Antithrombotic Therapy for Venous Thromboembolic Disease
© 2008 American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition)
د. حسين محمد جمعة
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
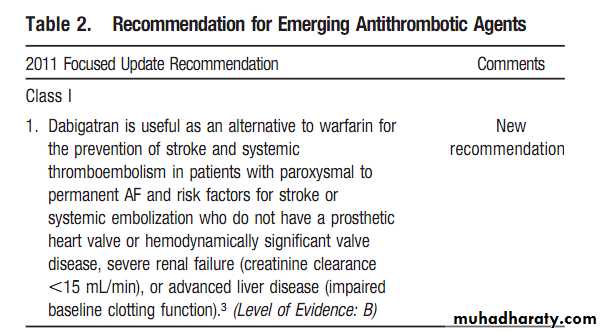
• Class I Benefit >>> Risk
• Procedure/ Treatment SHOULD be performed/ administered• Class IIa Benefit >> RiskAdditional studies with focused objectives needed
• IT IS REASONABLE to perform procedure/administer treatment
• Class IIb Benefit ≥ RiskAdditional studies with broad objectives needed; Additional registry data would be helpful
• Procedure/Treatment
• MAY BE CONSIDERED
• Class III
• Risk ≥ BenefitNo additional studies needed
• Procedure/Treatment should NOT be performed/administered SINCE IT IS NOT HELPFUL AND MAY BE HARMFUL
• Level A: Data derived from multiple randomized clinical trials or meta-analyses
• Multiple populations evaluated
• Level B: Data derived from a single randomized trial or nonrandomized studies
• Limited populations evaluated
• Level C: Only consensus of experts opinion, case studies, or standard of care
• Very limited populations evaluated
Applying Classification of Recommendations and Level of Evidence
Level of Evidence:
Initial Anticoagulation of Acute DVT of the Leg
For patients with objectively confirmedDVT, we recommend short-term treatment
with SC LMWH (Grade 1A), IV UFH (Grade 1A),monitored SC UFH (Grade 1A), fixed-dose SCUFH (Grade 1A), or SC fondaparinux (Grade 1A)rather than no such short-term treatment.
For patients with a high clinical suspicion
of DVT, we recommend treatment with anticoagulants while awaiting the outcome of diagnostic Tests.
In patients with acute DVT, we recommend
initial treatment with LMWH, UFH, orIn patients with acute DVT, we recommend
initiation of VKA together with LMWH,
UFH, or fondaparinux on the first treatment
day rather than delayed initiation of VKA
(Grade 1A).
In patients with acute DVT, if IV UFH is
chosen, we recommend that after an initial IV
bolus (80 U/kg or 5,000 U), it be administered by continuous infusion (initially at a dose of 18 U/kg/h or 1,300 U/h) with dose adjustment to achieve and maintain an activated partial thromboplastin time (APTT) prolongation that corresponds to plasma heparin levels of 0.3 to 0.7 IU/mL anti-Xa activity by the amidolytic assay.
In patients with acute DVT, if monitored SC
UFH is chosen, we recommend an initial dose of 17,500 U, or a weight-adjusted dose of about 250 U/kg bid, with dose adjustment to achieve and maintain an APTT prolongation that corresponds to plasma heparin levels of 0.3 to 0.7 IU/mL anti-Xa activity when measured 6 h after injection [Grade 1C].In patients with acute DVT, if fixed-dose,unmonitored SC UFH is chosen, we recommend an initial dose of 333 U/Kg followed by 250 U/kg bid [Grade 1C].In patients with acute DVT, we recommend
initial treatment with LMWH SC once ortwice daily, as an outpatient if possible (Grade
1C), or as an inpatient if necessary (Grade 1A),
rather than treatment with IV UFH.
In patients with acute DVT treated with
LMWH, we recommend against routine monitoring with anti-factor Xa level measurements (Grade 1A).
In patients with acute DVT and severe
renal failure, we suggest UFH over LMWH (Grade 2C).
In selected patients with extensive acute proximal DVT (eg, iliofemoral DVT, symptoms for <14 days, good functional status, life expectancy of≥1 year) who have a low risk of bleeding, we suggest that catheter-directed thrombolysis (CDT) may be used to reduce acute symptoms and postthrombotic morbidity if appropriate expertise and resources are available (Grade 2B).
After successful CDT in patients with acute DVT, we suggest correction of underlying venous lesions using balloon angioplasty and stents(Grade 2C).
We suggest pharmacomechanical thrombolysis (eg, with inclusion of thrombus fragmentation and/or aspiration) in preference to CDT alone to shorten treatment time if appropriate expertise and resources are available (Grade 2C).
After successful CDT in patients with acute DVT, we recommend the same intensity and duration of anticoagulant therapy as for comparable patients who do not undergo CDT (Grade 1C).
In selected patients with extensive proximal
DVT (eg, symptoms for < 14 days, good
functional status, life expectancy of≥1 year)
who have a low risk of bleeding, we suggest that
systemic thrombolytic therapy may be used to
reduce acute symptoms and postthrombotic
morbidity if CDT is not available (Grade 2C).
Percutaneous Venous Thrombectomy
In patients with acute DVT, we suggestthat they should not be treated with percutaneous mechanical thrombectomy alone (Grade 2C).
Operative Venous Thrombectomy for Acute DVT
In selected patients with acute iliofemoral DVT (eg, symptoms for < 7 days, good functional status, and life expectancy of≥1 year), we suggest that operative venous thrombectomy may be used to reduce acute symptoms and postthrombotic morbidity if appropriate expertise and resources are available (Grade 2B).If such patients do not have a high risk of bleeding, we suggest that catheter-directed thrombolysis is usually preferable to operative venous thrombectomy (Grade 2C).In patients who undergo operative venous thrombectomy, we recommend the same intensity and duration of anticoagulant therapy afterwards as for comparable patients who do not undergo venous thrombectomy (Grade 1C).
For patients with DVT, we recommend
against the routine use of a vena cava filter inaddition to anticoagulants (Grade 1A).
For patients with acute proximal DVT,
if anticoagulant therapy is not possible because
of the risk of bleeding, we recommend
placement of an inferior vena cava (IVC) filter
(Grade 1C).
For patients with acute DVT who have
an IVC filter inserted as an alternative to
anticoagulation, we recommend that they
should subsequently receive a conventional
course of anticoagulant therapy if their risk of bleeding resolves (Grade 1C).
In patients with acute DVT, we recommend
early ambulation in preference to initial bed rest when this is feasible (Grade 1A).Duration of Anticoagulant Therapy
For patients with DVT secondary to atransient (reversible) risk factor, we recommend treatment with a VKA for 3 months over treatment for shorter periods (Grade 1A).For patients with unprovoked DVT, we recommend treatment with a VKA for at least 3 months (Grade 1A).
Values and preferences: This recommendation attaches
a relatively high value to prevention of recurrent VTE
and a lower value to the burden of long-term anticoagulant
therapy.
We recommend that after 3 months of anticoagulant therapy, all patients with unprovoked DVT should be evaluated for the risk-benefit ratio of long-term therapy (Grade 1C).
For patients with a first unprovoked VTE that is aproximal DVT, and in whom risk factors for bleeding are absent and for whom good anticoagulant monitoring is achievable, we recommend
long-term treatment (Grade 1A).
Values and preferences: This recommendation attaches
a relatively high value to prevention of recurrent VTE
and a lower value to the burden of long-term anticoagulant
therapy.
For patients with a second episode of unprovoked VTE, we recommend long-term treatment (Grade 1A). For patients with a first isolated distal DVT that is unprovoked, we suggest that 3 months of anticoagulant therapy is sufficient rather than indefinite therapy (Grade 2B).
For patients with DVT and cancer, we recommend LMWH for the first 3 to 6 months of long-term anticoagulant therapy (Grade 1A).For these patients, we recommend subsequent anticoagulant therapy with VKA or LMWH indefinitely or until the cancer is resolved [Grade 1C].
In patients who receive long-term anticoagulant treatment, the risk-benefit ratio of continuing such treatment should be reassessed in the individual patient at periodic intervals (Grade 1C).
Intensity of Anticoagulant Effect
In patients with DVT, we recommend that the dose of VKA be adjusted to maintain atarget INR of 2.5 (range, 2.0 to 3.0) for all treatment durations (Grade 1A).For patients with unprovoked DVT who have a strong preference for less frequent INR testing to monitor their therapy, after the first 3 months of conventional-intensity anticoagulation (INR range,2.0 to 3.0), we recommend low-intensity therapy (range, 1.5 to 1.9) with less frequent INR monitoring over stopping treatment (Grade 1A).
Treatment of Asymptomatic DVT
of the Leg .In patients who are unexpectedly found to have asymptomatic DVT, we recommend the same initial and long-term anticoagulation asfor comparable patients with symptomatic DVT (Grade 1C).
Elastic Stockings and Compression Bandages To Prevent postthrombotic syndrome PTS
For a patient who has had a symptomatic proximal DVT, we recommend the use of an elastic compression stocking with an ankle pressure gradient of 30 to 40 mm Hg if feasible (Grade 1A).Compression therapy, which may include use of bandages acutely, should be started as soon as feasible after starting anticoagulant therapy and should be continued for aminimum of 2 years, and longer if patients have symptoms of PTS. (Note: feasibility, both short and long term, refers to ability of patients and their caregivers to apply and remove stockings.)
Values and preferences: This recommendation attaches a relatively high value to long-term prevention of the PTS and a low value to the burden (eg,inconvenience or discomfort) associated with wearing stockings.
Physical Treatment of PTS Without Venous Leg Ulcers
For patients with severe edema of the legdue to PTS, we suggest a course of intermittent pneumatic compression (IPC) [Grade 2B].
For patients with mild edema of the leg
due to PTS, we suggest the use of elastic compression stockings (Grade 2C).
Physical Treatment of Venous Leg Ulcers
In patients with venous ulcers resistant to
healing with wound care and compression, we suggest the addition of IPC (Grade 2B).
For patients with venous ulcers, we suggest
that hyperbaric oxygen not be used (Grade 2B). We suggest pentoxifylline, 400 mg po tid, in addition to local care and compression and/or IPC (Grade 2B).
In patients with persistent venous ulcers,
we suggest that rutosides, in the form of micronized purified flavonoid fraction administered orally, or sulodexide administered intramuscularlyand then orally, be added to local
care and compression (Grade 2B).
For patients with objectively confirmed PE,
we recommend short-term treatment with SCLMWH (Grade 1A), IV UFH (Grade 1A), monitored SC UFH (Grade 1A), fixed-dose SC UFH (Grade 1A), or SC fondaparinux (Grade 1A) rather than no such acute treatment. Patients with acute PE should also be routinely assessed for treatment with thrombolytic therapy.
For patients in whom there is a high clinical suspicion of PE, we recommend treatment with
anticoagulants while awaiting the outcome of diagnostictests (Grade 1C).
In patients with acute PE, we recommend initial treatment with LMWH, UFH or fondaparinux for at least 5 days and until the INR is > 2.0 for at least 24 h (Grade 1C).In patients with acute PE, we recommend initiation of VKA together with LMWH, UFH, or fondaparinux on the first treatment day rather than delayed initiation of VKA (Grade 1A).
In patients with acute PE, if IV UFH is chosen, we recommend that after an initial IV bolus (80 U/kg or 5,000 U), it be administered by continuous infusion (initially at dose of 18 U/kg/h or 1,300 U/h) with dose adjustment to achieve and maintain an APTT prolongation that corresponds to plasma heparin levels of 0.3 to 0.7 IU/mL anti-Xa activity by the amidolytic assay rather than administration as IV boluses throughout treatment, or administration without coagulation monitoring (Grade 1C).
In patients with acute PE, if monitored SC UFH is chosen, we recommend an initial dose of 17,500 U, or a weight-adjusted dose of approximately 250 U/kg bid, with dose adjustment to achieve and maintain an APTT prolongation that corresponds to plasma heparin levels of 0.3 to 0.7 IU/mL anti-Xa activity when measured 6 h after injection rather than starting with a smaller initial dose (Grade 1C).
In patients with acute PE, if fixed-dose, unmonitored SC UFH is chosen, we recommend an initial dose of 333 U/Kg followed by a twice daily dose of 250 U/kg rather than non–weightbased dosing (Grade 1C).
In patients with acute nonmassive PE, we recommend initial treatment withLMWH over IV UFH (Grade 1A).
In patients with massive PE, in other situations where there is concern about SC absorption, or in patients for whom thrombolytic therapy is being considered or planned, we suggest IV UFH over SC LMWH, SC fondaparinux,or SC UFH
(Grade 2C).
In patients with acute PE treated with LMWH, we recommend against routine monitoring with anti-factor Xa level measurements (Grade 1A).
In patients with acute PE and severe renal failure, we suggest UFH over LMWH (Grade 2C).
All PE patients should undergo rapid risk stratification (Grade 1C). For patients with evidence of hemodynamic compromise, we recommend use of thrombolytic therapy
unless there are major contraindications owing to bleeding risk (Grade 1B). Thrombolysis in these patients should not be delayed because irreversible cardiogenic shock may ensue.
In selected high-risk patients without hypotension who are judged to have a low risk of bleeding, we suggest dministration of thrombolytic therapy (Grade 2B).
The decision to use thrombolytic therapy depends on the
clinician’s assessment of PE severity, prognosis,and risk of bleeding.For the majority of patients with PE, we recommend against using thrombolytic therapy (Grade 1B).
In patients with acute PE, when a thrombolytic agent is used, we recommend that treatment be dministered via a peripheral vein rather than placing a pulmonary artery catheter to administer treatment (Grade 1B).
