د. حسين محمد جمعه
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2012
ModulesCVS
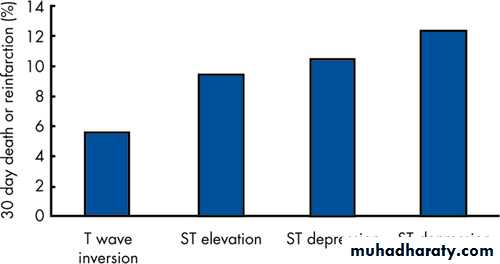
In the TIMI IIIb study the use of recombinant tissue plasminogen activator (r-tPA) in patients with non-Q wave myocardial infarction or unstable angina was associated with increased death or later myocardial infarction and with a nearly statistically significant increase in intracranial haemorrhage.T wave inversion in the context of an acute coronary syndrome is associated with a less adverse outcome than ST segment depression.
Troponin I values peak eight to 12 hours after the onset of chest pain and therefore early sample may represent a false negative.
Risk stratification
Scoring systems for the prediction of risk in patients with suspected acute coronary syndrome have been developed from the ESSENCE, TIMI IIB, and PURSUIT trials. For example, the TIMI risk score is based on seven risk factors identified through multivariate analysis and predicts the incidence of the composite end point of death/myocardial infarction or severe recurrent ischaemia requiring urgent revascularisation at 14 days.The factors include:
• Age ≥65 years
• At least three risk factors for coronary artery disease (including family history, hypertension, hypercholesterolaemia, diabetes, and current smoking)
• Prior coronary stenosis of 50% or greater
• ST segment deviation
• Two or more anginal symptoms within 24 hours
• Aspirin use within seven days and
• Elevated concentrations of the MB isoenzyme of creatine kinase (CK-MB) or troponin.
The rate of the composite end point was:
4.7% with zero to one risk factor8.3% with two risk factors
13.2% with three risk factors
19.9% with four risk factors
26.2% with five risk factors and
40.9% with six to seven risk factors.
Although many factors have an influence on prognosis of the patient with an acute coronary syndrome perhaps the most important are:
Age >65 years
Previous myocardial infarction
Diabetes mellitus
Failure to settle clinically
Evidence of myocardial damage (for example troponin rise) and non-ST elevated myocardial infarction
ECG changes particularly when there is ST shift.
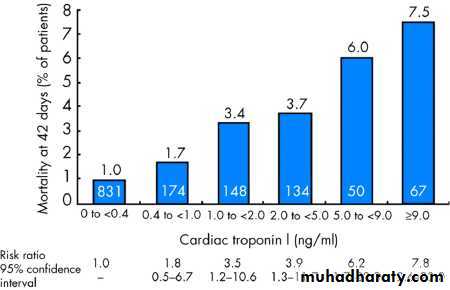
A raised troponin value is a powerful independent marker of adverse outcome in patients with unstable coronary syndromes. In the TIMI IIIB study the 42 day mortality rate was significantly higher in patients with troponin I concentrations of ≥0.4 ng/ml (3.7%) than in patients with troponin I concentrations <0.4 ng/ml (1.0%)
Furthermore, the value of troponins is not limited to whether they are merely "positive" or "negative"; there is also an excellent correlation between troponin values and worsening outcome.
Although there are some differences in the time course of the rise and fall of troponin I and T, with the troponin T rise occurring somewhat earlier, in real life they are probably equally useful in detecting myocardial damage in the context of an acute coronary syndrome.
Mortality rates at 42 days according to the concentration of cardiac troponin I measured at enrolment.
The 12 lead ECG in stratifying risk
The ECG remains a simple and helpful test for risk stratification. A normal ECG without ST shift or T wave changes usually denotes good prognosis, while at the other end of the spectrum a high level of risk is suggested by dynamic ST segment changes. T wave changes carry intermediate significanceThe value of the 12 lead ECG in risk stratification: death or reinfarction rates in patients presenting with symptoms of cardiac ischaemia at rest and signs of myocardial ischaemia confirmed by ECG.
