Scrotal Pathologies
Incompletely descended testis (Undescended Testis):
The testis is arrested in some part of its path to the scrotum.Incidence: 4% of boys are born with one or both testes incompletely descended.
Half of these reach the scrotum during the first month of life.
two thirds of these reach the scrotum during the first three months of life
incidence of testicular maldescent at the age of one year is around 1 per cent
In 10% of unilateral cases there is a family history.
Pathology
The epithelial elements are immature histologically and by late puberty irreversible destructive changes halt spermatogenesis and limit the production of androgens.Early repositioning of an incompletely descended testis can preserve function
Clinical features
The scrotum is empty & underdeveloped
More common on the right
Bilateral in 20% of cases.
Secondary sexual characteristics are typically normal.
The testis may be:
• intra-abdominal, lying extraperitoneally above the internal inguinal ring.• inguinal, it may or may not be palpable
• in the superficial inguinal pouch, in which case it must be distinguished from retractile testis.
Sequels of incomplete descent
Sterility in bilateral cases (especially intra-abdominal testes)Pain as a result of trauma
Indirect inguinal hernia often present
Torsion of the testis
Epididymo-orchitis
Atrophy of an inguinal testis before puberty may possibly be caused by recurrent minor trauma
Testicular cancer is more common in an incompletely descended testes
N.B. orchidopexy may or may not diminish the risk of testicular cancer but it does improve the prospect of early diagnosis
Treatment
Orchidopexy is usually performed after the age of one year
The testes should be brought down into the scrotum before the boy starts school.
Orchidectomy should be considered if the incompletely descended testis is atrophic
Hormone treatment with human chorionic gonadotrophin is appropriate only when there is established hypogonadism.
ECTOPIC TESTIS
The testis is abnormally placed outside this pathThe sites of ectopic testis are:
• at the superficial inguinal ring: superfecial to the inguinal canal
• the perineum
• the root of the penis
• the femoral triangle.
An ectopic testis is usually fully developed. The main hazard is liability to injury.
Treatment: orchidopexy
N.B.: Retractile testis is normal testis with active cremasteric reflex
INJURIES TO THE TESTIS
Blunt or penetrating traumaContusion and rupture of the testis are associated with a collection of blood around the testis and cannot usually be distinguished with certainty without exploration.
O/E: scrotal swelling, bruises, Loss of testicular contour
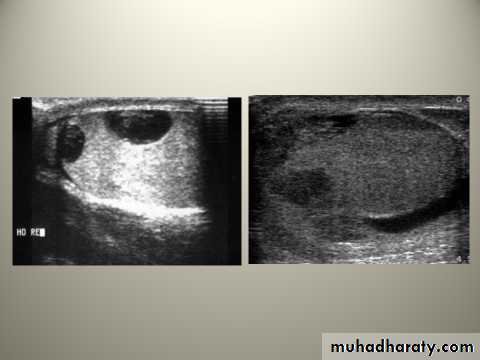
U/S is the investigation of choice
Haematocele ( collection of blood between two layers of tunica vaginalis) should be drained and the tunica albuginea repaired after evacuation of haematoma.
A severely damaged testis may have to be removed.
ABSENT TESTIS
‘Vanishing’ testis: a condition in which a testis develops but disappears before birth.Cause: prenatal torsion.
True agenesis of the testis is rarer.
Laparoscopy is useful in distinguishing these causes of clinically absent testis from intra-abdominal maldescended testis.
Scrotal Swelling
Scrotal swelling with pain:Epididymitis
Orchitis
Testicular trauma
Testicular torsion
Incarcerated scrotal hernia
Testicular tumor
Scrotal Swelling without pain:
HydroceleSpermatocele
Varicocele
Hematocele
Scrotal hernia
Testicular tumor
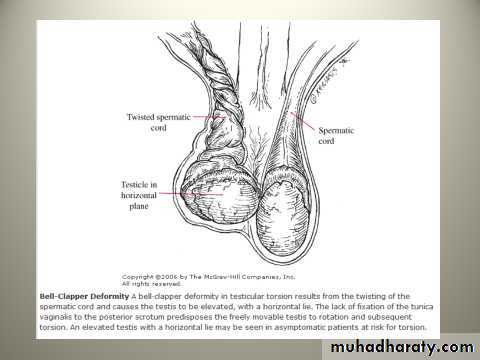
TORSION OF THE TESTIS ( Torsion of spermatic cord)
Rotation of the testis around the vertical axis of the cord
It is time limited due to arterial obstruction & the patient might lose his testis by ischemia (gangrene) if the diagnosis is delayed (6 hours).