In patients with acute PE, with administration
of thrombolytic therapy, we recommend use
of regimens with short infusion times
(eg, a 2-h infusion) over those with prolonged infusion times (eg, a 24-h infusion) [Grade 1B].
For most patients with PE, we recommend against use of interventional catheterization techniques (Grade 1C).
In selected highly compromised patients who are unable to receive thrombolytic therapy because of bleeding risk, or whose critical status does not allow sufficient time for systemic thrombolytic therapy to be effective, we suggest use of interventional catheterization techniques if appropriate expertise is available (Grade 2C).
In selected highly compromised patients
who are unable to receive thrombolytic therapy because of bleeding risk, or whose critical status does not allow sufficient time for systemic thrombolytic therapy to be effective, we suggest that pulmonary embolectomy may be used ifappropriate expertise is available
(Grade 2C).
For most patients with PE, we recommend against the routine use of a vena caval filter in addition to anticoagulants (Grade 1A).
In patients with acute PE, if anticoagulant therapy is not possible because of risk of bleeding, we recommend placement of an IVC filter (Grade 1C).
For patients with acute PE who have an IVC
filter inserted as an alternative to anticoagulation,we recommend that they should subsequently receive a conventional course of anticoagulant therapy if their risk of bleeding resolves (Grade 1C).
For patients with PE secondary to a transient (reversible) risk factor, we recommend treatment
with a VKA for 3 months over treatment for shorter periods (Grade 1A).
For patients with unprovoked PE, we recommend treatment with a VKA for at least 3 months (Grade 1A). We recommend that after 3 months of anticoagulant therapy, all patients with unprovoked PE should be evaluated for the risk benefit ratio of long-term therapy (Grade 1C). For patients with a first unprovoked episode of VTE that is a PE, and in whom risk factors for bleeding are absent and for whom good anticoagulant monitoring is achievable, we recommend longterm
treatment (Grade 1A).
For patients with a second episode of unprovoked VTE, we recommend long-term treatment (Grade 1A).
For patients with PE and cancer, we recommend LMWH for the first 3 to 6 months of longterm anticoagulant therapy (Grade 1A). For these patients, we recommend subsequent anticoagulant therapy with VKA or LMWH indefinitely or until the cancer is resolved
(Grade 1C).
In patients with PE, we recommend that the dose of VKA be adjusted to maintain a target INR of 2.5 (INR range, 2.0 to 3.0) for all treatment durations (Grade 1A). For patients with unprovoked PE who have a strong preference for less frequent INR testing to monitor their therapy,after the first 3 months of conventional-intensity anticoagulation (INR range, 2.0 to 3.0), we recommend low-intensity therapy (INR range, 1.5 to 1.9) with less frequent INR monitoring over stopping treatment (Grade 1A).
We recommend against high-intensity VKA therapy (INR range,3.1 to 4.0) compared with an INR range of 2.0 to 3.0 (Grade 1A).
In patients who are unexpectedly found to
have asymptomatic PE, we recommend the same initial and long-term anticoagulation as for comparablepatients with symptomatic PE (Grade 1C).
Pulmonary Thromboendarterectomy, VKA, and Vena Caval Filter for the Treatment of Chronic Thromboembolic Pulmonary Hypertension .In selected patients with chronic thromboembolic
pulmonary hypertension (CTPH),such as those with central disease under the care of an experienced surgical/medical team,we recommend pulmonary thromboendarterectomy (Grade 1C).
For all patients with CTPH, we recommend life-long treatment with a VKA targeted to an INR of 2.0 to 3.0 (Grade 1C).
For patients with CTPH undergoing pulmonary thromboendarterectomy, we suggest the placement of a permanent vena caval filter before
or at the time of the procedure (Grade 2C).
For patients with inoperable CTPH, we
suggest referral to a center with expertise in pulmonary hypertension so that patients can be evaluated for alternative treatments, such as vasodilator therapy or balloon pulmonary angioplasty(Grade 2C).
Treatment of Infusion Thrombophlebitis
For patients with symptomatic infusionthrombophlebitis as a complication of IV infusion,
we suggest oral diclofenac or another nonsteroidal antiinflammatory drug (Grade 2B), topical diclofenac gel (Grade 2B), or heparin gel
(Grade 2B) until resolution of symptoms or for up
to 2 weeks. We recommend against the use of
systemic anticoagulation (Grade 1C).
Treatment of SVT
For patients with spontaneous superficial vein thrombosis, we suggest prophylactic or intermediate doses of LMWH (Grade 2B) or intermediate doses of UFH (Grade 2B) for at least 4 weeks.We suggest that as an alternative to 4 weeks of LMWH or UFH, VKA (target INR, 2.5; range, 2.0 to 3.0) can be overlapped with 5 days of UFH and LMWH and continued for 4 weeks (Grade 2C). We suggest that oral nonsteriodal antiinflammatory drugs should not be used in addition to anticoagulation (Grade 2B).
We recommend medical treatment with anticoagulants over surgical treatment
(Grade 1B).
Remark: It is likely that less extensive superficial vein thrombosis (ie, where the affected venous segment is short in length or further from the saphenofemoral junction) does not require treatment with anticoagulants.
It is reasonable to use oral or topical nonsteriodal antiinflammatory drugs for symptom control in such cases.
For patients with acute upper-extremity
DVT (UEDVT), we recommend initial treatment with therapeutic doses of LMWH, UFH,or fondaparinux as described for leg DVTFor most patients with UEDVT in association
with an indwelling central venous catheter,we suggest that the catheter not be removed
if it is functional and there is an ongoing
need for the catheter (Grade 2C).
For patients who have UEDVT in association
with an indwelling central venous catheter that is removed, we do not recommend that the duration of long-term anticoagulant treatment be shortened to< 3 months (Grade 2C).
In patients with UEDVT who have persistent
edema and pain, we suggest elastic bandagesor elastic compression sleeves to reduce symptoms of PTS of the upper extremity
(Grade 2C).
Anticoagulation is the main therapy for acute DVT of the leg. The main objectives of anticoagulant therapy in the initial treatment of this disease are to prevent thrombus extension and early and late recurrences of VTE.
Five options are available for the initial treatment of DVT:
(1) low-molecular-weight heparin (LMWH), administered (SC), without monitoring;(2) IV unfractionated heparin (UFH), with monitoring;
(3) SC UFH, with monitoring
(4); weight-based SC UFH,without monitoring; and
(5) SC fondaparinux, without monitoring.
In relationship to the duration of initial heparin therapy, two randomized clinical trial (RCTs) in patients with proximal DVT reported that IV UFH administered for 5 to 7 days is as effective as UFH administered for 10 to 14 days, providing that it is followed by adequate long-term anticoagulant therapy.The efficacy of this therapeutic approach is supported by subsequent studies that showed acceptable rates of recurrent VTE during 3 months of VKA therapy after 5 to7 days of heparin.
Shortening the duration of initial heparin therapy from approximately 10 to 5 days is
expected to have the added advantage of reducing the risk of heparin-induced thrombocytopenia. The currently recommended approach is to start both heparin and VKA at the time of diagnosis, and to discontinue heparin after 5 days provided the international normalized ratio (INR) is 2.0 for at least 24 h.Warfarin is generally started at a dose of 2.5 to 10 mg. Two trials performed in hospitalized patients showed that starting warfarin at a dose of 5 mg, compared to 10 mg, is associated with less excessive anticoagulation .A similar study
in outpatients failed to demonstrate an advantage to starting warfarin at a dose of 5 mg compared with 10 mg.
Observational studies have shown that lower VKA maintenance doses are required in older patients, women, and those with impaired nutrition and vitamin K deficiency. Taken together, these data suggest that warfarin can usually be started at a dose of 10 mg in younger (eg,<60 years), otherwise healthy outpatients, and at a dose of 5 mg in older patients and in those who are hospitalized. Subsequent doses should be adjusted
to maintain the INR at a target of 2.5
(range 2.0 to 3.0).
Heparin was initially administered by intermittent IV boluses, but this practice was replaced by continuous IV infusion, which was shown to be associated with a lower risk of bleeding. Initially, continuous IV infusions of UFH were administered at a starting dose of 1,000 U/h.
A prospective observational study showed that adjustment of the initial infusion rate of 1,000 U/h to achieve an activated partial thromboplastin time (APTT) ratio 1.5 improved efficacy. Such adjustment also resulted in patients receiving a mean UFH dose of adpproximately 1,300 U/h, rather than the initial infusion dose of 1,000U/h,and the higher initial infusion rate was adopted in clinical practice.
Adjustment of initial heparin dose in proportion to body weight has also been shown to be of value. When patients are treated with an initial heparin infusion of at least 1,250 U/h (corresponding to 30,000 U/d), or 18U/kg/h, it is uncertain if adjustment of heparin dose in response to the APTT or heparin levels improves efficacy or safety. However, as all studies that have used continuous IV UFH for treatment of thrombosis have adjusted UFH dose in response to coagulation monitoring, this practice is standard and uniformly recommended.
The starting dose of IV UFH for the treatment of DVT is either of the following:
(1) a bolus dose of 5,000 U, followed by a continuous infusion of at least 30,000 U for the first 24 h; or(2) a weight-adjusted regimen of a 80 U/kg bolus, followed by 18 U/kg/h. With both of these regimens, the infused dose of UFH should be adjusted using a standard nomogram to rapidly reach,and maintain, the APTT at levels that correspond to therapeutic heparin levels.
As noted in the preceding section, the requirement for an initial course of heparin was confirmed in a randomized controlled Study that reported a threefold-higher rate of recurrent VTE in patients who received VKA only.
Recommendation
In patients with acute DVT, if IV UFH is chosen, we recommend that after an initial IV bolus (80 U/kg or 5,000 U), it be administered by continuous infusion (initially at a dose of 18 U/kg/h or 1,300 U/h), with dose adjustment to achieve and maintain an APTT prolongation that corresponds to plasma heparin levels of 0.3 to 0.7 IU/mL anti-Xa activity by the amidolytic assay rather than administration as IV boluses throughout treatment, or administration without coagulation monitoringSC UFH Compared With IV Heparin for the Initial Treatment of DVT
UFH can be administered SC twice daily as an alternative to continuous IV infusion for the initial treatment of DVT. The relative value of IV and SC administration of UFH has been evaluated in eight clinical studies that included a total of 972 patients, and were reviewed in a metaanalysis .SC UFH administered twice daily appeared to be more effective (relative risk [RR] of extension or recurrence of VTE, 0.62; 95% confidence interval [CI], 0.39 to 0.98), and at least as safe (RR of major bleeding, 0.79; 95% CI, 0.42 to 1.48) as IV UFH, provided an adequate starting dose of SC UFH was administered.The usual regimen in these studies included an initial IV bolus of approximately 5,000 U followed by an SC dose of approximately 17,500 U bid on the first day, with subsequent adjustment to achieve a 1.5 to 2.5 prolongation of the APTT drawn 6 h after the morning dose. More recently, SC UFH, with and without dose adjustment in response to APTT measurements, has been compared with LMWH .
Recommendations
In patients with acute DVT, if monitored SC UFH is chosen, we recommend an initial dose of 17,500 U, or a weight-adjusted dose of approximately 250 U/kg bid, with dose adjustment to achieve and maintain an APTT prolongation that corresponds to plasma heparin levels of 0.3 to 0.7 IU/mL anti-Xa activity when measured 6 h after injection rather than starting with a smaller initial dose [Grade 1C].In patients with acute DVT, if fixed-dose, unmonitored SC UFH is chosen, we recommend an initial dose of 333 U/Kg followed by a twice daily dose of 250 U/kg rather than non–weightbased dosing [Grade 1C].
LMWHs have more predictable pharmacokinetics and greater bioavailability than UFH Due to these pharmacologic features, body weight-adjusted doses of LMWH can be administered SC once or twice daily without laboratory monitoring in the majority of patients.However, in certain clinical situations, such as
severe renal failure or pregnancy ,LMWH dose adjustment may be required using anti-Xa heparin levels. The usual time to perform the anti-Xa assay is 4 h after an injection, when heparin levels are expected to be at their highest. A target range of 0.6 to 1.0 IU/mL is suggested for twice-daily administration, and
a target range of 1.0 to 2.0 IU/mL is suggested for once-daily administration, although neither recommendation is firmly founded.
Indirect comparisons across studies also support that there is similar efficacy and safety with the following:
(1) once- and twice-daily administration,
(2) outpatient and inpatient administration, and
(3) use of different preparations of LMWH.
Recommendations
In patients with acute DVT, we recommendinitial treatment with LMWH SC once or twice daily, as an outpatient if possible (Grade 1C), or as an inpatient if necessary (Grade 1A),rather than treatment with IV UFH.
In patients with acute DVT treated with
LMWH, we recommend against routine monitoring
In patients with acute DVT and severe renal
failure, we suggest UFH over LMWH
(Grade 2C).
SC UFH Compared With SC LMWH for the Initial Treatment of DVT
Four randomized trials that included a total of 1,645 patients have compared SC UFH with SC LMWH .UFH was administered as an initial IV bolus followed by twice-daily SC injections of 12,500, 15,000, or 17,500 U initially, depending on the patient’s weight; subsequent UFH dosing was adjusted in response to APTT measurements. compared with LMWH, monitored SC UFH,there was no difference in recurrent VTE, major bleeding, or deaths .