Although metformin has been reported to cause a lactic acidosis following radiocontrast exposure, this tends to occur only if the drug is continued in the face of radiocontrast nephropathy. Metformin toxicity occurs since metformin is 90% renally excreted. For routine angiography current recommendations state that metformin should be stopped immediately before radiocontrast exposure, withheld for 48 hours, and only restarted when the renal function has been demonstrated to be normal.
Approximately 10% of medically treated patients presenting with unstable angina will suffer either myocardial infarction or death within 4-6 weeks of admission
Role of antiplatelet agents in acute coronary syndrome
Aspirin has long been established as an effective treatment in patients with acute coronary syndrome. More recently other antiplatelet agents such as the glycoprotein IIb/IIIa receptor blockers (abciximab, tirofiban, and eptifibatide) and the thienopyridines (clopidogrel, which inhibits ADP mediated platelet aggregation) have been tested in this context.Glycoprotein IIb/IIIa receptor blocking agents
The role of glycoprotein IIb/IIIa inhibitors in unstable angina has recently been reviewed16 and revised (September 2002) recommendations from the UK's National Institute for Health and Clinical Excellence (NICE).
In summary, NICE has recommended the use of "small molecule GP IIb/IIIa inhibitors as part of the initial medical management of patients with unstable angina or non-ST elevation myocardial infarction who are at high risk of myocardial infarction or death."
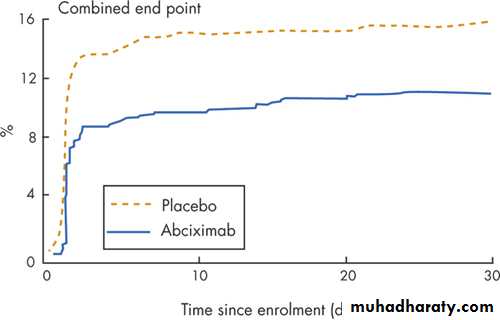
The evidence from which this conclusion was derived comes from a variety of studies; however, it is clear from these studies that benefit is, in general, confined to patients also undergoing percutaneous coronary intervention.9 17 Thus, if these agents are to be used it should be with the intention of undertaking angiography and revascularisation where possible. Abciximab (a monoclonal antibody fragment against the IIb/IIIa receptor) is not recommended by NICE in the medical treatment of acute coronary syndrome since the GUSTO-IV acute coronary syndrome trial18 showed no benefit from abciximab in this context.
NICE also recommend the use of glycoprotein IIb/IIIa inhibitors if percutaneous intervention is undertaken in patients with unstable angina or non-ST elevation myocardial infarction. The use of abciximab, as in the current case, is supported by data from the CAPTURE study19 which reported a significant reduction in the combined end point of death, myocardial infarction, or urgent reintervention at 30 days in patients undergoing percutaneous intervention for unstable angina or non-ST elevation myocardial infarction, though at the expense of an increase in major bleeding .It should be noted that the evidence for low molecular weight agents as an adjunct to percutaneous intervention is less robust20 21 and in a direct comparison in elective percutaneous intervention tirofiban has proved less effective than abciximab.22
The CAPTURE study randomised 1265 patients with refractory unstable angina undergoing percutaneous intervention to abciximab or placebo for 18-24 hours before percutaneous intervention, continuing until one hour afterwards. By 30 days, the primary combined end point (death from any cause, myocardial infarction, or urgent intervention for recurrent ischaemia) had occurred in 71 (11.3%) of 630 patients who received abciximab compared with 101 (15.9%) of 635 placebo recipients (p=0.012).
Percutaneous intervention and surgery are both accepted treatments for stenosis of the proximal left anterior descending artery. Although some old data suggest that bypass grafting may be superior to percutaneous intervention in patients with diabetes these data are mainly from the analysis of small subsets of patients with diabetes in larger studies and do not include many patients with acute coronary syndrome. The use of drug eluting stents is likely to further reduce the gap between surgery and percutaneous intervention in the future.
