
Urinary Imaging
Dr. Khaleel Ibraheem
Techniques
Ultrasound
INDICATIONS:
1. First investigation in suspected UT pathology.
2.
Follow up for renal size in CRF , scarring in children with UTI, transplanted kidney &
possible complication
3.
Assess the presence & the cause, if possible of hydronephrosis in non-functioning kidney.
4.
Evaluate tumors, cysts, abscess.
5.
Guide percutaneous procedures.
6.
Assess renal blood flow by Doppler US.
7.
Assess the bladder & prostate.
Normal US:
1. Size (9-12 cm), there may be a difference between the two kidneys of < 1.5 cm.
2. Smooth outlines
3. Central echogenic area (PCS ,blood vessels & surrounding fat ) : renal sinus echo
4. The cortical echoes are less than that of liver & spleen
5. Pyramids appear as triangular structures of low echo texture
6. Ureters not visualized normally
7. UB: sharp walls , < 3 mm in distended state , < 5 mm in partially filled state
X-Ray
1-Bolus IVP
Indications:
1. When detailed demonstration of PC system & ureters is required.
2. Suspected ureteric colic.
3. Investigation of renal calculi.
4. Investigation of hematuria.

Procedure
1. plain : full length -Kidney, ureter, bladder (KUB)-
to assess
radiopaque shadows overlying
the renal, ureteric or vesical regions ,and to assess bone & soft tissue abnormalities
2. Inject of iodinated contrast
3. 1-min(nephrogram) and 5-min film(pyelogram) of both kidneys
4. 10-min KUB
5. postvoiding film.
What to see in IVP
The renal size
1. adult's kidney measures 10-16 cm
2. A difference of 1.5 cm is acceptable between the two sites
3. A kidney with bifid collecting system is usually 1-2 cm larger than normal
The renal position
1. Rt. K.is lower than the Lt.K.
2. The renal axis is parallel to the psoas muscle (abnormal axis in malrotation or displacement
of the kidney )
3. Abnormal position (ectopic, displaced by mass, nephroptosis, transplanted K.)
The renal outlines
1. Renal parenchymal width should be symmetrical & uniform , renal cortex measurement (1.5-
2 cm ) except at the poles
2. Minor indentation as in Persistence of fetal lobulation
3. Significant indentations particularly if opposite a calyx (CH. PN, TB , Renal infarction)
4. Local bulge of renal outlines usually due to mass lesion , an important normal variant is the
“splenic (Dromedary) hump”
The calices
1. Normal calices are cup shape, evenly distributed & fairly symmetrical.
2. Dilated calyx is clubbed in shape
3. Causes of dilatation
a. obstruction (with hold up & dilatation down to a specific point)
b. papillary destruction (CH.PN, TB, papillary necrosis)
The renal pelvis:
Should be funnel shaped, could be intra or extra renal in location
The ureters
1. Only portion of the ureter is seen due to peristalsis
MRI used in selected cases of
renal artery stenosis (MRA) &
assess possible extension of
tumor into IVC (MRV)
2. Diameter =<7 mm
3. Course: along the transverse processes of the lumbar vertebrae.
4. Dilatation of the renal pelvis & ureter can occur in obstruction, congenital variant, and VU
reflux).
5. Look for filling defects (tumors, stones, blood clot).
6. Commonest congenital variant is bifid collecting system.
The UB
1. Smooth outlines
2. May show indentation on the superior aspect from the uterus or sigmoid colon
3. Post voiding residue should be small
2.Retrograde & antegrade pyelography:
Direct injection of contrast into PC system or ureters through catheters placed via cystoscopy
(retrograde pyelography) or percutaneously (antegrade pyelography). The main indication is
to confirm a possible transitional cell carcinoma.
3.Voiding cystourethrography:
The bladder is filled with contrast through a catheter & films are taken during voiding to
identify vesicoureteric reflux or urethral valves.
4.Urethrography:
For full visualization of the male urethra, an ascending urethrogram with contrast injection via
the external urethral meatus is necessary. The usual indications are the identification of
urethral strictures & to demonstrate extravasation from urethra or bladder neck
following trauma.
CT & MRI
Used for further assessment of certain situations that were diagnosed by US or IVP
CT has advantage over MRI
in showing calcifications &
stones that MRI usually miss
1. To characterize renal masses & staging renal
tumors.