Fondaparinux Compared With LMWH for the Initial Treatment of DVT
The synthetic pentasaccharide fondaparinux has been evaluated for short-term treatment of DVT and PE in the Matisse studies. In the Matisse DVT trial,59 2,205 patients were treated with a once-daily SC dose of fondaparinux (7.5 mg if 50 to 100 kg; 5.0 mg if 50 kg; 10 mg if 100 kg) or twice-daily SC LMWH (enoxaparin 1 mg/kg) for at least 5 days using a blinded design. With fondaparinux vs LMWH, there was no difference in recurrent VTE at 3 months (3.9% vs 4.1%; difference, 0.15%; 95% CI, – 1.8 to 1.5%]), major bleeding during treatment (1.1% vs 1.2%; difference, – 0.1%;95% CI, – 1.0 to 0.8%), or death at 3 months (3.8%vs 3.0%; difference, 0.8%; 95% CI, – 0.8 to 2.3%)(judged Grade 1A for noninferiority).New Antithrombotic Agents for the Short-term Treatment of DVT
A comparison of 6 months of ximelagatran (since withdrawn because of hepatic toxicity)with standard therapy in patients with DVT, and a comparison of 3 months or 6 months of idraparinux with standard therapy, are described in Section 2.5.
Treatment Strategies of Thrombus Removal for Acute DVT
Treatments that actively remove thrombus in patients with acute DVT have the potential to reduce acute symptoms and the risk for PTS. Thrombus removal directly reverses venous obstruction and can restore function in valves that were immobilized by thrombus. Indirectly, early removal of thrombus obstruction can prevent late development of venous valvular incompetence secondary to venous dilatation in distal venous segments that were never involved with thrombosis.Randomized trials, patient registries,and studies of other designs support that successful thrombus removal, using a variety of techniques,can improve patient outcomes .It is also possible that thrombus removal and relief of venous obstruction may reduce the risk of recurrent VTE. Patients with iliofemoral DVT are the subset of patients with the largest thrombus burden and highest risk for postthrombotic morbidity, with up to 75% having chronic painful edema and 40% having venous claudication when treated with anticoagulant therapy alone.
Catheter-Directed Thrombolysis for Acute DVT
The rationale for catheter-directed thrombolysis (CDT), which was established in patients with acute arterial occlusion, is that rapid lysis is achieved with lower doses of thrombolytic therapy, resulting in fewer serious bleeding complications.The addition of mechanical thrombus fragmentation,with or without aspiration, during CDT is commonly used as part of the procedure (collectively referred to as pharmacomechanical thrombolysis).
While randomized comparisons of CDT alone vs pharmacomechanical thrombolysis are not available, retrospective analyses suggest they are associated with similar rates of successful thrombolysis (70 to 80%) and of major bleeding (5 to 8%); however, pharmacomechanical thrombolysis is associated with shorter treatment times,shorter ICU and hospital stays, and reduced costs.
No randomized trial has compared CDT with systemic thrombolysis (see following); however, a single-center, retrospective study81 suggests that CDT achieves better lysis (50% vs 31%) and preservation of valve function
(44% vs 13%).
Recommendations
In selected patients with extensive acute proximal DVT (eg, iliofemoral DVT, symptomsfor < 14 days, good functional status, life expectancy > 1 year) who have a low risk of bleeding, we suggest that CDT may be used to reduce acute symptoms and postthrombotic morbidity if appropriate expertise and resources are available (Grade 2B).After successful CDT in patients with acute DVT, we suggest correction of underlying venous lesions using balloon angioplasty and stents (Grade 2C).
We suggest pharmacomechanical thrombolysis (eg, with inclusion of thrombus fragmentation and/or aspiration) in preference to CDT alone to shorten treatment time if appropriate expertise and resources are available (Grade 2C).
After successful CDT in patients with acute DVT, we recommend the same intensity and duration of anticoagulant therapy as for comparable patients who do not undergo CDT (Grade 1C).
Systemic Thrombolytic Therapy for Acute DVT
In 15 trials that randomized a total of 811patients with acute DVT to systemic thrombolytictherapy or to anticoagulant therapy alone, as assessed by early repeat phlebography, systemic thrombolytic therapy achieved a higher frequency of complete or significant lysis (54% vs 4%) or partial lysis (18% vs 14%) .thrombolytic therapy reduced postthrombotic morbidity and leg ulceration
Percutaneous Venous Thrombectomy
refers to catheter-based fragmentation of thrombus (eg, with pulse-spray or rotational devices) with, or without, aspiration of thrombus fragments,often combined with CDT, which, collectively, are referred to as pharmacomechanical thrombolysis.No randomized trials have compared percutaneous mechanical venous thrombectomy with other catheterbased, or noncatheter-based, treatments for DVT.Small retrospective studies suggest that percutaneous mechanical venous thrombectomy alone often fails to remove much of the thrombus and is associated with a high risk of PE.
Operative Venous Thrombectomy for
Acute DVTIs an alternative approach for thrombus removal that is generally
reserved for patients with iliofemoral DVT. Contemporary operative techniques and more effective anticoagulant regimens have improved outcomes compared to earlier reports.
Iliofemoral venous thrombectomy with a temporary arteriovenous fistula
plus anticoagulation was compared with anticoagulation alone in a randomized trial of 63 patients who were followed for a long term. Results at 6 months, 5 years, and 10 years were consistent with improved iliac vein patency, less leg swelling, and fewer leg ulcers .
Recommendations
In selected patients with acute iliofemoral DVT (eg, symptoms for < 7 days, good functional status, and life expectancy > 1 year), we suggest that operative venous thrombectomy may be used to reduce acute symptoms and postthrombotic morbidity if appropriate expertise and resources are available (Grade 2B). If such patients do not have a high risk of bleeding, we suggest that CDT is usually preferable to operative venous thrombectomy(Grade 2C).
In patients who undergo operative venous thrombectomy, we recommend the same intensity and duration of anticoagulant therapy afterwards as for comparable patients who do not undergo venous thrombectomy (Grade 1C).
Vena Caval Filters for the Initial Treatment of DVT
IVCs (and rarely superior vena caval [SVC]) filters can be used instead of initial anticoagulation (eg, unacceptable risk of bleeding), or as an adjunct to anticoagulation, in patients with acute DVT. No randomized trial or prospective cohort study have evaluated IVC filters as sole therapy in patients with DVT (ie, without concurrent anticoagulation).Permanent IVC filter insertion as an adjunct to anticoagulant therapy has been evaluated in a single, large RCT of patients with acute DVT who were considered to be at high risk for PE .
The findings of that study, which were reported after 2 years and 8 years of follow-up ,provide the strongest evidence to guide use of IVC filters in patients with acute VTE, and can be summarized as follows.
First, routine insertion of filters in patients who are also anticoagulated does not alter the frequency of recurrent VTE or total mortality.
Second, filters reduce PE at 12 days, 2 years and at 8 years
Third, filters increase DVT at 2 years .
Fourth, despite more frequent DVT during follow-up and frequent evidence of thrombosis at the filter site in those with recurrent VTE (43% of cases), filters were not associated with a higher frequency of PTS (defined as presence of at least one of edema, varicose veins, trophic disorders or ulcers)A comprehensive review136 of mostly retrospective case series of vena caval filter insertions (a total of 6,500 patients in 89 reports who had filters inserted for many different reasons) suggests that venous thrombosis at the site of filter insertion sites is common (eg, approximately 10% of patients),that filters can be placed above the renal veins if necessary, and that it is feasible to place filters in the SVC.
Epidemiologic data suggest that IVC filters are not associated with an increased risk of recurrent VTE in patients who present with DVT. If an IVC filter is being inserted in apatient with acute DVT or PE because anticoagulant therapy is temporarily contraindicated (eg,active bleeding), there is the option of inserting aretrievable filter and removing the filter when it is safe to start anticoagulant therapy. However, the risks and benefits of using a retrievable filter compared with a permanent filter in this setting are uncertain.
Recommendations
For patients with DVT, we recommend against the routine use of a vena cava filter in addition to anticoagulants (Grade 1A).For patients with acute proximal DVT if anticoagulant therapy is not possible because of risk of bleeding, we recommend placement of an IVC filter (Grade 1C).
For patients with acute DVT who have an IVC filter inserted as an alternative to anticoagulation,we recommend that they should subsequently receive a conventional course of
anticoagulant therapy if their risk of bleeding resolves
(Grade 1C).
Duration of Anticoagulant Therapy
Anticoagulant therapy for VTE should be continued for the following:(1) until its benefits (reduction of recurrent VTE) no longer clearly outweigh its risks (increase in bleeding), or
(2) it is patient preference to stop treatment even if continuing
treatment is expected to be of net benefit.
In order to assess if the benefits of continuing anticoagulant therapy will outweigh its risks, the increase in recurrent VTE and the decrease in bleeding that will occur with stopping treatment need to be known or estimated.
In addition, the consequences of a new episode of VTE and of an episode of bleeding need to considered.In patients with an average risk of bleeding while receiving anticoagulant therapy, therefore, the decision to stop or continue therapy is dominated by the risk of recurrent VTE if treatment is stopped.
Current evidence suggests that the risk of recurrence after stopping therapy is largely determined by two factors:
• whether the acute episode of VTE has been effectively treated;
• the patient’s intrinsic risk of having a new episode of VTE (ie, not arising directly from the episode of thrombosis for which patients have been receiving treatment).
If therapy is stopped before the acute episode of thrombosis is adequately treated, the risk of recurrent VTE will be higher than if anticoagulants were stopped after a longer course of treatment.
If patients have a persistently high intrinsic risk for thrombosis, even if the acute episode of thrombosis has effectively been treated, they will have a high risk of recurrence once anticoagulant therapy is stopped; if this risk is sufficiently high relative to the patient’s risk of bleeding, long-term anticoagulant therapy will be indicated.
During the past 15 years, a series of trials have compared different durations of anticoagulant therapy for VTE .Most of these studies excluded patients with active cancer
because they were judged to require long-term anticoagulant therapy because of a high risk of recurrence.
The earlier trials, in addition to comparing outcomes with different durations of treatment, identified that the risk of recurrent
VTE after stopping VKA therapy was much lower if VTE had been provoked by a reversible risk factor, such as surgery, rather than if the episode of VTE was unprovoked (also called idiopathic VTE). This observation was also made in a number of other prospective studies during the same period.
Longer or indefinite durations of anticoagulant therapy were generally evaluated in patients with unprovoked VTE, and shorter durations of therapy were evaluated in patients with a reversible provoking factor.
Because the presence of a reversible provoking risk factor, unprovoked VTE, and presence of active cancer were used to select patients for many of the studies, and have been shown to be the most important factors that influence risk of recurrent VTE after stopping VKA, separate recommendations for duration of anticoagulant therapy will be made for each of these three categories of patients with VTE.
Reversible provoking risk factors include the following: major factors such as surgery, hospitalization, or plaster cast immobilization, all within 1 month; and minor factors such as estrogen therapy, pregnancy, prolonged travel (eg, 8 h), or the previously noted major factors when they have occurred 1 to 3 months before diagnosis of VTE.
The greater the provoking reversible risk factor (eg, such as recent major surgery), the lower the expected risk of recurrence after stopping anticoagulant therapy. Within each of these three groups, we will consider if there are additional factors that influence the risk of recurrence enough to modify recommendations about duration of therapy.
The most important of such factors are the following:
(1) whether DVT was confined to the distal veins (often called isolated calf DVT) or involved the proximal veins, and
(2) whether the DVT was a first episode of VTE or a second or subsequent episode of VTE.
The presence of hereditary thrombophilia has not been used as a major factor to guide duration of anticoagulation for VTE in these guidelines because evidence from prospective studies suggests that these factors are not major determinants of the risk of recurrence.
VKAs for the Long-term Treatment of DVT
Clinical trials that have evaluated different durations of anticoagulant therapy can be divided into three categories according to the durations of therapy that were compared:• short vs intermediate durations,
• different intermediate durations,
(3) indefinite therapy vs intermediate durations.
Within each of these categories we will first consider studies that included heterogeneous (ie, less selected) patients with VTE, and then studies that enrolled subgroups of (ie, selected) patients who were expected to have either a lower (eg, associated with reversible risk factors) or a higher (eg,unprovoked, or second episodes, of VTE) risk of recurrence.
Short (4 Weeks or 6 Weeks) vs Intermediate (3 Months or 6 Months) Durations of Therapy
The first three studies (British Thoracic Society, Levine, DURAC 1; )which mainly enrolled unselected patients with proximal DVT or PE, found that shortening the duration of anticoagulation was associated with about double the frequency of recurrent VTE during follow-up of 1 to 2 years (an absolute risk increase of approximately 5%).
Major bleeding was uncommon during the incremental period of anticoagulation in these three studies (estimated at seven episodes among 1,009 patients during 259 patient-years of additional treatment [2.7%/yr]). Therefore, the main finding of these studies was that anticoagulant therapy should not be shortened to 4 or 6 weeks in patients with VTE.
Different Intermediate Durations of Therapy (6 Months or 12 Months vs 3 Months)
Two studies have compared 6 months vs 3 months of anticoagulant therapy in patients with predominantly first episodes of DVT or PE (unprovoked,or provoked by a reversible risk factor) .There was no difference in the risk of recurrence during follow-up in both studies.Indefinite vs Intermediate Durations of Anticoagulant Therapy
Four trials have compared indefinite (where indefinite refers to extended therapy without scheduled stopping of treatment) with stopping therapy in patients with VTE who were believed to have a high risk of recurrence because thrombosis was a second episode,
unprovoked,or was unprovoked and had a positive d-dimer result 1 month after stopping therapy .The results indicate that randomization to indefinite treatment with conventional-intensity VKA (target INR, 2.5) reduces recurrent VTE by approximately 90% (RR for the three studies, 0.10; 95% CI,
The benefit of indefinite treatment with VKA is partially offset by the risk of major bleeding. In the two initial studies of extended treatment ,the incidence of major bleeding was approximately 3%/yr during extended treatment with conventional-intensity warfarin (included bleeding during the first 6 months of therapy.However, in the more recent PROLONG study and a randomized comparison of conventional-intensity and low-intensity VKAextended treatment with conventional intensity VKA was associated with a risk of major bleeding of approximately 1% per patient-year .
