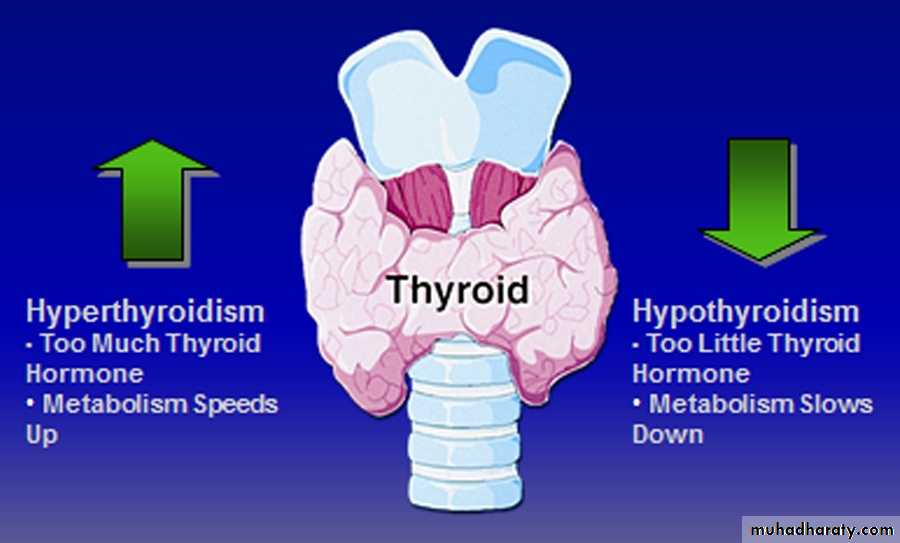
Hyperthyroidism
Dr.fakhir yousifThyroid gland
Bilobed gland in the neckLargest of all endocrine glands
Produces hormones
Thyroxine (T4) and tri-iodothyronine (T3)When the Thyroid Doesn’t Work
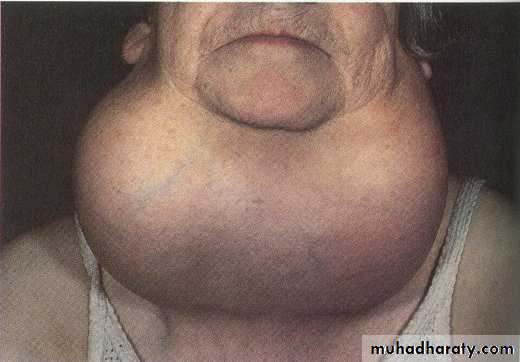
When the Thyroid Doesn’t WorkG O I T E R
G O I T E RThe functions of thyroid hormone are
1- Facilitated growth and development.2- Interfere with carbohydrate protein and fat metabolism.
3- Increase oxygen consumption by the tissue, basal metabolic rate, and heat production.
4- Increase oxygen release from HB.
5- Augmentation of adrenalin and noradrenalin function.
Thyrotoxicosis))Hyperthyroidism
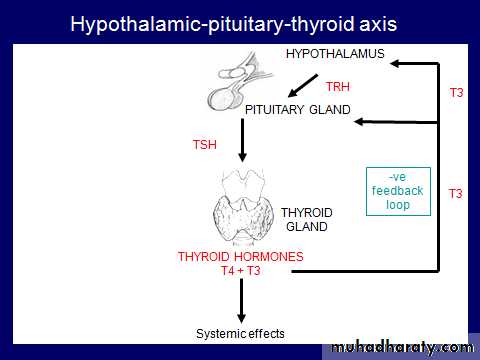
“Hyperthyroidism” refers to overactivity of the thyroid gland leading to excessive synthesis of thyroid hormones and accelerated metabolism in the peripheral tissues. The secretion of thyroid hormone is no longer under the regulatory control of the hypothalamic-pituitary center.Hyperthyroidism