2. To delineate vascular anatomy.
3. To diagnose or exclude renal trauma.
4. To demonstrate radiolucent stones.
5. To assess acute ureteric colic.

Radionuclide scanning
For assessment of renal scarring & renal function
Nephrocalcinosis and Lithiasis
Renal calcifications can be located in renal parenchyma (nephrocalcinosis), in abnormal tissue
(e.g., dystrophic calcification in cysts, tumors), or in the collecting system (e.g., nephrolithiasis,
calculi).
Calculi
The radiographic density of a calculus depends mainly on its calcium content , Calcium
calculi (opaque), 75%,while Struvite calculi (opaque), 15%
Nonopaque calculi include: Uric acid, Xanthine, Mucoprotein matrix calculi and
Protease inhibitor indinavir used in HIV treatment can result in radiolucent stones.
Three narrow sites in the ureter at which calculi often lodge
UPJ: junction of renal pelvis and ureter proper
At crossing of ureter with iliac vessels
Ureterovesical junction (UVJ): insertion of ureters into bladder
Imaging Features:
Radiopaque calculus, 90% of plain film
Radiolucent calculi are best detected by IVP,IVP also shows
1. Delayed and persistent ,dense nephrogram(caused by concentrated non excreted
contrast) due to
acute
ureteral obstruction
2. Column of opacified urine extends in ureter from renal pelvis to lodged calculus
(diminished or absent peristalsis).
3. Ureter distal to calculus is narrowed (edema, inflammation); may create false impression
of stricture.
4. Ureter proximal to calculus is minimally dilated and straightened: columnization; degree
of dilatation has no relation to stone size.
5.
In intermittent obstruction
, IVP may be normal between attacks, but a normal IVP
taken during an episode of acute pain effectively excludes ureteric colic as the cause of
pain.
Renal calculi can be detected by US: hyperechoic focus (calculus), posterior shadowing;
calculi 3 mm or less may not be detected.
• CT detects most calculi regardless of calcium content. The exceptions are matrix stones.
Cortical nephrocalcinosis
Peripheral or tramline calcifications seen in plain film or CT (medullary pyramids are spared)
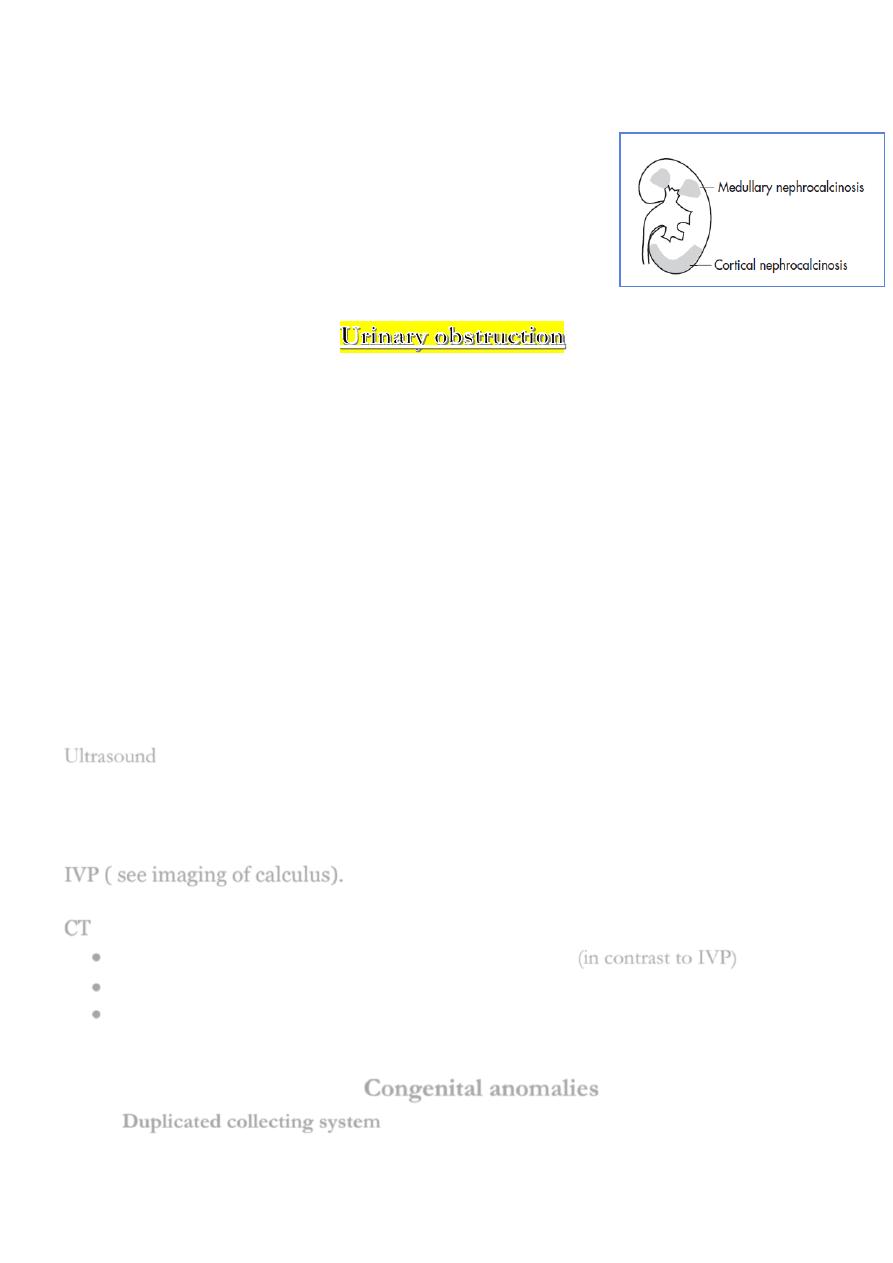
Medullary nephrocalcinosis
Causes : Hyperparathyroidism (hypercalciuria, hypercalcemia),40%
• Renal tubular acidosis, 20%
• Medullary sponge kidney, 20%