A metaanalysis of seven studies that compared durations of conventional-intensity anticoagulant therapy for VTE estimated the rate of major bleeding to be 1.1% per patient-year .Thus, for patients with unprovoked DVT (and PE), the benefit of long-term treatment is partially offset by a higher risk of bleeding, and patients lose protection against recurrent VTE if anticoagulants are withdrawn.
For these reasons, values and preferences regarding preventing recurrent thromboembolism,avoiding bleeding complications and inconvenience of treatment, bear on the recommendation for long-term anticoagulant treatment for unprovoked VTE, particularly after a first episode of DVT (lower risk of recurrence than after a second episode of VTE, and expected to have a lower risk of death with a recurrence than after a first episode of PE .
Individual patient risk of recurrent VTE and of major bleeding may differ from the average values that have been reported in the previously noted trials and, in selected patients, may influence the decision to continue or stop anticoagulant therapy once 3 months of initial treatment has
been completed.
Of factors that have been evaluated as risk factors for recurrent VTE among patients with unprovoked DVT,
isolated calf DVT vs proximal DVT
one or more previous episodes of VTE .
negative d-dimer findings 1 month after withdrawal of VKA .Antiphospholipid antibody .
hereditary thrombophilia
males vs females (relative risk 1.6)
residual thrombosis in the proximal veins
Of factors that have been evaluated as risk factors for major bleeding during anticoagulant therapy, the following appear to have the greatest potential to be clinically useful markers of increased risk:
• older age,particularly after 75 years;
• previous GI bleeding,particularly if not associated with a reversible cause;
• previous noncardioembolic stroke;
• chronic renal or hepatic disease;
• concomitant antiplatelet therapy (to be avoided if possible);
• other serious acute or chronic illness;
• poor anticoagulant control; suboptimal monitoring of anticoagulant therapy
Recommendations
For patients with DVT secondary to atransient (reversible) risk factor, we recommend treatment with a VKA for 3 months over treatment for shorter periods (Grade 1A).2.1.2. For patients with unprovoked DVT, we recommend treatment with a VKA for at least 3 months (Grade 1A). We recommend that after 3 months of anticoagulant therapy, all patients with unprovoked DVT should be evaluated for the risk-to-benefit ratio of long-term therapy (Grade 1C).For patients with a first unprovoked VTE that is a proximal DVT, and in whom risk factors for bleeding are absent and for whom good anticoagulant monitoring is achievable,we recommend long-term treatment (Grade 1A).
Values and preferences: This recommendation attaches a relatively high value to prevention of recurrent VTE and a lower value to the burden of long-term anticoagulant therapy.
For patients with a second episode of unprovoked VTE, we recommend long-term treatment (Grade 1A).
For patients with a first isolated distal DVT that is unprovoked, we suggest that 3 months of anticoagulant therapy is sufficient
rather than indefinite therapy (Grade 2B).
For patients with DVT and cancer, we recommend LMWH for the first 3 to 6 months of long-term anticoagulant therapy (Grade 1A).
For these patients, we recommend subsequent anticoagulant therapy with VKA or LMWH indefinitely or until the cancer is resolved [Grade 1C].
Intensity of Anticoagulant Effect
The preferred intensity of the anticoagulant effect of treatment with VKA has been established by the results of randomized trials. The ELATE study was a randomized, blinded trial that compared low-intensity VKA (target INR, 1.5 to 1.9) with conventional-intensity VKA (INR, 2.0 to 3.0) for indefinite treatment of patients with unprovoked VTE who had completed at least 3 months of initial conventional-intensity anticoagulation .
The incidences of recurrent VTE were 1.9% per patient year in the low-intensity group, and 0.6% per patient-year in the conventional-intensity group.
The incidences of major bleeding were 0.96% per patient-year in the low-intensity group and 0.93% per patient-year in the conventional-intensity group; the corresponding incidences of all bleeding (major and minor) were 4.9% per patient-year and 3.6% per patient-year. Thus, low-intensity VKA treatment was less effective than conventional-intensity therapy and did not provide a safety advantage. although
more effective, requires more frequent INR monitoring
Recommendation
In patients with DVT, we recommend that the dose of VKA be adjusted to maintain atarget INR of 2.5 (range, 2.0 to 3.0) for all treatment durations (Grade 1A).For patients with unprovoked DVT who have a strong preference for less frequent INR testing to monitor their therapy, after the first 3 months of conventional-intensity anticoagulation (INR range,2.0 to 3.0).we recommend low-intensity therapy (INR range, 1.5 to 1.9) with less frequent INR monitoring over stopping treatment (Grade1A). We recommend against high-intensity VKA therapy (INR range, 3.1 to 4.0) compared to an INR range of 2.0 to 3.0 (Grade 1A).
New Antithrombotic Agents for Long-term Treatment of DVT
Ximelagatran (since withdrawn because of hepatic toxicity) has been evaluated for both short-term and long-term treatment of VTE. In the short-term treatment study, patients with acute DVT were treated for 6 months with ximelagatran, 36 mg bid, or LMWH followed by VKA therapy (INR, 2.0 to 3.0),using a blinded design. The frequency of recurrent VTE at 6 months was similar with ximelagatran (2.1%) and usual therapy (2.0%).The long-acting pentasaccharide idraparinux
was reported to be as effective and as safe as VKA for the first 3 or 6 months of treatment of DVT (but less effective that VKA in patients with PE). After an initial 6 months of treatment with either idraparinux or warfarin (52% of patients initially presented with symptomatic DVT), compared with placebo, 6 months of extended therapy with idraparinux markedly reduced recurrent VTE and increased bleeding.Treatment of Asymptomatic DVT of the Leg
Screening of postoperative patients for the presence of asymptomatic DVT is not recommended;instead, surgical patients should receive appropriate primary prophylaxis for VTE. If asymptomatic proximal DVT is detected, for example, in patients who have screening performed because they could not receive recommended VTE prophylaxis or in patients who have imaging studies performed for other reasons (eg, staging of cancer), care should be taken to ensure that DVT is truly present and patients should be treated.we recommend the same initial and long-term anticoagulation as for comparable patients with symptomatic DVT (Grade 1C). Asymptomatic proximal DVT detected by routine ultrasound screening in the setting of aclinical trial evaluating VTE prophylaxis in hospitalized medical patients has been shown to be associated with increased mortality at 3 months
Postthrombotic Syndrome
PTS is a cluster of leg symptoms and signs inpatients with previous DVT. PTS occurs in 20 to 50% of patients after acute DVT. The initial treatment of acute DVT may influence the presence and severity of PTS, as discussed earlier .The most prominent symptoms are
1.chronic postural dependent swelling and pain, 2.ambulatory discomfort, and skin pigmentation.
3.most extreme manifestation is a venous ulcer of the lower leg.
Elastic Stockings and Compression Bandages To Prevent PTS
Four randomized trials have evaluated the efficacy of compression stockings for the prevention of PTS following DVT .(30 to 40 mm Hg ankle gradient) or no stockings after a first episode of acute symptomatic proximal DVT, demonstrated that 47% of the control group had mild-to-moderate PTS compared with 20% of patients in the stocking group. Twentythree percent of patients in the control group vs 11% of patients in the stocking group had severe PTS.Recommendation
For a patient who has had a symptomatic proximal DVT, we recommend the use of an elastic compression stocking with an ankle pressure gradient of 30 to 40 mm Hg if feasible (Grade 1A). Compression therapy, which may include use of bandages acutely,should be started as soon as feasible after starting anticoagulant therapy and should be continued for a minimum of 2 years, and longer if patients have symptoms of PTS.(Note: feasibility, both short-term and longterm,refers to ability of patients and their caregivers to apply and remove stockings.)
Values and preferences: This recommendation attaches
a relatively high value to long-term prevention of the PTS and a low value to the burden (eg, inconvenience or discomfort) associated with wearing stockings.
Recommendations
For patients with severe edema of the leg due to PTS, we suggest a course of IPC (Grade 2B).For patients with mild edema of the leg due to PTS, we suggest the use of elastic compression stockings (Grade 2C).
Recommendation
In patients with venous ulcers resistant to
healing with wound care and compression, we
suggest the addition of IPC (Grade 2B).
IPC for 4 h daily added to standard
wound care and compression significantly increased healing.(IPC was found to increase transcutaneous oxygen tension, reduce edema, and increase skin temperature in the short-term
Recommendation
For patients with venous ulcers, we suggestthat hyperbaric oxygen not be used
(Grade 2B).
Recommendations
In patients with venous leg ulcers, wesuggest pentoxifylline, 400 mg po tid, in addition to local care and compression and/or IPC (Grade 2B).
In patients with persistent venous ulcers,
we suggest that rutosides, in the form of
MPFF adminstered orally, or sulodexide administered intramuscularly and then orally,be added to local care and compression(Grade 2B).
Initial Treatment of Acute PE
Treatment regimens for DVT and PE are similar because the two conditions are manifestations of the same disease process. When patients with VTE are carefully studied, the majority of those with proximal DVT also have PE (symptomatic or asymptomatic) andvice versa.
Furthermore, clinical trials of anticoagulant therapy have yielded similar estimates for efficacy and safety in patients with DVT alone, in those with both DVT and PE, and in patients with only PE.
The risk of recurrence also appears to be similar after PE and after proximal DVT.
The vast majority of patients with VTE who receive adequate anticoagulation survive. However, there are some important differences between patients who present with PE and those who present with DVT that justify separate consideration of treatment for PE.
First, the risk of early death (within 1 month) from VTE, due to either the initial acute episode or recurrent VTE, is much greater after presenting with PE than after DVT; this difference may justify more aggressive initial treatment for PE (eg, thrombolytic therapy, insertion of an IVC filter, more intensive anticoagulant therapy) compared with DVT.
Second, recurrent episodes of VTE are about three times as likely to be PE after an initial PE than after an initial DVT (ie, approximately 60% after a PE vs 20% after a DVT) this difference may justify more aggressive, or more prolonged, long-term therapy.
Third, the long-term sequelae of PE are cardiorespiratory impairment, especially due to pulmonary hypertension,rather than PTS of the legs or arms.
IV or SC UFH, SC LMWH, SC Fondaparinux,
and VKA for the Initial Treatment of PEAnticoagulant Therapy vs No Anticoagulant Therapy
Recommendations
For patients with objectively confirmed PE, we recommend short-term treatment with SC LMWH (Grade 1A), IV UFH (Grade 1A),monitored SC UFH (Grade 1A), fixed-dose SC UFH (Grade 1A), or SC fondaparinux (Grade 1A)rather than no such short-term treatment.
Patients with acute PE should also be routinely assessed for treatment with thrombolytic therapy .
For patients for whom there is a high clinical suspicion of PE, we recommend treatment with anticoagulants while awaiting the outcome of diagnostic tests (Grade 1C).
In patients with acute PE, we recommend initial treatment with LMWH, UFH, or fondaparinux for at least 5 days and until the
INR is > 2.0 for at least 24 h (Grade 1C).
In patients with acute PE, we recommend initiation of VKA together with LMWH, UFH, or fondaparinux on the first treatment day rather than delayed initiation of VKA
(Grade 1A).
In patients with acute PE, if IV UFH is chosen, we recommend that after an initial IV bolus (80 U/kg or 5,000 U), it be administered
by continuous infusion (initially at dose of 18 U/kg/h or 1,300 U/h) with dose adjustment to achieve and maintain an APTT prolongation
that corresponds to plasma heparin levels of 0.3 to 0.7 IU/mL anti-Xa activity by the amidolytic assay rather than administration as IV boluses throughout treatment, or administration without coagulation monitoring (Grade 1C).
In patients with acute PE, if monitored SC UFH is chosen, we recommend an initial dose of 17,500 U, or a weight-adjusted dose of about 250 U/kg bid, with dose adjustment to achieve and maintain an APTT prolongation that corresponds to plasma heparin levels of 0.3 to 0.7 IU/mL anti-Xa activity when measured
6 h after injection rather than starting with a smaller initial dose (Grade 1C).
In patients with acute PE, if fixed-dose,unmonitored SC UFH is chosen, we recommend an initial dose of 333 U/Kg followed by
a twice-daily dose of 250 U/kg rather than non–weight-based dosing
(Grade 1C).
In patients with acute nonmassive PE, we recommend initial treatment withLMWHover IV UFH (Grade 1A). In patients with massive PE, in other situations where there is concern about SC absorption, or in patients for whom thrombolytic therapy is being considered or planned, we suggest
IV UFH over SC LMWH, SC fondaparinux, or SC UFH (Grade 2C).
In patients with acute PE treated with LMWH, we recommend against routine monitoring with anti-factor Xa level measurements (Grade 1A).
In patients with acute PE and severe renal failure, we suggest UFH over LMWH (Grade 2C).
New Antithrombotic Agents for the Initial Treatment of PE
In addition to the synthetic pentasaccharide fondaparinux ,several other new antithrombotic agents have recently been developed . ximelagatran has been compared with LMWH and VKA therapy for the initial 6 months of short-term treatment of DVT, and one third of these patients had concomitant PE (not available for clinical use because of associated liver toxicity). The long-acting pentasaccharide idraparinux was reported to be less effective than standard therapy with heparins and VKA for the first 3 to 6 months of treatment of PE.Systemically and Locally Administered Thrombolytic Therapy for PE
Thrombolytic therapy for PE remains controversial. The fundamental problem is that 800 PEpatients have been enrolled in randomized trials of thrombolysis plus anticoagulation vs anticoagulation alone .The results of such trials have been summarized in three recently published metaanalyses. In one overview, which included 11 studies totalling 748 patients with PE of varying severity, thrombolysis was associated with trends toward reduction in recurrent PE (2.7% vs4.3%;), reduction in all-cause mortality (4.3% vs 5.9%;), and an increase in major bleeding (9.1% vs 6.1%;).