1- Graves' disease 2- Multinodular goiter 3- Toxic adenomaPathogenesis
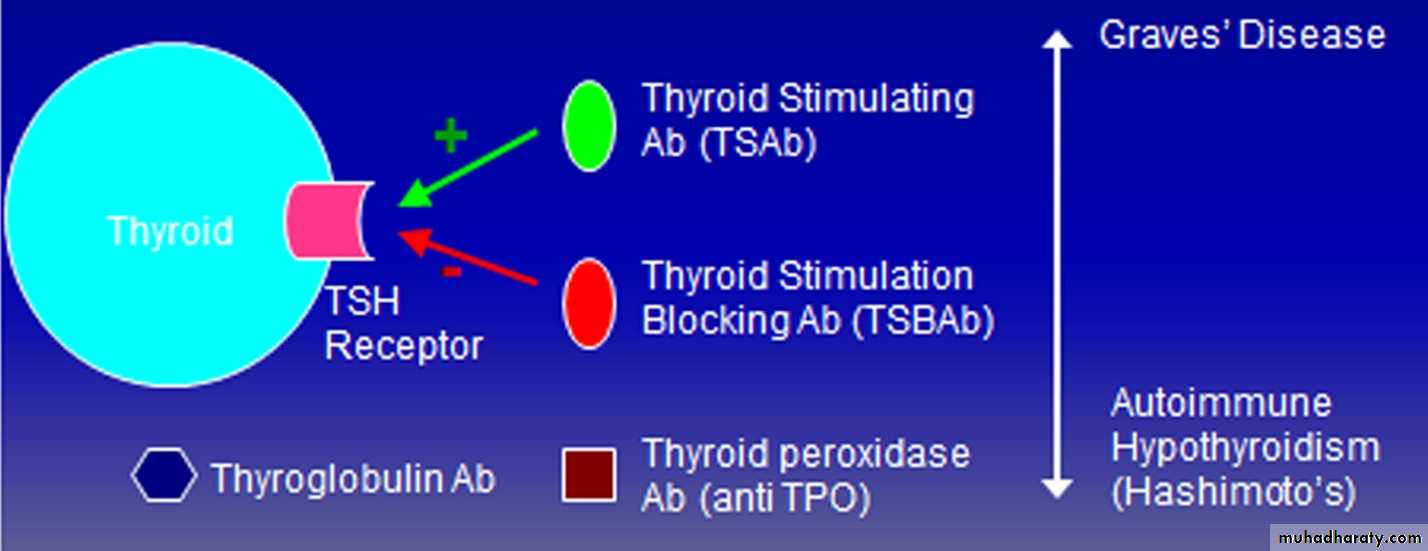
An autoimmune phenomenon – presentation determined by ratio of antibodies
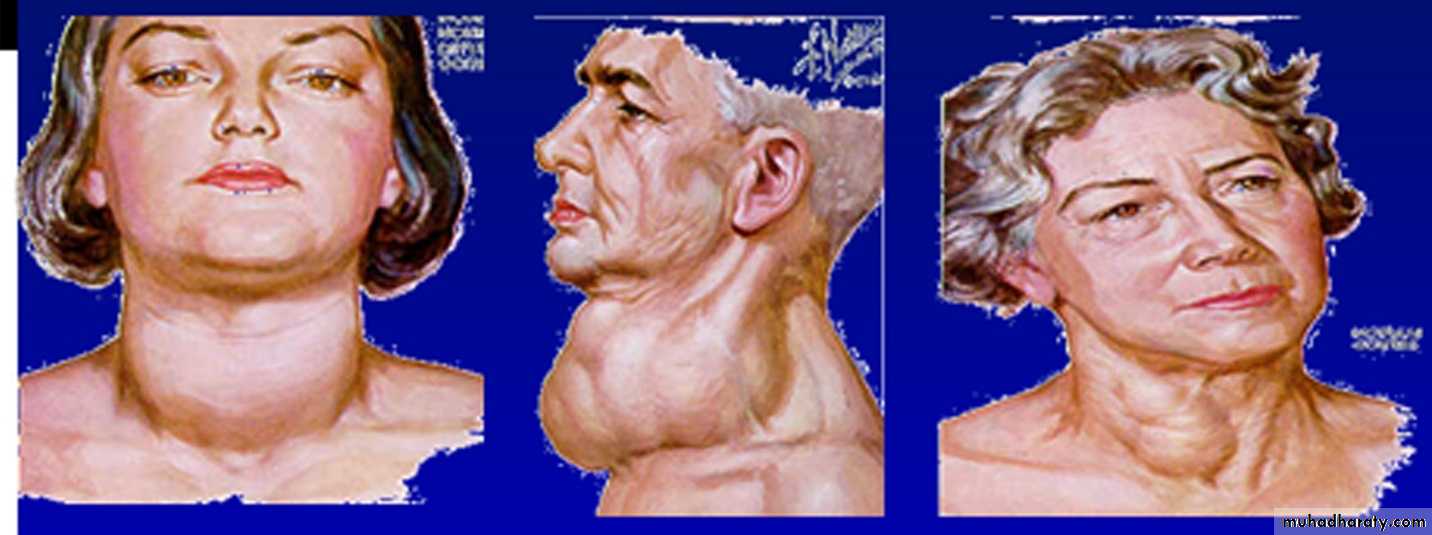
GRAVES' DISEASE
The most common manifestation is thyrotoxicosis with or without a diffuse goitre.Graves' disease also causes ophthalmopathy and rarely pretibial myxoedema
These features usually occur in thyrotoxic patients. Graves' disease can occur at any age but is unusual before puberty and most commonly affects women aged 30-50 years
The Classic Triad of Graves’ Disease
1-Hyperthyroidism (90%)2-Ophthalmopathy (20-40%)
3-Dermopathy (0.5-4.3%)
Graves’ Ophthalmopathy
Antibodies to the TSH receptor also target retroorbital tissuesT-cell inflammatory infiltrate, fibroblast growth(exophthalmus)
Severe: exposure keratopathy, diplopia, ,com-pressive optic neuropathy
Pretibial myxedema
Asymmetric, raised, firm, pink-to-purple, brown plaques of nonpitting edema on the anterior surface of the legAsymmetric, raised, firm, pink-to-purple, brown plaques of nonpitting edema on the anterior surface of the leg