Plain film and CT shows Bilateral, stippled calcification of medullary pyramids
The principal feature is dilatation of PC system & ureters.
The primary imaging techniques used are US & IVU, CT can be used
causes are:
1. Stones
2. Tumors (TCC of renal pelvis, ureter, bladder )
3. Blood clot ,sloughed papilla (rare)
4. Strictures, surgical ligation of the ureter
5. Congenital: PUJ obstruction, posterior urethral valve
6. Enlarged prostate
7
.
Compression from adjacent retroperitoneal structures or masses (aberrant vessel ,
retroperitoneal LAP, retroperitoneal fibrosis )
Ultrasound
Shows splaying of the renal sinus fat due to dilatation of PCS, the proximal ureter
and vesicoureteric junction can be easily identified but the mid ureter is usually
obscured by overlying bowel.
IVP ( see imaging of calculus).
CT
identify very small stones regardless of their consistency
(in contrast to IVP)
stone situated in the mid (better than ultrasound) or distal ureter
show & stage ureteric tumors or an external tumors causing compression that are usually
missed in IVP
Congenital anomalies
Duplicated collecting system
Bifid Renal Pelvis
:
One pelvis drains upper pole calyces; the other drains the middle
and lower pole calyces. The two pelvises join proximally to the ureteropelvic junction
(UPJ). Incidence: 10% of population
Incomplete Ureteral Duplication :Duplications join distal to UPJ and proximal to
bladder:
Y-shaped ureters. No complications.
Complete Ureteral Duplication : duplication of renal pelvis ,ureters down to bladder
,upper pelvis ureter had ectopic insertion and liable for obstruction and ureterocele
,while the lower pelvis ureter is inserted normally and liable for reflux.
Ectopic kidney
Usually in the lower abdomen & rotated so that the pelvis points forwards with short ureter, in
some cases, both lie on same side of pelvis & fused. hydronephrosis & stones are more
common in ectopic kidneys. Diagnosed by easily by US or IVP.
Horseshoe kidney
The two kidneys are connected across the midline by an isthmus. This is the
most common
fusion anomaly (other fusion anomalies: cross-fused ectopia, pancake kidney). The isthmus
may contain parenchymal tissue with its own blood supply or consist of fibrous tissue.
Polycystic kidney disease
IVU show bilaterally enlarged kidneys with stretching & distortion of the calices.
