د. حسين محمد جمعة
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
• CVS
• The following are indications for AV replacement in severe Aortic regurgitation• Class II or greater symptoms, and /or
• LV dysfunction (EF < 55%), and/or
• LV dilatation (LVEDV > 55 ml/ square meter BSA or LVESD > 55 mm), even with preserved LV function.
• The grading of AS severity
• (in the presence of a normal LV function) based on Doppler gradients is as follows
• (Severe: gradient > 75 mmHg, moderate:
• 50-75 mmHg, mild: 25-49 mmHg).
• Severe AS in presence of symptoms;
• Severe AS in the absence of symptoms, in the presence of LV dysfunction, or with abnormal response to exercise (e.g., hypotension);• Moderate AS undergoing CABG.
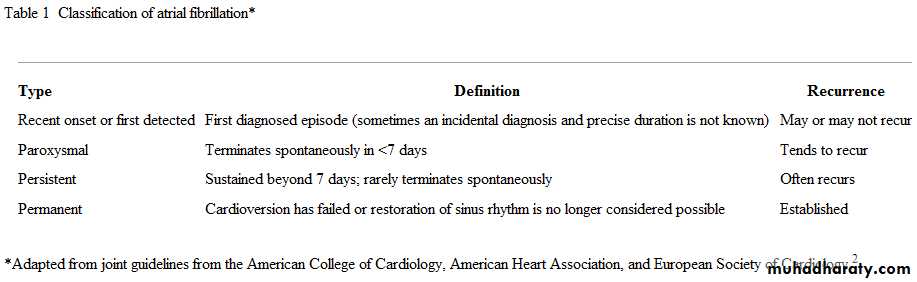
Are there other alternatives for rhythm control?
Patients with infrequent paroxysmal atrial fibrillation may receive no treatment between episodes. If their atrial fibrillation recurs they may have repeated electrical or pharmacological cardioversion, sometimes following a "pill in the pocket" approach (that is, patients who have been given flecainide or propafenone in hospital to reduce paroxysmal atrial fibrillation, and tolerate them well, can be prescribed a single, oral loading dose of flecainide or propafenone for them to take outside hospital if they experience sudden and persistent heart palpitations). A prospective non-controlled trial found that this approach was effective and safe in patients with no underlying heart disease.
Which patients should be referred for rhythm control?
Current guidelines recommend considering rhythm control in patients with(a) lone atrial fibrillation, especially younger patients;
(b) symptomatic atrial fibrillation, such as frequent symptomatic paroxysmal atrial fibrillation or symptoms despite rate control; or
(c) atrial fibrillation secondary to a corrected precipitant.
(d)patients who should but cannot take warfarin might reduce their risk of stroke if sinus rhythm is restored.
Rhythm control has also been recommended for patients with heart failure. However, a recent large randomised trial in patients with systolic heart failure found no difference between rate and rhythm control for any outcome, including worsening heart failure.
• Summary points
• Atrial fibrillation is common and highly variable in its clinical presentation and evolution; it causes substantial morbidity and mortality, including impaired quality of life, heart failure, systemic emboli, and stroke• The first priority is to control heart rate (if tachycardia is present) and provide adequate antithrombotic treatment for preventing complications of embolism
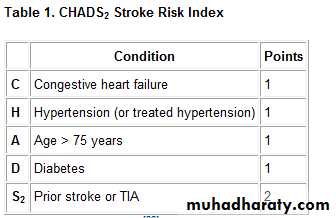
• Patients with moderate to high risk of stroke require warfarin long term for preventing emboli; aspirin is adequate in patients with low risk of stroke.
BMJDecember 2009
When a patient should but cannot take warfarin, aspirin plus clopidogrel can be an intermediate option For long term treatment of atrial fibrillation, rate control matches rhythm control in terms of mortality and major cardiovascular events but has fewer adverse events related to the treatment and fewer hospital admissions
Consider referring for rhythm control younger patients with lone atrial fibrillation, patients with symptomatic atrial fibrillation, and patients with atrial fibrillation secondary to a corrected precipitant
If antiarrhythmic drugs fail to maintain sinus rhythm, percutaneous catheter ablation is an alternative for rhythm control.
Which non-pharmacological treatments can be used for atrial fibrillation?
Atrioventricular nodal catheter ablation with permanent ventricular pacing is used as a palliative approach for controlling ventricular rate in patients with symptomatic atrial fibrillation refractory to medical treatment. A meta-analysis of randomised and non-randomised studies showed that this technique is highly effective and significantly improves quality of life.
The main limitations are a small risk of sudden death during the few months after ablation and lifelong dependency on a pacemaker.
Non-pharmacological interventions aiming to "cure" atrial fibrillation have been tried, initially using open surgery. A more successful approach has been the development of closed chest endocardial ablation, after the discovery that in many patients atrial fibrillation is triggered and/or perpetuated by extrasystoles originating in the pulmonary veins. Briefly, catheters are introduced into the left atrium after a transeptal puncture, and atrial tissue is selectively destroyed (by radiofrequency or cryoenergy) to electrically isolate pulmonary veins. In experienced centres, the success rates are above 70% at one year for paroxysmal atrial fibrillation.
In persistent atrial fibrillation, pulmonary vein isolation alone is not sufficient to achieve acceptable success rates, and atrial substrate modification (discrete ablation and/or linear ablations) is usually necessary. Redoing procedures is required in 9-20% of patients. The rate of related major complications of ablation is below 5% (i.e., pulmonary vein stenosis, stroke, peripheral vascular complications or atrioesophageal fistula) The advances obtained with endocardial catheter ablation have also led to the development of off-pump, epicardial surgical ablation, following the same principles.
Which patients should be referred for catheter ablation?Catheter ablation for patients with atrial fibrillation has become widely used only recently and has not yet been tested in large randomised studies with a mortality end point. However, several well conducted randomised trials and systematic reviews have shown that, in both paroxysmal and persistent atrial fibrillation, catheter ablation is better than antiarrhythmic drugs at preventing recurrences of atrial fibrillation. According to recent guidelines, prevention of recurrence of atrial fibrillation by ablation is justified only when atrial fibrillation is associated with disabling symptoms, and its use depends on the type of atrial fibrillation.2
In patients with paroxysmal symptomatic atrial fibrillation, catheter ablation may be considered after failure of a first line antiarrhythmic drug. Hence, in patients with a structurally normal heart, ablation is an alternative to amiodarone if a class IC antiarrhythmic fails. When amiodarone is the first line treatment because class IC drugs are contraindicated, ablation can be considered if amiodarone fails.
The guidelines are less clear for patients with persistent atrial fibrillation. In such patients, catheter ablation can be considered for "severely symptomatic recurrent atrial fibrillation after failure of greater than or equal to one antiarrhythmic drug plus rate control." This recommendation is not based on strong evidence but is supported by small case series and randomised studies showing that restoration of sinus rhythm by catheter ablation may be associated with a significant improvement in left ventricular ejection fraction in patients with either heart failure induced by tachycardia or pre-existing heart failure.
Addition of clopidogrel to aspirin has been shown to provide incremental benefit over aspirin alone,but the reduction in risk with dual antiplatelet therapy is still not as great as that provided by warfarin.
The role of dual antiplatelet therapy in prevention of thromboembolic events in patients with AF is not clear.
Idiopathic Ventricular Fibrillation Is Becoming Less Idiopathic
More than 50% of individuals with idiopathic VF can ultimately receive diagnoses of a cardiac disease after a thorough investigation.Idiopathic ventricular fibrillation (VF) is defined as cardiac arrest in which the results of a reasonable cardiac work-up — including electrocardiogram, catheterization or stress test, and echocardiography — are normal. Idiopathic VF accounts for a sizable fraction of all cardiac arrests, especially in younger patients.
Journal Watch Cardiology September 2, 2009
In this study, patients with initial diagnoses of idiopathic VF at nine centers in Canada underwent a systematic, exceptionally thorough work-up. Evaluation included the standard tests described above plus cardiac magnetic resonance imaging, exercise testing and adrenaline challenge to examine for long QT syndrome (LQTS) and catecholaminergic polymorphic ventricular tachycardia (CPMVT), procainamide administration to examine for Brugada syndrome, and targeted genetic testing
Of 63 patients enrolled, 35 (56%) received more-specific diagnoses: LQTS in 8, CPMVT in 8, arrhythmogenic right ventricular cardiomyopathy in 6, early repolarization in 5, coronary spasm in 4, Brugada syndrome in 3, and myocarditis .
Major hemorrhage was defined as any overt bleeding requiring transfusion of at least two units of blood or any overt bleeding meeting the criteria for severe hemorrhage, which included any of the following: fatal hemorrhage, a drop in the hemoglobin level of 5.0 g per deciliter or more, hypotension requiring inotropic agents, intraocular bleeding leading to substantial loss of vision, requirement for surgical intervention, symptomatic intracranial hemorrhage, or requirement for transfusion of four units or more of blood. Minor bleeding was defined as any nonmajor bleeding associated with modification of the study-drug regimen.
• Antithrombotics (thrombolytics, anticoagulants and antiplatelet drugs)
• Vitamin K antagonists• Acenocoumarol • Clorindione • Coumatetralyl • Dicumarol (Dicoumarol) • Diphenadione • Ethyl biscoumacetate • Phenprocoumon • Phenindione • Tioclomarol • Warfarin
• Heparin group
• Antithrombin III • Danaparoid • Heparin • Sulodexide •
• low molecular weight heparin
• (Bemiparin, Dalteparin, Enoxaparin, Nadroparin, Parnaparin, Reviparin, Tinzaparin)
• Glycoprotein IIb/IIIa inhibitors
• Abciximab • Eptifibatide • Tirofiban
• Other platelet aggregation inhibitors
• Acetylsalicylic acid/Aspirin • Aloxiprin • Ditazole • Carbasalate calcium • Cloricromen • Dipyridamole • Indobufen • Picotamide • Triflusal • ADP receptor inhibitors (Clopidogrel, Ticlopidine, Prasugrel) • prostaglandin analogue (Beraprost, Prostacyclin, Iloprost, Treprostinil)
• Enzymesplasminogen activators
• (Alteplase/Reteplase/Tenecteplase, Streptokinase, Urokinase/Saruplase, Anistreplase) • other serine endopeptidases (Ancrod, Drotrecogin alfa/Protein C, Fibrinolysin) • Brinase
• Direct thrombin inhibitors
• Argatroban • Bivalirudin • Dabigatran • Desirudin • Hirudin • Lepirudin • Melagatran • Ximelagatran
• Other antithrombotics
• Apixaban • Defibrotide • Dermatan sulfate • Fondaparinux • Idraparinux • Otamixaban • Rivaroxaban
• Non-medicinal
• Citrate • EDTA • Oxalate
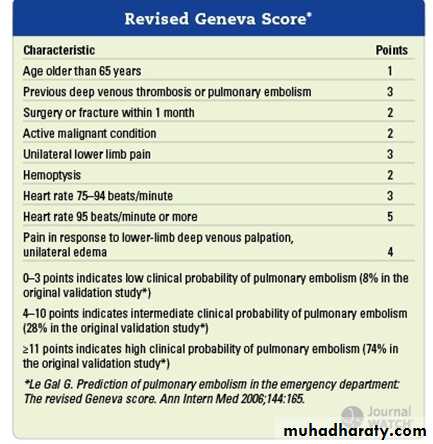
Another Validation of Clinical Assessment and D-Dimer to Rule Out PE
Among patients with low or intermediate risk, the sensitivity and negative predictive value of D-dimer testing were 100%.Despite research showing that clinically important pulmonary embolism (PE) can be excluded when patients with low clinical probabilities have negative D-dimer test results, many clinicians continue to order pulmonary computed tomography angiograms (CTAs) in virtually every patient with suspected PE.
Researchers conducted this study at a community teaching hospital in Chicago to determine the accuracy of clinical risk assessment plus D-dimer testing in 627 emergency department patients in whom clinicians considered PE as a diagnostic possibility. All patients underwent clinical risk assessment (using the previously published revised Geneva score ,D-dimer testing (using a quantitative immunoturbidimetric assay by Dade Behring), and CTA.
Comment: Among patients with low or intermediate risk for PE, the sensitivity and negative predictive value of D-dimer testing were 100% — i.e., no false-negatives were reported. Thus, patients with low or intermediate clinical probability scores and negative D-dimer test results — 27% of the cohort — could safely have avoided CT angiography. For patients with high clinical probability, the current consensus is to skip D-dimer testing and go directly to imaging.
Journal Watch General Medicine August 13, 2009
Arteriolosclerosis is any hardening (and loss of elasticity) of arterioles (small arteries). It is often due to hypertension.
Atherosclerosis is a hardening of an artery specifically due to an atheromatous plaque. Atherosclerosis is the most common form of arteriosclerosis. Atherosclerosis is characterized by a thickening of the intima with plaques that can contain lipid-laden macrophages ("foam cells"). The plaques contain free lipid (cholesterol, etc.) and are prone to calcification and ulceration.
Arteriosclerosis obliterans is typically seen in medium and large arteries of the lower extremity. Characterized by fibrosis of the intima and calcification of the media. The lumen of the vessel may be obliterated or markedly narrowed.
Medial calcific sclerosis (Monckeberg’s calcific sclerosis) is seen mostly in the elderly, commonly in arteries of the thyroid and uterus. Characterized by calcification of the internal elastic lamina but without thickening of the intima or narrowing of the vessel lumen. A similar form of an intramural calcification, presenting the picture of an early phase of arteriosclerosis, appears to be induced by a number of drugs that have an antiproliferative mechanism of action.
Diagnosis of venous thromboembolism
D-dimer tests can help management but cannot replace clinical judgment Because the signs and symptoms of deep venous thrombosis and pulmonary embolism are common but non-specific, they often present a diagnostic challenge. Both underdiagnosis and overdiagnosis are associated with substantial morbidity and mortality.BMJ 2009
D-dimers are fibrin degradation products resulting from endogenous fibrinolysis associated with intravascular thrombosis. A non-specific increase in D-dimer concentration is seen in many situations, precluding its use for diagnosing venous thromboembolism (VTE).
However, a low D-dimer concentration is thought to rule out the presence of circulating fibrin and therefore VTE. Early enzyme linked immunosorbent assay D-dimer tests took a long time to do, limiting their usefulness in acute care. Second generation assays provide results within an hour, and point of care tests produce results within 10-15 minutes.
Oral contraceptives and venous thromboembolism
Pills containing either levonorgestrel or norethisterone with the lowest possible dose of oestrogen are advised as first choice. More than 100 million women use the oral contraceptive pill worldwide. Venous thromboembolism is one of the most serious side effects, and although it is rare, it can cause death (in about 1-2% of all cases of venous thromboembolism in women taking the pill). All of the more recent progestogens, possibly except norgestimate, now seem to be at a disadvantage with regard to venous thromboembolism.BMJ 2009
However, the absolute risk of having venous thromboembolism is low—the baseline risk is five per 100 000 person years, and this increases to about 15-25 per 100 000 person years when taking the pill.1 This incidence is low enough to enable some negotiation when dealing with individual patients, for whom personal experiences or prejudices about side effects should be considered, and a pill containing a recent progestagen or a higher dose of oestrogen may be more appropriate.
Patients with a personal or family history of venous thromboembolism should not take combined oral contraceptives.
Hormonal contraception was categorised according to time of usage (current, previous, or never), regimen (combined oral contraceptives, progestogen only pills, or hormone releasing intrauterine device), oestrogen dose (50 µg, 30-40 µg, or 20 µg), type of progestogen (norethisterone, levonorgestrel, norgestimate, desogestrel, gestodene, drospirenone, or cyproterone), and length of use of combined oral contraceptives in current users (<1 year, 1-4 years, or >4 years). Progestogen only pills were subdivided into those containing 30 µg levonorgestrel or 350 µg norethisterone and those containing 75 µg desogestrel.
Progestogen only pills and hormone releasing intrauterine devices were not associated with any increased risk of venous thrombosis.
For women of normal weight and without known genetic predispositions, we recommend a low dose combined pill as first choice for contraception. For women genetically predisposed to venous thrombosis who still want hormonal contraception, however, a progestogen only pill or hormone releasing intrauterine device seems to be the appropriate first choice.
Before firm general clinical recommendations on type of progestogen can be made we need data on the effect of drospirenone on arterial end points.
BMJ 13 August 2009
For women with an increased body mass index; however, a low dose combined pill with levonorgestrel should be first choice. If the risk of arterial diseases is the same for the new progestogens as for levonorgestrel then according to our figures about 7400 women should change from the newer products to oral contraceptives containing levonorgestrel to prevent one case of venous thrombosis. The absolute risk of venous thrombosis with use of any types of combined oral contraceptives in young women is less than one in 1000 user years.
Currently available oral contraceptives increased the risk of venous thrombosis fivefold compared with non-use (odds ratio 5.0, 95% CI 4.2 to 5.8). The risk clearly differed by type of progestogen and dose of oestrogen. The use of oral contraceptives containing levonorgestrel was associated with an almost fourfold increased risk of venous thrombosis (odds ratio 3.6, 2.9 to 4.6) relative to non-users, whereas the risk of venous thrombosis compared with non-use was increased 5.6-fold for gestodene (5.6, 3.7 to 8.4), 7.3-fold for desogestrel (7.3, 5.3 to 10.0), 6.8-fold for cyproterone acetate (6.8, 4.7 to 10.0), and 6.3-fold for drospirenone (6.3, 2.9 to 13.7).
The Venous Thrombotic Risk of Oral Contraceptives
BMJ. 2009
The risk of venous thrombosis was positively associated with oestrogen dose. We confirmed a high risk of venous thrombosis during the first months of oral contraceptive use irrespective of the type of oral contraceptives.
The first report of an increased risk of venous thrombosis associated with oral contraceptives appeared in 1961.[1] Since then, several large studies have confirmed a twofold to sixfold increased risk of deep venous thrombosis associated with current oral contraceptive use.[2-5] To decrease the risk of thrombosis, the oestrogen dose in combined oral contraceptives was stepwise reduced over the years. A lowering of the oestrogen dose from 100 µg to 50 µg has been associated with a decreased risk of venous thrombosis.[6-8] There is no clear evidence that the lowering of the oestrogen dose to 30 µg or 20 µg led to a further decrease of the risk of deep venous thrombosis.
Oral contraceptives may contain different types of progestogens. First generation oral contraceptives contained lynestrenol, but these are now little used. Second generation oral contraceptives, which are widely used, contain levonorgestrel or, less often, norgestrel. Third generation oral contraceptives, containing desogestrel or gestodene, which became available in the 1980s, are also widely used. Two other types of oral contraceptives are not included in this classification. Preparations containing cyproterone acetate are used for treatment of acne vulgaris, seborrhoea, or mild hirsutism and have anti-ovulatory action similar to that of a progestogen.Preparations containing drospirenone, which is an antimineralocorticoid, also inhibit ovulation and have been on the market since 2001.
The risk was greatest in the first six weeks after surgery, peaking in the third week. Risk continued to be strong between seven and 12 weeks and stayed high for 12 months. This is clinically important because most patients receive preventive treatment only while in hospital, and median stays for surgical patients worldwide are six days.4 So in most cases, thromboprophylaxis stops two weeks before the peak incidence of VTE.
BMJ 3 December 2009
Prevention of postoperative venous thromboembolism
The current recommendations for prolonged prophylaxis vary and are limited to four weeks for some orthopaedic patients with hip fractures or hip replacements who have additional risk factors,5 or five weeks for patients having hip surgery and high risk general surgery.3 These recommendations advocate treatment for a shorter time than the length of high risk shown by Sweetland and colleagues, and in a more limited group of patients.