Direct stenting, which is the insertion of a stent into a lesion without predilating the lesion with a balloon, has attraction in this situation. It probably reduces the chance of a dissection being produced and also may reduce the amount of distal embolisation by trapping loose material at the lesion site.
Any percutaneous intervention should be covered by the use of abciximab (evidence from the CAPTURE study would support this).
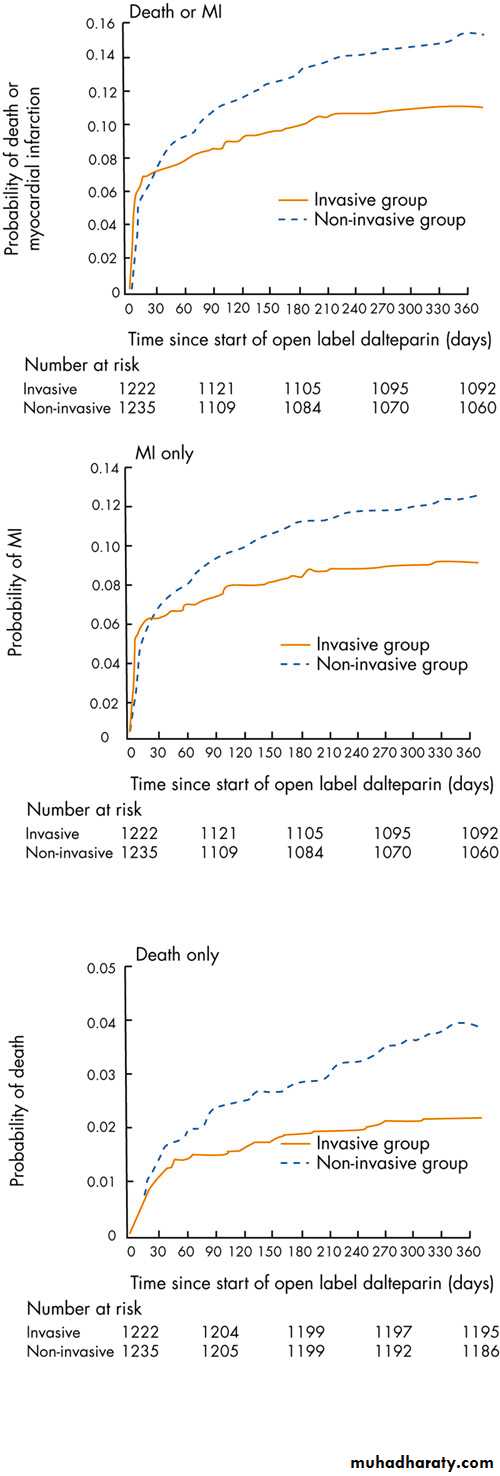
FRISC II
The FRISC II trial, in which an early invasive approach in acute coronary syndrome was compared to a non-invasive one in patients treated with low molecular weight heparin (dalteparin), clearly shows a significantly lower death rate in the group of patients randomised to an invasive approach. Similar reductions were also seen in the incidence of myocardial infarction and in the composite end points of death and myocardial infarction.The results of the FRISC II study showing the differences in death and MI (top), MI (middle), and death (bottom panel) between the groups of patients treated conservatively (dashed line) and invasively (solid line).
Drug eluting (coated) stents
The use of a coating to inhibit smooth muscle proliferation and thus reduce in-stent restenosis is an attractive idea. Anti-proliferative, anti-inflammatory, immunosuppressive, and anti-migratory agents all have potential. Compounds studied with varying degrees of success include rapamycin, tacrolimus, paclitaxol, dexamethasone, mycophenolic acid, and batimastat.Currently stents coated with sirolimus (rapamycin, Cypher, Cordis, Johnson and Johnson) and paclitaxol (Taxus, Boston Scientific) are commercially available; their use is supported by randomised, controlled data from the SIRIUS (rapamycin) and Taxus IV (slow release paclitaxol) trials .