Renal agenesis
The other kidney show compensatory hypertrophy
Inflammation
Acute pyelonephritis
Indication of imaging
1. After first attack of UTI in male child
2. after second attack of UTI in female child
3. repeated infection
4. Sever ureteric colic
Imaging studies (IVP, CT, US) are normal in 75%. In the remaining 25%, there are nonspecific
findings:
• Renal enlargement (edema)
• Loss of the corticomedullary differentiation
(edema)
• IVP findings: Delay of contrast excretion
Narrowing of collecting system (edema)
Striated nephrogram
• Areas of decreased perfusion by contrast enhanced CT
• Complications: abscess, scarring
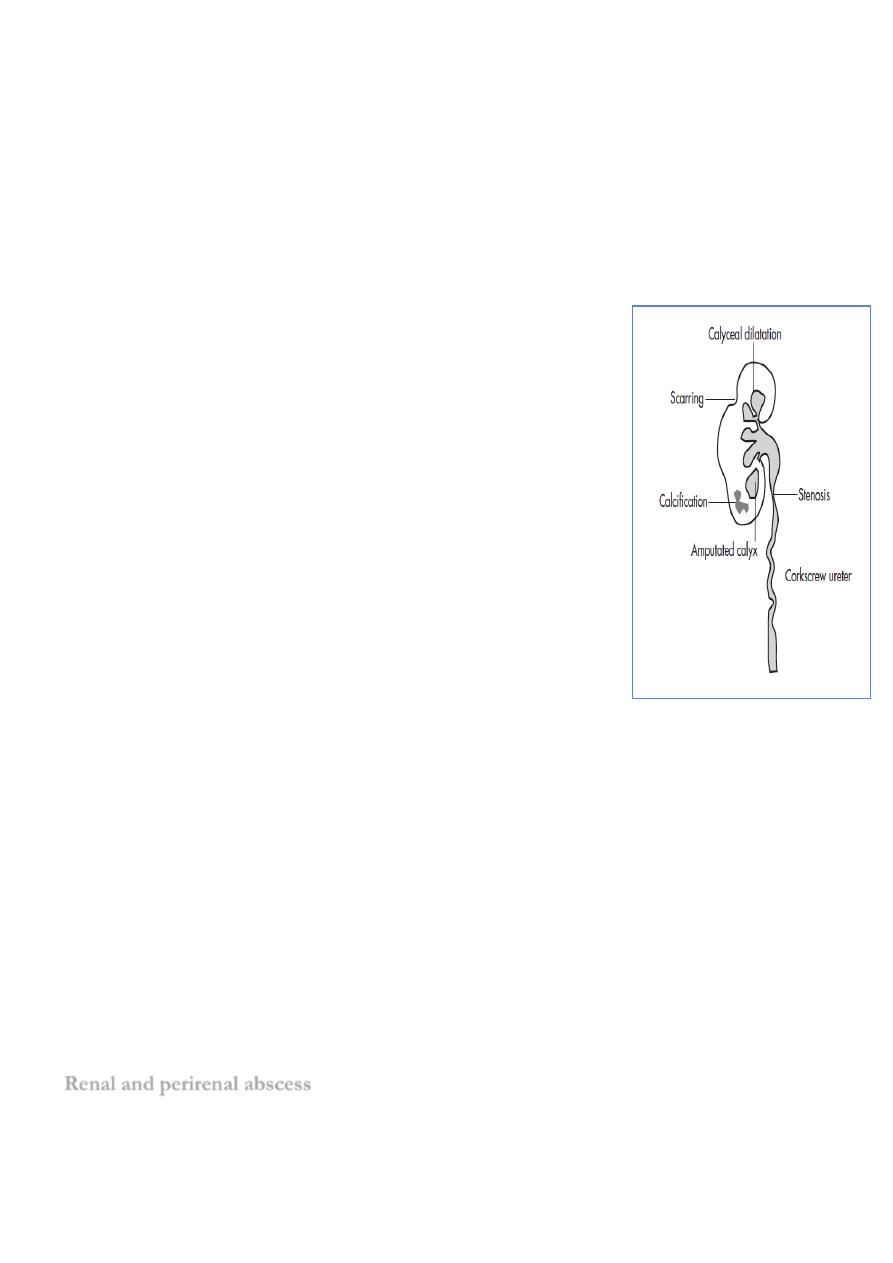
Tuberculosis
The genitourinary (GU) tract is the second most common site of tuberculosis involvement
after the lung.
Sites of Involvement
• Renal
• Ureteral
• Bladder
• Seminal vesicles, epididymis
Imaging features
Distribution
• Unilateral involvement is more common (70%) than bilateral (30%).