Glycosaminoglycans (GAGs) are the most abundant group of heteropolysaccharides found in the body. These long unbranched molecules contain a repeating disaccharide unit. GAGs are located primarily in the extracellular matrix or on the surface of cells. These molecules serve as lubricants in the joints while at the same time providing structural rigidity to cells. Sulodexide is a highly purified glycosaminoglycan composed of a fast mobility heparin fraction as well as dermatan sulfate.
Sulodexide differs from other glycosaminoglycans, like heparin, by having a longer half-life and a reduced effect on systemic clotting and bleeding. In addition, sulodexide demonstrates a lipolytic activity that is increased in comparison to heparin. Oral administration of sulodexide results in the release of tissue plasminogen activator and an increase in fibrinolytic activities. An increasing body of research has demonstrated the safety and efficacy of sulodexide in a wide range of vascular pathologies.
Upper-Extremity DVT as Prevalent as Lower-Extremity DVT in ICU Patients
There was a significantly higher incidence of upper-extremity DVT in patients with sepsis or central lines. "The treatment for upper-extremity DVT is the same as for lower-extremity DVT, and that is with anticoagulants. "One key difference is that most upper-extremity DVT is associated with the placement of a central venous catheter, so management should include removal of the line when possible, and the duration of therapy might not need to be as long as in lower-extremity DVT.
thromboembolism in travelers was twice as high as in nontravelers. It must be cautioned that although the relative risk for VTE was high, the absolute risk has been estimated to be 1 case per 4600 (or more) airline flights. For now, hydration and ambulation remain the best interventions for preventing travel-related VTE.
Travel and Venous Thromboembolism
Vitamin K antagonists are cumbersome to use, because of their multiple interactions with food and drugs, and they require frequent laboratory monitoring. Many patients receiving warfarin still have inadequate anticoagulation. Thus, there is a need for new anticoagulant agents that are effective, safe, and convenient to use.
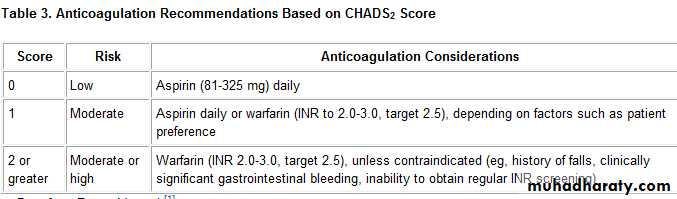
Scoring system for estimating risk of stroke patients with atrial fibrillation not associated with valvular disease CHADS-2. Risk factors
• Age >75 years—1 point
• Hypertension—1 point
• Diabetes mellitus—1 point
• Congestive heart failure—1 point
• History of stroke or transient ischaemic attack—2 points
Annual risk of stroke (based on points accrued)
0 points—1.9%1 point—2.8%
2 points—4.0%
3 points—5.9%
4 points—8.5%
5 points—12.5%
6 points—18.2%
• Scoring system for estimating risk of major bleeding related to warfarin*Risk factors
• Age >65 years—1 point
• History of stroke—1 point
• History of gastrointestinal bleeding—1 point
• Any, or several combined, of the following—1 point:
• -Diabetes mellitus
• -Recent myocardial infarction
• -Packed cell volume <30%
• -Creatinine >1.5 mg/l
Annual risk of stroke (based on points accrued)
Low risk (0 points)—0.8%Intermediate risk (1 to 2 points)—2.5%
High risk (3 to 4 points)—10.6%
*Using the bleeding risk index
Oral Antithrombin Dabigatran Outshines Warfarin in Atrial Fib
In the new trial, the Randomized Evaluation of Long-Term Anticoagulant Therapy (RE-LY), dabigatran given at 150 mg twice a day reduced the annualized risk of the primary end point, stroke/peripheral embolic events, by 34% (p<0.001) and the risk of hemorrhagic stroke by 74% (p<0.001) compared with warfarin. The higher dabigatran dose was associated with a slightly but significantly (p=0.048) increased risk of MI, a secondary end point.Dabigatran etexilate is an oral prodrug that is rapidly converted by a serum esterase to dabigatran, a potent, direct, competitive inhibitor of thrombin, excreted by the kidneys, its serum half-life is 12 to 17 hours, and it does not require regular monitoring. a large, randomized trial comparing the use of dabigatran, at doses of 110 mg twice daily and 150 mg twice daily, with warfarin.
The only adverse effect that was significantly more common with dabigatran than with warfarin was dyspepsia Dyspepsia occurred (5.8%) in the warfarin group and (11.8%) dabigatran groups. By selectively inhibiting only thrombin, dabigatran may have antithrombotic efficacy while preserving some other hemostatic mechanisms in the coagulation system and thus potentially mitigating the risk of bleeding.
The most devastating complication of warfarin therapy is intracranial hemorrhage, especially hemorrhagic stroke. As compared with aspirin, warfarin doubles the risk of intracranial hemorrhage. Thus, our finding that the rate of this complication with both doses of dabigatran was less than one third the rate with warfarin, without a reduction in the efficacy against ischemic stroke, suggests an important advantage of dabigatran.
The rate of myocardial infarction was higher with both doses of dabigatran than with warfarin. An explanation might be that warfarin provides better protection against coronary ischemic events than dabigatran, and warfarin is known to reduce the risk of myocardial infarction.
After a median follow-up of 2 years, dabigatran 110 mg twice daily was associated with a similar rate of stroke or systemic embolism as warfarin (1.53% vs 1.69%, respectively) and a lower rate of major hemorrhage (2.71% vs 3.36%, respectively); dabigatran 150 mg twice daily was associated with a lower rate of stroke or systemic embolism than warfarin (1.11% vs 1.69%, respectively), and a similar rate of major hemorrhage (3.11% vs 3.36%, respectively).
In an editorial accompanying the published RE-LY report [2], Dr Brian F Gage (Washington University, St Louis, MO) writes, "Because of dabigatran's twice-daily dosing and greater risk of nonhemorrhagic side effects, patients already taking warfarin with excellent INR [international normalized ratio] control have little to gain by switching to dabigatran." Dabigatran was associated with more dyspepsia in the trial, and more patients went off the drug than those who went off warfarin.
We did not find evidence of hepatotoxicity" from dabigatran, according to the published report from Connolly et al.
It was liver toxicity that had derailed the otherwise-promising oral thrombin inhibitor ximelagatran for the same clinical use, they observe.
Warfarin is clearly effective in preventing strokes in patients with AF who are at high risk, but it can also provide significant protection in patients with a low risk of stroke. A recent comparison of warfarin therapy with a regimen of clopidogrel plus aspirin reported treatment-specific rates of stroke and major bleeding for patients with AF and a CHADS2 score of 1 and compared the results in patients with a CHADS2 score greater than 1.19 The study found that even patients with a low risk of stroke (ie, CHADS2 = 1) derived a modest (<1% per year) but significant absolute reduction in stroke accompanied by low rates of major hemorrhage with warfarin.
The European Society of Cardiology has recently begun to recommend warfarin use in patients with AF and CHADS2 scores as low as 1, in contrast to the prior recommendation of equivalent consideration of aspirin.17 However, a number of factors, including significant variability in dose-response, drug and dietary interactions, and a narrow therapeutic window, have influenced some clinicians to underuse warfarin in this patient population.20 Underuse has subsequently driven a search for alternative orally administered antithrombotic agents that couple efficacy with a lower risk of major bleeding.
Several new and emerging anticoagulant agents, such as the factor Xa inhibitors apixaban and rivaroxaban, are in the late stages of development. The direct thrombin inhibitor dabigatran has recently been approved by the FDA for stroke prophylaxis in AF.18 Results from clinical trials suggest that dabigatran may provide a safe, effective alternative to warfarin in AF. Apixaban was superior to aspirin for stroke prevention in AF6; whether it is a viable alternative to warfarin in patients with AF remains to be seen.
Trials designed to make clinical comparisons between warfarin and rivaroxaban in AF are under way. The possibility of eliminating the need for continual INR testing is expected to offset a substantial portion of the cost of these new agents.
Ticagrelor — Is There Need for a New Player in the Antiplatelet-Therapy Field?
The thienopyridine clopidogrel, which irreversibly blocks the adenosine diphosphate (ADP) receptor P2Y12 on platelets, has become an essential component of therapy in patients with acute coronary syndromes, because it significantly improves the outcomes.1 However, clopidogrel has at least three drawbacks: delayed onset of action, large interindividual variability in platelet response, and irreversibility of its inhibitory effect on platelets .
NEJM Sept- 2009
The two-step activation process, involving a series of cytochrome P-450 (CYP) isoenzymes, is susceptible to the interference of genetic polymorphisms2 and drug–drug interactions.3 Patients with a poor response to clopidogrel have an increased risk of coronary thrombosis.4
The increased risk of bleeding due to prolonged persistence of the clopidogrel effect is of concern when patients need nondeferrable surgery such as urgent coronary-artery bypass grafting (CABG).
Ticagrelor, a cyclopentyl triazolopyrimidine, is rapidly absorbed in the intestine. The absorbed drug does not require further biotransformation for activation. It directly and reversibly binds to the platelet adenosine diphosphate (ADP) receptor P2Y12. The half-life of ticagrelor is 7 to 8 hours. The thienopyridines prasugrel and clopidogrel are prodrugs. Their active metabolites irreversibly bind to P2Y12 for the platelet's life span.
After intestinal absorption of clopidogrel, it requires two cytochrome P-450 (CYP)–dependent oxidation steps to generate its active compound. After intestinal absorption of prasugrel, it is rapidly hydrolyzed, by means of esterases, to an intermediate metabolite and requires one further CYP-dependent oxidation step to generate its active compound. Most of the CYP-dependent activation occurs in the liver. Relevant CYP isoenzymes involved in the activation of both clopidogrel and prasugrel are also shown. Their activity may be affected by genetic polymorphisms.
Prasugrel is a newer thienopyridine that also irreversibly binds to P2Y12. It has a more rapid onset of action and a stronger inhibitory effect than clopidogrel.5 As compared with clopidogrel, prasugrel shows lower variability in platelet response6 and no measurable vulnerability to genetic variation in CYP isoenzymes .However, the limitation of the irreversibility of the thienopyridine effect is even more evident with prasugrel than with clopidogrel.
Ticagrelor is an orally active drug that binds reversibly to P2Y12 ,with a stronger and more rapid antiplatelet effect than clopidogrel. In this issue of the Journal, Wallentin et al. report on the results of the Study of Platelet Inhibition and Patient Outcomes (PLATO), comparing ticagrelor with clopidogrel.9 As compared with clopidogrel, ticagrelor was associated with a 16% relative risk reduction with regard to the primary end point — a composite of death from cardiovascular causes, myocardial infarction, and stroke — but no significant increase in the overall risk of major bleeding.
PLATO is the third randomized trial evaluating novel antagonists of platelet ADP receptors in patients with acute coronary syndromes, following the Clopidogrel in Unstable Angina to Prevent Recurrent Events (CURE) trial and TRITON–TIMI 38 .Two striking differences among the outcomes of these three trials deserve special consideration .
First, in both the CURE trial and TRITON–TIMI 38, stronger platelet inhibition was associated with an increased risk of bleeding, whereas in PLATO, the risk of major bleeding was not increased with ticagrelor. As compared with clopidogrel, ticagrelor was associated with more frequent non–CABG-related bleeding, but it was safer than clopidogrel in patients undergoing CABG. This result highlights the important advantage of reversibility in the mechanism of action of ticagrelor.
Second, neither the CURE study nor TRITON–TIMI 38 showed a significant reduction in the mortality rate in association with stronger platelet inhibition. In PLATO, the rates of death from any cause were 4.5% with ticagrelor and 5.9% with clopidogrel, with a significant relative risk reduction (22%). This finding may simply reflect the play of chance, because the trial was not powered to detect differences in the mortality rate.
However, since the mortality rate in patients treated with antiplatelet drugs is determined by the risks of both ischemia and bleeding, ticagrelor may reduce the mortality rate by reducing the risk of death from ischemia without increasing the risk of death from bleeding. This hypothesis needs to be addressed in future investigations.
Third, new side effects, not seen with clopidogrel or prasugrel, were seen with the use of ticagrelor. These include dyspnea, bradyarrhythmia, and increased serum levels of uric acid and creatinine. Although they do not seem to have put patients at higher risk for death, these side effects may certainly have a negative effect on the quality of life. There was also a trend toward a higher risk of hemorrhagic stroke with ticagrelor than with clopidogrel, which becomes significant if cases of stroke classified as being of unknown origin are also counted as hemorrhagic strokes.
The availability of three agents for antagonizing platelet ADP receptors may make it possible to individualize antiplatelet therapy. In particular, ticagrelor therapy may be preferred in patients whose coronary anatomy is unknown and for whom a CABG procedure is deemed probable. If patients who are receiving clopidogrel or prasugrel need elective surgery, it is reasonable to switch them to ticagrelor 5 to 7 days before surgery.
NEJM Sept- 2009
Avoidance of the use of prasugrel in patients with a history of stroke or transient ischemic attacks has been advised.10 It seems prudent to apply the same advice to ticagrelor. The use of prasugrel has been discouraged in patients with an excessively high risk of bleeding.10 It might also be prudent to avoid the use of ticagrelor in patients with a high bleeding risk (presumably those with multiple risk factors).
Ticagrelor therapy should be discouraged in patients who have chronic obstructive pulmonary disease, hyperuricemia, moderate or severe renal failure, bradyarrhythmias unprotected by pacemakers, a history of syncope, or a need for treatment with an ADP-receptor antagonist for more than 1 year. We should further recognize that the rapidly reversible effect of ticagrelor makes careful surveillance of patients' compliance with the drug mandatory. For all remaining patients with acute coronary syndromes, either ticagrelor or prasugrel may be preferred, at least until data from studies specifically comparing these two agents become available.
Like clopidogrel and ticlopidine, ticagrelor blocks ADP receptors of subtype P2Y12. In contrast to the other antiplatelet drugs, the blockage is reversible. Moreover, it does not need hepatic activation, which could reduce the risk of drug interactions.
Ticagrelor
Weighing Benefits and Risks — The FDA's Review of PrasugrelThe (FDA) approved prasugrel on July 10, 2009. Developed by Eli Lilly and Daiichi Sankyo, prasugrel is a thienopyridine that inhibits platelet aggregation. It was approved for the reduction of thrombotic cardiovascular events in patients with acute coronary syndrome (unstable angina or myocardial infarction) who undergo percutaneous coronary intervention (PCI).
Refining Antiplatelet Treatment in Patients with Acute Coronary Syndromes
Clopidogrel's antiplatelet effect is hindered by the slow and variable biotransformation of the prodrug and by impaired response in a small minority of patients. Ticagrelor, a reversible, direct-acting, oral P2Y12 antagonist, inhibits more platelet aggregation faster and more consistently than clopidogrel.Journal Watch Cardiology September 2, 2009
bleeding was more common or more serious with prasugrel than with clopidogrel. Patients who received prasugrel and underwent CABG were at higher risk for bleeding; the frequencies of major or minor bleeding were 14.1% with prasugrel and 4.5% with clopidogrel. Among patients 75 years of age or older, fatal hemorrhage occurred in 9 of 891 patients in the prasugrel group (1.0%) versus 1 of 894 patients in the clopidogrel group (0.1%). However, older patients in two subgroups at particularly high risk (patients with diabetes and patients with a prior myocardial infarction) appeared to benefit substantially from prasugrel.
The principal advantage of prasugrel over clopidogrel appears to be the prevention of nonfatal myocardial infarctions, many of which would not have immediate overt clinical consequences. The cost of this prevention is excess bleeding — an important adverse effect, but one that is transient and does not result in increases in strokes or deaths. Ultimately, deciding which drug is preferable will be a matter of individual clinical judgment. The FDA made sure that prasugrel's label clearly articulates the balance between efficacy and risk — a balance that physicians will need to assess carefully when choosing treatment for individual patients.
NEJM Sept- 2009
• fondaparinux
• is a synthetic pentasaccharide that selectively inhibits factor Xa. can be administered daily without laboratory monitoring.• was compared with enoxaparin in 20,078 patients with acute coronary syndromes. Treatment of about 150 patients with fondaparinux rather than enoxaparin would result in three fewer bleeding events and one fewer death at 180 days.
The specific anti–factor Xa activity of fondaparinux, as compared with the antithrombin and anti–factor Xa effect of enoxaparin, may in part be responsible for its safer profile. Fondaparinux inhibits factor Xa within the clot, preventing thrombus progression and thus enhancing effectiveness, but does not inhibit platelet function, thus enhancing safety.
The ACCF/AHA 2009 Expert Consensus Document on Pulmonary Hypertension: A Report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents
Pulmonary arterial hypertension (PAH) is a syndrome resulting from restricted flow through the pulmonary arterial circulation, resulting in increased pulmonary vascular resistance (PVR) and ultimately in right heart failure. Multiple pathogenic pathways are responsible for modifying smooth muscle and endothelial cells and adventitia, and the imbalance in the vasoconstrictor/vasodilator milieu.
The prevalence of PAH is 15 per million in the French registry.
1. Idiopathic PAH (IPAH) is the most common type of PAH and is more common in women. Familial PAH often results from a mutation in the bone morphogenic protein receptor-2 and is inherited as an autosomal dominant disease with incomplete penetrance and genetic anticipation.2. PAH is also associated with congenital heart disease (CHD),
3. connective tissue diseases,4. drugs and toxins,
5. human immunodeficiency virus,
6. portal hypertension,
7. hemoglobinopathies, and
8. myeloproliferative disorders.
The 1-year mortality in PAH is about 15% on modern therapy. Predictors of a poor prognosis include: advanced functional class, poor exercise capacity, high right atrial pressure, significant right ventricular (RV) dysfunction, RV failure, low cardiac index, elevated brain natriuretic peptide, and the scleroderma spectrum of diseases.
Patients at sufficient risk for the development of PAH to warrant periodic screening include those with a family history of IPAH, scleroderma spectrum of diseases, and portal hypertension who are undergoing evaluation for liver transplantation. The most appropriate study to obtain in patients suspected of having PH is an echocardiogram.
The diagnosis
Requires confirmation with a complete right heart catheterization. The hemodynamic definition of PAH is a mean pulmonary artery pressure >25 mm Hg; a pulmonary capillary wedge pressure (PCW), left atrial pressure, or left ventricular end-diastolic pressure ≤15 mm Hg; and a PVR >3 Wood units. Acute vasodilator testing should be performed in experienced centers on IPAH patients to screen eligibility for long-term calcium channel blocker (CCB) therapy. Exceptions include those with overt right heart failure or hemodynamic instability.General treatment measures include
diet, exercise, appropriate vaccinations, and avoidance of pregnancy. Warfarin anticoagulation is recommended in all patients with IPAH. Diuretics are used for symptomatic management of RV volume overload. Oxygen is recommended to maintain oxygen saturation >90%. Acute responders to vasodilator testing treated with CCB should be followed closely for both the safety and the efficacy of this therapy.Continuous intravenous epoprostenol improves exercise capacity, hemodynamics, and survival in IPAH and is the preferred treatment option for the most critically ill patients. Treprostinil, a prostanoid, may be delivered via either continuous intravenous or subcutaneous infusion. Iloprost is a prostanoid delivered by an adaptive aerosolized device 6 times daily.
The endothelin receptor antagonists (ETAs) are oral therapies that improve exercise capacity in PAH. Liver function tests must be monitored indefinitely on a monthly basis. Phosphodiesterase (PDE)-5 inhibitors also improve exercise capacity and hemodynamics in PAH. Patients with poor prognostic indexes should be initiated on parenteral therapy, while patients with class II or early III symptoms can commence therapy with either ETAs or PDE-5 inhibitors. Initial trials suggest that combination therapy may be useful.