It may develop spontaneously during sleep.
Straining at stool, lifting a heavy weight, trauma, and coitus are all possible precipitating factors.
Clinical features
Most common between 10 and 25 years of ageSudden agonizing pain in the groin and the lower abdomen.
The patient feels nauseated and may vomit.
The testis lie transversely high and the tender twisted cord can be palpated above it.
Testicular elevation does not relief pain
Loss of cremasteric reflex
Diagnosis
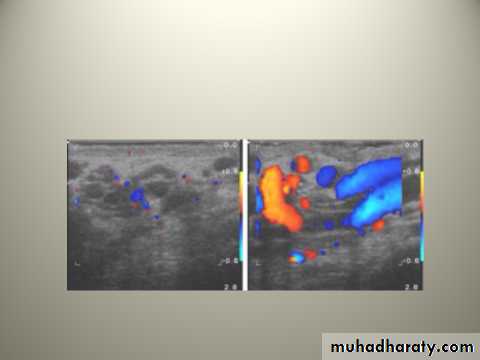
Doppler ultrasound scan will confirm the absence of the blood supply to the affected testis
Treatment
Exploration for torsionIf the testis is viable when the cord is untwisted then it is fixed (orcheopexy).
An infarcted testis (gangrenous) should be removed (orchidectomy).
The other testis should also be fixed because the anatomical predisposition is likely to be bilateral.
N.B: In the first hours it may be possible to untwist the testis manually, then early orcheopexy to avoid recurrent torsion
VARICOCELE
It is a varicose dilatation of the veins draining the testis ( abnormal dilatation of the pampiniform plexus)Most varicoceles present in adolescence or early adulthood
Usually on the left.
Clinical Features
Usually symptomless
There may be dragging scrotal discomfort
The scrotum on the affected side hangs lower than normal
On palpation, with the patient standing, the varicose plexus feels like a bag of worms.
Infertility ?
Investigations: Scrotal Doppler U/S
Treatment
Operation is not indicated for asymptomatic varicocele.Indicatioins: pain, infertility, cosmetic
Types of operations:
Varicocele ligation
laparoscopic ligation
Embolisation of the testicular vein under radiographic control
HYDROCELE
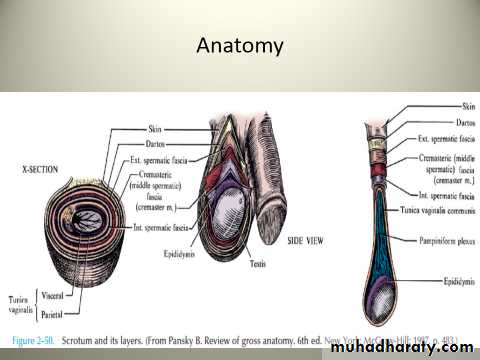
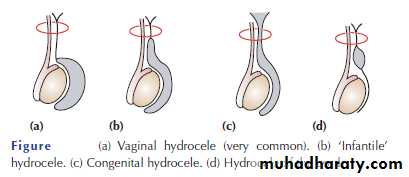
Hydrocele is an abnormal collection of serous fluid in a part of the processus vaginalis, usually the tunica.Vaginal hydrocele abnormal collection of serous fluid between the two layers of tunica vaginalis.
In congenital hydrocele, the processus vaginalis is patent and
connects with the peritoneal cavity.
Etiology
Acquired hydroceles are primary (idiopathic), or secondary to testicular disease.
A hydrocele can be produced in four different ways
• by excessive production of fluid within the sac, e.g. secondary hydrocele
• by defective absorption of fluid; this appears to be the explanation for most primary hydroceles although the reason why the fluid is not absorbed is obscure
• by interference with lymphatic drainage of scrotal structures
• by connection with the peritoneal cavity via a patent processus
vaginalis (congenital).