In the subset of five trials (total of 254 patients) that focused on patients with more severe PE, the reduction in mortality (6.2% vs 12.7%;) and the increase in major bleeding (21.9% vs 11.9%;) were more marked with thrombolytic therapy.
There is widespread agreement that thrombolytic therapy should be used to treat PE associated with hemodynamic compromise. Justification for this is that, compared with anticoagulation alone, thrombolytic therapy has demonstrated the following:
(1) acceleration of thrombus lysis as evidenced by more rapid
resolution of perfusion scan abnormalities, decrement in angiographic thrombus, reduction in elevated pulmonary artery pressures, and normalization of right ventricular dysfunction ,and(2) trends toward improved clinical outcomes in subgroups of patients
with hemodynamic compromise.
However, delaying thrombolytic therapy until patients with PE are pressor dependent is detrimental because prolonged inadequate tissue perfusion can cause irreversible multisystem organ failure. Consequently, selection of patients with PE to receive thrombolytic therapy requires rapid and accurate risk stratification of the competing risks of death from PE and of bleeding.
The risk of death is very high in the presence of sustained hypotension and cardiogenic shock .However, such patients are rare, accounting for approximately 5% of patients with a diagnosis of PE.
In the presence of normal systemic arterial pressure,prognostication depends on the following:
• Clinical evaluation,
• cardiac biomarkers such as troponin,and
• assessment of right ventricular size and function.
• Clinical evaluation begins with general appearance, BP, heart rate, respiratory rate, temperature, and pulse oximetry. The next step is physical examination to detect findings of right ventricular dysfunction such as distended jugular veins, asystolic murmur of tricuspid regurgitation, or an accentuated P2.
Right ventricular enlargement on the CT pulmonary angiogram, defined as a right ventricular diameter 90% than the left ventricular diameter,appears to be an independent risk factor for death and nonfatal clinical complications.
Clues on the ECG include right-bundlebranch block, SIQIIITIII, and T wave inversion in leads V1 through V4. Elevation of cardiac troponins indicates right ventricular microinfarction; echocardiography may show right ventricular hypokinesis; both are independent risk factors for early mortality and are associated with a worse outcome when they occur together.
Among patients without hemodynamic compromise,
poor prognostic indicators include the following:(1)patients who appear ill, with marked dyspnea, anxiety,and low oxygen satuartion;
(2) elevated troponin, indicating right ventricular microinfarction;
(3) right ventricular dysfunction on echocardiography; and
(4) Right ventricular enlargement on chest CT.
These sick patients are at high risk for an adverse outcome and may derive benefit from thrombolytic therapy, even if they initially maintain systemic arterial pressure. Consequently,in distinction to the last version of these guidelines that generally discouraged treatment of PE with thrombolytic therapy unless there was hemodynamic compromize, we suggest administration of thrombolytic therapy in selected high-risk patients without hypotension who are judged to have a low risk of bleeding.
Assessment of bleeding risk with thrombolytic therapy is similar in patients with PE and with acute ST-segment elevation myocardial infarction.Assessment of bleeding risk with thrombolytic therapy is similar in patients with PE and with acute ST-segment elevation myocardial infarction.
Major contraindications to thrombolytic therapy include intracranial disease,
Uncontrolled hypertension at presentation, and recent major surgery or trauma.Because of the inadequacy of currently available data, further studies are required to determine the risk and benefits of thrombolytic therapy in patients with severe PE who do not have hemodynamic compromise.In 2007, a European trial began enrolling patients with submassive PE who had preserved systolic BP, elevated troponin levels, and right ventricular enlargement on echocardiography. This trial will randomize approximately 1,000 patients to thrombolysis with a bolus regimen of tenecteplase plus heparin vs heparin alone.
In summary, there is good evidence that thrombolytic therapy accelerates resolution of PE and results in more rapid hemodynamic improvement.The evidence that thrombolytic therapy improves clinical outcome is less secure. In the absence of risk factors for bleeding, patients who are hemodynamically
compromised are very likely to benefit, as are sick patients with major pulmonary arterial obstruction,although the evidence supporting the latter group is indirect.
Choice of Thrombolytic Therapy Regimen
Nine randomized trials (total of 621 patients)
have compared the rate of thrombus resolution
achieved with various IV thrombolytic regimens. These regimens included urokinase administered over 2 h or 12 h; streptokinase given over 2 h, 12 h or 24 h; and recombinant tissue plasminogen activator (rt-PA) administered over 15 min or 2 h.42,–An additional study compared IV with catheterdirected pulmonary arterial administration of rt-PA (50 mg 2 h).
The results of these studies suggest the following:
• prolonged infusions of thrombolytic agents (eg, 12 h) are associated with higher rates of bleeding;• 2-h infusions achieve more rapid clot lysis than 12- or 24- h infusions;
• when a high-concentration, 2-h infusion of thrombolysis is administered, there is no clear difference in the efficacy or safety of rt-PA vs streptokinase;
(4) the relative efficacy and safety of bolus rt-PA regimens (eg, approximately 50 mg in 15 min) compared with a 2-h infusion of 100 mg of rt-PA is uncertain293,299,301; and
(5) infusion of rt-PA directly into a pulmonary artery as opposed to a peripheral vein does not accelerate thrombolysis but does cause more frequent bleeding at the catheter insertion site (there was no attempt to infuse rt-PA directly into, or to mechanically disrupt, the thrombus in this study from 1988).
When a lytic agent is appropriate for PE, current evidence supports that thrombolytic therapy should be infused into a peripheral vein over 2 h or less. rt-PA, at a dose of 100 mg over 2 h, is currently the most widely used and evaluated regimen. In patients with imminent or actual cardiac arrest, bolus infusion of thrombolytic therapy is indicated.
Initial Anticoagulant Therapy in Patients Treated
With Thrombolytic TherapyIn the absence of a contraindication, anticoagulationwith UFH, LMWH, or fondaparinux should not be delayed until diagnostic testing for PE has been completed. IV UFH has been used in conjunction with thrombolytic therapy in the trials that have evaluated thrombolysis for PE .
Consequently, initial anticoagulation with IV UFH is
appropriate if thrombolytic therapy is being considered.Different regimens of IV UFH have not been compared in randomized trials in patients with PE who are treated with thrombolytic therapy.
Before thrombolytic therapy is administered, IV
UFH should be administered in full therapeutic
doses (eg, bolus of 80 U/kg followed by 18U/kg/h initially). During administration of thrombolytic therapy, it is acceptable to either continue, or suspend, the UFH infusion (these two practices have never been compared). During a 2-h infusion of 100 mg of tPA, US regulatory bodies recommend suspension of IV UFH, whereas IV UFH is continued during the tPA infusion in manyother countries.
After administration of thrombolytic therapy, IV UFH should be restarted or continued.In the United States, it is recommended that the APTT is checked immediately after completion of the tPA infusion and that, provided the APTT is not 80 s, IV UFH is restarted without a bolus at the same rate of infusion as was being used before tPA was started. If UFH has not been suspended, the infusion is continued at the same rate with ongoing adjustment according to APTT results.
Recommendations
All PE patients should undergo rapid riskstratification (Grade 1C). For patients with evidence of hemodynamic compromise, we recommend use of thrombolytic therapy unless there are major contraindications owing to bleeding risk (Grade 1B). Thrombolysis in these patients should not be delayed because irreversible cardiogenic shock may ensue. In selected high-risk patients without hypotension who are judged to have a low risk of bleeding, we suggest administration of thrombolytic therapy (Grade 2B).
The decision to use thrombolytic therapy depends on the clinician’s assessment of PE severity,prognosis, and risk of bleeding. For the
majority of patients with PE, we recommend
against using thrombolytic therapy (Grade 1B).
In patients with acute PE, when a thrombolytic
agent is used, we recommend that treatment
be administered via a peripheral vein rather than placing a pulmonary artery catheter to administer treatment (Grade 1B).
In patients with acute PE, with administration of thrombolytic therapy, we recommend use of regimens with short infusion times (eg, a 2-h infusion) over those with prolonged infusion times (eg, a 24-h infusion) [Grade 1B].
Catheter Extraction or Fragmentation for the Initial Treatment of PE
Interventional catheterization techniques for massive PE include mechanical fragmentation of thrombus with a standard pulmonary artery catheter, clot pulverization with a rotating basket catheter, percutaneous rheolytic thrombectomy, or pigtail rotational catheter embolectomy. Pharmacologic thrombolysis and mechanical interventions can be combined when bleeding risk is not high.The goal of catheter extraction of thrombus is to reduce pulmonary arterial resistance enough to reduce pulmonary artery hypertension, alleviating right ventricular dilatation and dysfunction, and rapidly increase cardiac output. Catheter embolectomy rarely results in extraction of massive pulmonary arterial thrombus. More often, clot fragments are suctioned through the catheter or displaced distally with modest angiographic improvement.
Recommendation
For most patients with PE, we recommendagainst use of interventional catheterization
techniques (Grade 1C). In selected highly
compromised patients who are unable to receive
thrombolytic therapy because of bleeding
risk, or whose critical status does not allow
sufficient time for systemic thrombolytic therapy
to be effective, we suggest use of interventional
catheterization techniques if appropriate
expertise is available (Grade 2C).
Pulmonary Embolectomy for the Initial Treatment of PE
Emergency surgical embolectomy with cardiopulmonary bypass is another management strategy for patients with massive PE. This operation is also suited for acute PE patients who require surgical excision of aright atrial thrombus or impending paradoxical arterial embolism, or closure of a patent foramen ovale.Surgical embolectomy can also be performed to rescue patients in whom thrombolysis has been unsuccessful.
Outcomes are better when patients are referred before the onset of cardiogenic shock. At one hospital, 47 patients underwent surgical embolectomy in a 4-year period with a 96% survival rate. The procedure isbest performed on a warm, beating heart, without aortic cross-clamping, cardioplegia, or fibrillatory arrest.
Recommendation
In selected highly compromised patientswho are unable to receive thrombolytic therapy because of bleeding risk, or whose critical status does not allow sufficient time for systemic thrombolytic therapy to be effective, we suggest that pulmonary embolectomy may be used if
appropriate expertise is available
Vena Caval Filters for the Initial Treatment of PE
vena caval filters can be used instead of initial anticoagulant therapy (eg, unacceptable risk of bleeding) or as an adjunct to anticoagulation in patients with acute VTE.The PREPIC study, which evaluated IVC filters as an adjunct to anticoagulation in 400 high-risk patients with proximal DVT, showed that filters reduced PE, increased DVT, and did not change overall frequency of VTE (DVT and/or PEcombined).
The PREPIC study included 145 patients (36% of total) with symptomatic PE and 52 patients (13% of total) with asymptomatic PE at enrolment in addition to proximal DVT. Multivariable analyses did not find an association between the presence of PE at entry and the frequency of PE at 2 years; however, such an association was present after 8 years of follow-up.
There is uncertainty about the risk and benefits of inserting an IVC filter as an adjunct to anticoagulant and thrombolytic therapy in patients with massive PE. Among patients with hemodynamic compromise in the International Cooperative Pulmonary Embolism
Registry, insertion of an IVC filter was associated with a reduction of early recurrent PE and death.
Epidemiologic data suggest that insertion
of an IVC filter in patients who present with PE (with or without symptomatic DVT) is associated with about a doubling of the frequency of VTE during follow-up;most of this increase is due to a higher frequency of DVT (approximately 2.6-fold increase) rather than PE
(approximately 1.3-fold increase).
Recommendations
For patients with PE, we recommend against the routine use of a vena caval filter inaddition to anticoagulants (Grade 1A).. In patients with acute PE, if anticoagulant therapy is not possible because of risk of bleeding,we recommend placement of an IVC filter (Grade 1C).For patients with acute PE who have an IVC filter inserted as an alternative to anticoagulation,we recommend that they should subsequently receive a conventional course of anticoagulant therapy if the risk of bleeding resolves (Grade 1C).
Long-term Treatment of Acute PE
In the following sections, studies that were performed exclusively in patients with PE will be emphasized.In addition, subgroup analyses of PE patients enrolled in studies that included patients who only presented with symptoms of DVT will be presented. As the findings of studies with DVT patients are relevant to PE patients, and as the findings of studies performed exclusively in patients with PE have been consistent with studies that included DVT patients, the recommendations for long-term treatment of PE are the same as for DVT.VKA for the Long-term Treatment of PE
There has been only one evaluation of duration of VKA therapy exclusively in patients with PE. After 3 months of initial treatment, patients with PE provoked by a temporary risk factor were randomized to stop or to receive 3 more months of therapy, and those with unprovoked PE were randomized to stop or to receive 6 more months of therapy.Consistent with studies that included patients who presented with DVT, extended VKA therapy was effective while treatment was being received. However, extending the duration of treatment beyond 3 months did not lower the rates of recurrence that were observed when anticoagulants were subsequently stopped.
LMWH for the Long-term Treatment of PE
Two small studies have compared long-term LMWH (enoxaparin,1 mg/kg SC bid for approximately 14 days, followed by 1.5 mg/kg/d SC) with long-term VKA exclusively in patients who presented with PE. The combined results of these two studies are that there was a similar frequency of recurrent VTE (enoxaparin: 4/60; VKA:1/40) and major bleeding (enoxaparin: 1/60; VKA: 2/40) with the two treatments.Of the 12 other studies that compared LMWH with VKA therapy for long term treatment of VTE ,only 2 studies included patients with PE; in these 2 studies, all patients had cancer and 295 patients had PE (36% of all enrolled patients; some PE may have been asymptomatic in one study); subgroup analyses were not reported for the PE patients.