Lung transplantation is an option for selected patients who progress despite optimal medical management.
Due to the complex nature of the disease and its treatments, PAH patients must be closely followed by experienced physicians and nurse clinicians. In general, office visits should be more frequent for patients with advanced symptoms, right heart failure, and advanced hemodynamics and those on parenteral or combination therapy. Most experts obtain an assessment of functional class and exercise capacity, such as a 6-minute walk or graded treadmill test, with each office visit.
Any disorder that elevates left heart filling pressures, including systolic dysfunction, diastolic dysfunction, and valvular heart disease, can result in elevated pulmonary artery pressures. In rare instances, PAH-specific therapy may be considered if the underlying cause has been optimally treated, the PCW is normal or minimally elevated, and the transpulmonary gradient and PVR are significantly elevated. The latter is known as “disproportionate” PH or greater than expected on the basis of the elevated left heart pressure or lung disease. The potential adverse effects of PAH-specific therapies in such patients include worsening fluid retention, pulmonary edema, and ventilation perfusion mismatch.
August 4, 2009 — The US Food and Drug Administration (FDA) has approved treprostinil inhalation solution (Tyvaso, United Therapeutics Corp) for increasing walk distance in patients with New York Heart Association class 3 symptoms associated with World Health Organization group 1 pulmonary arterial hypertension (PAH).administered 4 times daily, contains the same active ingredient as treprostinil sodium injection . (Remodulin, United Therapeutics), which is also approved for the treatment of PAH.
Adverse events most commonly reported in the study (incidence ≥ 10%) included cough, headache, nausea, dizziness, flushing, throat irritation, pharyngolaryngeal pain, and diarrhea.Treprostinil inhalation solution has not been studied in patients with significant underlying lung disease (eg, asthma or chronic obstructive pulmonary disease) and should be used with caution in those with acute pulmonary infections.Also may increase the risk for hypotension in patients with low systemic arterial pressure and those receiving diuretics, antihypertensives, or other vasodilator therapies.An additional study will evaluate the long-term risk for oropharyngeal and pulmonary toxicities .
Results of well-controlled study show that arterial events (mainly myocardial infarction and stroke) occur more often in patients with unprovoked PE than in either matched controls or those with provoked PE. This finding suggests that a shared pathophysiological mechanism underlies events in both venous and arterial systems and raises the issue of whether patients with unprovoked VTE should receive prophylactic agents that have proven to be effective for the prevention of arterial events.
Journal Watch Oncology and Hematology September 22, 2009
Two-thirds of all clots have no identifiable cause, and this is the subject of ongoing research.Two risk factors recently discovered are Factor V Leiden and an elevated homocysteine level.
Q. What is Factor V Leiden? Factor V Leiden is a hereditary condition present in 15-20% of PE/DVT patients of European ancestry. A positive test for Factor V Leiden increases the risk of clots about three to four times compared to someone without it. In general, this risk is still small.
However, if you are taking oral contraceptives and you have Factor V Leiden, the risk of a clot increases dramatically (about 35-fold). If you have Factor V Leiden, the risk of clots also increases with age. For Factor V Leiden patients who stop anticoagulant therapy after treatment, the risk for a second clot is about three times greater than for those without it.
Q. If I have Factor V Leiden, should family members be tested for it? If family members are considering taking oral contraceptives or becoming pregnant, they may wish to be tested. Recommendations for family testing remain controversial.
Q. What is homocysteine? A. Homocysteine is a byproduct of protein metabolism that promotes clotting via an unknown mechanism. An elevated homocysteine level is treatable with folic acid, B6, and B12. This condition (hyperhomocysteinernia) is much less common than the Factor V Leiden mutation.
Is the VQ scan the best non-invasive method for detecting a PE? A. It is the best current non-invasive technique for detecting a PE.
Spiral CT (computed tomography) imaging is a new non-invasive technique being developed and has potential for replacing the VQ scan.
Q. Do Coumadin and Heparin dissolve clots? A. No, they prevent new clots from forming.
Q. What happens to a clot after anticoagulation therapy has begun? A. Over time, the body will usually dissolve some, but not all, of the clot. The remainder of the clot embeds in the vessel wall and becomes scar tissue.Q. What is an INR? A. International Normalized Ratio or standardized prothrombin time (PT). This is a measure of how long it takes for blood to clot.
Q. Will anticoagulation therapy cause changes in menstruation? A. Usually not.
Q. Is it safe to breastfeed while on Coumadin? A. Yes.
A selective endothelin-receptor antagonist to reduce blood pressure in patients with treatment-resistant hypertension
We investigated the blood-pressure-lowering effects of the new vasodilatory, selective endothelin type A antagonist, darusentan, in patients with treatment-resistant hypertension. Darusentan provides additional reduction in blood pressure in patients who have not attained their treatment goals with three or more antihypertensive drugs. As with other vasodilatory drugs, fluid management with effective diuretic therapy might be needed.
Resistant hypertension — blood pressure (BP) that remains above the target level, despite treatment with a diuretic and optimal doses of at least two other drugs (10% to 15% of all cases of hypertension), —
is associated with older age,
obesity,
diabetes, and chronic
kidney disease;
One explanation may be that the patient has an underlying so-called "secondary cause'" for hypertension that does not respond to drugs -- for example, an adrenal cortex tumor, a pheochromocytoma, renal artery stenosis, or advanced kidney disease. The other main cause of not responding adequately despite a good treatment regimen is that the patient is taking a medication that is raising blood pressure and interfering with the actions of the antihypertensive drugs. Culprits include nonsteroidal anti-inflammatory drugs (NSAIDs), oral contraceptives, and some common cold remedies.
Aliskiren: An Oral Direct Renin Inhibitor for the Treatment of Hypertension
By inhibiting renin, aliskiren blocks the conversion of angiotensinogen to angiotensin I, which subsequently results in a reduction in angiotensin II concentrations. Unlike the angiotensin-converting enzyme inhibitors and the angiotensin II receptor blockers (ARBs), which reactively stimulate an increase in plasma renin activity, aliskiren suppresses the effects of renin and leads to a reduction in plasma renin activity, aliskiren provided antihypertensive efficacy that was comparable to that of an ARB..Combination therapy with aliskiren and an ARB may provide additional blood pressure-lowering effects compared with the respective monotherapies with each of the agents. Because aliskiren does not significantly affect the cytochrome P450 system, it has been associated with few drug interactions.
In clinical studies, aliskiren was well tolerated, and its adverse-effect profile was similar to that of placebo. Fatigue, headache, dizziness, diarrhea, nasopharyngitis, and back pain were the most commonly reported adverse events. Overall, aliskiren appears to be a reasonable treatment option for patients with mild-to-moderate hypertension who are intolerant of first-line antihypertensive therapies. Aliskiren may also be a promising renoprotective strategy in patients with concomitant hypertension and diabetes mellitus.
By acting at an earlier step of the RAS cascade, aliskiren has the theoretical advantage, over ACEIs, of inhibiting the synthesis of angiotensin I, thereby eliminating the main substrate for the 'escape' phenomenon. On the other hand, ACEIs may induce vasodilation and natriuresis by inhibiting the degradation of bradykinin, an effect not shared by aliskiren. Unfortunately, increased levels of kinines may also cause cough and angioneurotic edema, thereby worsening tolerability of ACEIs.
Over the past 2 years, three studies have been published which directly compared aliskiren with ramipril in patients with hypertension [Duprez et al. 2009; Andersen et al. 2008; Uresin et al. 2007]. These three studies were remarkably consistent in showing a definite, albeit slight, superiority of aliskiren over ramipril in reducing systolic BP.
Potential Explanations
It could be speculated that aliskiren, by reducing the levels of angiotensin I, the main substrate for the 'escape' phenomenon, may have induced a more complete and effective 'upstream' inhibition of the synthesis of angiotensin II as compared with ramipril. On the other hand, the rise in plasma renin concentration under aliskiren treatment does not seem to be associated with 'escape' angiotensin I production in the long term.Another potential explanation is related to the long terminal elimination half-life of aliskiren, which approximates 40 hours .This contrasts with the shorter halflife of ramiprilat, the active metabolite of ramipril, which approximates 13–17 hours.
The antihypertensive efficacy of aliskiren is increased by combination with drugs that elicit a reactive increase in the plasma renin activity such as diuretics, ACEIs and ARBs [Andersen et al. 2007; Oparil et al. 2007; Strasser et al. 2007; Villamil et al. 2007; Uresin et al. 2006; Gradman et al. 2005; Stanton et al. 2003]. In this setting, aliskiren appears to be particularly indicated in patients who are intolerant to ACEIs, as well as in those with elevated activity of the renin—angiotensin system, often found in White subjects and young people.
Aliskiren is generally well tolerated, with a placebo-like profile at doses of 150 and 300mg [Weir et al. 2006]. Diarrhea is more frequent than with placebo only outside the marketed range at the dose of 600mg [Brown, 2008]. Of particular note, the hepatic route of elimination of aliskiren makes this drug suitable also in patients with reduced kidney function. In addition, because of its highly specific mode of action, aliskiren does not interfere with several agents including warfarin and statins. Pregnancy and bilateral renal artery stenosis are the two main contraindications to the use of aliskiren.
Hypertension, diabetic nephropathy and heart failure are clinical conditions for which aliskiren appears particularly attractive. In the Aliskiren in the Evaluation of Proteinuria in Diabetes (AVOID) Trial [Parving et al. 2008], aliskiren reduced the urinary albumin creatinine ratio by 18% as compared with placebo in hypertensive patients with type 2 diabetes and macroalbuminuria. In the aliskiren observation of heart failure treatment (ALOFT) study [McMurray et al. 2008], aliskiren significantly reduced, compared with placebo, the plasma N-terminal prohormone brain natriuretic peptide (NT-pro BNP), BNP and urinary aldosterone. In the Aliskiren in Left Ventricular Hypertrophy (ALLAY) study [Solomon, 2008], aliskiren was as effective as losartan in inducing left ventricular hypertrophy regression in hypertensive patients.
Endothelin-1 receptor antagonists are believed to be potentially useful in resistant hypertension. They are currently used in the treatment of primary pulmonary hypertension, but proved disappointing in trials in patients with congestive heart failure (CHF). Endothelin-1 is a potent endogenous vasoconstrictor that also can exert proliferative, inflammatory, and fibrotic changes in blood vessels and other organs. Stimulation of endothelin A (ETA) and endothelin B (ETB) receptors results in different and often opposing effects that contribute to the regulation of vascular tone and blood pressure. Dysregulation of the endothelin system can induce or mediate endothelial dysfunction and organ damage in systemic hypertension.
Both selective and dual-acting endothelin receptor blockers have been shown to reduce systemic blood pressure in healthy and hypertensive humans.[9,10] However, it has been suggested that as well as potentially improving endothelial function, reducing inflammation fibrosis, and reversing vascular remodeling, selective ETA blockade may produce additional benefits of renoprotection beyond those associated with the renin-angiotensin system. Chronic treatment with ETA antagonists has been shown to reduce urinary protein excretion, limit glomerular injury, and prevent renal dysfunction in patients with diabetes and chronic kidney disease.
One of the interventional approaches being developed for the management of
resistant hypertension is a percutaneous catheter-based procedure to ablate the renal sympathetic nerves via the lumen of the main renal artery using a catheter connected to a radiofrequency generator . First results were presented at the 2009 annual meeting of the American College of Cardiology . They indicated that renal denervation produced substantial, sustained reductions in blood pressure, with no renovascular complications.Activating the Carotid Sinus Baroreflex
An implantable device being developed for the treatment of resistant hypertension. It acts to control blood pressure by electrical activation of the carotid sinus baroreflex. The Rheos® system consists of the pulse generator, a small device similar to a pacemaker that is implanted under the collarbone; 2 thin lead wires are implanted at the left and right carotid arteries and connected to the pulse generator; and an external device is used to noninvasively regulate the activation energy from the generator to the lead wires.
Two open-label safety and efficacy trials were conducted with the Rheos® system: the Rheos® Feasibility Trial in the United States, and the CVRx Device Based Therapy in Hypertension Trial (DEBuT-HT) in Europe. Both trials enrolled patients with resistant hypertension, defined as blood pressure ≥ 160 mm Hg SBP and/or ≥ 90 mm Hg DBP despite at least 2 months of full therapy with 3 or more antihypertensive medications, including at least 1 diuretic. In all patients the Rheos® system was surgically implanted and activated 1 month later. Patients showed sustained decreases in blood pressure after 1 year in both studies.
Two-year data for 38 patients, presented at the 2009 annual meeting of the American College of Cardiology,showed that blood pressure reductions seen at 1 year were sustained at 2 years and were even greater at 3 years. All blood pressure reductions were significant compared with baseline and most patients reduced their SBP to ≤ 150 mm Hg at 3 years. Heart rate was also significantly reduced at all 3 time points.
It is generally recommended that
orthostatic blood pressure be measured while the patient is in the standing position every minute during the first 3 minutes after he or she has been lying supine for 5 minutes.2 If the patient cannot stand for this period of time, the lowest systolic blood pressure should be recorded.Orthostatic hypotension is a physical sign defined as a reduction of at least 20 mm Hg in systolic blood pressure or of at least 10 mm Hg in diastolic blood pressure within 3 minutes after standing.3
Guidelines for the management of hypertension recommend that orthostatic blood pressure be assessed in patients with diabetes, the elderly, patients receiving antihypertensive treatment, and patients with other conditions in which orthostatic hypotension may be common or suspected.4,5 The diagnosis of orthostatic hypotension is extremely important, since this condition is responsible for recurrent symptoms such as syncope, dizziness, and light-headedness, as well as serious injuries and deterioration in the quality of life.
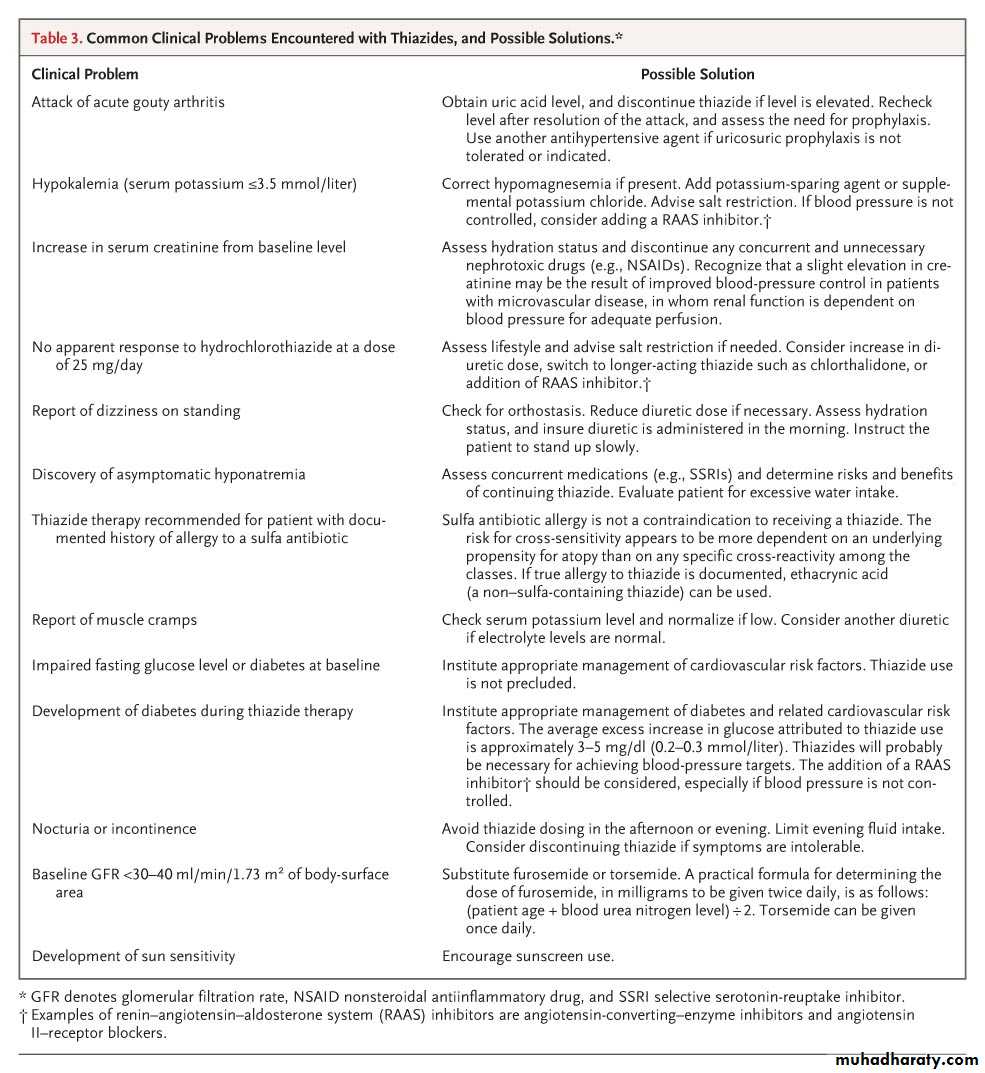
Use of Diuretics in Patients with Hypertension
Clinical Pharmacology of ThiazidesChlorothiazide, a benzothiadiazine derivative, was isolated during a search for more potent inhibitors of carbonic anhydrase5; chlorothiazide was found to be a more effective diuretic and also to unexpectedly increase the excretion of chloride, rather than bicarbonate. This effect on excretion eventually led to identification of the upstream portion of the distal convoluted tubule as the major site of action of the thiazides, where they interfere with sodium reabsorption by inhibiting the electroneutral sodium–chloride symporter .
Activity against carbonic anhydrase, although maintained by some thiazides, is considered irrelevant to their mechanism of action, since sodium that is rejected proximally is reabsorbed downstream in the renal tubule in the thick ascending limb. Despite structural variation among the different congeners, the term thiazide diuretic includes all diuretics believed to have a primary action in the distal tubule. The onset of action occurs after approximately 2 to 3 hours for most thiazides, with little natriuretic effect beyond 6 hours.
The long-term antihypertensive response to thiazides cannot be reliably predicted by the degree of initial reduction in plasma volume, which eventually returns to near-normal levels. Volume expansion due to the use of dextran at this stage no longer restores the blood pressure to pretreatment levels. A more likely explanation for the persistent antihypertensive effects of most thiazides is an overall reduction in systemic resistance, although the exact mechanisms are unclear. Evidence suggests that chlorthalidone may not lower systemic resistance, even after 8 to 12 months of therapy, indicating that other mechanisms may be responsible.
It is not yet clear whether thiazides have direct vasodilatory properties or induce a reverse autoregulation phenomenon; they have also been proposed to cause structural membrane changes or altered ion gradients.24 A simpler possibility is that a low level of prolonged diuresis produced by long-term thiazide administration may maintain a nominal state of volume contraction, thereby promoting a downward shift in vascular resistance.
Tolerance to Diuretics
The use of diuretics elicits both short- and long-term adaptations intended to protect intravascular volume. Short-term tolerance may result from a period of post-dose antinatriuresis triggered by the initial reduction in extracellular fluid volume, corresponding to a decline in the drug level in plasma and tubular fluid to below the diuretic threshold. Activation of the renin–angiotensin–aldosterone system and the sympathetic nervous system, as well as suppression of the secretion of atrial natriuretic peptide and renal prostaglandin, also contribute to short-term tolerance. Post-dose sodium retention is significantly influenced by dietary sodium intake. Sodium restriction promotes an overall negative sodium balance and enhances the therapeutic response to thiazides, whereas persistently high dietary sodium offsets this effect.Long-term diuretic adaptation, or the braking effect, refers to a gradual return of the sodium–chloride balance to an electroneutral level. Persistent volume removal appears to trigger long-term activation of the renin–angiotensin–aldosterone system, increasing circulating angiotensin II levels, which in turn promotes increased proximal sodium reabsorption and limits the overall delivery of sodium to the distal site. Other volume-independent mechanisms may be involved, including the up-regulation of sodium transporters downstream from the primary site of diuretic action and structural hypertrophy of distal nephron segments.