Renal Size
• Early, kidneys are enlarged.
• Later, kidneys are small.
• Autonephrectomy (nonfunctioning kidney)
Parenchyma
• Parenchymal calcifications, 70%
• Calcification may take on multiple forms: curvilinear, mottled, or amorphous; “putty kidney”
results when calcification has homogeneous, ground-glass appearance.
Collecting system
• Mucosal irregularity
• Infundibular stenosis, hiked-up pelvis with narrowed pelvis pointing up
• Amputated calyx
• Corkscrew ureter: multiple infundibular and
ureteral stenoses
(hallmark finding)
• Renal calculi, 10%
UB: thick walled contracted
Renal and perirenal abscess
US & CT are the modalities of choice in the diagnosis
US findings :
1. Cystic lesion of thick walls
2. Internal septations
3. Layering of echogenic material (debris)
4. May look like simple cyst.
CT findings:
-Thick walled cyst
-Enhancement of the cyst walls after contrast
-The underlying pre-disposing factor may be seen (e.g. stones)
Pyonephrosis:
Occurs only in obstructed PCS
US is the investigation of choice , it shows dilated PCS (hydronephrosis) with echogenic debris
filling the PCS
IVU : Poor renal function
Trauma
Mechanism
• Blunt trauma, 70%-80%
• Penetrating trauma, 20%-30%
CT is the study of choice.
One-shot IVP: visualization of both kidneys excludes pedicle avulsion.
Why imaging
?:
1-
assess the renal perfusion
2-
ensure that opposite kidney is normal
3-
show the extent of renal parenchymal damage
4-
Demonstrate injury to other abdominal organs
Minor injury (contusion & small capsular hematomas) produce swelling of parenchyma with
compression of calyces. If the kidney substance is torn, the renal outline is irregular & calyces
separated. Contrast extravasation noted in subcapsular & extracapsular hematomas.
Retroperitoneal hemorrhage may displace the kidney. Fragmentation of the kidney is serious &
usually need nephrectomy.
Absent nephrogram suggests thrombosis or rupture of renal artery. Renal infarction may also
ensue.
Tumors

Most common solitary mass: simple renal cysts & malignant tumors (adult RCC,
children Wilm’s T.)
Multiple masses : multiple simple renal cysts , polycystic disease , lymphoma
Other causes include abscess, benign tumors (e.g. angiomyolipoma) & metastasis.
Signs of renal mass :
A.
IVP :
A rounded lucency in the nephrogram.
bulging of renal outlines
displacement of calyces
enlargement of the kidney
calcification in a small proportion of renal carcinomas or wall of a cyst
B.
US: determine if the mass is cystic or solid
1. Simple renal cyst: spherical, anechoic, posterior acoustic enhancement, no or few
septations
2. Solid mass: most likely malignant, others benign angiomyolipoma, adenoma
3. mixed (complex) mass: renal tumor, renal abscess
When a solid is demonstrated, the ultrasonographer will also look for extension into the renal
vein & IVC, check for liver & retroperitoneal metastases & examine the opposite kidney.
C.
CT & MRI: differentiate cysts from solid masses, diagnose angiomyolipoma & stage renal
cancer.
.
Simple Cyst at CT is well defined, homogenous, and spherical with attenuation value similar to
that of water, no enhancement after IV contrast.