New Antithrombotic Agents for the Long-term Treatment of PE
Fondaparinux has not been evaluated as a long-term treatment for VTE. As previously noted ,ximelagatran has been shown to markedly reduce recurrent VTE without increasing bleeding in patients with VTE who had completed 6 months of initial treatment with VKAs. In this study, ximelagatran was noted to be equally effective in thesubgroup of 447 patients with PE (35% of total) as in the patients with DVT alone.
The long-acting pentasaccharide idraparinux
was reported to be less effective than standard therapy with heparins and VKA for the first 3 to 6 months of treatment of PE. After an initial 6 months of treatment with either idraparinux or warfarin (48%of patients initially presented with symptomatic PE),compared with placebo, 6 months of extended therapy with idraparinux markedly reduced recurrent VTE and increased bleeding.Treatment of Asymptomatic PE
Diagnosis of unexpected PE when contrast-enhanced CT is performed for other indications has become relatively common. Usually (eg, approximately 80% of cases), CT has been performed to evaluate known cancer, and the prevalence of incidental PE is higher in inpatients that in outpatients (eg, approximately 4% vs 1% of CTscans). When there is evidence of an unexpected PE, the first priority is to review the CT scans to determine if the findings are convincing for acute PE.Other recent CT scans may be available for comparison, or the current scan may also reveal DVT in the central deep veins (eg, subclavian, IVC, iliac).If there is any uncertainty about the presence of acute PE, additional diagnostic testing is required (eg, d-dimer, ultrasonography of the deep veins,dedicated CT pulmonary angiography). When PE is diagnosed unexpectedly in patients with cancer, the clinical history often reveals symptoms suggestive of PE.
Recommendations
For patients with PE secondary to a transient (reversible) risk factor, we recommend treatment with a VKA for 3 months over treatment for shorter periods (Grade 1A).For patients with unprovoked PE, we recommend treatment with a VKA for at least 3 months (Grade 1A). We recommend that after 3 months of anticoagulant therapy, all patients with unprovoked PE should be evaluated for
the risk-benefit ratio of long-term therapy (Grade 1C).
For patients with a first unprovoked episode of VTE that is a PE, and in whom risk factors for bleeding are absent and for whom good anticoagulant monitoring is achievable,we recommend long-term treatment (Grade 1A).
Values and preferences: This recommendation attaches a relatively high value to prevention of recurrent
VTE and a lower value to the burden of
long-term anticoagulant therapy.
For patients with a second episode of unprovoked VTE, we recommend long-term treatment (Grade 1A).
For patients with PE and cancer, we recommend LMWH for the first 3 to 6 months of long-term anticoagulant therapy (Grade 1A).
For these patients, we recommend subsequent anticoagulant therapy with VKA or LMWH indefinitely or until the cancer is resolved (1C).
In patients who receive long-term anticoagulant
treatment, the risk-benefit ratio of continuing
such treatment should be reassessed in the
individual patient at periodic intervals (1C).
In patients with PE, we recommend that the dose of VKA be adjusted to maintain a target INR of 2.5 (INR range, 2.0 to 3.0) for all treatment durations (Grade 1A). For patients with unprovoked PE who have a strong preference for less frequent INR testing to monitor their therapy, after the first 3 months of conventional-intensity anticoagulation (INR range, 2.0 to 3.0), we recommend low-intensity therapy (INR range, 1.5 to 1.9) with less frequent INR monitoring over stopping treatment (Grade 1A). We recommend against high-intensity VKA therapy (INR range, 3.1 to 4.0) compared with an INR range of 2.0 to 3.0 (Grade 1A).
In patients who are unexpectedly found to have asymptomatic PE, we recommend the same initial and long-term anticoagulation as for comparable patients with symptomatic PE (Grade 1C). Chronic Thromboembolic Pulmonary Hypertension CTPH occurs much more frequently after acute PE than had previously been believed. The old teaching was that CTPH had a prevalence of not more than 1 in 500 cases of acute PE; however,data from prospective cohort studies indicate. the frequency is approximately 3%. After acute PE initiates CTPH, pulmonary vascular remodeling may cause severe pulmonary hypertension out of proportion to pulmonary vascular thrombosis.
Pulmonary Thromboendarterectomy, VKA, and Vena Cava Filter for the Treatment of CTPH
Primary therapy forCTPH is pulmonary thromboendarterectomy,which, if successful, can reduce and sometimes cure pulmonary hypertension. The operation requires a median sternotomy, institution of cardiopulmonary bypass,deep hypothermia with circulatory arrest periods,and exploration of both pulmonary arteries. Pulmonarythromboendarterectomy removes organized thrombus by establishing an endarterectomy plane in all involved vessels. most experienced centers, the mortality rate is 5%.The most common postoperative problem is reperfusion pulmonary edema, generally managed with supportive care that requires several days of mechanical ventilation. When pulmonary thromboendarterectomy is successful, patients can usually resume normal daily activities and experience a greatly improved quality of life. Management usually includes insertion of a permanent vena cava filter before or during pulmonary endarterectomy and indefinite anticoagulant therapy with a target INR of 2.5.
Patients with CTPH who are not candidates for pulmonary endarterectomy because of comorbid disease or surgically inaccessible lesions may be candidates for pulmonary artery angioplasty. It is possible that some of the medical
therapies for idiopathic pulmonary hypertension
might have a beneficial role in CTPH, especially in
those patients who are not surgical candidates or who have a poor response to thrombendarterectomy due to distal microvascular disease.
Novel therapies include prostacyclin analogs such as epoprostenol,beraprost, iloprost and treprostinil, endothelin receptor antagonists such as bosentan, and phosphodiesterase-5 inhibitors such as sildenafil.
Recommendations
In selected patients with CTPH, such as those with central disease under the care of an experienced surgical/medical team, we recommend pulmonary thromboendarterectomy (Grade 1C).For all patients with CTPH, we recommend life-long treatment with a VKA targeted to an INR of 2.0 to 3.0 (Grade 1C).
For patients with CTPH who undergo pulmonary thromboendarterectomy, we suggest the placement of a permanent vena caval filter before or at the time of the procedure (2C).
For patients with inoperable CTPH, we suggest referral to a center with expertise in pulmonary hypertension so that patients can be
evaluated for alternative treatments, such as vasodilator therapy or balloon pulmonary angioplasty (Grade 2C).
Superficial Vein Thrombosis
Treatment of Infusion Thrombophlebitis , Peripheral vein infusion thrombophlebitis is estimated to occur in 25 to 35% of hospitalized patients who have peripheral IV catheters. In a three-arm randomized trial hospitalized patients with infusion thrombophlebitis, diclofenac emulsion gel used topically three times daily and oral diclofenac (75 mg bid) were superior to placebo in relieving local symptoms of thrombophlebitis at 48 h, with positive responses in 60% in both active treatment groups vs only 20% in the control group.Recommendation
For patients with symptomatic infusionthrombophlebitis as a complication of IV infusion,we suggest oral diclofenac or another nonsteroidal antiinflammatory drug (NSAID) [Grade 2B],topical diclofenac gel (Grade 2B), or heparin gel (Grade 2B) until resolution of symptoms or for up to 2 weeks. We recommend against the use of
systemic anticoagulation (Grade 1C).
Treatment of SVT
SVT has been less well studied than DVT but is estimated to occur more often. It commonly
affects the lower limbs, often involves a varicose vein, is associated with chronic venous insufficiency, malignancy, thrombophilia, pregnancy or exogenous
estrogens, obesity, sclerotherapy and a history of VTE, or it may be unprovoked.
Although traditionally considered a benign disease,a number of studiesindicate that the consequences of SVT may be more serious and have led to trials of more aggressive treatment with the goals of reducing symptoms, extension, recurrence,and progression to .The treatment of superficial vein thrombosis has been the subject of arecent Cochrane Collaboration systematic review.
Short-Duration Heparin, LMWH, and NSAIDs
In a placebo-controlled trial, patients with SVT were randomly allocated to receive 8 to 12 days of enoxaparin in two dosages (40 mg and 1.5 mg/kg SC daily, tenoxicam 20 mg po daily, or placebo).During the treatment period and at 3-month followup,rates of SVT extension or recurrence were 29.5% and 33.0%, respectively, in the placebo group, significantly higher than that of the other three treatment groups (enoxaparin 40 mg, 8.3% and 14.5%;enoxaparin 1.5 mg/kg, 5.7% and 15.1%; tenoxicam,13.1% and 15.2%).Rates of DVT tended to be lower in the treatment groups vs the placebo group during the initial treatment period, but this trend was lost by 3 months, predominantly due to the occurrence of VTE in the treatment groups during the first 3 weeks after treatment was stopped, suggesting that the initial duration of therapy was inadequate.
Longer Courses of Heparin or LMWH
A blinded randomized trial337 compared a 30-day course of low- vs high-dose SC nadroparin in 164 patients with SVT. During 3 months of follow-up, there were five cases of SVT extension in the lowdosegroup (all occurred on treatment), compared with two cases in the high-dose group (one occurred on treatment).
There were two symptomatic DVTs in the low-dose group vs three DVTs (two symptomatic)
and one symptomatic PE (occurred on treatment) in the high-dose group. Lack of a control group precludes assessment of whether either of the treatments was more effective than no treatment; for example, the rate of VTE at 3 months in the high dose group (4.8%) was similar to the 3-month rate of VTE in the placebo group (4.5%) of the previouslydescribed STENOX trial.
Surgical vs Medical Therapy
A nonblinded randomized trial with six treatment arms that included approximately 70 patients per group showed that compression alone or in addition to flush ligation of the saphenous vein were inferior to complete vein stripping or treatment with UFH, LMWH, or warfarin (doses and durations of treatment were not specified) for the end point of SVT extension at 3 months.A second trial342 compared saphenofemoral ligation, performed under local anesthesia, with enoxaparin 1 mg/kg bid for 1 week, and then daily for 3 weeks. During 6-month follow-up, VTE occurred in two patients (6.7%) in the surgery group (both PE) vs none in the enoxaparin group, while SVT occurred inone patient (3.3%) in the surgery group and three patients (10%) in the enoxaparin group.
Two patients in the surgical group had wound infections, and the cost of surgical treatment was more than three times higher that of medical treatment. comparing surgical therapy to anticoagulation for SVT showed similar rates of SVT progression but higher rates of VTE and complications with surgical therapy.
Recommendation
For patients with spontaneous superficial vein thrombosis, we suggest prophylactic or intermediate doses of LMWH (Grade 2B) or intermediate doses of UFH (Grade 2B) for at least 4 weeks. We suggest that as an alternative to 4 weeks of LMWH or UFH, VKA (target INR,2.5; range, 2.0 to 3.0) can be overlapped with 5 days of UFH and LMWH and continued for 4 weeks (Grade 2C).We suggest that oral NSAIDs should not be used in addition to anticoagulation (Grade 2B). We recommend medical treatment with anticoagulants over surgical treatment (Grade 1B).
Remark: It is likely that less extensive superficial vein thrombosis (ie, where the affected venous segment is short in length or further from the saphenofemoral junction) does not require treatment with anticoagulants. It is reasonable to use oral or topical NSAIDs for symptom control in such cases.
Acute UEDVT
Although most episodes of DVT occur in the lower limbs, it is estimated that 1 to 4% of cases involve the upper extremities. UEDVT can be classified into two etiologic groups: primary (includes unprovoked with orwithout thrombophilia, effort related, and thoracic outlet syndrome) and secondary (provoked by central venous catheters, pacemakers, or cancer); secondary
UEDVT accounts for 75 to 80% of all cases.
UEDVT may involve the subclavian, axillary or brachial veins. Clinical manifestations include edema, dilated collateral veins over the arm, neck, or chest, and limb pain or discoloration. The disease may lead to complications, including pulmonary embolism (estimated to occur in up to one third of patients),recurrent UEDVT.
a prospective study reported cumulative incidence rates of 2.0%, 4.2% and 7.7% after 1, 2, and 5 years, respectively) and PTS of the arm. The treatment of patients with acute UEDVT may be divided into the initial treatment phase (with anticoagulants, thrombolytic therapy, catheter/surgical techniques, or filter placement) and longtermlongterm treatment (or secondary prophylaxis) with anticoagulants to prevent recurrent VTE.
IV UFH or LMWH for the Initial Treatment of UEDVT
It is generally accepted that, as for patients with lower-limb DVT, patients with UEDVT require treatment with anticoagulants to prevent thrombus extension and PE .To date, no RCTs have evaluated UFH, LMWH, or other anticoagulants for the initial treatment of UEDVT.Several small prospective cohort studies have reported low rates of recurrent DVT, PE, and major bleeds using treatment regimens for UEDVT similar to those for patients with lower-limb DVT .
In a prospective two-center cohort study, 46 outpatients with UEDVT were treated with SC LMWH followed by warfarin. At 3 months, there was one recurrence, one major bleed, and no episodes of PE. In 36 inpatients with UEDVT, LMWH twice daily for up to 7 days followed by warfarin for an average of 5 months (target INR, 2.0 to 2.5) led to significant early symptom relief and no recurrent DVT or PE at 1 year.
Rates of VTE recurrence were similarly low in a cohort of 53 patients who received UFH or LMWH for the initial treatment of UEDVT followed by warfarin for 3 months, and in 74 cancer patients with central venous catheter-associated UEDVT, in whom treatment with LMWH for 5 to 7 days followed by warfarin for 3 months appeared to prevent catheter failure and was not associated with any recurrent VTE.