Clinical features
Primary vaginal hydrocele is most common in middle and later life but can also occur in older children presents withscrotal swelling
Painless
Typically translucent (transillumination +ve)
It is possible to ‘get above the swelling’ on examination of the scrotum
N.B: in a young man; there may be a testicular tumour, so scrotal US should be done.
Treatment
Congenital hydroceles are treated by herniotomy if they do not resolve spontaneouslyAcquired hydroceles: excision of the wall
N.B: A secondary hydrocele may subsides when the primary lesion resolves.
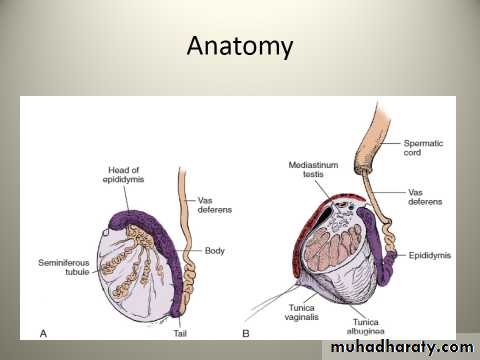
Epididymal cysts
They represent cystic degeneration of the epididymis.
Filled with a crystal-clear fluid.
Found in middle age
The cysts are multilocular
Excision may cause obstruction of the epididymis therefore it is better to leave it.
Spermatocele
A unilocular retention cyst derived from some portion of the sperm-conducting mechanism of the epididymis.Typically lies in the epididymal head above and
behind the upper pole of the testis.
The fluid contains spermatozoa
Small spermatoceles can be ignored. Larger ones can be aspirated or excised through a scrotal incision.
EPIDIDYMO-ORCHITIS
Inflammation confined to the epididymis is epididymitisInfection spreading to the testis is epididymo-orchitis.
Acute epididymo-orchitis
Mode of infection
Infection reaches the epididymis via the vas from a primary infection of the urethra, prostate or seminal vesicles
Blood-borne infections of the epididymis are less common
N.B: Acute epididymo-orchitis can follow any form of urethral
instrumentation. It is particularly common when an indwelling
catheter is associated with infection of the prostate.
Clinical features
The initial symptoms are those of urinary tract infection.
The epididymis and testis swell and become painful.
Fever
The scrotal wall, at first red, oedematous and shiny, may become adherent to the epididymis.
Resolution may take 6–8 weeks to complete.
Occasionally, an abscess may form and discharge of pus through the scrotal skin.
N.B: Acute epididymo-orchitis develops in about 18% of males suffering from mumps. The main complication is testicular atrophy, which may cause infertility if the condition is bilateral.
Investigations
GUE
Urine C&S
WBC count
Scrotal U/S
Treatment
Broad spectrum antibiotics for 2 weeks (3rd generation cephalosporin or quinolones)Scrotal support
Supportive therapy (analgesics, antipyretics, anti emetics, IVF)
If suppuration occurs(Abscess): drainage is necessary.
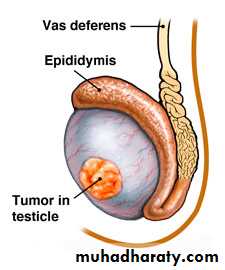
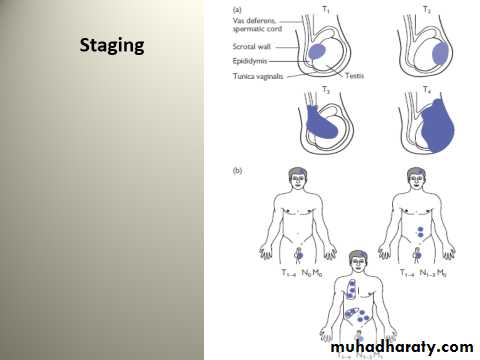
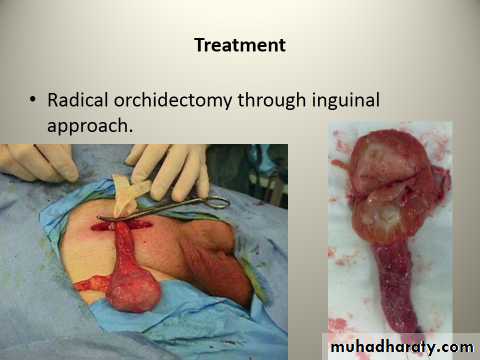
TUMOURS OF THE TESTES
Most testicular neoplasms are malignant
It is one of the most common forms of cancer in young men.