In the SIRIUS trial,25 1101 patients undergoing intervention to lesions between 15-30 mm in length and 2.5-3.5 mm diameter were randomised to either uncoated or sirolimus coated stents; 44% of patients underwent intervention to the left anterior descending artery and >26% had diabetes. The primary end point of target vessel failure was reduced from 21% to 8.6% at nine months (figure 14).
Angiographic in-segment restenosis (including a 5 mm area at each end of the stent) was reduced from 36.2% to 8.9% (75% reduction) and in-stent restenosis reduced from 35.4% to 3.2%. Target lesion revascularisation rates fell from 16.6% to 4.1% (75% reduction).
Similar findings from the TAXUS IV study were presented at the Transcatheter Therapies Meeting in September 2003. This study randomised 1326 patients and demonstrated a reduction in ischaemia driven target vessel revascularisation from 12.0% to 4.7% at nine months. Impressive reductions in target lesion revascularisation were also seen in small vessels and in the >24% of patients with diabetes in the study. Although there was also a reduction in major adverse coronary events at one year in this study, neither coating has yet been shown to reduce mortality. The Reality trial is currently comparing the two stents.
NICE has recently (October 2003) reviewed the role of coated stents and advises their use in vessels <3 mm in diameter or >15 mm in length. Recent myocardial infarction (<24 hours) or the presence of thrombus in the target vessel are listed as contraindications to coated stents:
Since the rate of endothelialisation is probably slower than after insertion of a conventional stent, because the drug inhibits cell division in the endothelium, a longer course of clopidogrel (3-6 months) is advised to prevent stent thrombosis rather than the four weeks used with conventional stents.
Troponins in patients with acute coronary syndrome: comparison of troponin I and T
This is a comparison of the time at which the two isoforms of troponin rise - this shows that troponin T rises somewhat sooner than I and has its greatest sensitivity and specificity at 8-12 hours.Summary
For many years there was doubt about the correct management of patients with acute coronary syndrome.
The evidence now favours the following approach:
Immediate stabilisation with medical treatment including aspirin, clopidogrel (CURE), low molecular weight heparin, (ESSENCE26) and beta blockade. Aspirin is probably the single most important agent (RISC study). The use of small molecule glycoprotein IIb/IIIa inhibitors should be considered .
Conclusions
For many years there was doubt about the correct management of patients with acute coronary syndrome.The evidence now favours the following approach:
Immediate stabilisation with medical treatment including aspirin, clopidogrel (CURE), low molecular weight heparin (ESSENCE26), and beta blockade. Aspirin is probably the single most important agent (RISC study). The use of small molecule glycoprotein IIb/IIIa inhibitors should be considered.
In the presence of dynamic ST segment depression/T wave changes and/or a rise in troponin concentrations, angiography and revascularisation should be undertaken as soon as possible (FRISC II and TIMI 18)
In a stable, low risk patient, with no ischaemic ECG changes or troponin rise, then risk stratification with an exercise test or other non-invasive test of myocardial perfusion is appropriate
If percutaneous intervention is to be undertaken then a glycoprotein IIb/IIIa inhibitor should be given (CAPTURE); the evidence suggests that abciximab is the most effective
If percutaneous intervention is undertaken consideration should be given to the use of either rapamycin or paclitaxol coated stents, especially in small calibre vessels or in long lesions.
Rapamycin and paclitaxol coated stents are proved to reduce target vessel failure compared with bare metal stents but they have not been shown to reduce mortality.
Metformin treatment has been associated with a lactic acidosis following coronary angiography. In elective procedures metformin should be stopped 48 hours before radiocontrast exposure. Metformin should not be restarted for 48 hours after radiocontrast and until the creatinine has been ascertained to be normal.
Abciximab has its greatest benefits as an adjunctive treatment with percutaneous intervention for patients suffering an acute coronary syndrome. Glycoprotein IIb/IIIa inhibitors should be given to selected patients admitted with cardiac type chest pain.