Recommendation
For patients with acute UEDVT, werecommend initial treatment with therapeutic doses of LMWH, UFH, or fondaparinux as described for leg DVT [Grade 1C].
Thrombolytic Therapy for the Initial Treatment of UEDVT
No randomized controlled studies have evaluated the efficacy and safety of thrombolytic therapy compared with standard anticoagulation for the initial treatment of patients with UEDVT.A number of retrospective and small prospective studies that included 6 to 118 patients have evaluated streptokinase, urokinase,or rT-PA administered with varying doses, methodsof administration (IV, catheter directed), andinfusion durations.
Three of these studies included control groups that received anticoagulation alone. In some studies, a few patients additionallyhad venous angioplasty or surgical decompression.
In the largest of the studies, 118 consecutive patients with UEDVT were assessed retrospectively.At a median of 40 months of follow-up,venous patency on ultrasound was noted in 65% of patients who had been treated with IV urokinase compared with 20% of patients treated with standard anticoagulants; however, the rates of recurrent VTE were similar in the two groups and the lysis group had a 15.2% rate of bleeding, compared with no bleeds in the anticoagulant group, a difference that was highly statistically significant.
In the largest of the prospective studies, among 35 patients with primary UEDVT treated with CDT followed by warfarin for a mean of 5 months,the rate of ipsilateral UEDVT recurrence at 54 months of follow-up was substantial at 23%.
To summarize the heterogeneous, low-to-moderate quality data available, some studies report good-to-excellent success of thrombolytic therapy in terms of early and late venous patency. However, for important clinical end points such as PE, recurrent VTE, bleeding, and PTS, it is not known if initial thrombolytic therapy is, on balance,superior or inferior to nticoagulant therapy, or whether one thrombolytic approach is better or worse than another, as no prospective, controlled comparisons have been performed.
Recommendations
For most patients with acute UEDVT, we
recommend against the routine use of systemic
or catheter-directed thrombolytic therapy
(Grade 1C).In selected patients with acute UEDVT(eg, those with a low risk of bleeding and
severe symptoms of recent onset), we suggest
that CDT may be used for initial treatment if
appropriate expertise and resources are available (Grade 2C).
Catheter Extraction, Surgical Thrombectomy,
Transluminal Angioplasty, Stent Placement, Staged Approach of Lysis Followed by Interventional or Surgical Procedure, SVC Filter Insertion, for the Initial Treatment of UEDVT.A number of reviews have advocated staged, multidisciplinary approaches to the management of primary UEDVT that involve thrombolysis and angioplasty or stent placement, followed by early or late surgical decompression of the thoracic outlet. However, data on the efficacy and safety of these approaches are limited.
SVC filters have been used in small series of
patients with contraindications to or failure ofanticoagulant therapy. In a prospective
studyof 41 patients with UEDVT who had SVC
filters placed, the rates of PE and PTS during
long-term follow-up were 2.4% and 0%, respectively.
In a retrospective series364 of 72 patients
with SVC filters, there were no episodes of PE or SVC thrombosis during long-term follow-up.
Recommendations
For most patients with acute UEDVT, we recommend against the routine use of catheter extraction, surgical thrombectomy, transluminal angioplasty, stent placement, staged approach of lysis followed by interventional or surgical procedure, or SVC filter placement (Grade 1C)..
In selected patients with acute UEDVT (eg, those with primary UEDVT and failure of
anticoagulant or thrombolytic treatment who that catheter extraction, surgical thrombectomy,transluminal angioplasty, or a staged approach of lysis followed by a vascular interventional or surgical procedure may be used if appropriate expertise and resources are available (all Grade 2C).In selected patients with acute UEDVT (eg, those in whom anticoagulant treatment is contraindicated and there is clear evidence of DVT progression or clinically significant PE), we suggest placement of an SVC filter (Grade 2C).
Anticoagulants for the Long-term Treatment of UEDVT
There are no randomized studies of duration orintensity of long-term anticoagulation for the prevention of recurrent VTE in patients with UEDVT. There is general agreement that, as for patients with lower-extremity DVT, patients with symptomatic acute DVT of the upper extremity require long-term treatment with anticoagulants following initial treatment, and that a similar process as for lowerextremity DVT should be used to determine the optimal duration of anticoagulation. However,there is little evidence to support indefinite anticoagulant therapy for a first unprovoked UEDVT.
In prospective cohort studies of the treatment of UEDVT, patients received VKA (target INR, 2.5; range, 2.0 to 3.0) for periods of 3 to 6 months or longer. Similar regimens were reported in retrospective studies. No data are available regarding the long-term use of LMWH monotherapy or newer anticoagulants, such as fondaparinux, for the long-term treatment of UEDVT.
Recommendations
For patients with acute UEDVT, we recommend treatment with a VKA for > 3 months (1C).Remark: A similar process as for lower-extremity DVT should be used to determine the optimal duration of anticoagulation. For most patients with UEDVT in association with an indwelling central venous catheter,we suggest that the catheter not be removed if it is functional and there is an ongoing need for the catheter (Grade 2C).
For patients who have UEDVT in association with an indwelling central venous catheter that is removed, we do not recommend that the duration of long-term anticoagulant treatment be shortened to < 3 months (Grade 2C).
Prevention of PTS of the Arm
PTS of the arm occurs in 15 to 25% of patientsafter treated UEDVT. Upper-extremity PTS is a potentially disabling condition that adversely affect QOL, particularly if the dominant arm is involved.384 To date, no controlled studies have evaluated the effectiveness of elastic bandages, compression sleeves, or venoactive drugs to prevent PTS after UEDVT.
Recommendation
For patients at risk for PTS after UEDVT,
we do not suggest routine use of elastic compression or venoactive medications (Grade 2C).
Treatment of PTS of the Arm
Symptoms of PTS of the arm include swelling,heaviness, and limb fatigue with exertion. No
controlled studies have evaluated the effectiveness of elastic bandages, compression sleeves (as are used for lymphedema), or venoactive drugs to treat PTS after UEDVT.
Recommendation
In patients with UEDVT who have persistentedema and pain, we suggest elastic bandages or elastic compression sleeves to reduce symptoms of PTS of the upper extremity (Grade 2C).
September 7, 2010 (Stockholm, Sweden)
A host of new recommendations for the management of atrial fibrillation are included in the latest guidelines on the subject, issued last week at the European Society of Cardiology (ESC) 2010 Congress by the ESC.Chair of the ESC task force for the management of AF, Dr A John Camm (University of London, UK), told heartwire that this is the first time that the Europeans have produced independent advice on AF; the previous guidelines were collated in conjunction with the AHA and ACC four years ago.Highlights of the new recommendations include the introduction of a symptom score for AF; the addition of "long-standing persistent AF" as a patient category; the adoption of risk profiling to assess who will benefit most from new anticoagulants to prevent stroke; new guidance in the area of rate control; advice on how to use the antiarrhythmic drug dronedarone (Multaq, Sanofi-Aventis); formal indications for the use of ablation therapy; recommendations on "upstream" therapies to prevent the deterioration of AF; and advice on certain "special situations."
"
We estimate that around 1% to 2% of the population are affected by AF; it has become an epidemic," said Camm. "And this figure is expected to at least double, in line with the demographics of an aging population, because the condition is particularly prevalent among older people. We needed to create contemporary guidelines because of new drug therapies that are available and because of accumulating evidence on how to refine treatment regimens to obtain the best outcomes," he added.
Asked by heartwire to comment on the new guidelines, Dr Gabriel Steg (Hôpital Bichat-Claude Bernard, Paris, France), who was not involved in drafting them but who last week reported preliminary data from a new registry of more than 10 000 patients with atrial fibrillation, REALISE-AF, said: "These new recommendations appear simpler and more pragmatic. I hope having this approach will help popularize the guidelines, because I can understand that cardiologists and GPs might have had trouble remembering the complex algorithms for decision-making used in the past. We're moving in the right direction."
All New: EHRA Symptom Score, Another Category for AF, Risk Profiling .These new recommendations appear simpler and more pragmatic. We're moving in the right direction. In an interview with heartwire , Camm outlined how the new guidelines--developed together with the European Heart Rhythm Association (EHRA) and endorsed by the European Association for Cardio-Thoracic Surgery (EACTS)--differ from the last recommendations on the management of AF, issued in 2006.
A third development was to establish better risk profiles for assessing the likelihood of stroke in patients with AF, he said. AF confers a fivefold increase in the risk of stroke if left untreated and a doubling of the risk of death from such strokes.
These changes have been made in anticipation that we are going to get safer and more effective anticoagulants soon.
Included is some refinement with regard to use of the CHADS2 score, with the advent of a new, "more sensitive system" called CHADS2-VASc, said Camm.
"Although CHADS2 is easy to remember, it doesn't pick up some of the people who are in need of anticoagulation, so we've added in other risk factors," he explained. These include additional score points for specific age categories and for the presence of vascular disease and female gender. Also linked to this is a new score, HAS-BLED, for assessing bleeding risk. "These changes have been made in anticipation that we are going to get safer and more effective anticoagulants soon," he said.
Camm was referring to new oral anticoagulants for stroke prevention in AF that could be approved in coming months. The furthest ahead is the direct thrombin inhibitor dabigatran (Pradaxa, Boehringer Ingelheim), which is due to be considered by a US FDA advisory committee on September 20, 2010 for the prevention of stroke in patients with AF, based on the RE-LY megastudy.
Also in similar trials are the factor Xa inhibitors, rivaroxaban (Xarelto, Bayer/Johnson & Johnson) which is currently being tested for stroke prevention in the ROCKET-AF study, due to be reported at the American Heart Association meeting in November, and apixaban (Bristol-Myers Squibb/Pfizer), in a similar trial, called ARISTOTLE, with results expected next year. Another trial presented last week at the ESC meeting, AVERROES, showed that patients with atrial fibrillation and unable to take warfarin who were given apixaban had a significantly lower risk of stroke and systemic embolic events compared with similar patients treated with aspirin.
Changes to Rate and Rhythm Control, Formal Acceptance of Ablation
Another focus of the new guidelines is the recognition that AF is treated not only by cardiologists but also by specialists from many other branches of medicine, including geriatricians and primary-care doctors, said Camm, "So we have provided guidance for all levels of patient management.".
In regard to rate control, Camm said: "We have introduced the notion that lenient rate control--that is, a resting heart rate of <110 bpm--is satisfactory and that we don't need to get resting heart rate to <80 bpm." This recommendation has been made on the basis of the RACE-2 trial, reported earlier this year, he noted.
For rhythm control, the guidelines incorporate the new antiarrhythmic drug dronedarone, which was approved by the European Medicines Agency at the end of last year, into the recommendations. "We're saying, from a benefit/risk point of view, that dronedarone is widely applicable," said Camm
Catheter ablation also gains a stronger footing as a treatment for AF in the new European guidelines. "We've given a formal indication for ablation therapy, which was implied but not formally recommended in the previous 2006 guidelines," Camm said. "Potentially provocative" is the suggestion that patients may have an ablation without previous trials of antiarrhythmic drugs if they have paroxysmal AF, no prior heart disease, or are unwilling to take antiarrhythmics, he says.
European Society of Cardiology (ESC) Congress 2010
The task force also attempts to give advice on a number of "special situations." For example, in athletes with AF, it is recognized that treatment with drugs is often difficult, Camm noted, "so we've suggested ablation or a pill-in-the pocket approach, whereby the athlete takes an antiarrhythmic drug only if he or she has AF."
Finally, the recommendations give updated advice on so-called "upstream" therapy that may be prescribed in an attempt to prevent the deterioration of AF, covering the use of ACE inhibitors, angiotensin-receptor blockers (ARBs), and statins.
Lung Imaging Might Not Be Beneficial for Diagnosis of Pulmonary Embolism
A decision analysis led to the surprising conclusion that health outcomes would be maximized and costs minimized by eliminating lung imaging altogether.Investigators constructed a decision model to determine the most cost-effective diagnostic strategy for pulmonary embolism (PE). They evaluated 60 strategies that differed according to tests used, test order, and values of numerous parameters (e.g., cutoff for a "normal" D-dimer result).
Published in Journal Watch Emergency Medicine October 1, 2010
The diagnostic tests were D-dimer measurement, lower-extremity compression ultrasonography, computed tomography (CT) pulmonary angiography, and ventilation-perfusion scanning. The analysis relied on numerous assumptions, most importantly that 1.96% of patients tested for PE actually had PE.
The most cost-effective strategy was as follows:
(1) Categorize risk using Wells score modified by whether deep venous thrombosis is clinically evident;(2) measure D-dimer, using different cutoffs for different risk categories;
(3) if D-dimer negative, PE is ruled out; if D-dimer positive, perform compression ultrasonography;
(4) if ultrasound negative, PE is ruled out; and
(5) if ultrasound positive, PE is ruled in; treat with no further testing.
The advantage of the preferred strategy was slight. Chest CT or ventilation-perfusion scanning to prove that PE is present or absent would not add benefit (but would add cost); this finding did not change when assumptions were varied across their plausible ranges in sensitivity analyses, even with a PE prevalence as high as 11%.
Comment: This paper challenges existing practice by suggesting that pulmonary imaging is slightly counterproductive in the diagnostic work-up of pulmonary embolism. Remarkably, the authors reached this conclusion even though they accounted for the cost of malpractice suits for missed PE. If a prospective trial validates the safety and effectiveness of this approach, a substantial reduction in chest CT scanning could ensue.
Recommendation for Use of Oral Direct Thrombin Inhibitor Anticoagulant Agents
Dabigatran etexilate is a prodrug that is rapidly converted to the active direct thrombin (factor IIa) inhibitor dabigatran.This conversion is independent of cytochrome P-450, making drug-drug and drug-diet interactions less likely. Dabigatran is predominantly excreted via a renal pathway.