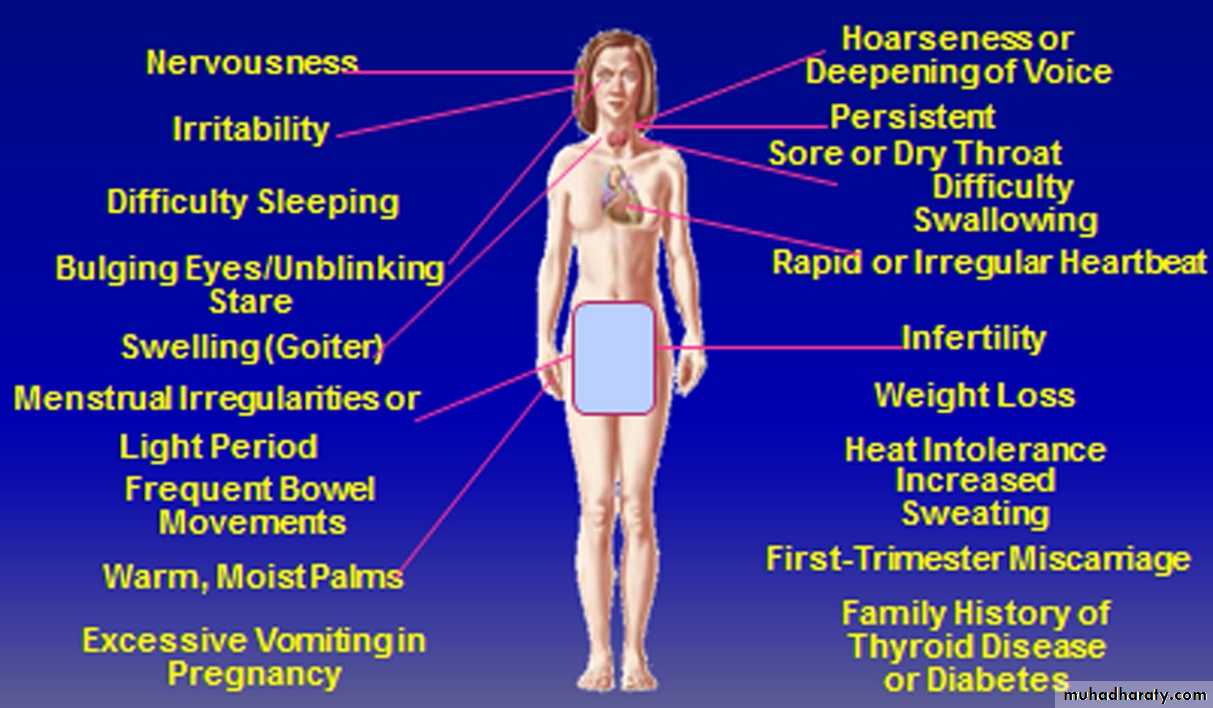
Features of Hyperthyroidism
General :Weight loss, heat intolerance
Thinning of hair, softening of nails
Cardiac
Atrial fibrillation Sinus tachycardia
Dyspnoea on exertionAnginaAnkle swelling
Systolic hypertensionincreased pulse pressureCardiac failure
Gastroenterology
Diarrhoea, steatorrhoea, hyperdefecation
Dermatological
Sweating Pruritis
Neuromuscular
Anxiety, irritability, emotional lability, psyachosisTremorMuscle weaknessHyper-reflexiasustained clonusProximal myopathyBulbar myopathy
Eyes
1) Lid lag
slowly moving point from above eye level to below and see if eyelid smoothly follows movement of eye -
2) Lid retraction
Lid retraction due to exophalmos (protrusion)AlopeciaReproductive
Amenorrhoea/oligomenorrhoeInfertility, spontaneous abortionLoss of libido, impotenceSigns and Symptoms of Hyperthyroidism
Thyroid function tests
Total T3 = 1.2 to 2.8 nmol\LTotal T4 = 150 nmol\L
TSH 0.5 to 5 mU\L.