Maldescent predisposes to malignancy
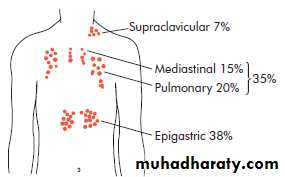
The lymphatic drainage of the testes is to the para-aortic lymph nodes near the origin of the gonadal vessel.
The inguinal lymph nodes are affected only if the scrotal skin is involved.
Classification
They are classified according to their predominant cellular type:GCTs:
Seminoma (40%):
The enlarged testis is smooth and firm.
metastasize via the lymphatics.
Hematogenous spread is uncommon.
Nonseminomatous GCT or Teratoma (32%):
Arises from totipotent cells in the rete testis and often contains a variety of cell types, of which one or more predominate.
They may secrete human chorionic gonadotrophin (HCG) & alpha-fetoprotein.
Combined seminoma and teratoma (14%)
2. Interstitial tumours (1.5%):
arise from Leydig or Sertoli cells3. Lymphoma (7%)
4. Other tumours (5.5%)
Clinical features
testicular lump which is usually painless
sensation of heaviness occurs when the testis is two or three times its normal size
The testis is enlarged, smooth, firm and heavy
Secondary hydrocele
Secondary retroperitoneal deposits may be palpable, just above the umbilicus, hepatic enlargement, enlarged supraclavicular nodes
Symptoms of metastatic disease: abdominal or lumbar pain, chest pain, dyspnoea and haemoptysis
Rarely, patients present with severe pain and acute enlargement of the testis because of haemorrhage into a neoplasm
Between 1% and 5% of cases have gynaecomastia (mainly the teratomas).
Investigations
Tumour markers (HCG, alpha-fetoprotein and lactate dehydrogenase)
U/S scanning of the testis
CXR: pulmonary metastases especially in teratoma
CT scan and MRI are the most useful means of detecting secondaries and o f monitoring the response to therapy.
Further Mx:
Further treatment depend on staging and histological diagnosis (after orchidectomy):Seminomas
Radiosensitive
Highly sensitive to cisplatin, which is used for patients with metastatic disease.
Teratomas
less sensitive to radiation
Chemotherapy:
Cisplatin, methotrexate, bleomycin and vincristine : used in combination with great success.
For both seminoma & teratomas: Retroperitoneal lymph node dissection is sometimes needed when retroperitoneal masses remain after chemotherapy
Prognosis
Seminoma: the 5 years survival after orchidectomy and radiotherapy or chemotherapy:If there are no metastases 95%.
If there are metastases 75%
Teratoma: 5-year survival rate:
stage 1 - 2: of more than 85%
stage 3 - 4 : about 60%
Idiopathic scrotal gangrene- Necrotizing fasciatis (Fournier’s gangrene)
Fulminating inflammation of the subcutaneous tissues, which results in an obliterative arteritis of the arterioles to the scrotal skin
Most commonly occurs in immunocompromised patients
Causative organisms: mixed infection of Haemolytic streptococci (sometimes microaerophilic), Staphylococcus, E. coli, Clostridium welchii.
Clinically:
Sudden scrotal inflammationRapid onset of gangrene and loss of scrotal skin leading to exposure of the scrotal contents
The absence of any obvious cause in over half the cases.
The condition can follow minor injuries or procedures in the perineal area, such as a bruise, scratch, urethral dilatation, injection of haemorrhoids or opening of a periurethral abscess.
Clinical features
Sudden pain in the scrotum, prostration, pallor and pyrexia.Cellulitis spreads until the entire scrotal coverings slough, leaving the testes exposed but healthy
Treatment
The microorganisms are usually sensitive to gentamicin and a cephalosporin
Wide excision of the necrotic scrotal skin
Many patients die despite active treatment\