Renal cell carcinoma is shown as spherical mass, poorly defined outlines, solid mass +/- central
necrotic area +/- calcification, enhancement after contrast administration
CT is the method of choice in diagnosis & staging of Renal Cell Ca
Preoperative renal biopsy is rarely needed as CT diagnosis is sufficiently accurate
The role of CT in staging RCC
can demonstrate the local spread to the adjacent structures
Assess LAP in the retroperitoneum
Liver metastases
Extension of tumor thrombus into the renal vein & IVC
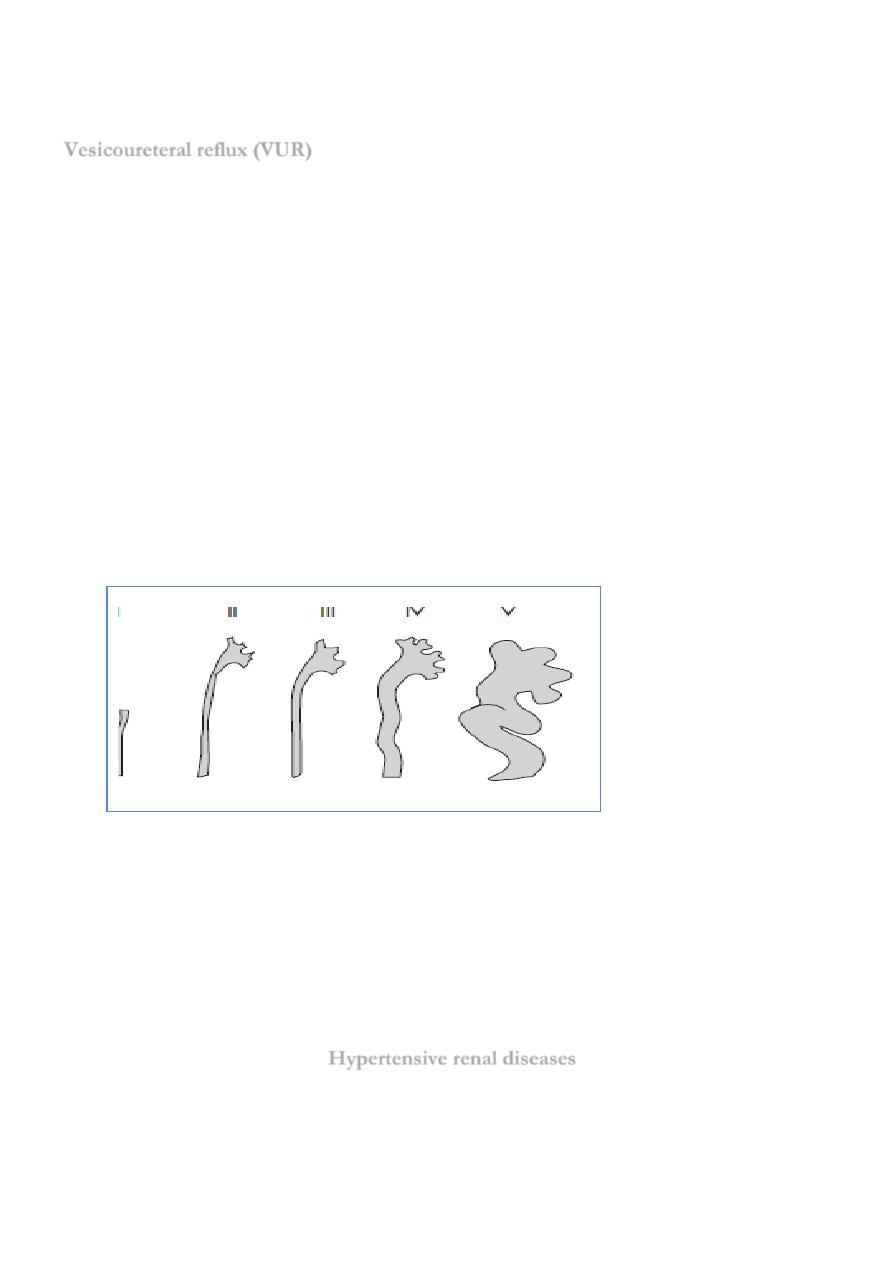
Vesicoureteral reflux (VUR)
Primary VUR is due to immaturity or maldevelopment of the UVJ with incompetence of the
antireflux flap valve action ,so usually affect pediatric age group.
Other causes of reflux (secondary reflux):
• Periureteral diverticulum
• Ureterocele
• Ureteral duplication
• Bladder outlet obstruction
Radiographic Features
Grading of reflux (international grading system)
• Grade I: reflux to ureter but not to kidney
• Grade II: reflux into ureter, pelvis, and calyces without dilatations
• Grade III: reflux to calyces with mild dilatation, blunted fornices
• Grade IV: to calyces with moderate dilatation, obliteration of fornices
• Grade V: gross dilatation, tortuous ureters
This is complicated by chronic pyelonephritis –reflux nephropathy- in which
there is
Dilatation of calyces in scarred areas.
Overall reduction in renal size.
Dilatation of affected collecting system due to reflux.
Reflux may be demonstrated at micturating cystourethrography.
Hypertensive renal diseases
Hypertension due to renal diseases include renal artery stenosis (RAS), chronic
glomerulonephritis (CGN), chronic pyelonephritis (CPN), polycystic disease, polyarteritis

nodosa (PAN) & diabetic nephropathy. The common feature is a reduction in blood supply to
the kidney.