Tolerance to diuretics can be overcome by administering higher doses or combinations of diuretics. For example, synergistic diuresis occurs when a thiazide is added to loop-diuretic monotherapy in patients with edema.32 Occult volume expansion can be present in patients with resistant hypertension, despite existing diuretic therapy; increasing the dose of diuretics may improve the blood pressure.33
High doses and combinations of diuretics must be used carefully to avoid renal injury and marked electrolyte disturbances.
Many physicians consider thiazides the diuretics of choice for long-term therapy. On average, after adjustment for reductions seen with the use of placebo, thiazides induce a reduction in the systolic and diastolic blood pressures of 10 to 15 mm Hg and 5 to 10 mm Hg, respectively. Hypertension responding preferentially to thiazides is considered to be low-renin or salt-sensitive hypertension. The elderly, blacks, and patients with characteristics associated with high cardiac output (e.g., obesity) tend to have this type of hypertension. Thiazides also correct the hypertension and electrolyte abnormalities associated with pseudohypoaldosteronism type 2 (Gordon's syndrome), a rare mendelian form of hypertension in which the sodium–chloride symporter is excessively active.
Combined meta-analyses and systematic reviews report that, as compared with placebo, thiazide-based therapy reduces relative rates of heart failure (by 41 to 49%), stroke (by 29 to 38%), coronary heart disease (by 14 to 21%), and death from any cause (by 10 to 11%). These and other analyses also show that the benefit from thiazides is broadly similar to that from other antihypertensive drugs, with results consistent across age and sex strata.
Thiazides potentiate other antihypertensive agents when they are used in combination, often producing an additive decrease in blood pressure. The addition of a thiazide minimizes racial differences usually observed in response to monotherapy with inhibitors of the renin–angiotensin–aldosterone system, and the use of such an inhibitor can lessen the degree of the hypokalemia and the metabolic perturbations that may be evoked by thiazides.
Safety and Adverse Effects of Thiazides
Much of the criticism against thiazides is directed toward their adverse-effect profile, but low doses are usually well tolerated and have been shown to improve quality-of-life measures.77 Most complications of thiazide therapy are related to the dose and duration of use.Diuretics in Renal Impairment
Thiazides are typically considered ineffective when the glomerular filtration rate decreases below 30 to 40 ml per minute per 1.73 m2 of body-surface area, although direct evidence is lacking. Small studies have shown that thiazides can elicit an antihypertensive response in patients with chronic kidney disease; however, their use in patients with severe renal impairment remains impractical, for two reasons:first, the reduced glomerular filtration rate limits the overall filtered sodium load reaching the distal tubule; and
second, reabsorption in the distal tubule is only modestly effective as compared with that in the large-capacity, thick ascending limb.12 These features underscore the rationale for substituting so-called high-ceiling diuretics that act more proximally, in the loop of Henle, in hypertensive patients with renal impairment.
Metolazone, a quinazoline derivative, is an exception among thiazides because it retains its efficacy in patients who have renal insufficiency or other diuretic-resistance states. Its effect is limited by slow, erratic absorption; the more predictable bioavailability of other thiazides makes them better suited as long-term therapy of hypertension. Metolazone should be reserved for use in combination with loop diuretics in patients with volume overload whose fluid and electrolyte balance are being closely monitored. It is administered daily for a short period (3 to 5 days), with administration reduced to thrice weekly after this period or after euvolemia is achieved
Loop Diuretics
Diuretics that act in the loop of Henle can lower blood pressure but are less effective in the long term than thiazides. Most loop diuretics have a short duration of action (approximately 6 hours), resulting in an initial diuresis that is followed closely by a period of antinatriuresis lasting up to 18 hours per day when the drug is administered once daily. A net neutral sodium balance, or even a positive balance, can occur with the use of loop diuretics.These agents are most appropriate for the treatment of hypertension that is complicated by a reduced glomerular filtration rate (<30 to 40 ml per minute per 1.73 m2 of body-surface area) or by volume overload (e.g., in congestive heart failure or the nephrotic syndrome); in patients with such complications, loop diuretics provide consistent natriuresis and diuresis.
Furosemide should be administered twice daily, whereas torsemide is a longer-acting alternative that may be administered once daily.
Potassium-Sparing Agents and Mineralocorticoid-Receptor Antagonists
Induce only minimal natriuresis and are relatively ineffective in lowering blood pressure .Their primary value is their ability to reduce the loss of potassium when they are used with thiazides. They also avert the urinary loss of magnesium, which is important, since restoration of magnesium balance is necessary for optimal correction of diuretic-induced hypokalemia. Triamterene is commonly administered with hydrochlorothiazide, although other fixed-dose combinations of thiazides and potassium-sparing agents are available. Amiloride, an epithelial sodium-channel blocker, is reportedly more effective than spironolactone as therapy in blacks who have resistance to treatment.The phenomenon of aldosterone escape, whereby aldosterone activity is incompletely suppressed in hypertensive patients who are receiving inhibitors of the renin–angiotensin–aldosterone system, can lead to increased salt and water retention. Agents that block the effect of aldosterone are useful for treating this retention. Spironolactone, a nonselective mineralocorticoid-receptor antagonist, is well absorbed and has a long half-life (approximately 20 hours), attributable to its active metabolites.
Spironolactone not only corrects thiazide-induced potassium and magnesium losses, but also, in low doses (12.5 to 50 mg per day), provides additive hypotensive effects in patients who have resistance to treatment.44 Spironolactone remains effective when renal function is impaired, but patients must be monitored carefully for the development of hyperkalemia.
Eplerenone, a newer agent that is more selective for aldosterone than for androgen and progesterone receptors, is associated with less gynecomastia and breast tenderness than is found with spironolactone. However, direct comparisons of the efficacies of eplerenone and spironolactone in patients with treatment-resistant hypertension are lacking.
Specialists have known for a long time that renal artery stenosis (RAS) is the major cause of renovascular hypertension and that it may account for 1-10% of the 50 million people in the United States who have hypertension.
Apart from its role in the pathogenesis of hypertension, renal artery stenosis is also being increasingly recognized as an important cause of chronic renal insufficiency and end-stage renal disease.
In older individuals, atherosclerosis (ATH) is by far the most common etiology of renal artery stenosis. As the renal artery lumen progressively narrows, renal blood flow decreases and eventually compromises renal function and structure.
Pathophysiology
In patients with ATH, the initiator of endothelial injury is not clear; however, dyslipidemia, hypertension, cigarette smoking, diabetes mellitus, viral infection, immune injury, and increased homocysteine levels may contribute to endothelial injury. In the atherosclerotic lesion site, endothelium permeability to plasma macromolecules (eg, low-density lipoprotein [LDL]) increases, turnover of endothelial cells and smooth muscle cells increases, and intimal macrophages increase. When atherogenic lipoproteins exceed certain critical levels, the mechanical forces may enhance lipoprotein insudation in these regions, leading to early atheromatous lesions.The degree of renal artery stenosis that would justify any attempt at either surgical intervention or radiologic intervention is not known. A recent study suggested that a ratio of pressure, measured distal to renal artery stenosis, less than 90% relative to aortic pressure, was found to be associated with significant renin release from the affected kidney, renin being measured in the ipsilateral renal vein. This might be useful as a functional measurement of significant renovascular stenosis leading to hypertension and, thus, a marker of those individuals more likely to benefit from angioplasty and stenting.
Renal ultrasound is performed frequently in patients with renal dysfunction.
Ultrasound is an anatomic, not a functional, test. The only contribution to the entity of renal artery stenosis is a suggestion of the diagnosis when examination results indicate significant asymmetry of kidney size (ie, size discrepancy of >1.5 cm).Additionally, ultrasound may be useful in detecting the presence of a solitary kidney, in which case, renal artery stenosis of that solitary kidney takes on more significant prognostic and therapeutic importance.
Imaging Studies Ultrasound
Radionuclide scanning
Use of radionuclide scanning, particularly following a single dose of captopril, is more useful in patients with normal renal function, in whom fibromuscular disease is suspected.Patients with possible ischemic nephropathy (ie, serum creatinine values >2 mg/dL) frequently have associated parenchymal disease or bilateral vascular disease, in which case, the results obtained with scanning are unable to distinguish between parenchymal renal disease and renal artery stenosis/ischemic nephropathy.
Duplex ultrasound scanning
This noninvasive diagnostic technique combines a B-mode ultrasound image with a pulse Doppler unit to obtain flow velocity data.The test is very sensitive and specific (98%); however, it is very labor intensive and technician-dependent.
In a study reported in the New England Journal of Medicine, Radermacher et al were able to use the renal resistance index value to predict the outcome of therapy in patients aggressively treated for renal artery stenosis.5 Specifically, an index of greater than 80, indicating small vessel and large vessel disease, was indicative of a poor response to either angioplasty or surgery with respect to improvement in hypertension, renal function, or kidney survival.
SpiralCT angiography
This technique involves the use of an intravenous injection of a relatively large dose of iodinated contrast material and allows 3-dimensional reconstruction images of the renal arteries. In 1995, Olbricht et al compared renal CT angiography with arterial digital subtraction angiography for detecting renal artery narrowing of more than 50%.6 The CT technique showed positive and negative predictive values of 91%. SpiralCT angiography is a useful technique that avoids arterial catheterization and produces accurate images of renal artery anatomy. This technique requires iodinated contrast material and significant time to perform the computer-based reconstruction. This technique avoids arterial puncture and, thus, the risk of atheroemboli, but it can be associated with contrast associated nephropathy, particularly in patients with preexisting chronic kidney disease.
Magnetic resonance angiography
(MRA) is a noninvasive technique capable of demonstrating the renal vascular anatomy and revealing physiological information about kidney function. is capable of direct visualization of renal artery lesions without iodinated contrast material and provides a measurement of the absolute blood flow rate, GFR, and renal perfusion rate. Furthermore, MRA can provide accurate serial renal size and volume measurement. The limitations of MRA are its expense and its contraindication in patients with metallic clips, pacemakers, intraocular metallic devices, or other implants.Recent concern regarding the association of gadolinium use with the development of nephrogenic systemic fibrosis in patients with moderate-to-severe renal insufficiency significantly limits the use of this agent and, therefore, this modality for the recognition of anatomic renal artery stenosis.The technique has been validated only for the stenosis situated in the proximal 3-3.5 cm of renal arteries. Distal renal artery stenosis and segmental renal artery stenosis were generally not analyzed. The sensitivity of MRA was 90% for proximal renal artery stenosis, 82% for main renal artery stenosis, and 0% for segmental stenosis.
An additional study compared the accuracy of CT angiography and MRA to digital subtraction angiography and concluded that digital subtraction remains the method of choice to establish a diagnosis.
Conventional arteriography
This technique remains the criterion standard for the confirmation and identification of renal artery occlusion in persons with IRD. Specialists can perform renal arteriography by conventional aortography, intravenous subtraction angiography, intra-arterial subtraction angiography, or carbon dioxide angiography.Conventional aortography produces excellent radiographic images of the renal artery, requires an arterial puncture, carries the risk of cholesterol emboli, and uses a moderate amount of contrast material with the risk of contrast-induced acute tubular necrosis (ATN).
Contrast nephrotoxicity
Patients with progressive ischemic nephropathy (ie, underlying chronic renal failure) are at risk for contrast nephrotoxicity and should be informed of this risk prior to any contrast procedure.Contrast nephropathy typically manifests as a brief rise in the serum creatinine level 3-6 days after exposure to radiocontrast and is reported in up to 40% of patients with underlying renal failure.
Most patients with contrast nephropathy ultimately recover renal function. Porter reviewed results from nearly 300 patients with contrast nephropathy and concluded that fewer than 10% of these patients required dialysis permanently.
Renal Artery Stenosis: Treatment & Medication
All patients with significant (>80%) bilateral stenosis and stenosis in a solitary functioning kidney are candidates for revascularization, regardless of whether they have renal insufficiency. When renal insufficiency is present, patients with unilateral stenosis are also possible candidates for revascularization.Restrict conservative treatment in patients with an established diagnosis of IRD to those with absolute contraindications to surgery or angioplasty or to patients who are likely to succumb due to other comorbid conditions before advancing to end-stage renal disease because of IRD. Clinicians must rely on pharmacologic agents (eg, combination of calcium channels blockers to control blood pressure and optimize renal perfusion), accepting the high probability of deterioration in renal function and shortened survival.
Reports from retrospective studies clearly document that surgical revascularization can improve renal function in patients with ischemic nephropathy. In 1993, Rimmer and Gennari reported postoperative improvement (ie, 20% decrease in serum creatinine concentration) in more than half the patients in 9 studies.
Bypass procedures include aortorenal, hepatorenal, splenorenal, and ileorenal conduits constructed with autologous saphenous veins, autologous arteries, or prosthetic material. For atherosclerotic disease, surgeons can also perform atherectomy to improve renal blood flow. In persons with nonatheromatous renal artery disease, surgeons can reconstruct the renal arteries ex vivo and then can reimplant the revascularized kidney.
Reilly and coworkers reported an operative mortality rate of only 6% and immediate improvement in the serum creatinine level of 32% of surgical bypass procedures in 35 patients with solitary kidneys.17 In the last few years, researchers report that the results are more consistent. The largest series suggests that the GFR improved postoperatively in 49-80% of patients with underlying renal failure.
Angioplasty
Angioplasty is effective for treating renovascular hypertension associated with atheromatous lesions.Medication
The general approach to therapy of ischemic nephropathy involves control of hypertension, preferably with ACE inhibitors or angiotensin II antagonists. Unfortunately, these 2 classes of drugs may lead to increased serum creatine levels and hyperkalemia, limiting their utility. In this case, calcium channel blockers are likely the most useful and best-tolerated agents. Initiate strict control of serum cholesterol, which usually requires the use of HMG-CoA reductase inhibitors, as with all conditions associated with ATH. A study by Bianchi et al (2003) suggests that statins, in addition to ACE inhibitors and angiotensin receptor blockers (ARBs), may reduce proteinuria and slow the progression of kidney disease.• Overview
• Renal artery stenosis (RAS) is the narrowing of the lining of the main artery that supplies the kidney. Depending on the degree of narrowing, patients can develop hypertension called renal vascular hypertension (RVH). This form of hypertension is the most common cause of secondary hypertension.Renal Artery Stenosis, Renal Vascular Hypertension
RVH occurs when RAS produces a critical narrowing of the artery that supplies one of the kidneys. Critical RAS is defined as at least 70% narrowing of the renal artery, based on angiographic (blood vessel x-ray) evaluation.
Reduced blood flow through the renal artery causes the kidney to release increased amounts of the hormone renin. Renin, a powerful blood pressure regulator, initiates a series of chemical events that result in hypertension
Renal vascular hypertension can be very severe and difficult to control.
The kidney with RAS suffers from the decreased blood flow and often shrinks in size (atrophies). This process is called ischemic nephropathy. The other kidney is at risk for developing damage from the hypertension. Often developing hypertensive nephrosclerosis. The persistent elevated blood pressures in this non-stenotic kidney can cause progressive scarring (sclerosis) leading to progressive loss of filtering function in this kidney as well. Both unilateral RAS and bilateral RAS can ultimately lead to chronic renal failure.Atherosclerotic Renal Artery Stenosis (AS-RAS) and Fibromuscular Dysplasia (FMD) AS-RAS is due to the build-up of cholesterol on the inner lining of the renal artery. It is exceedingly more common than the unusual case of FMD-RAS.
FMD-RAS FMD-RAS occurs almost exclusively in women aged 30 to 40 and rarely affects African Americans or Asians. FMD-RAS is due to an abnormality in the muscular lining of the renal artery.
FMD-RAS is often not as well detected on MRA as it is on other non-invasive studies such as, renal scan with ACE-inhibitor challenge, or ultrasound with Doppler interrogation. FMD responds well to angioplasty and stenting. After plasty long-term patency of the lesion is typically seen.
Risk Factors Risk factors associated with the development of atherosclerotic RAS include the following:
Carotid artery disease
Coronary artery disease
Diabetes mellitus
Hypertension (high blood pressure)
Obesity
Age
Peripheral vascular disease (vascular disease in the extremities, e.g., the legs)
Smoking
There is often a familial history of FMD RAS.
Signs and Symptoms
Conditions that may indicate atherosclerotic RAS include :• Asymmetrical (differently sized and shaped) kidneys seen on ultrasound
• History of calf pain when walking—indicates impaired circulation to the legs
• Intolerance of specific antihypertensive medications—angiotensin-I (ACE-I) inhibitors or angiotensin receptor blockers (ARBs) with a sudden worsening of renal function
• More than three antihypertensive medications needed for blood pressure control
• New onset of hypertension in a patient over 55
• Presence of a bruit in the abdomen ,neck, or other area
• Sudden worsening of high blood pressure in a patient whose blood pressure had been well controlled, especially if the patient is over 60
Treatment
Diuretics, ACE inhibitors, beta blockers, calcium channel blockers, and angiotensin receptor blockers (ARBs) may be effective. A selective aldosterone inhibitor (e.g., eplerenone [Inspra®]) may be used to treat mild RAS.
These medications are discontinued if they cause a decrease in renal function. In some cases, patients with RAS are resistant to medication for control of blood pressure.
Angioplasty and stenting may be used to improve blood flow. The goal is to improve the circulation of blood flow to the kidney and prevent the release of excess renin, which can help to decrease blood pressure. This helps to prevent atrophy of the kidney. In general, patients with AS-RAS should have stenting done because plasty by itself has a very high incidence of re-stenosis.
Surgery to bypass the narrowing may be performed. If the kidney with RAS has atrophied, a nephrectomy, may be advised.
Prognosis Patients with fibromuscular dysplasia (FMD) RAS often have good, long-term results with angioplasty, but those with atherosclerotic RAS frequently experience a recurrence. Even after partial or complete repair of the narrowed blood vessel, most patients still have hypertension, but require less medication to control it.
BP-Lowering Drugs and Prevention of Cardiovascular Disease
Compared with placebo or no treatment, β-blockers resulted in 31% fewer CHD events in patients with recent myocardial infarctions (i.e., during the previous 2 years), 13% fewer CHD events in patients with CHD but without recent MIs, and 15% fewer CHD events in patients without histories of CHD. In the absence of recent MI, other BP-lowering drugs were as effective as β-blockers in preventing CHD events among patients with histories of CHD.Compared with placebo or no treatment, BP-lowering drugs led to significantly fewer CHD events and strokes (by 22% and 41%, respectively, when standardized to BP reductions of 10 mm Hg systolic or 5 mm Hg diastolic).Journal Watch General Medicine June 25, 2009
The five classes of drugs (thiazides, β-blockers, angiotensin-converting–enzyme (ACE) inhibitors, angiotensin-receptor blockers, and calcium-channel blockers) all similarly lowered rates of CHD events. Calcium-channel blockers were more effective in preventing stroke than were the others, although all drugs were more effective than no treatment.
Relative reductions in CHD events and stroke were similar among people with no histories of vascular disease and among those with prior CHD or stroke.With the exception of non-cardioselective β-blockers, each class of BP-lowering drugs significantly lessened risk for heart failure.
Compared with placebo or no treatment, BP-lowering drugs were associated with significantly lower all-cause mortality (by 13%).