Dabigatran was evaluated in a large, open-label, randomized trial (RE-LY) in
which it was compared with warfarin (goal international normalized ratio [INR] 2.0 to 3.0) in 18 113 patients with nonvalvular AF.Dabigatran was administered in fixed doses
without laboratory monitoring of anticoagulation intensity. Eligible participants had at least 1 risk factor for stroke (previous stroke or transient ischemic attack or systemic embolism, left ventricular ejection fraction <40% or symptomatic heart failure [New York Heart Association class II or higher in the last 6 months], hypertension, age≥75 years, or age 65 to 74 years with either diabetes mellitus or coronary artery disease). Exclusion criteria in RE-LY includeda prosthetic heart valve or hemodynamically significant valvular heart disease, disabling or recent stroke, recent or pending
surgery, recent or known bleeding disorders, uncontrolled hypertension, need for anticoagulation of disorders other than
AF, planned ablation or surgery for AF, reversible causes of AF, severe renal dysfunction (creatinine clearance<30 mL/min), active liver disease, or pregnancy.
Two doses of dabigatran (110 mg and 150 mg twice daily) were evaluated.The mean age of participants was 71 years, 63.6% were male, half had prior long-term therapy with vitamin K antagonists,and the mean CHADS2 (Congestive heart failure, Hypertension, Age, Diabetes, prior Stroke) risk prediction score was 2.1. The primary outcome was all stroke (ischemic or hemorrhagic) or systemic embolism; safety outcomes included bleeding, liver dysfunction, and other adverse events.
Results of the RE-LY trial were published in 2009.Rates for the primary outcome of all stroke (ischemic or hemorrhagic) or systemic embolism were 1.71% per year in the warfarin group.Dabigatran etexilate, 150 mg twice daily, reduced the rate by 34% (to 1.11% per year; P0.001 for superiority; RR: 0.65; 95% CI:
0.52 to 0.81), and at this dose there was no increase in major bleeding.
Dabigatran etexilate, 110 mg twice daily, was also associated with a rate of stroke and systemic embolism (1.54% per
year) that was noninferior to warfarin (P0.001 for noninferiority; RR with dabigatran: 0.90; 95% CI: 0.74 to 1.10), and at this dose
there was a 20% reduction in major bleeding risk compared with warfarin (P=0.003 for superiority).
Rates of major bleeding were 3.57% per year for patients taking warfarin, 2.87% per year for those on dabigatran 110 mg twice daily (P=0.003), and 3.32% per year for those on dabigatran 150 mg twice daily (P=0.32). In the warfarin group, INR values were within the target range 64.4% of the time.
In addition, the results showed other secondary benefits and
In addition, the results showed other secondary benefits and adverse outcomes. For safety, both doses showed a reduction in life-threatening, intracranial, and total bleeding, including lower rates of intracerebral hemorrhage with both 150 mg and 110 mg twice-daily doses (from 0.38% per year in the warfarin group to 0.12% per year with dabigatran 110 mg twice daily [P<0.001] and 0.10% per year with dabigatran 150 mg twice daily [P<0.001]).
Dyspepsia occurred more frequently with dabigatran (11.8% and 11.3% of patients in the low-dose [110 mg] and high-dose [150 mg] groups, respectively) compared to warfarin (5.8% of patients). Also, myocardial infarction was more frequent with dabigatran and occurred at rates of 0.82% (RR: 1.29; 95% CI: 0.96 to 1.75; P=0.09) and 0.81% (RR: 1.27; 95% CI: 0.94 to 1.71; P=0.12) with dabigatran 110 mg and 150 mg twice Increased or decreased
rates of myocardial infarction have been reported with other oral thrombin inhibitors in different patient populations; however, the increase in myocardial infarction seen in RE-LY was not statistically significant in the dabigatran groups.
In RE-LY, dabigatran did not cause hepatotoxicity. Drug discontinuation rates were slightly higher in the dabigatran groups compared with warfarin. There was no difference in mortality with dabigatran compared with warfarin. Both dabigatran doses appeared to be noninferior to warfarin with respect to the primary efficacy outcome of stroke or systemic embolism. In addition, the 150-mg twice– daily dose was superior to warfarin with respect to stroke or systemic embolism, and the 110-mg twice– daily dose was superior to warfarin with respect to majorbleeding.
There is no specific antidote for dabigatran, which has a half-life of 12 to 17 hours. Supportive therapy for severe
hemorrhage may include transfusions of fresh-frozen plasma, packed red blood cells, or surgical intervention if appropriate.
Because of the twice-daily dosing and greater risk of
nonhemorrhagic side effects with dabigatran, patients already taking warfarin with excellent INR control may have little to gain by switching to dabigatran. Selection of patients with AF and at least 1 additional risk factor for stroke who could benefit from treatment with dabigatran as opposed to warfarin
should consider individual clinical features, including the
ability to comply with twice-daily dosing, availability of an anticoagulation management program to sustain routine monitoring of INR, patient preferences, cost, and other factors.
Dabigatran etexilate was approved by the FDA on October 19, 2010, for marketing in the United States for the prevention of stroke and systemic embolism in patients with nonvalvular AF. A dose of 150 mg twice daily was approved for patients with a creatinine clearance>30 mL/min, whereas in patients with severe renal insufficiency (creatinine clearance 15 to 30 mL/ min) the approved dose is 75 mg twice daily, a dose currently marketed in the European Union but not evaluated in the RE-LY trial.
There are no dosing recommendations for patients with creatinine clearance <15 mL/min or patients on dialysis. The 110-mg twice– daily dose used in the RE-LY trial did not receive FDA approval. The approval requires distribution of a medication guide with each prescription that details the risk of serious bleeding in patients receiving dabigatran in this open-label (or “unblinded”) trial. Dabigatran is the first new oral anticoagulant to become available for clinical use in>50 years.
With several oral anticoagulants encroaching on likely FDA review for approval for the AF indication, dabigatran is for the time being the only available warfarin alternative in AF. Many patients and clinicians find warfarin difficult to manage and are welcoming another oral anticoagulation option.
But the new statement cautions that warfarin may still be appropriate for some patients. "Because of the twice-daily dosing and greater risk of nonhemorrhagic side effects with dabigatran, patients already taking warfarin with excellent [international normalized ratio] INR control may have little to gain by switching to dabigatran," it states.
Abciximab is made from the Fab fragments of an immunoglobulin that targets the glycoprotein IIb/IIIa receptor on the platelet membrane.
is a platelet aggregation inhibitor mainly used during and after angioplasty to prevent platelets from sticking together and causing thrombus. Its mechanism of action is inhibition of glycoprotein IIb/IIIa.
In practice, platelet aggregation gradually returns to normal about 24 to 48 hours after discontinuation of the drug. While Abciximab has a short plasma half life, due to its strong affinity for its receptor on the platelets, it may occupy some receptors for weeks Abciximab has a plasma half life of about ten minutes, with a second phase half life of about 30 minutes. However, its effects on platelet function can be seen for up to 48 hours after the infusion has been terminated, and low levels of glycoprotein IIb/IIIa receptor blockade are present for up to 15 days after the infusion is terminated.
Many of the side effects of abciximab are due to its anti-platelet effects. This includes an increased risk of bleeding. The most common type of bleeding due to abciximab is gastrointestinal hemorrhage.
Thrombocytopenia is a rare but known serious risk. Abciximab-induced thrombocytopenia can typically be treated with transfusion of platelets. Abciximab induced thrombocytopenia can last for five days after initial drug administration. Transfusing platelets is the only known treatment and may have limited effectiveness as the drug may also bind to the new platelets. Platelet counts which should average 250,000-400,000 can effectively drop to zero
ReoPro is a clear, colorless, sterile, non-pyrogenic solution for intravenous (IV) use.
Each single use vial contains 2 mg/mL of Abciximab in a buffered solution (pH 7.2) of 0.01 M sodium phosphate, 0.15 M sodium chloride and 0.001% polysorbate 80 in Water for Injection. No preservatives are added.
Abciximab is indicated as an adjunct
to patients undergoing percutaneous coronary interventionin patients with unstable angina not responding to conventional medical therapy when percutaneous coronary intervention is planned within 24 hours
Safety and efficacy of Abciximab use in patients not undergoing percutaneous coronary intervention have not been established.
Abciximab is intended for use with aspirin and heparin and has been studied only in that setting, as described in CLINICAL STUDIES.
The safety and efficacy of Abciximab have only been investigated with concomitant administration of heparin and aspirin as described in Clinical Studies. In patients with failed PCIs, the continuous infusion of Abciximab should be stopped because there is no evidence for Abciximab efficacy in that setting.
In the event of serious bleeding that cannot be controlled by compression, Abciximab and heparin should be discontinued immediately.
The recommended dosage of Abciximab in adults is a 0.25 mg/kg intravenous bolus administered 10-60 minutes before the start of PCI, followed by a continuous intravenous infusion of 0.125 µg/kg/min (to a maximum of 10 µg/min) for 12 hours.
Patients with unstable angina not responding to conventional medical therapy and who are planned to undergo PCI within 24 hours may be treated with an Abciximab 0.25 mg/kg intravenous bolus followed by an 18- to 24-hour intravenous infusion of 10 µg/min, concluding one hour after the PCI.
Hypersensitivity reactions should be anticipated whenever protein solutions such as Abciximab are administered. Epinephrine, dopamine, theophylline, antihistamines and corticosteroids should be available for immediate use. If symptoms of an allergic reaction or anaphylaxis appear, the infusion should be stopped and appropriate treatment given .
Therapeutic Potential of Oral Factor Xa Inhibitors
Venous thromboembolism is the third leadingcause of cardiovascular death, after myocardial
infarction and stroke. Total hip or knee arthroplasty is the procedure with the highest risk of venous thromboembolism.
two studies affirm and extend the efficacy
and safety of the novel oral factor Xa inhibitors,
rivaroxaban and apixaban, in the management of venous thromboembolic disease.
NEJM december 23, 2010
Unlike the case with warfarin, drug elimination in the case of the factor Xa inhibitors involves multiple pathways.
The degree of renal clearance is 66% in the case of rivaroxaban, 25% in the case of apixaban, and 35% in the case of edoxaban. As compared with warfarin’s half-life of 20 to 60 hours, the respective half-lives of these agents are 7 to 11 hours, 12 hours, and 9 to 11 hours.
The shorter halflife of these agents may improve their overall safety profile but, conversely, will also result in the drugs’ providing less protection if doses are missed. All these drugs are metabolized to different degrees by cytochrome P-450 3A4 (CYP3A4) and are substrates for P-glycoprotein. Therefore, the concomitant use of drugs that inhibit both pathways, such as azole antifungal agents or protease inhibitors, is contraindicated.
The potential impact of these oral,highly specific, fixed-dose drugs that do not require routine monitoring will no doubt be substantial. It is conceivable that the oral factor Xa inhibitors, as compared with warfarin, will prove to be safer in clinical practice because they are administered in fixed doses, do not interfere
with diet, and have fewer interactions with other
drugs.
In one study, 3449 patients with acute symptomatic proximal deep venous thrombosis (DVT) — but without clinically apparent pulmonary embolism — were randomized to receive either oral rivaroxaban or standard therapy (enoxaparin followed by warfarin); treatment duration was 3 to 12 months. The incidence of recurrent venous thromboembolism was slightly lower with rivaroxaban than with standard therapy (2.1% vs. 3.0%), and the incidence of bleeding was the same in both groups.
In another study, 1197 patients who had completed 6 to 12 months of treatment for acute venous thromboembolism were randomized to receive either oral rivaroxaban or placebo for 6 to 12 additional months. Recurrent venous thromboembolism occurred significantly less often with rivaroxaban than with placebo (1.3% vs. 7.1%); DVT accounted for most of the difference. Rivaroxaban recipients experienced fewer pulmonary embolic events than did placebo recipients (3 vs. 14) but suffered more major bleeding episodes (4 vs. 0).
In conclusion, oral rivaroxaban, at a dose of
15 mg twice daily for the first 3 weeks, followedby 20 mg once daily thereafter, without the need
for laboratory monitoring, may provide an effective,
safe, single-drug approach to the initial and
continued treatment of venous thrombosis.
Apixaban with Antiplatelet Therapy
after Acute Coronary SyndromeThe trial was terminated prematurely after recruitment of 7392 patients because of an increase in major bleeding events with apixaban in the absence of a counterbalancing reduction in recurrent ischemic events.
Conclusions
The addition of apixaban, at a dose of 5 mg twice daily, to antiplatelet therapy in highrisk patients after an acute coronary syndrome increased the number of major bleeding events without a significant reduction in recurrent ischemic events.
nejm.708 org august 25, 2011
Time to reconsider NICE guidance on heparin
prophylaxis in medical inpatients
Domnick Felix D’Costa consultant physician
Royal Wolverhampton Hospital, Wolverhampton WV10 0QP, UK
The recent clinical practice guideline on venous
thromboembolism prophylaxis from the American College of
Physicians indicates that for every 1000 patients treated the
absolute benefit is a reduction of three pulmonary embolisms but with an absolute increase of nine haemorrhages, four of them major.
BMJ 6 December 2011
There is thus no net benefit and no significant
reduction in mortality.Are we as doctors thus unwittingly doing medical inpatients
more harm than good in prescribing heparin prophylactically
according to diktat? We probably do more harm, particularly
in patients staying longer than two weeks because they receive
heparin for longer than the two weeks used in trials. Our
anecdotal experience has been an increase in haemorrhages.
Perhaps an open debate or an editorial in the BMJ is needed to
raise awareness among doctors lest we fail on the first principle
of the practice of medicine: primum non nocere