Chronic renal diseases
Main role of imaging is to determine the presence of UT obstruction & to assess the renal size
US is very useful to exclude or confirm the presence of obstructive uropathy. The
presence of normal PCS virtually excludes obstruction. KUB should be taken to
exclude stones if hydronephrosis is seen by US.
Intrinsic renal diseases as chronic glomerlonephritis result in reduction in the size of the
kidney & cortical thickness, increased cortical echotexture & accentuated
corticomedullary differentiation
In acute tubular necrosis, US shows normal or enlarged with normal pelvicalyceal
system with diffuse echogenic parenchyma. IVP shows a persistently dense nephrogram
without visible caliceal filling.
Renal papillary necrosis
RPN represents an ischemic coagulative necrosis involving variable amounts of pyramids and
medullary
Papillae
Causes
Ischemic necrosis
• Diabetes mellitus
• Chronic obstruction, calculus
• Sickle cell disease
• Analgesics
Necrosis due to infections
• TB
• Fungal
Imaging features (see the nearby figure)

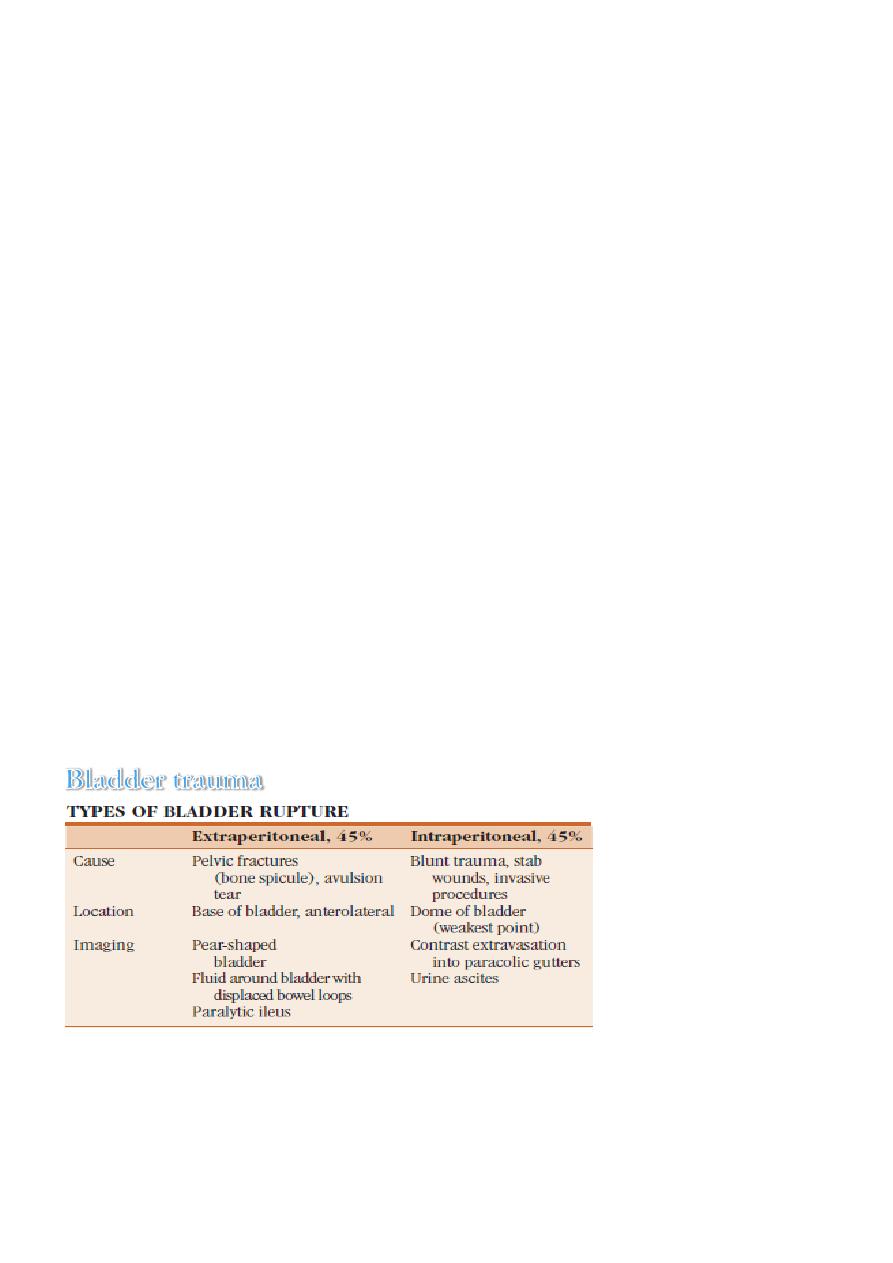
URINARY BLADDER
ULTRASOUND is the simplest imaging study to assess the UB
Normal UB lumen should be free of echogenic structures & its walls should be
uniform thickness
Normal wall thickness in distended state < 3 mm
Normal wall thickness in partially filled UB is < 5 mm
Neurogenic bladder
Types
• Spastic bladder: upper motor neuron defect, there is thick & trabeculated walls with dilatation
of the PCS & ureters secondary to bladder outlet obstruction
• Atonic bladder: lower motor neuron defect,there is smooth walled UB of large volume &
large residual volume
Bladder diverticulum
Types
Hutch diverticulum –primary-: congenital weakness of musculature near UVJ
• Usually associated with reflux
Acquired diverticulum in bladder outlet obstruction
• Usually multiple
• Not associated with reflux
Complications
Infection
Calculi, 25%
Tumor, 3%
-Filled with contrast in IVP, cystourethrography & in post voiding film
-Readily diagnosed with US, CT & MRI.
Bladder calculi
Could be single or multiple
May be associated with calculi elsewhere in the UT
Phleboliths may be confused with bladder stones, the former are usually rounded with
rather lucent center.
Malignant bladder neoplasm
Clinical Finding
• Painless hematuria
Types and Underlying Causes
Transitional cell carcinoma, 90%
SCC, 5%
• Calculi
• Chronic infection, leukoplakia
• Schistosomiasis
Adenocarcinoma, 2%
• Bladder exstrophy