No changes in cancer incidence or nonvascular-related mortality were noted.
In the last few years, questions have been raised about the use of beta-blockers as first-line therapy for hypertension. A number of large studies and meta-analyses have suggested that patients with uncomplicated hypertension may be at greater risk of stroke with no benefit for the endpoints of all-cause mortality and cardiovascular morbidity and mortality.The analysis includes a look at the risk/benefit ratio. Compared with other antihypertensive agents, the number needed to harm (NNH) for beta-blockers is 2,500 patients, (i.e., treatment of 2,500 patients with beta-blockers for 1 year results in one excess stroke).
New Review of the Evidence
Beta-blockers reduce blood pressure compared with placebo. However, compared with other antihypertensive agents, the blood pressure-lowering efficacy of beta-blockers is suboptimal.Beta-blockers are not only less efficacious at reducing peripheral blood pressure but also have a lesser effect on perhaps the more important central aortic pressure when compared with RAAS blockers, diuretics, and calcium antagonists
Beta-blockers often are not well tolerated, and the compliance rate with these medications is dismal.
Beta-blocker use, however, has been associated with small but systematic weight gain (as much as 1.2 kg)
Exercise endurance in a healthy person depends, in part, on a properly functioning sympathetic nervous system. Beta-blockers, by antagonizing this effect, may hamper exercise capacity.
It turns out that carvedilol, since it's a non-selective beta-1, beta-2, and alpha-1 blocker, does not have an adverse effect on insulin resistance. That may be one reason why it looks like carvedilol will become the beta-blocker of choice.
studies have consistently shown a substantial reduction in the rate of mortality (~30%) and morbidity with the use of beta-blocker therapy for treating patients with heart failure. This approach also improves symptoms and patient well-being.Depending on the beta-blocker study, treatment of 15 to 43 patients with heart failure prevents one death; thus, beta-blockers are very effective in patients with heart failure. The mortality benefit has been demonstrated in overall cohorts, in the elderly or the young, in men or women, in patients with or without diabetes, in patients with ejection fraction < 25% or ≥ 25%, and in patients on or not on background RAAS-blocker therapy. The current American College of Cardiology/American Heart Association (ACC/AHA) guidelines recommend beta-blockers in patients with systolic heart failure.
In the new 2007 review in JACC, the authors conclude that for patients with uncomplicated hypertension, there is a paucity of data or an absence of evidence to support the use of beta-blockers as monotherapy or as first-line agents. Given the risk of stroke, lack of cardiovascular morbidity and mortality benefit, numerous adverse effects, and lack of regression of target end-organ effects of hypertension (e.g., left ventricular hypertrophy and endothelial dysfunction), they said, “The risk benefit ratio for beta-blockers is not acceptable for this indication.
Guideline committees should revise recommendations for beta-blockers as first-line therapy for uncomplicated hypertension.” The ACC/AHA committee recommends beta-blockers as the first-line therapy for chronic stable angina based on two pieces of evidence: first, the evidence of improved mortality with beta-blockers in post-MI patients, and, second, by extrapolation from the supposed effects of these agents in hypertension to patients with stable angina.
As for directly affecting current guidelines, the first official change came recently from the British National Institute for Health and Clinical Excellence (NICE) and the British Hypertension Society (BHS). The organizations released an update of their hypertension treatment guidelines, which stated, “Beta-blockers are no longer preferred as a routine initial therapy for hypertension.The guidelines suggest that beta-blockers still be considered for some patients with uncontrolled or complicated hypertension.
Copyright © 2008 American College of Cardiology.
Two Surprising Theories About Hypertension
Mouse models for hypertension suggest new pathways.In two new studies, researchers put forward provocative new theories about hypertension.
A European team studied salt-sensitive hypertension in mice. Excess salt intake led not only to expansion of intravascular volume but also to proliferation of lymphatic vessels under the skin that stored excess fluid. This phenomenon lessened intravascular volume and, thus, reversed the rise in blood pressure that resulted from initial salt loading. The proliferation of lymphatic vessels was produced by the angiogenesis molecule VEGF-C, which had been stimulated by another molecule (TonEBP) that is produced in response to hypertonic conditions. The investigators postulated that defects in this system cause salt-sensitive hypertension.
A team from Boston reported that infecting mouse endothelial cells with mouse cytomegalovirus (MCMV) caused hypertension, excess release of renin and angiotensin II, excess production of proinflammatory cytokines, and development of intimal hyperplasia and atherosclerosis in a mouse model. The investigators also found that, as in the mouse model, human CMV could infect human endothelial cells in culture and cause them to secrete renin and proinflammatory cytokines.
Journal Watch General Medicine June 4, 2009
What is Vastarel MR?
Vastarel MR is the new twice-daily formulation of trimetazidine, the first 3-KAT inhibitor.Trimetazidine is a metabolic anti-ischemic agent that was discovered and developped by Servier Research. reduces the metabolic damage caused during ischemia, by acting on a critical step in cardiac metabolism: fatty acid β-oxidation. This is made possible by selective inhibition of an enzyme of fatty acid β-oxidation: the long-chain 3-ketoacyl CoA thioloase (3-KAT).This inhibition results in:
1- Reduction in fatty acid oxidation 2- Stimulation of glucose oxidationThus, the coupling of glycolysis with glucose oxidation is improved, and ATP production is further increased, while the deleterious consequences of acidosis and of Ca2+ overload are limited
Under ischemic conditions, Vastarel MR optimizes cardiac metabolism through a metabolic switch from fatty acid oxidation to glucose oxidation.
Trimetazidine is a drug for angina pectoris, sometimes referred to by the brand name Vastarel MR. Each tablet contains 35 mg of trimetazidine. Trimetazidine is an anti-ischemic (anti-anginal) metabolic agent, which improves myocardial glucose utilization through inhibition of fatty acid metabolism.
By preserving the energy metabolism in cells exposed to hypoxia or ischemia, trimetazidine prevents a decrease in intracellular adenosine triphosphate levels, thereby ensuring the proper functioning of ionic pumps and transmembranous sodium-potassium flow whilst maintaining cellular homeostasis. It also inhibits oxidation of fatty acid in blood vessels.
Controlled studies in angina patients have shown that trimetazidine increases coronary flow reserve, thereby delaying the onset of ischemia associated with exercise, limits rapid swings in blood pressure without any significant variations in heart rate, significantly decreases the frequency of angina attacks, and leads to a significant decrease in the use of nitrates.
It improves left ventricular function in diabetic patients with coronary heart disease. Recently, it has been shown to be effective in patients with heart failure of different etiologies .
Trimetazidine is described as the first cytoprotective anti-ischemic agent developed and marketed by Les Laboratories Servier (France). It acts by directly counteracting all the major metabolic disorders occurring within the ischemic cell. The actions of trimetazidine include limitation of intracellular acidosis, correction of disturbances of transmembrane ion exchanges, and prevention of excessive production of free radicals.
Trimetazidine is usually prescribed as a long-term treatment of angina pectoris, and in some countries (including France) for tinnitus and dizziness. It is taken twice a day.
Trimetazidine has high safety and tolerability profile. It has no known drug interactions. There is scarce information about trimetazidine's effect on mortality, cardiovascular events or quality of life. Long term trials comparing trimetazidine against standard anti-anginal agents, using clinically important outcomes would be justifiable.
Aborted Myocardial Infarction: Is it Real in the Troponin Era?
Cardiac troponins are the markers of choice for the diagnosis of acute myocardial infarction. The objective of this study was to compare the frequency of "aborted myocardial infarction" (no detectable myocardial injury) determined by measurement of troponin versus that determined by creatine kinase (CK) and creatine kinase-muscle brain (CK-MB) measurement criteria among patients with ST-elevation myocardial infarction (STEMI) who received reperfusion therapy.American Heart Journal. 2009
Reperfusion therapy has revolutionized the treatment of patients with ST-elevation myocardial infarction (STEMI).[1] Integral to this approach is the principle that mortality and infarct size correlate with total ischemic time from coronary occlusion to reperfusion.It has been hypothesized that if reperfusion therapy is administered very early after symptom onset, there might be no detectable cardiac biomarker release and thus no cardiac injury that could be diagnosed. This scenario has been referred to as aborted myocardial infarction and, as expected, its observed frequency correlates well, although not perfectly with shorter total ischemic times.
The diagnosis of STEMI was confirmed in 765 (99.7%) patients. Using the 99th percentile cutoff value, troponin T elevations occurred in 765 (100%) of 765 patients when serial samples were available. Creatine kinase-MB levels of twice or more the upper limit of normal occurred in 681 (90.1%) of 749 patients with serial samples for CK-MB, and CK equal or greater than twice the gender-specific upper limits of normal occurred in 521 (78.8%) of 661 patients with serial samples for CK available.Conclusion: The frequency of aborted myocardial infarction is 0% when using troponin at the 99th percentile cutoff as recommended by contemporary guidelines from the European Society of Cardiology (Nice, France) and American College of Cardiology (Washington, DC).
Aborted myocardial infarction has been previously defined based on the absence of increases in total creatine kinase (CK) or the muscle brain isoenzyme of creatine kinase (CK-MB) to greater than twice the upper limit of normal.[5-7] However, the use of CK biomarkers to define the diagnosis of acute myocardial infarction has been superseded by cardiac troponin.[8,9
Regardless of the type of reperfusion treatment used, this study has demonstrated that no MI was aborted when using troponin at the 99th percentile cutoff to diagnose acute MI as recommended by current guidelines. In contrast, aborted myocardial infarctions using CK-MB manifested a prevalence of 9.1% and using CK a prevalence of 21.7%. These data suggest that the concept of an aborted myocardial infarction itself was a function of less sensitive biomarker assays and not the true absence of cardiac injury. However, we did observe that those who met criteria for "aborted MI" had substantially lower levels of cTn than those who did not, suggesting that the amount of damage was less. For that reason perhaps, mortality was modest in those patients.
Absence of Coronary Calcium Predicts Excellent 10-Year Survival: Study
In asymptomatic individuals at intermediate risk for atherosclerosis, the absence of coronary artery calcium (CAC) is a valuable "negative risk factor" for major cardiovascular events, according to a report in the June 2009 issue of the Journal of the American College of Cardiology: Cardiovascular Imaging.19,898 patients (45%) had no CAC, 5,388 (12%) had low CAC scores (CAC 1 to 10), and 18,766 (43%) had CAC scores greater than 10. There were 104 deaths, 58 deaths and 739 deaths, respectively, in these three groups.
With a mean follow-up of 5.6 years (range 1 to 13 years), a CAC score of 0 was associated with "excellent survival," with all-cause mortality rates of 0.87 per 1,000 person-years (less than 1% 10-year risk or less than 0.1% per year).
After adjusting for risk factors, individuals with low CAC scores had a nearly twofold increased risk of death (1.92 per 1,000 person-years), compared with those with no CAC, "suggesting that low CAC represents a distinct risk group," the authors say. Nonetheless, the researchers report that "mortality rates in individuals with low CAC scores remained low" (less than 5% 10-year risk or less than 0.5% per year).
In contrast to the no CAC and low CAC groups, individuals with high CAC scores had annualized all-cause mortality rates of 7.48 per 1,000 person-years.
After Two Years, Vessels Treated With the ABSORB Stent Show Minimal Traces of the Stent and Function Normally
March 13, 2009 (London, United Kingdom) — Bioabsorbable stents have been billed as a "now-you see-it-now-you-don't" solution to problems like stent thrombosis and delayed vessel healing: two-year imaging results from the ABSORB study of Abbott's everolimus-eluting bioabsorbable stent, using some of the most advanced intravascular-imaging techniques, indicate that at least one-third of the stent has been absorbed by the vessel wall. Moreover, write Dr Patrick Serruys (Thoraxcenter, Rotterdam, the Netherlands) and colleagues in the March 14, 2009 issue of the Lancet, all signs point to normal healing of the vessel wall and restored vasomotion; only one major adverse cardiac event (MACE) occurred over the follow-up period.
ACC 2009: MRI Study Shows Plaque Lipid Core Depletion With Intensive Lipid-Lowering Therapy
Intensive statin therapy in patients with coronary or carotid artery disease significantly depleted the lipid content of atherosclerotic plaques, a new study has shown. Plaque depletion, as measured by MRI, occurred in the first two years of treatment, slowing down in year three. the observed reduction in cardiovascular events with lipid-lowering therapy is hypothesized to occur as a result of depletion of cholesterol esters from a vulnerable subgroup of lipid-, foam-, and macrophage-rich lesions.
In these high-risk lesions, based on pathology studies, as well as animal models, improved mechanical strength (such as a strengthened fibrous cap), reduced inflammatory activity, and stabilized endothelial function are thought to be some of the positive changes that result from the depletion of these cholesterol esters. "If you deplete the lipid content and increase the fibrous tissue, it makes sense that the plaque is going to be more stable,"Recent advances in MRI have made it possible to identify lipid plaque composition and to measure changes in the lipid core that result from lipid-modifying therapies
Physicians should remember that standard of care is not determined by being right 100% of the time, but rather by providing care that would be considered "reasonable." The problem is that "reasonable" is very subjective, and until we as a society can agree on what is "reasonable," we'll continue to debate this question and similar ones for many years.
Which Revascularization Strategy Is Best for Severe Coronary Artery Lesions?
Results of the SYNTAX trial failed to show that PCI is noninferior to CABG in patients with 3-vessel or left main disease.1800 patients with three-vessel or left main coronary artery disease were randomly assigned to coronary artery bypass grafting or percutaneous coronary intervention with DES. Before randomization, an interventional cardiologist and a cardiac surgeon evaluated all patients’ angiograms and agreed that equivalent anatomic revascularization was feasible with either technique. The primary endpoint, a composite of major adverse cardiac and cerebrovascular events (MACCE), included repeat revascularization.
After 12 months, the MACCE rate was significantly lower in the CABG group (12%) than in the PCI group (18%). The CABG group had a significantly higher stroke rate than the PCI group (2.2% vs. 0.6%), whereas the PCI group had a significantly higher repeat revascularization rate than the CABG group (13.5% vs. 5.9%). Mortality was similar in the two groups. PCI was associated with a higher MACCE rate in patients with the highest scores of disease severity than in lower-scoring patients; the same association was not seen with CABG. This finding thus increased the between-group difference in MACCE among the most severely ill patients (PCI, 23%; CABG, 11%). In an observational analysis of the left main subgroup, the overall MACCE rate was similar after CABG and after PCI, although somewhat greater benefit with CABG was observed in left main patients who also had two- or three-vessel disease.
Triple versus dual antiplatelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention.
A total of 4203 ST-segment elevation myocardial infarction patients who underwent primary percutaneous coronary intervention with drug-eluting stents were analyzed retrospectively in the Korean Acute Myocardial Infarction Registry (KAMIR). They received either dual (aspirin plus clopidogrel; dual group; n=2569) or triple ((aspirin plus clopidogrel plus cilostazol(phosphodiesterase III inhibitor) ; triple group; n=1634)) antiplatelet therapy. The triple group received additional cilostazol at least for 1 month. Various major adverse cardiac events at 8 months were compared between these 2 groups. Compared with the dual group, the triple group had a similar incidence of major bleeding events but a significantly lower incidence of in-hospital mortality.
• Early or Delayed Intervention for Acute Coronary Syndromes Without ST-Segment-Elevation?
• In a randomized trial, only high-risk patients clearly benefited from invasive treatment within 24 hours.
Although routine invasive treatment of acute coronary syndromes without ST-segment-elevation is associated with improved outcomes, the optimal timing of such interventions is unclear. To compare outcomes of early versus delayed coronary angiography and revascularization, investigators from the Timing of Intervention in Acute Coronary Syndromes (TIMACS) study assigned 3031 adults with non–ST-segment-elevation ACS (mean age, 65; women, 35%) to receive such treatment either within 24 hours of symptom onset or more than 36 hours afterward. All patients also had at least two of the following risk factors: age ≥60, elevated cardiac biomarkers, or electrocardiographic signs of ischemia.
• At 6 months, the primary outcome — a composite of death, MI, and stroke — occurred in 9.6% of patients in the early-intervention group and in 11.3% of those in the delayed-intervention group, a nonsignificant difference. However, 1.0% of patients in the early-intervention group had refractory ischemia, compared with 3.1% in the delayed-intervention group: a significant 70% relative reduction. In prespecified analyses, early intervention significantly improved the primary outcome in patients in the highest-risk tertile as stratified by GRACE score, compared with those in the lower-risk tertiles.
• Comment: These findings suggest that early intervention in patients with ACS without ST-segment-elevation is not superior to delayed intervention for the prevention of death, MI, or stroke. However, an early-intervention strategy significantly reduced the rate of refractory ischemia, especially in high-risk patients. Overall, these results provide reassurance that most ACS patients can safely undergo interventional treatment at any time.
• Journal Watch Cardiology May 20, 2009
Aspirin for the Prevention of Cardiovascular Disease
U.S. Preventive Services Task Force (USPSTF)Summary of Recommendations
The USPSTF recommends the use of aspirin for men age 45 to 79 years when the potential benefit due to a reduction in myocardial infarctions outweighs the potential harm due to an increase in gastrointestinal hemorrhage Grade: A recommendation.The USPSTF recommends the use of aspirin for women age 55 to 79 years when the potential benefit of a reduction in ischemic strokes outweighs the potential harm of an increase in gastrointestinal hemorrhage. Grade: A recommendation.
The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of aspirin for cardiovascular disease prevention in men and women 80 years or older.Grade: I statement.
The USPSTF recommends against the use of aspirin for stroke prevention in women younger than 55 years and for myocardial infarction prevention in men younger than 45 years. Grade: D recommendation.
Assessment of Risk for Cardiovascular Disease Men
The net benefit of aspirin depends on the initial risk for coronary heart disease events and gastrointestinal bleeding. Thus, decisions about aspirin therapy should consider the overall risks for coronary heart disease and gastrointestinal bleeding.Risk assessment for coronary disease should include ascertainment of risk factors: age, diabetes, total cholesterol levels, high-density lipoprotein cholesterol levels, blood pressure, and smoking. Available tools provide estimations of coronary heart disease risk.
Women
The net benefit of aspirin depends on the initial risks for stroke and gastrointestinal bleeding. Thus, decisions about aspirin therapy should consider the overall risk for stroke and gastrointestinal bleeding.
Risk factors for stroke include age, high blood pressure, diabetes, smoking, a history of cardiovascular disease, atrial fibrillation, and left ventricular hypertrophy. Tools for estimation of stroke risk are available.
Assessment of Risk for Gastrointestinal Bleeding
Evidence shows that the risk for gastrointestinal bleeding with and without aspirin use increases with age.2,4 For the purposes of making this recommendation, the USPSTF considered age and sex to be the most important risk factors for gastrointestinal bleeding. Other risk factors for bleeding include upper gastrointestinal tract pain, gastrointestinal ulcers, and NSAID use.NSAID therapy combined with aspirin approximately quadruples the risk for serious gastrointestinal bleeding compared with the risk with aspirin alone.
The rate of serious bleeding in aspirin users is approximately 2 to 3 times greater in patients with a history of a gastrointestinal ulcer. Men have twice the risk for serious gastrointestinal bleeding than women. These risk factors increase the risk for bleeding substantially and should be considered in the overall decision about the balance of benefits and harms of aspirin therapy. Enteric-coated or buffered preparations do not clearly reduce the adverse gastrointestinal effects of aspirin. Uncontrolled hypertension and concomitant use of anticoagulants also increase the risk for serious bleeding.