Recently
1-free T4=10-30nmol\L2-free T3=0.3-3.3nmol\L
which is the most sensitive and specific test
Autoantibody
assessment: include TPH (thyroid peroxidase) normally less than 25nmol\l, and anti thyroglobulin anti body.
Diagnostic Imaging
Radioactive Iodine UptakeShows distribution of uptake
Technetium-99
Distinguishes high-uptake from low-uptake
Thyroid ultrasonography
Identifies nodules
Thyroid scanning: iodine 123 (123I) and iodine 131 (131I) Technetium Tc 99m
The images obtained by these studies provide thesize and shape of the gland and the distribution of functional activity.
Thyrotoxicosis treatment
The choice of therapy depends on:
1-Age of the patient
2-Size of the thyroid
3-Type of thyroxicosis
1- Age less than 45
Antithyroid drugsCarbimazole 40-60 mg daily or prophylthiouracil 400-600 mg daily. There is subjective improvement within 10-14 days and the patient is usually clinically and biochemically euthyroid at 3-4 weeks, when the dose can be reduced. The maintenance dose is determined by measurement of T4 and TSH,
Unfortunately, thyrotoxicosis recurs in at least 50%, usually within 2 years of stopping treatment.
In all patients with thyrotoxicosis a non-selective β-adrenoceptor antagonist (β-blocker), such as propranolol (160 mg daily) or nadolol (40-80 mg daily), will alleviate but not abolish symptoms within 24-48 hours. Beta-blockers cannot be recommended for long-term treatment, but they are extremely useful in the short term, e.g. for patients awaiting hospital consultation or following 131I therapy.
Adverse effects
Rash
Arthralgias
Urticaria
GI symptoms
Agranulocytosis
2- Age more than 45
Radioactive iodine131I is administered orally as a single dose and is trapped and organified in the thyroid ., the effects of its radiation are long-lasting, with cumulative effects on follicular cell survival and replication.
This regimen is effective in 75% of patients within 4-12 weeks. During the lag period, symptoms can be controlled by a β-blocker or, in more severe cases, by carbimazoleis, therefore, necessary.
3- Subtotal thyroidectomy
Toxic nodule or multinodular
Patients must be rendered euthyroid with antithyroid drugs before operation. Potassium iodide, 60 mg 8-hourly orally, is often added for 2 weeks before surgery to inhibit thyroid hormone release and reduce the size and vascularity of the gland, making surgery technically easier.
Treatment of Ophthalmopathy
Mild SymptomsEye shades, artificial tears
Progressive symptoms (injection, pain)
Oral steroids – typical dosage from 30-40mg/day for 4 weeksImpending corneal ulceration, loss of vision
Oral versus IV steroidsOrbital Decompression surgery
Sources of Dietary Iodine
Iodine in soil, water and cropsSeafood
Dairy Products
Iodised salt and other fortified foods
Medicines/health foods/supplements
Thyrotoxic crisis
(Thyroid storm') This is a rare and life-threatening increase in the severity of the clinical features of thyrotoxicosis. The most prominent signs are fever, agitation, confusion, tachycardia or atrial fibrillation and, in the older patient, cardiac failure. It is a medical emergency and, despite early recognition and treatment, the mortality rate is 10%. Thyrotoxic crisis is most commonly precipitated by infection in a patient with previously unrecognised or inadequately treated thyrotoxicosis.