• Urachal remnant
• Cystitis glandularis. 10% pass mucus in urine.
Imaging Features
• Mass in bladder wall: US > contrast CT, MRI
• Obstructive uropathy due to involvement of ureteric orifices
:
cystourethrography is modality of choice
Trans rectal US is the examination of first choice in suspected prostatic pathology
TRUS can identify small masses but can not differentiate benign from malignant one
Masses in the peripheral zone are likely to be malignant & those in the central zone are
more likely to be benign.
FNA under US guidance is the definitive diagnostic procedure for CA prostate
MRI is used for staging of CA prostate by assessing extension into the UB , seminal
vesicle & rectum , assess the pelvic LAP
Plain X ray of the pelvis & spine is performed to assess bone metastases
IVP plays minor role except for showing the back pressure effect of Bladder outlet
obstruction
CT does not demonstrate the internal structure of prostate as well as TRUS & MRI.
Prostatic calcification is common & due to prostatic calculi
BLADDER OUTFLOW OBSTRUCTION:
Due to:
Prostatic enlargement.
Bladder tumors.
Urethral strictures.
Posterior urethral valves.
Neurogenic bladder.
Imaging signs of bladder outflow obstruction:
1.
Increased trabeculation & thickness of bladder wall, often with diverticula
formation.
2.
Residual urine in bladder after micturition.
3.
Dilatation of collecting system.
Urethrography either antegrade as part of voiding cystourethrography or
retrograde through a catheter is the study of choice.
Post Inflammatory & post traumatic strictures occur at any site particularly the anterior
urethra
The benign strictures are smooth & short while the malignant are irregular in outlines
Posterior urethral valves: may be suspected at antenatal US, when there is bilateral
hydronephrosis, hydroureters & a thick-walled bladder. Cannot be demonstrated by
retrograde Urethrography
, but easily demonstrated at
micturating
cystourethrography
(show substantial dilatation of posterior urethra, which
terminates abruptly in a convex border).
urethra

TWO main indications for scrotal US are scrotal swelling & pain.
Doppler US can be used in acute testicular pain & swelling to distinguish between
torsion & epididymitis/orchitis.
MRI is used when US does not provide sufficient information. Ectopic testis can be
diagnosed by US & (if US fail), MRI is the investigation of choice.
Most solid testicular mass are malignant while cystic lesions are mostly benign