Right Ventricular Infarction
Patients with right ventricular infarctions associated with inferior infarctions have much higher rates of significant hypotension, bradycardia requiring pacing support, and in-hospital mortality than isolated inferior infarctions.1 The right ventricle is a thin-walled chamber that functions at low oxygen demands and pressure. It is perfused throughout the cardiac cycle in both systole and diastole, and its ability to extract oxygen is increased during hemodynamic stress. All of these factors make the right ventricle less susceptible to infarction than the left ventricle.Isolated infarction of the right ventricle is extremely rare; right ventricular infarction usually is noted in association with inferior wall myocardial infarction. The incidence of right ventricular infarction in such cases ranges from 10-50%, depending on the series.
Although right ventricular infarction occurs in more than 30% of patients with inferior posterior left ventricular myocardial infarction, hemodynamically significant right ventricular infarction occurs in less than 10% of these patients.A right ventricular infarct should be considered in all patients who present with an acute inferior wall myocardial infarction, especially in the setting of a low cardiac output. Patients may describe symptoms consistent with hypotension. A subtle clue to the presence of hemodynamically significant right ventricular infarction is a marked sensitivity to preload-reducing agents such as nitrates, morphine, or diuretics.Other presentations include high-grade atrioventricular block, tricuspid regurgitation, cardiogenic shock, right ventricular free wall rupture, and cardiac tamponade.
The classic clinical triad of right ventricular infarction includes distended neck veins, clear lung fields, and hypotension.
Infrequent clinical manifestations include right ventricular third and fourth heart sounds, which are typically audible at the left lower sternal border and increase with inspiration.
On hemodynamic monitoring, disproportionate elevation of right-sided filling pressures compared with left-sided hemodynamics represents the hallmark of right ventricular infarction.
The early-repolarization pattern in the inferior leads was a stronger predictor of death from cardiac causes or from arrhythmia than J-point elevation in the lateral leads. Similarly, previous studies have reported that the J wave is present in inferior leads among many patients with idiopathic ventricular fibrillation. In addition to the location of the early-repolarization pattern, the amplitude of the J-point elevation had some prognostic value: there was a higher risk of death from cardiac causes among subjects with a markedly elevated J point (>0.2 mV) than among those with a more moderate elevation (>0.1 mV).). A similar phenomenon was previously observed in survivors of primary ventricular fibrillation.4
Long-Term Outcome Associated with Early Repolarization on Electrocardiography
Coronary Revascularization in Context(CABG), introduced in 1968, was the only method of coronary revascularization until 1977, when percutaneous balloon angioplasty was first performed. The complications of balloon angioplasty (acute vessel closure in 3 to 5% of patients and restenosis in almost half) prevented its use in patients with severe coronary artery disease. In the 1990s, the introduction of bare-metal stents led to reduced rates of these complications. The improved short-term and long-term procedural success with ntion (PCI) allowed for its safe and effective performance in patients with severe coronary artery disease.
NEJM February 18, 2009
By the year 2000, more PCI procedures than CABG procedures were being performed in the United States. In early 2000, drug-eluting stents were approved for use in Europe and North America, after studies showed a markedly reduced incidence of restenosis with drug-eluting stents as compared with bare-metal stents. Subsequently, the use of drug-eluting stents was rapidly adopted; in 2006, a total of 253,000 CABG procedures and 1,131,000 PCI procedures were performed in the United States,1 with drug-eluting stents used in 90% of the PCIs.2
Do CABG and PCI result in similar outcomes? A recent review3 of 23 randomized, controlled comparisons of CABG and PCI (by means of balloon angioplasty or bare-metal stenting) in approximately 10,000 patients showed that CABG was superior to PCI in relieving angina and averting repeat revascularization procedures. The rates of survival at 1, 5, and 10 years were similar for the two procedures, even though CABG carried a higher risk of stroke (1.2%, vs. 0.6% with PCI). However, most of the 23 studies did not involve patients with severe coronary artery disease (i.e., left main or three-vessel coronary artery disease) and did not use the latest revascularization techniques.
Newer Options for Treatment of Chronic Angina
Over the past decade, for example, several new anti-anginal agents have been evaluated in large clinical studies and offer novel approaches to altering the ischemia supply-and-demand mismatch, as well as improving anginal symptoms.Of these new agents, nicorandil, ivabradine, and ranolazine have been most extensively studied. At present, ranolazine is the only one to be approved in the United States to treat angina, whereas nicorandil and ivabradine are available in other areas of the world. Each agent modifies the fundamental oxygen supply-and-demand equation via novel mechanisms and therefore may offer complementary anti-ischemic activity in addition to traditional anti-anginal agents.
2009 Medscape
Nicorandil
Nicorandil has 2 proposed mechanisms of action that improve ischemia. The first is via activating ATP-dependent potassium channels, which directly dilate peripheral and coronary arteries. In addition, like nitrates, nicorandil promotes smooth muscle cell relaxation and vasodilation via increased cGMP activity through a nitrate moiety.The drug may have cardioprotective properties. In the Impact Of Nicorandil in Angina (IONA) trial[18] of 5126 patients with stable angina, for example, treatment with nicorandil resulted in a significant 17% reduction in the primary endpoint of coronary heart disease death, MI, or unplanned hospitalization for chest pain compared with placebo (13.1% vs 15.5%, hazard ratio [HR] 0.83, 95% confidence interval [CI] 0.72-0.97; P = .014), although there was no difference in overall mortality (Figure 3). Similar to nitrates, chronic therapy may promote tachyphalaxis, although tolerance does not cross-react with nitrates so they can be used in combination. Although not approved in the United States, nicorandil is currently approved in several countries in Europe and Asia.
Ivabradine
Ivabradine, an inhibitor of the If current in the sinoatrial cells, reduces both resting and exercise heart rate in patients in sinus rhythm but has no significant hemodynamic effects.In studies of patients with chronic angina, ivabradine has been shown to increase the time to 1-mm ST-segment depression and time to limiting angina during exercise stress testing.Such improvements in exercise tolerance have been associated with reductions in anginal symptoms and nitroglycerin use that are comparable to the effects of atenolol.In the recently published ASSOCIATE trial, the addition to ivabradine to a regimen of atenolol significantly improved exercise parameters after 4 months of therapy.Ivabradine is approved in Europe for the treatment of chronic stable angina in patients in normal sinus rhythm who have a contraindication or intolerance to beta-blockers. The recommended starting dose is 5 mg twice daily, which can be increased to 7.5 mg twice daily. The dose should be reduced or therapy stopped in patients who develop persistent bradycardia less than 50 bpm or signs and symptoms of hypotension. Ivabradine should not be used in patients with second-degree AV block or in patients with a resting heart rate less than 50 bpm.
Ranolazine
Ranolazine is a piperazine derivative that has been preferentially shown in experimental models of induced ischemia and heart failure to inhibit the late phase of the sodium current (late INa). In disease states, such as ischemia and heart failure, late INa is augmented, causing increased concentrations of intracellular sodium and calcium overload that leads to deleterious effects on both cardiac electrical and mechanical function. Inhibition of late INa reduces intracellular sodium and calcium overload, thereby improving diastolic function.Ranolazine is approved in Europe as add-on therapy for patients with chronic angina with inadequate control or in patients who cannot tolerate first-line agents, such as beta-blockers or calcium antagonists. In the United States, ranolazine is indicated for the treatment of chronic angina and may be used alone or in combination with other traditional therapies.
Ranolazine should be started at 500 mg twice daily and can be increased to 1000 mg twice daily if needed. Ranolazine prolongs the QTc interval from 2 msec to 6 msec, although this does not appear to increase the risk for arrhythmia. In patients on moderate inhibitors of CYP3A4, the dose should be limited to 500 mg twice daily. The most commonly reported side effects are dizziness, headache, constipation, and nausea.
In addition to its anti-anginal effects, in the setting of angina, ranolazine has also been shown to lower levels of hemoglobin A1c (HbA1c) in patients with diabetes and is associated with antiarrhythmic properties in patients with coronary artery disease. The exact mechanisms associated with these effects require further investigation.
centrally active ACE inhibitors were associated with 65% less decline in cognitive-function scores per year of exposure.
The data also reveal that non–centrally active ACE inhibitors were associated with a greater risk for incident dementia and greater odds of disability in IADLs compared with other antihypertensive medications.
Centrally active ACE inhibitors included captopril ,fosinopril ,lisinopril, perindopril, ramipril, and trandolapril .
Non–centrally active ACE inhibitors included benazepril ,enalapril ,moexipril ,and quinapril.
Centrally Active ACE Inhibitors May Help Prevent Dementia
The researchers suspect that this difference is due primarily not to the antihypertensive effects of centrally acting ACE inhibitors but to their effect on the brain's intrinsic renin-angiotensin system (RAS), which is involved in memory and cognition.
Stimulation of the renin-angiotensin system also mediates activation of inflammatory cytokines that have been implicated in degenerative dementias, explained Dr. Sink.
The researchers also suspect that the slight increase dementia risk associated with the non–centrally acting ACE inhibitors in this comparison was probably a sign that they are "simply less helpful in the prevention of dementia and IADL disability than other antihypertension drug classes combined."
Arch Intern Med. 2009
Sildenafil is contraindicated in combination with nitrates due to the risk for a pharmacodynamic drug interaction that can result in severe hypotension and death.
administration of any form of nitrates in a patient who has taken sildenafil poses a real and serious risk for serious hypotension. Coadministration is contraindicated and should be avoided. The American College of Cardiology (ACC) and American Heart Association (AHA) joint guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction recommend that NTG or nitrates not be given to these patients within 24 hours of sildenafil.[5] Nitrates should also be avoided after use of other PDE5 inhibitors.[5,6
An ACC/AHA expert consensus document suggests that nitrates may be considered 24 hours after sildenafil dosing. Further delay may be necessary in the patient who might have a prolonged elimination half-life of sildenafil due to renal or hepatic dysfunction or coadministration of a cytochrome P450 3A4 inhibitor. If NTG is initiated in such circumstances, caution and careful monitoring are necessary
Whole Grains and Fiber
Any food made from wheat, rice, oats, corn, or another cereal is a grain product. Bread, pasta, oatmeal and grits are all grain products. There are two main types of grain products: whole grains and refined grains.
Whole grains contain the entire grain – the bran, germ and endosperm. Examples include whole-wheat flour, oatmeal, whole cornmeal, brown rice and bulgur.
Refined grains have been milled (ground into flour or meal) which results in the bran and germ being removed. This process removes much of the B-vitamins, iron and dietary fiber. Some examples of refined grains are wheat flour, enriched bread and white rice.
whole grains health benefits:
good sources of dietary fiber, helps reduce blood cholesterol levels and may lower risk of heart disease.
provide a feeling of fullness with fewer calories and so may help with weight management.
Grains are also important sources of many nutrients:
B vitamins (thiamin, riboflavin, niacin and folate).
Iron is used to carry oxygen in the blood.
Magnesium is a mineral used in building bones and releasing energy from muscles.
Selenium is important for a healthy immune system.
• Dietary Fiber
• Dietary fiber is the term for several materials that make up the parts of plants your body can't digest.• Fiber is classified as soluble or insoluble.
• When eaten regularly as part of a diet low in saturated fat, trans fat and cholesterol, soluble fiber has been associated with increased diet quality and decreased risk of cardiovascular disease. Soluble or viscous fibers modestly reduce LDL (“bad”) cholesterol beyond levels achieved by a diet low in saturated and trans fats and cholesterol alone. Oats have the highest proportion of soluble fiber of any grain. Foods high in soluble fiber include oat bran, oatmeal, beans, peas, rice bran, barley, citrus fruits, strawberries and apple pulp.
Insoluble fiber has been associated with decreased cardiovascular risk and slower progression of cardiovascular disease in high-risk individuals. Dietary fiber can make you feel full, so you may eat fewer calories.
Foods high in insoluble fiber include whole-wheat breads, wheat cereals, wheat bran, rye, rice, barley, most other grains, cabbage, beets, carrots, Brussels sprouts, turnips, cauliflower and apple skin.
Acute Pulmonary Embolism
The clinical presentation of acute pulmonary embolism ranges from shock or sustained hypotension to mild dyspnea. Pulmonary embolism may even be asymptomatic and diagnosed by imaging procedures performed for other purposes. Depending on the clinical presentation, the case fatality rate for acute pulmonary embolism ranges from about 60% to less than 1%.July 15 , 2010, NEJM.
In patients with hemodynamic stability, the diagnosis of pulmonary embolism should follow a sequential diagnostic workup consisting of clinical probability assessment, D-dimer testing, and (if necessary) multidetector (CT) or ventilation–perfusion scanning . The use of the D-dimer assay is of limited value in patients with a high clinical probability of pulmonary embolism. The specificity of an increased D-dimer level is reduced in patients with cancer, pregnant women, and hospitalized and elderly patients.
In patients who are candidates for percutaneous embolectomy, conventional pulmonary angiography can be performed to confirm the diagnosis of pulmonary embolism immediately before the procedure, after the finding of right ventricular dysfunction.
In pregnant women with clinical findings suggestive of pulmonary embolism, the concern about radiation is overcome by the hazard of missing a potentially fatal diagnosis or exposing the mother and fetus to unnecessary anticoagulant treatment. Multidetector CT delivers a higher dose of radiation to the mother but a lower dose to the fetus than ventilation–perfusion lung scanning. magnetic resonance angiography was recently shown to have insufficient sensitivity and a high rate of technically inadequate images when used for the diagnosis of pulmonary embolism.
In cases in which multidetector CT is not available or in patients with renal failure or allergy to contrast dye, ventilation–perfusion scanning is an alternative. A normal ventilation–perfusion scan essentially rules out pulmonary embolism, with a negative predictive value of 97%.A lung scan with findings that suggest a high probability of pulmonary embolism has a positive predictive value of 85 to 90%. However, ventilation–perfusion scanning is diagnostic in only 30 to 50% of patients with suspected pulmonary embolism.
If venous ultrasonography of the lower limbs is performed first, lung scanning or multidetector CT can be avoided in about 10% of patients with suspected pulmonary embolism. Hemodynamically stable patients with suspected pulmonary embolism and ultrasonographically confirmed deep-vein thrombosis can be given anticoagulant treatment without further testing. Venous ultrasonography should precede imaging tests in pregnant women with suspected pulmonary embolism and in patients with a contraindication to multidetector CT.
In hemodynamically unstable patients who are hypotensive or in shock, multidetector CT should be performed because of its 97% sensitivity for detecting emboli in the main pulmonary arteries. If multidetector CT is not available without delay, echocardiography should be performed to confirm the presence of right ventricular dysfunction. In most patients with hemodynamically unstable pulmonary embolism, transesophageal echocardiography may confirm the diagnosis by showing emboli in the main pulmonary arteries. In patients who are so critically ill that transport is unsafe or unfeasible, thrombolytic therapy should be considered if there are unequivocal signs of right ventricular overload on bedside echocardiography.
Risk Stratification
Shock and sustained hypotension identify patients at high risk for an adverse outcome. In the International Cooperative Pulmonary Embolism Registry, the death rate was nearly 58% among hemodynamically unstable patients and about 15% among hemodynamically stable patients. Immobilization because of a neurologic disease, an age of more than 75 years, cardiac or respiratory disease, and cancer are risk factors for death among patients with acute pulmonary embolism.Markers of myocardial dysfunction or injury may be useful for risk stratification of hemodynamically stable patients. Right ventricular dysfunction on echocardiography has been associated with increased mortality among patients with acute pulmonary embolism. Right ventricular hypokinesis and dilatation have been shown to be independent predictors of 30-day mortality among hemodynamically stable patients. Right ventricular dysfunction, as assessed by means of multidetector CT, has been suggested to be an independent predictor of 30-day mortality.
• Treatment of Acute Pulmonary Embolism.
• Low-molecular-weight heparin (administered either intravenously or subcutaneously) should be the treatment of choice in hemodynamically stable patients.• Thrombolysis should be administered to patients whose condition is unstable and should be considered for high-risk, hemodynamically stable patients.
Percutaneous mechanical thrombectomy should be restricted to high-risk patients with absolute contraindications to thrombolytic treatment and those in whom thrombolytic treatment has failed to improve hemodynamic status. Low-molecular-weight heparin is preferable to vitamin K antagonists in patients with cancer and in pregnant women. For patients receiving vitamin K antagonists, the international normalized ratio (INR) should be maintained within a therapeutic range (2.0 to 3.0) during long-term therapy ( 3 months); a low-intensity INR target of 1.5 to 1.9 is an option for extended (indefinite) anticoagulant therapy.
Extended treatment should be considered for patients with active cancer, unprovoked pulmonary embolism, or recurrent venous thromboembolism. Extended treatment requires a reassessment of the patient's risk–benefit ratio at periodic intervals. Indefinite treatment refers to anticoagulation that is continued without a scheduled stop date but that may be stopped because of an increase in the risk of bleeding or a change in the patient's preference.
In an open study involving hemodynamically stable patients, intravenous thrombolysis reduced the rate of clinical deterioration (mainly, the need for secondary thrombolysis) but not the rate of death, as compared with the use of unfractionated heparin. Intravenous thrombolytic treatment was associated with a more rapid resolution of right ventricular dysfunction; at 1 week, however, the degree of right ventricular dysfunction was similar in the two treatment groups. No clear advantage of catheter-directed thrombolysis, as compared with intravenous thrombolysis, has been shown. In a recent meta-analysis of case series, catheter-directed therapy had a clinical success rate of 86% and a rate of major procedural complications of 2.4%
Hemodynamically unstable patients are candidates for more aggressive treatment, such as pharmacologic or mechanical thrombolysis. This therapeutic option is justified by the high rate of death among such patients and by the faster resolution of thromboembolic obstruction with thrombolysis than with anticoagulant therapy. Mortality can be as high as 60% in untreated and can be reduced to less than 30% with prompt treatment. The most recent meta-analysis showed that intravenous thrombolysis was associated with a reduction in mortality among hemodynamically unstable patients with pulmonary embolism.42 Major bleeding was more common with intravenous thrombolysis than with anticoagulant therapy. Major contraindications to thrombolytic therapy include intracranial disease, uncontrolled hypertension, and recent major surgery or trauma (within the past 3 weeks).
Percutaneous mechanical thrombectomy (thrombus fragmentation and aspiration) and surgical embolectomy should be restricted to high-risk patients with an absolute contraindication to thrombolytic treatment and those in whom thrombolytic treatment has not improved hemodynamic status; percutaneous mechanical thrombectomy is an alternative to surgical embolectomy in cases in which immediate access to cardiopulmonary bypass is unavailable.
The use of vena cava filters should be reserved for patients with contraindications to anticoagulant treatment. To avoid thrombus extension and recurrence, such patients should receive a conventional course of anticoagulant therapy if and when the risk of bleeding is eliminated. Case series have shown that retrievable vena cava filters may be an option for patients with presumed time-limited contraindications to anticoagulant therapy or for patients requiring procedures that are associated with a risk of bleeding. However, the use of retrievable filters has not resulted in increased filter retrieval.
Long-Term Management
Patients with acute pulmonary embolism are at risk for recurrent thromboembolic events, mainly a second pulmonary embolism. The risk of recurrent pulmonary embolism is less than 1% per year while patients are receiving anticoagulant therapy, but the risk is 2 to 10% per year after the discontinuation of such therapy. Risk factors for recurrence include male sex, advanced age, and idiopathic or unprovoked pulmonary embolism (i.e., occurring in the absence of any identifiable risk factor for venous thromboembolism).The frequency of unprovoked pulmonary embolism can be as high as 50% among patients with pulmonary embolism. The risk of recurrence is particularly high among patients with cancer. The risk of recurrence is about 3% per year among patients in whom the first pulmonary embolism was associated with a temporary risk factor, such as major surgery, immobilization because of an acute medical illness, or trauma.
