occurrence of atrial fibrillation.
Unfortunately, catheter ablation also carries
with it a low but finite risk of death or majoradverse event. Registry and prospective studies in
children and adults have been published over the
last 15 years that allow very specific estimates of
acute and chronic efficacy of ablation for AP
mediated tachycardias, and the risk of procedural
death, major and minor adverse complications.
The Pediatric RF Registry provided acute outcome data on a multicentre series of 5383 AP ablations
performed in the 1990s. The acute success rate
for radiofrequency (RF) ablation in the ‘‘late era’’
(that is, post-learning curve) experience was 95.2%,
with variation based on AP location. In this broad
experience, one death occurred in 3187 ‘‘late era’’
ablations, and incidence of major acute complications
of higher grade AV block, perforation and
thrombus/thromboembolic event in this group
were 0.6%, 0.5%, and 0.2%, respectively.
Risk factors for adverse events in the RF Registry
included small patient size, pathway location and
presence of concomitant heart disease. The subsequent Prospective Assessment of PediatricCardiac Ablation (PAPCA) study looked closely at ablation outcomes in 481 patients with AP mediated SVTs. Acute success rate for ablations was 96%. Follow-up was exceptionally good over 12 months, and showed that recurrence rates averaged 10.7%, higher than had been suspected based on registry data.
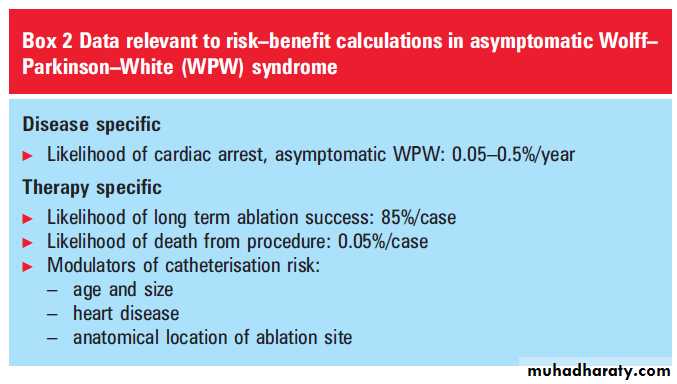
Estimates of annual risk of SCA in WPW vary roughly by a factor of 10, between 0.05–0.5%. If one considers 20 years as a‘‘risk reduction window’’ in the calculation of the value of prophylactic ablation, an assumption of 0.05% annual risk implies that˜111 patients would need to undergo ablation to prevent one SCA, while an assumption of 0.5% annual risk implies that the same effect could be achieved with ˜11 ablations.
Each of these ablated patients would incur the cost of the procedure in terms of health care expense and risk of sublethal adverse event, which can be used to perform other types of risk–benefit analyses. The pronounced difference between these two assumptions is mitigated somewhat by the fact that a proportion of asymptomatic patients over time develop symptoms and would then likely realise other treatment benefits.
Conversely, although the benefits of successful ablation are life long, it is unlikely that
healthy, asymptomatic patients, their families and
physicians routinely discount their cardiac risks
over several decades in deciding whether or not to
assume smaller but more immediate risks and
discomforts of an ablation procedure.
At present, asymptomatic WPW is considered to
be a class 2b indication for catheter ablation inpatients 5 years and older, and a class 3 indication
for patients younger than 5 years. This is a strong
indicator that, despite ongoing advances in ablation
technique and clinical research in WPW,
ablation in asymptomatic patients must be recommended only after careful consideration.
Clinical equipoise still exists on this question, with valid expert opinion expressed on both sides of the
question of indication for ablation. The divergence
of academic opinion and acceptable clinical practice in this condition highlights the difficulties in
quantifying the frequency of low frequency events
in patient populations, the importance of tracking
the evolution of procedural efficacy and adverse
event rates, and the variability of risk interpretation
among patients and physicians.
ACTIVITY RESTRICTION AND PRESCRIPTION DRUG
USE IN ASYMPTOMATIC WPWIn patients with WPW, no evidence based data
have been published indicating a clear association
between either activities (sports participation) or
prescription drug use, including stimulants and
psychoactive drugs. However, the increased risk of
sudden death associated with WPW in combination
with anecdotal, highly publicised events of
cardiac arrest in apparently healthy young people
have driven policy regarding sports participation
which is based on expert consensus.
Recent recommendations are that all patients with
untreated WPW undergo exercise test, echocardiogram (to exclude associated cardiovascular
abnormalities) and, perhaps, ambulatory ECG
recording during athletic activity.
Asymptomatic patients may be allowed to participate if these are reassuring, but EPS may be recommended before allowing participation in ‘‘moderate to high intensity competitive sports’’.
Athletes with high risk pathways are prohibited from sports participation, until they have been successfully ablated.
With respect to prescription drugs, it is known
that some commonly used agents, such as stimulants,
cause modest increases in heart rate and
adrenergic tone, and others, particularly psychotropic
agents, may for unclear reasons be associated
with an increased risk of sudden death.
To date, no expert guidance has been provided for the
use of prescription drugs in patients with WPW.It is useful to note that, in contrast to long QT
syndrome, proscriptions against intense physical
exertion and use of certain drugs are grounded in
well researched understanding of specific mechanisms
by which these activities or agents act to
increase the risk of lethal arrhythmia.
In contrast, the general risk associated with WPW has typically been conflated with the non-specific risks of these activities or agents, without proposal of any mechanistic hypotheses as to why they might be
synergistic.
RECOMMENDATIONS
What, then, is the proper management of asymptomaticWPW? Our understanding of the intrinsic
risk of this syndrome when left untreated is key to
answering this question, and the answer involves
balancing the small risk of an iatrogenic event at
the time of treatment against the low and difficult
to measure cumulative risk of the arrhythmia
untreated over decades.
Although the evidence for its efficacy is lacking, it is generally accepted that,
unless clearly shown to be ‘‘low risk’’, thesepatients should be restricted from varsity athletics
and higher level competition, and stimulant
medicines may only be used with heightened
medical supervision and intermittent monitoring
for arrhythmogenesis.
There is no evidence that administration of antiarrhythmic medications of any form reduce the risk of sudden death over time.
Thus the questions to be answered are: is
ablation indicated for all, some, or none of these patients?
The brief analysis above has shown that the
risk–benefit ratio for catheter ablation therapy ofasymptomatic WPW is strongly dependent on
one’s assumptions regarding perceived risk, and
the extent to which the physician and patient are
looking into the future when deciding on ablation.
Although that leaves considerable latitude for
individual decision making, it seems clear thatpatients in whom pre-excitation disappears at
physiological heart rates tend to have pathway
properties which do not place them in the higher
risk group, and they can be followed and allowed
to pursue normal lifestyle and activities with
reasonable safety.
Thus, an exercise stress test and ambulatory ECG should be a routine part of evaluation of patients determined to be asymptomatic WPW patients. It is our general practice that patients who do not have a reassuring pattern of clear loss of pre-excitation during one of these studies undergo risk stratification by intracardiac EPS.
This is often combined with catheter ablation
if it is deemed safe and necessary, based on patient
size (preferably >20–25 kg, in our institution),
pathway location (deferring ablation midseptal
and para-Hissian pathways when possible), and
any complicating medical or social issues (for
example, desire to participate in varsity or elite
athletic competition, need to treat with stimulant
or other proarrhythmic medications).