The duration of long-term anticoagulation should be based on the risk of recurrence after cessation of treatment with vitamin K antagonists, the risk of bleeding during treatment, and the patient's preference. In patients with pulmonary embolism secondary to a temporary (reversible) risk factor, therapy with vitamin K antagonists should be given for 3 months. Patients with unprovoked pulmonary embolism, those with cancer, and those with recurrent unprovoked pulmonary embolism are candidates for indefinite anticoagulation with periodic reassessment of the risk–benefit ratio.
Conventional-intensity warfarin therapy (INR target, 2.0 to 3.0) is recommended during the first 3 to 6 months after the acute event; after an initial course of conventional-intensity warfarin therapy, low-intensity warfarin therapy (INR target, 1.5 to 1.9) may be an option.Low-molecular-weight heparins should be chosen over warfarin for long-term therapy in patients with cancer and pregnant women.
Significance of Detectable Deep Venous Thrombosis in Patients with Pulmonary Embolism
Demonstrable DVT on compression ultrasonography appears to be associated with worse prognosis.
In patients with pulmonary embolism (PE), does coexistence of detectable deep venous thrombosis (DVT) have prognostic significance? Researchers in Spain addressed this question in a prospective cohort study of emergency department patients with acute PE confirmed by imaging. All patients additionally underwent compression ultrasonography of the lower extremities.Of 707 enrolled patients with PE, 51% had concomitant DVT. During 3 months of follow-up, all-cause mortality was significantly higher in patients with DVT than in those without DVT (15% vs. 6%).
Journal Watch General Medicine May 13, 2010
Comment: In patients with PE, demonstrable DVT on compression ultrasonography appears to be associated with worse prognosis. The next clinical question — not yet answered but worthy of investigation — is whether PE patients with detectable DVT should be treated more aggressively or for longer duration than those without DVT.
Should We Look for Silent PE in Patients with DVT?
Although one third of patients with lower-extremity deep venous thrombosis exhibited silent pulmonary embolism, routine screening for PE generally does not change management.Autopsy studies have shown that, even in patients with large or fatal pulmonary embolisms (PEs), most cases were unsuspected or undiagnosed ante mortem. This finding begs the question: Should standard screening for PE be performed in patients with deep venous thrombosis (DVT) but without clinical symptoms of PE?
Overall, silent PE was diagnosed in 32% of 5233 patients with DVT (27% in tier 1; 37% in tier 2). Silent PE was significantly more common among patients with proximal than with distal DVT (36% vs. 13%). Silent PE in DVT patients was associated with risk for recurrent PE.
New anticoagulant agents with a more predictable anticoagulant effect and reduced drug–drug interactions, as compared with warfarin, are currently under investigation for the treatment of venous thromboembolism. These agents do not require laboratory monitoring. Dabigatran, an oral antithrombin agent administered at fixed doses, has been shown to be as effective and safe as warfarin for the treatment of venous thromboembolism.
After an acute pulmonary embolism, patients should be monitored for chronic thromboembolic pulmonary hypertension.
The incidence of chronic thromboembolic pulmonary hypertension 2 years after the acute event ranges from 0.8 to 3.8%
Cardiovascular Safety of Inhaled Anticholinergic Agents for COPD
Two new analyses of tiotropium and ipratropium yield different results.A controversy has developed that involves the inhaled anticholinergic agents ipratropium (Atrovent) and tiotropium (Spiriva). In a 2008 meta-analysis of randomized trials in patients with chronic obstructive pulmonary disease, these drugs were associated with excess risks for cardiovascular death and myocardial infarction However, this meta-analysis did not include the UPLIFT trial .In UPLIFT, tiotropium was associated with significantly fewer serious cardiovascular events than was placebo.
Dual Antiplatelet Therapy After Drug-Eluting Stenting: When to Stop?
Combined data from two randomized trials suggest
no additional benefit after 1 year.
To determine the optimal duration of dual antiplatelet therapy (DAPT) with aspirin and clopidogrel after drug-eluting stent (DES) implantation, investigators in Korea combined data from two randomized trials that had similar designs and slower-than-anticipated enrollment. A total of 2701 patients who experienced no major adverse cardiovascular or bleeding events while taking DAPT for at least 12 months after receiving one or more DES (57% sirolimus-eluting) were assigned to either continue DAPT or receive low-dose aspirin alone.
Journal Watch cardiology March 15, 2010
Eighty-eight percent were enrolled between 12 and 18 months after stent implantation.
At 2-year follow-up (median, 19 months), the estimated rate of the primary composite endpoint — myocardial infarction (MI) and cardiac death — was 1.8% in the DAPT group and 1.2% in the aspirin-only group, a statistically nonsignificant difference. Compared with the aspirin-only group, the DAPT group showed a trend toward an increase in the secondary composite endpoint of MI, cardiac death, and stroke (hazard ratio, 1.84; P=0.06).The results also might not apply to patients who undergo surgery or who have multiple or more-complex stenting procedures, different DES types, or aspirin resistance. Until a larger randomized trial is completed, I will continue to recommend prolonged DAPT for most of my DES patients who have no contraindications or adverse effects.
Giving oxygen in acute myocardial infarction may raise death risk, Cochrane review concludes
Oxygen is routinely given to patients with acute myocardial infarction, with clinical guidelines in most countries recommending its use in emergency care. The rationale is that this may improve oxygenation of the ischaemic myocardium and so reduce cardiac pain, infarct size, and consequent morbidity and mortality. However, previous studies have found insufficient evidence to determine whether oxygen had any effect on these outcomes.
BMJ june 2010
None of the three trials—which had a total of 387 patients—showed that inhaled oxygen improved clinical outcomes. Among the 14 patients who died, nearly three times as many had been given oxygen as air in both the intention to treat analysis (including all patients) (relative risk 2.9 (95% confidence interval 0.9 to 9.8)) and the analysis of patients with confirmed acute myocardial infarction (relative risk 3.0 (0.9 to 9.4)). However, the small number meant that this difference did not reach statistical significance.
A definitive randomised controlled trial is urgently required given the mismatch between trial evidence suggestive of possible harm from routine oxygen use and recommendations for its use in clinical practice guidelines," the group recommend. They noted that as long ago as 1950 a study showed that giving pure oxygen through a face mask not only failed to reduce the duration of angina pain but also prolonged electrocardiographic changes indicative of acute myocardial infarction. "It is surprising that a definitive study to rule out the possibility that oxygen may do more harm than good has not been done," they said. Part of the failure to fund such a study may be due to the strong belief that giving oxygen will reduce the oxygen deficit in ischaemic myocardial tissue, the group suggests.
BMJ june 2010
Stenting versus Endarterectomy for Treatment of Carotid-Artery Stenosis
Among patients with symptomatic or asymptomatic carotid stenosis, the risk of the composite primary outcome of stroke, myocardial infarction, or death did not differ significantly in the group undergoing carotid-artery stenting and the group undergoing carotid endarterectomy. During the periprocedural period, there was a higher risk of stroke with stenting and a higher risk of myocardial infarction with endarterectomy.NEJM July 1 2010
The clinical durability of carotid-artery stenting and carotid endarterectomy is important. The rates of ipsilateral stroke during our follow-up period — 2.0% with carotid-artery stenting and 2.4% with carotid endarterectomy
Easily Missed?
Pulmonary embolismComplete occlusion of a peripheral pulmonary artery usually results in a pulmonary infarction with pleuritic chest pain and haemoptysis. When the blood clot is lodged in more proximal pulmonary arteries and is not occlusive, pulmonary infarction does not occur and pulmonary embolism might present as isolated dyspnoea. Massive pulmonary embolism is caused by large bilateral proximal clots resulting in haemodynamic collapse.
• However, most episodes of pulmonary embolism carry a low mortality risk (about 1%) when properly diagnosed and treated .
• Massive pulmonary embolism represents only 5% of all cases of pulmonary embolism and is fatal in about 40% of patients.
Why is it missed?
The classic triad of pleuritic chest pain, dyspnoea, and haemoptysis occurs in less than 10% of patients, but the most common symptoms (dyspnoea, chest pain) are non-specific. In 40% of cases, major thromboembolic risk factors are absent. Clinical signs of deep vein thrombosis are observed in only 15% of patients and haemoptysis in only 4.5-11% of cases.1 5 Pulmonary infarction with fever may mimic pneumonia. Chest pain reproducible on palpation also does not rule out pulmonary embolism.BMJ April 2010
In addition, abnormalities in chest radiographs or electrocardiograms are non-specific; sinus tachycardia is the most common electrocardiogram abnormality whereas right heart strain is observed only in severe cases. Arterial partial pressure of oxygen and the alveolar-arterial oxygen gradient are normal in 20% of patients; hypoxaemia with hypocapnia is the most common abnormality in blood gas pressures, but is non-specific. Symptoms and initial test findings can also be ascribed to underlying disease such as heart failure or chronic lung disease.
• Suspect pulmonary embolism in cases of unexplained dyspnoea or chest pain, or both, even in the absence of obvious risk or triggering factors
• Clinical probability assessment is the cornerstone of all validated diagnostic strategies.
FDA Approves Asclera to Treat Small Varicose Veins
The U.S. Food and Drug Administration approved Asclera (polidocanol) injection for the treatment of small types of abnormally swollen or twisted veins called varicose veins.Although they usually occur in the legs, varicose veins also can form in other parts of the body. Factors such as genetics, age, female gender, pregnancy, obesity, and prolonged periods of standing may increase the risk for varicose veins.
“Asclera is indicated for the treatment of small types of varicose veins when the aim of treatment is to improve appearance.”
Asclera is approved to close spider veins (tiny varicose veins less than 1 millimeter in diameter) and reticular veins (those that are 1 to 3 millimeters in diameter). Asclera acts by damaging the cell lining of blood vessels. This causes the blood vessel to close, and it is eventually replaced by other types of tissue.
Common adverse reactions to Asclera include leakage and collection of blood from damaged blood vessels at the injection site (hematoma), bruising, irritation, discoloration, and pain at the injection site.
Safety Announcement
[06-11-2010] The U.S. Food and Drug Administration (FDA) is evaluating data from two clinical trials in which patients with type 2 diabetes taking the blood pressure medication, Benicar (olmesartan) had a higher rate of death from a cardiovascular cause compared to patients taking a placebo.
FDA's review is ongoing and the Agency has not concluded that Benicar increases the risk of death. FDA currently believes that the benefits of Benicar in patients with high blood pressure continue to outweigh its potential risks.
FDA proposed to withdraw approval of the drug midodrine hydrochloride, used to treat the low blood pressure condition, orthostatic hypotension, because required post-approval studies that verify the clinical benefit of the drug have not been done.
This is defined as a narrowing of the aorta, usually just distal to the origin of the left subclavian artery, close to the ductus arteriosus/ligamentum arteriosum. Most patients have this juxtaductal coarctation. It is nearly always a congenital lesion but may very rarely be acquired through trauma causing aortic dissection, reducing the diameter of the true lumen of the aorta. It results in hypertension in the upper body and hypoperfusion of the lower body.
Severe cases may present in the neonatal period, or it may go unnoticed and be diagnosed in childhood or later, with the development of collateral circulation of blood to the lower body.
Coarctation of the Aorta
It can be particularly problematic for the pregnant woman. It is often associated with other cardiovascular malformations such as bicuspid aortic valve and ventriculo-septal defect (VSD). It may be associated with another syndrome, for example Turner's syndrome.Aortic coarctation is a cause of secondary hypertension and should be considered in its differential diagnosis. It may affect the abdominal aorta very rarely. Pseudo-coarctation of the aorta is due to excessive tortuosity of the aortic arch, but does not obstruct flow and there is no collateral circulation. It does not usually require active management after diagnosis.
Presentation
Antenatal presentationIt can be diagnosed with ultrasound in-utero. However it is difficult to diagnose antenatally.3
Neonatal presentation
If severe it usually presents in the first 3 weeks of life with poor feeding, lethargy, tachypnoea or overt congestive cardiac failure and shock. Initially the baby may be well depending on whether other anomalies are also present and how long the ductus arteriosus remains patent. However the infant becomes ill, often abruptly, with closure of the ductus arteriosus. The presence of a ventricular septal defect will accelerate development of symptoms.
Pulses may be reduced in amplitude and delayed between upper and lower limbs.
Blood pressure is higher in the upper limbs compared to lower limbs.
Differential cyanosis can occur with flow across the patent ductus from the right to the left side of the circulation. The upper body appears pink and the legs cyanotic.
A systolic murmur in the left infraclavicular area is typical but a range of murmurs may be heard depending on collateral circulation and the presence of other cardiac abnormalities.
Late presentation
Patients are usually asymptomatic and the diagnosis is usually made on examination, prompted often by the presence of for example a murmur or hypertension.It can cause headache, nosebleeds and leg cramps, particularly with exercise, although claudication is unusual.
If the left subclavian circulation is affected the left arm may be smaller.
Lower-limb muscle weakness, cold feet or neurological symptoms in the legs (poor blood supply to spinal cord) may be the presenting feature.
There may be physical features of Turner's syndrome when associated with this condition.
Pulses distal to the obstruction are diminished and delayed. Simultaneous palpation of upper and lower limb pulses reveals the clinical hallmark of radio-femoral delay with reduced pulse amplitude in lower limbs.Blood pressure (BP) may be higher in upper limbs, but the left arm BP can be normal or low if coarctation involves the origin of the left subclavian.
Auscultation reveals a systolic or continuous murmur, usually heard in left infraclavicular area and under the left scapula. An ejection click may signify associated bicuspid aortic valve (present in about 85% of cases). A thrill or hum due to flow in aberrant collateral vessels may be present over the chest or abdominal wall.
Imaging:
CXR may show signs of congestive cardiac failure, indentation of aortic shadow at site of coarctation, or notching on underside of ribs due to pressure from collateral blood vessels.Echocardiography allows estimation of the pressure gradient caused by the abnormality. This may help in determining severity and the need for intervention. Echocardiography is also used to delineate the coarctation and to help identify any associated abnormalities.
MRI is again used to fully delineate the nature of the coarctation and any associated abnormalities.
Management
Drug
Prostaglandin E1 is used in neonates to open the ductus and achieve improved haemodynamic stability when the patient presents acutely.
Diuretics and inotropes are used to treat congestive cardiac failure affecting neonates and adults alike.
Beta-blockers are used to treat hypertension in adults before physical correction of the coarctation, and may be used afterwards for persisting hypertension.
ACE inhibitors and angiotensin-II antagonists may be used alongside beta-blockers to treat post-correction hypertension if the aortic arch obstruction is eliminated. Patients are at risk of infective endocarditis and should receive appropriate antibiotic prophylaxis for procedures that may cause bacteraemia.
Surgery or balloon angioplasty
Angioplasty, with or without stenting, may be used to correct the coarctation. The decision on which technique to use will depend upon the severity of the coarctation, any associated abnormalities and the acuteness of the presentation.One small randomised controlled trial (RCT) reported an 86% reduction in peak systolic pressure gradient in both the balloon angioplasty group and the surgery group. A non-randomised study comparing balloon angioplasty with and without stent placement reported a statistically significant reduction in peak systolic gradient of 83% in the angioplasty alone group and 96% in the angioplasty with stent groupSurgery has been the standard treatment (for native coarctation and recoarctation) and involves open chest surgery. The surgery used depends on the anatomy of the lesion and preference of the surgeon, but may include resection of the coarctation site and end-to-end anastomosis repair, patch aortoplasty, left subclavian flap angioplasty, or bypass graft repair. More complex lesions require tailored reconstructive approaches.
Balloon angioplasty and stenting may be carried out as a first treatment (in native coarctation) or if previous surgical or angioplasty fails and coarctation recurs (recoarctation):
Prognosis If untreated, outlook is poor with less than a fifth surviving beyond age 50.2 Even after angioplasty or surgical treatment there is significant morbidity and mortality.
The main determinants of long term survival include factors such as age at operation and degree and duration of hypertension. With repair before age 14 the 20 year survival is 91% and after age 14 the 20 year survival is 79%.Long term follow-up studies have shown mean life expectancy of around 38 years of age for those treated in late childhood or early adulthood.8
Principal problems are recoarctation, late aneurysm formation, hypertension and/or premature coronary and cerebrovascular disease.
Long term follow-up with careful monitoring for development of complications and possible ongoing pharmacological therapy is needed.
Patients need to avoid excessively vigorous physical activity, contact sports and exercise that involves straining such as weightlifting. Those with good repair and blood pressure control can improve their outlook by taking regular gentle aerobic exercise.
Maternal mortality is high (3 to 8%) in pregnancy particularly if coarctation is not repaired. However whether repaired or not such pregnancies are high risk.
Complications
Re-coarctation after repair
Impaired left ventricular systolic/diastolic function progressing to congestive cardiac failure
Thoracic aortic aneurysm
Aortic dissection – high risk in pregnancy
Cerebral aneurysm rupture – high risk in pregnancy
Hypertension
Infective endocarditis
Paralysis due to spinal cord ischaemia
Recurrent laryngeal nerve palsy
Endocardial fibroelastosis
Hypertrophic cardiomyopathy
Postoperative chylothorax due to thoracic duct damage
Postoperative mesenteric arteritis due to sudden increase in visceral perfusion (post-coarctectomy syndrome)
In Hypertension, ACE Inhibitor Plus Calcium Channel Blocker Is Superior to ACE Inhibitor Plus Diuretic
Pairing an ACE inhibitor with a calcium channel blocker, rather than a diuretic, may offer greater cardiovascular benefit to hypertensive patients, reports the NEJM
ACCOMPLISH trial, some 11,500 hypertensive adults at high risk for cardiovascular events were randomized to receive the ACE inhibitor benazepril plus either the calcium channel blocker amlodipine or the diuretic hydrochlorothiazide.The trial was stopped early, after 3 years' follow-up, because of superior outcomes with benazepril-amlodipine. Namely, the incidence of the primary endpoint — a composite of cardiovascular events and cardiovascular death — was 9.6% with benazepril-amlodipine and 11.8% with benazepril-hydrochlorothiazide. (Blood pressure reductions were similar in the two groups.)
• Effects of Intensive Blood-Pressure Control in Type 2 Diabetes Mellitus
• The ACCORD Study GroupA total of 4733 participants with type 2 diabetes were randomly assigned to intensive therapy, targeting a systolic pressure of less than 120 mm Hg, or standard therapy, targeting a systolic pressure of less than 140 mm Hg. The primary composite outcome was nonfatal myocardial infarction, nonfatal stroke, or death from cardiovascular causes. The mean follow-up was 4.7 years. The annual rates of death from any cause were 1.28% and 1.19% in the two groups, respectively. The annual rates of stroke, a prespecified secondary outcome, were 0.32% and 0.53% in the two groups, respectively.
Serious adverse events attributed to antihypertensive treatment occurred in 77 of the 2362 participants in the intensive-therapy group (3.3%) and 30 of the 2371 participants in the standard-therapy group (1.3%) .
Conclusions In patients with type 2 diabetes at high risk for cardiovascular events, targeting a systolic blood pressure of less than 120 mm Hg, as compared with less than 140 mm Hg, did not reduce the rate of a composite outcome of fatal and nonfatal major cardiovascular events.
NEJM April 29 2010
Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysisCalcium supplements (without coadministered vitamin D) are associated with an increased risk of myocardial infarction. Ingestion of equivalent doses of calcium from dairy products has a much smaller effect than calcium supplements on serum calcium levels,53 which might account for the absence of a detrimental vascular effect of dietary calcium intake in the observational studies reviewed. Vascular calcification is an established risk factor for cardiovascular disease, and the process of vascular calcification is similar to osteogenesis.
BMJ July 2010
Because calcium supplements increase bone density it is possible that they may also increase vascular calcification and thereby cardiovascular events. calcium supplements accelerate vascular calcification and increase mortality in patients with renal failure, in both dialysis and predialysis populations. Primary hyperparathyroidism, a condition in which serum calcium levels are raised, has also been associated with an increased risk of cardiovascular events and death. A meta-analysis of trials totalling 12 000 participants found that calcium supplements increase the risk of myocardial infarction by about 30%.
Why Don't Implantable Cardioverter-Defibrillators Prevent Sudden Cardiac Death After Recent Myocardial Infarction?
The risk for sudden cardiac death (SCD) is particularly high in the early months after a myocardial infarction (MI). However, two trials of prophylactic implantable cardioverter-defibrillator (ICD) placement after MI failed to show a survival benefit in ICD recipients (JW Cardiol Jan 28 2005 and Oct 7 2009), in contrast to results of other ICD trials. To examine this lack of benefit more closely, investigators studied data from VALIANT, an international trial of valsartan in MI survivors
Of 14,703 participants with left ventricular dysfunction, clinical heart failure, or both, 2878 died during a median of 25 months of follow-up, and autopsy results were available for 398. Of these, the cause of death was clinically judged to be SCD in 105; autopsy revealed recurrent MI or cardiac rupture in 44; pump failure in 4; and stroke, pulmonary embolism, and drug overdose in 1 each. The proportion of clinically adjudicated SCDs that were nonarrhythmic on autopsy was even more dramatic during the first post-MI month (24 of 30 deaths).
This unique analysis of the causes of SCD early after MI yielded a surprising result: Nearly 50% of SCDs in the first 2 years — and 80% of SCDs within the first month — were nonarrhythmic. If confirmed in other populations, this finding would explain the failure of ICDs to prevent SCD in previous trials. This study appears to validate current guidelines that call for a 40-day delay in ICD placement after an acute MI.
Journal Watch cardiology August 11, 2010
• Pathophysiology of Heparin-Induced ThrombocytopeniaHeparin-induced thrombocytopenia (HIT) is caused by antibodies directed against a complex of heparin and platelet factor 4 (PF4); this antibody-heparin-PF4 complex activates platelets by binding to platelet Fc RIIa receptors. When this occurs, platelet counts can rapidly decline, and 30% to 50% of patients develop thrombosis. Why thrombi occur in some — but not all — patients was investigated by two research groups. Both groups concluded that monocytes play an important role in thrombus formation.
Journal Watch oncology and hematology January 26, 2010
Pneumatic Compression vs. Compression Stockings to Prevent Thrombosis
A guideline from the American College of Chest Physicians recommends that mechanical methods be used when high bleeding risk precludes use of antithrombotic drugs in patients at risk for deep venous thrombosis (DVT). However, the guideline does not take a position favoring intermittent pneumatic compression (IPC) or graduated compression stockings (GCS). because a recent study showed that GCS were associated with skin complications in stroke patients (Lancet 2009; 373:1958) — an editorialist favors IPC for patients who require mechanical prophylaxis.Targeted Temperature Management for Comatose Survivors of Cardiac Arrest Targeted temperature management, also known as therapeutic hypothermia, is a therapeutic intervention that is intended to limit neurologic injury after a patient’s resuscitation from cardiac arrest. Hypothermia causes a reduction in brain metabolism, including a reduction in oxygen utilization and ATP consumption.
• Therapeutic hypothermia should be considered for adult patients successfully resuscitated from a witnessed out-of-hospital cardiac arrest of presumed cardiac cause, though patients after in-hospital cardiac arrest may also benefit. This measure should also be considered in patients who are comatose, and in patients with an initial rhythm of ventricular fibrillation or nonperfusing ventricular tachycardia (or other initial rhythms such as asystole or pulseless electrical activity).
• What are the indications for therapeutic hypothermia?
• How is therapeutic hypothermia achieved?
• Several different cooling methods are available for use in therapeutic hypothermia. In the pivotal clinical trials, cooling was achieved by the application of numerous ice packs around the head, neck, torso, and limbs or with the use of a cold-air mattress covering the entire body. Other methods of surface cooling include the use of water-circulating cooling blankets or pads, refrigerated cooling pads, and thermal beds. Core cooling can be achieved with the use of intravascular cooling catheters (made of metal or containing balloons filled with cold saline) or by means of intravenous infusion of cold fluids. The objective is to reach a target temperature of 32 to 34°C and to maintain that temperature for 24 hours, if feasible.• What additional patient management is necessary before hypothermia is induced?
• Before hypothermia is induced, sedation, analgesia, and paralysis should be initiated to prevent shivering (which can lead to increased oxygen consumption, excessively laborious breathing, increased heart rate, and a general stress-like response, in addition to impeding the cooling process) and to minimize the patient’s discomfort.• What metabolic disturbances are induced by therapeutic hypothermia?
• Hypothermia can induce metabolic disturbances, including hypokalemia, hypomagnesemia, hypophosphatemia, and hyperglycemia. Therefore, regular measurement of electrolyte and glucose levels is necessary to guide the appropriate amount of electrolyte substitution and insulin therapy. Leukopenia and thrombocytopenia may occur but typically do not require intervention.Is CT Indicated for Patients With Isolated Syncope?
Syncope is defined as a sudden and brief loss of consciousness associated with loss of postural tone, from which recovery is rapid, spontaneous, and complete. Such events comprise up to 3% of all emergency department (ED) visits and up to 6% of all hospital admissions.The clinical evaluation of syncope begins with a thorough history, physical examination, and electrocardiogram. However, after careful evaluation, no readily diagnosed etiology of the syncopal event can be found in nearly 60% of patients.Even after a more thorough evaluation, which may include additional laboratory and imaging studies, no definitive cause may be found in as many as 57% of cases.As a result, the clinician may have continuing concern that these patients are at risk for life-threatening events.
Current guidelines have questioned the need for a "routine" computed tomography (CT) scan of the head to evaluate patients with isolated syncope.Yet, this remains a common practice in the United States.
Clinicians who order routine head CTs in patients with isolated syncope may be investigating the possibility of:
• Subarachnoid hemorrhage;
• Intraparenchymal hemorrhage;
• Subdural hemorrhage;
• Early infarct;
• Acute infarct; or
• Brain mass.
However, studies suggest that a head CT might provide new diagnostic information in only a fraction (4%) of patients with syncope.According to Day and colleagues, patients with positive findings on a head CT displayed either a focal neurologic deficit or had a history consistent with seizure.
Another study describes 117 patients who had head CTs following syncope, with no positive findings.Patients who had a competing indication for a head CT were excluded (eg, trauma, seizures, altered mental status, neurologic deficits upon presentation, intoxicated patients). Although this was a retrospective study, the results support the findings of previous studies by demonstrating that routine head CTs are not indicated in isolated syncopal events.
A more recent prospective, observational cohort study, which evaluated 113 consecutive patients, further demonstrated the low yield of head CT in syncope without associated trauma above the clavicles, use of warfarin, persistent neurologic deficit or complaint (dizziness, headache), or age > 65.Of 5 patients with positive head CTs, 2 had subarachnoid hemorrhage, 2 had intraparenchymal hemorrhage, and 1 patient had a cerebrovascular accident.
It is important to understand that strokes and syncope do not typically go together. Strokes generally do not lead to syncope, and most syncopal events do not present as stroke-like syndromes.One rare exception may occur in the setting of global bilateral cerebral ischemia or basilar artery disease affecting the reticular activating system, leading to ischemia that may present as a stroke-like syndrome. In theory, vertebrobasilar migraine also could lead to a syncopal event. However, in the evaluation of a patient with potential vertebrobasilar ischemia or transient ischemic attacks, magnetic resonance imaging and magnetic resonance angiograpy (not a CT scan) would be indicated.
Finally, in patients with sudden onset of a severe headache in the setting of a possible syncopal event (with concern for a subarachnoid hemorrhage), emergent head CT on arrival to the ED should be considered. Patients who present to the ED after a brief syncopal event, without focal neurologic symptoms, headache, altered mental status, or associated scalp trauma, and who are not taking anticoagulants, are unlikely to benefit from a routine head CT.
In fact, in 2006, the American Heart Association and American College of Cardiology stated that a neurologic cause of syncope should be considered only if suggested by history or physical examination.
With mostly retrospective data and only 1 published prospective observational cohort study to date,a formal randomized prospective study of head CTs in syncope would be ideal as the basis for a clinical decision rule that would enable risk stratification and would help determine the need for a head CT and further clinical evaluation.
Summary of Key Points
Patients who present to the ED with significant scalp trauma associated with syncope, patients with head trauma post-syncope who are taking oral anticoagulants, and patients with sudden onset of severe headache (with concern for subarachnoid hemorrhage) in the setting of syncope are candidates for head CTs.Patients without a history of trauma, lack of ongoing or persistent headache or neurologic deficits, or history of recent seizure activity in the setting of a syncopal event are unlikely to benefit from a routine head CT in the ED.
Medscape 09/17/2010
The document is an update of the 2008 consensus statement from the American College of Cardiology (ACC), the American Heart Association, and the American College of Gastroenterology (ACG), in which it was suggested that PPIs should be used in patients taking clopidogrel to reduce the risk of GI bleeding. The current document, released today, has taken a more cautious approach, acknowledging that concern about an interaction between these two classes of agent has been raised but adding that there is no good evidence that it has any clinical effect.
PPIs and Antiplatelets:
New Consensus Document
Heartwire © November 8 2010 Medscape
It concludes: "The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the cardiovascular efficacy of antiplatelet treatment because of a drug–drug interaction." It lists risk factors for GI bleeding as prior GI bleeding; advanced age; concomitant use of warfarin, steroids, or nonsteroidal anti-inflammatory drugs (NSAIDs); or Helicobacter pylori infection. It adds: "Patients without these risk factors for GI bleeding receive little if any absolute risk reduction from a PPI, and the risk/benefit balance would seem to favor use of antiplatelet therapy without concomitant PPI." But it also notes: "The reduction of GI symptoms by PPIs (ie, treatment of dyspepsia) may also prevent patients from discontinuing their antiplatelet treatment. The discontinuation of antiplatelet therapy in patients with GI bleeding may increase the risk of CV events."
Cardiologist Dr Mark Hlatky (Stanford University School of Medicine, CA), vice chair of the new consensus document's writing committee, commented to heartwire : "We brought this update out focused on this one particular issue because there have been many new studies on this interaction and people are confused. This interaction was just one section of the last consensus document on the GI risk with antiplatelet agents and NSAIDs. But that small section has now turned out to be a very important issue, so we have dedicated a whole new consensus document to it. We brought a group of experts together from both the cardiac and the GI sides, and we sifted through all the evidence available now to try to make sense of it all. Because the data are not definitive, our conclusions should be viewed as provisional."
Implanted heart devices are becoming more common, according to the statement. From 1997 to 2004, the rate of implantation increased 19% for permanent pacemakers and 60% for implantable cardioverter-defibrillators; despite improved methods for device implantation, the prevalence of infection has increased faster than the rate of implantation.
The notion of prescribing antibiotics to prevent infections from dental procedures dates back to a 1955 AHA statement, said Dr. Lockhart, but that recommendation was based on speculation at a time when antibiotics were seen as miracle drugs that could do no harm.
Recommendations for prophylaxis for various conditions such as orthopedic implants proliferated after that, all without evidence to support them.
Since then, several studies, including some by Dr. Lockhart, have failed to show an advantage to the prophylaxis.
Bacteria do enter the bloodstream from dental procedures, and oral bacteria can cause endocarditis, explained Dr. Lockhart, but most endocarditits is not caused by these strains of bacteria. He has not been able to find an actual case in which a dental procedure led to a bloodborne infection, and daily tooth brushing and food chewing release far more bacteria into the bloodstream than procedures that take place in a dental office.
Michael A. Siegel, DDS, chair of oral medicine at Nova Southeastern University in Fort Lauderdale-Davie, Florida, told Medscape Medical News that the new guidelines increase the legal risks for dentists who prescribe antibiotics as prophylaxis in most heart patients. "These dentists who give it to everyone just in case are going to be hung out to dry," he said.
If physicians recommend antibiotics contrary to the guidelines, dentists should insist that the physicians write the prescriptions, he said.
So who should get antibiotics to prevent endocarditis during dental procedures? The 2007 guidelines list the following conditions:
prosthetic cardiac valve or prosthetic material used for cardiac valve repair,previous infective endocarditis,
specific types of congenital heart disease, and
cardiac transplantation in patients who develop cardiac valvulopathy.
Patients with implanted devices probably do not run the risk of infection once their incisions are healed, said Dr. Siegel. "The long and the short of it is that once it's put in, give them 30 days to heal, and then there's no problem," said Dr. Siegel.
Unfractionated heparin has many well-recognized disadvantages, including the need for frequent monitoring, a risk of thrombocytopenia, and an increased risk of bleeding.
In contrast, low-molecular-weight heparins have a more predictable anticoagulant effect; in addition, there is no need for laboratory monitoring, rates of thrombocytopenia are lower, and administration can be performed by subcutaneous injection. Although low-molecular-weight heparins are generally indicated in myocardial infarction without ST-segment elevation or unstable angina, the limited evidence regarding their use in myocardial infarction with ST-segment elevation is conflicting. Prehospital administration of enoxaparin, as compared with unfractionated heparin, caused an increase in intracranial hemorrhage among elderly patients.
Fondaparinux is a synthetic pentasaccharide that selectively inhibits factor Xa.
Fondaparinux can be administered daily without laboratory monitoring.In small dose-ranging studies, a low dose of fondaparinux (2.5 mg) had similar efficacy to higher doses of fondaparinux and the standard dose of enoxaparin, with a similar or lower risk of bleeding.
Predicting prognosis in stable angina—results from the Euro heart survey of stable angina: prospective observational study
The rate of death and non-fatal myocardial infarction in the first year was 2.3 per 100 patient years; factors most predictive of adverse outcome were comorbidity, diabetes, shorter duration of symptoms, increasing severity of symptoms, abnormal ventricular function, resting electrocardiogaphic changes, The annual incidence of death in the survey was 1.5%, and the incidence of non-fatal myocardial infarction was 1.4%. In the subgroup with proved coronary disease these rates were 1.8% and 3.2%.
Unanswered research questions
• How long should patients with ST elevation myocardial infarction who have been treated with thrombolysis take aspirin plus clopidogrel, compared with aspirin alone?• How effective is long term continuation of drugs for secondary prevention after a myocardial infarction? For example, do all patients with normal left ventricular function benefit from long term treatment with blockers and angiotensin converting enzyme inhibitors?
• How effective is spironolactone compared with eplerenone in patients with heart failure and left ventricular dysfunction early after myocardial infarction?
• 4. What strategies are effective in improving uptake of and adherence to comprehensive cardiac rehabilitation programmes, particularly in groups under-represented in those programmes?
• 5. What is the added value of the non-exercise components of comprehensive cardiac rehabilitation programmes?
• 6. How effective are omega 3 acid ethyl esters in all patients after myocardial infarction?
• 7. What measures encourage the maintenance of regular exercise and a Mediterranean style diet beyond the period of comprehensive cardiac rehabilitation?
differences in thrombus formation between the arterial and venous systems
The low-flow and low-pressure venous system is susceptible to reduced blood flow (stasis) and systemic activation of the coagulation cascade, as Virchow described more than 150 years ago, which predisposes to a thrombus even in a nonstenotic vessel. Most venous thrombi consist predominantly of red cells enmeshed in fibrin and contain relatively few platelets; hence, they have been described pathologically as "red thrombi.“In contrast, in the high-flow and high-pressure arterial system, thrombi form under the influence of local shear forces, platelet activation, and exposure to thrombogenic substances on damaged vascular surfaces. Arterial thrombi, referred to as "white thrombi," typically are composed predominantly of platelets with relatively little fibrin or red-cell accumulation. Thus, it is plausible to expect that an anticoagulant would be used to prevent venous thromboemboli, whereas an antiplatelet agent would be used to prevent arterial thrombosis.
Angiogenesis: From Basic Science to Clinical Applications
In 1989, two consecutive reports in Science described the cloning of vascular endothelial growth factor (VEGF). Napoleone Ferrara, the editor of Angiogenesis, was an author of one of the 1989 reports in Science; his laboratory not only cloned the VEGF gene but also developed the anti–VEGF monoclonal antibodies bevacizumab and ranibizumab, now (FDA) approved for the treatment of malignant and ocular diseases, respectively.Abciximab is made from the Fab fragments of an immunoglobulin that targets the glycoprotein IIb/IIIa receptor on the platelet membrane.
is a platelet aggregation inhibitor mainly used during and after angioplasty to prevent platelets from sticking together and causing thrombus. Its mechanism of action is inhibition of glycoprotein IIb/IIIa.
In practice, platelet aggregation gradually returns to normal about 24 to 48 hours after discontinuation of the drug. While Abciximab has a short plasma half life, due to its strong affinity for its receptor on the platelets, it may occupy some receptors for weeks Abciximab has a plasma half life of about ten minutes, with a second phase half life of about 30 minutes. However, its effects on platelet function can be seen for up to 48 hours after the infusion has been terminated, and low levels of glycoprotein IIb/IIIa receptor blockade are present for up to 15 days after the infusion is terminated.
Many of the side effects of abciximab are due to its anti-platelet effects. This includes an increased risk of bleeding. The most common type of bleeding due to abciximab is gastrointestinal hemorrhage.
Thrombocytopenia is a rare but known serious risk. Abciximab-induced thrombocytopenia can typically be treated with transfusion of platelets. Abciximab induced thrombocytopenia can last for five days after initial drug administration. Transfusing platelets is the only known treatment and may have limited effectiveness as the drug may also bind to the new platelets. Platelet counts which should average 250,000-400,000 can effectively drop to zero
ReoPro is a clear, colorless, sterile, non-pyrogenic solution for intravenous (IV) use.
Each single use vial contains 2 mg/mL of Abciximab in a buffered solution (pH 7.2) of 0.01 M sodium phosphate, 0.15 M sodium chloride and 0.001% polysorbate 80 in Water for Injection. No preservatives are added.Abciximab is indicated as an adjunct
to patients undergoing percutaneous coronary intervention .in patients with unstable angina not responding to conventional medical therapy when percutaneous coronary intervention is planned within 24 hours
Safety and efficacy of Abciximab use in patients not undergoing percutaneous coronary intervention have not been established.
Abciximab is intended for use with aspirin and heparin and has been studied only in that setting, as described in CLINICAL STUDIES.
The safety and efficacy of Abciximab have only been investigated with concomitant administration of heparin and aspirin as described in Clinical Studies. In patients with failed PCIs, the continuous infusion of Abciximab should be stopped because there is no evidence for Abciximab efficacy in that setting.
In the event of serious bleeding that cannot be controlled by compression, Abciximab and heparin should be discontinued immediately.
The recommended dosage of Abciximab in adults is a 0.25 mg/kg intravenous bolus administered 10-60 minutes before the start of PCI, followed by a continuous intravenous infusion of 0.125 µg/kg/min (to a maximum of 10 µg/min) for 12 hours.
Patients with unstable angina not responding to conventional medical therapy and who are planned to undergo PCI within 24 hours may be treated with an Abciximab 0.25 mg/kg intravenous bolus followed by an 18- to 24-hour intravenous infusion of 10 µg/min, concluding one hour after the PCI.
Hypersensitivity reactions should be anticipated whenever protein solutions such as Abciximab are administered.
Epinephrine, dopamine, theophylline, antihistamines and corticosteroids should be available for immediate use. If symptoms of an allergic reaction or anaphylaxis appear, the infusion should be stopped and appropriate treatment given .