مكتب الجامعة للطباعة والاستنساخ
عدد: 4 السعر:250مكتب الجامعة للطباعة والاستنساخ
عدد: 4 السعر:250
Neurogenic bladder
Neurogenic bladder
The urinary bladder is probably the only visceral smooth muscle that is under complete voluntary control from cerebral cortexIt has both somatic & autonomic innervations
The functional features include:
A normal capacity of 400 – 500 ml
Sensation of fullness
Volume change without change in intraluminal pressure
Initiation & maintenance of contraction until bladder is empty
Voluntary initiation or inhibition of voiding
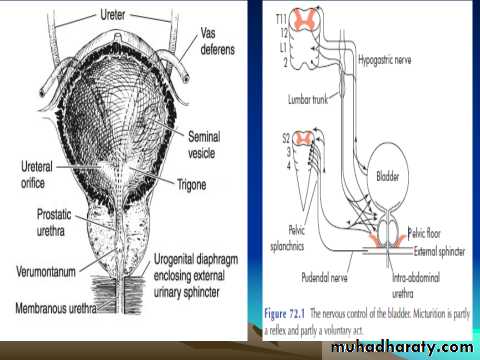
The sphincteric unit
In both male & females : two sphinctersInternal involuntary SM sph. at bladder neck
External voluntary striated M. sph. from the prostate to membranous urethra in males & at mid urethra in females
N.B. : the ureterovesical junction prevent backflow of urine from the bladder to the upper urinary tract.
Innervations
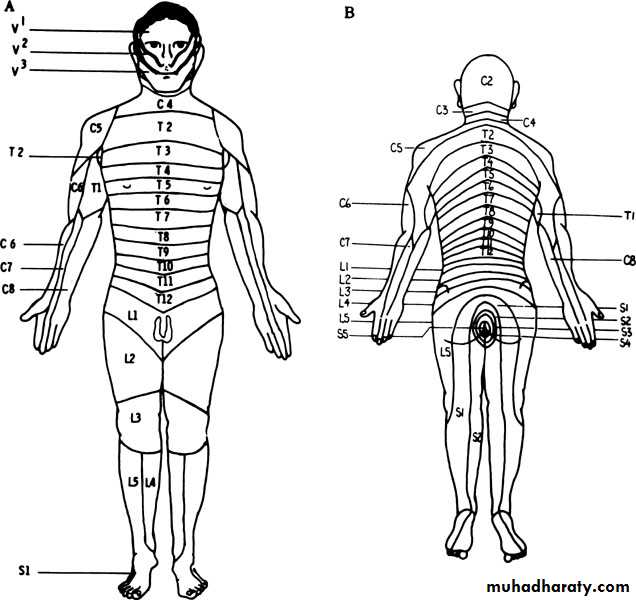
Parasympathetic : the anterior primary divisions S 2 – 4
Sympathetic : T10 – L 2
Somatic motor innervation :S 2 – 3 though the pudendal N.
The micturition reflex
Intact pathway via the spinal cord & pons required for normal micturition.The pontine center send either excitatory or inhibitory impulses to regulate the micturition reflex
Disruption of pontine control as in upper spinal cord injury lead to contraction of the bladder without sphenecteric Relaxation ( detrusor-sphincter dyssynergia)
Classification of neurogenic bladder
Upper motor neuron : spastic , uninhibited : injury above spinal cord micturition centerLower motor neuron: flaccid , atonic, areflexic : injury in the pelvic nerves or spinal micturition center
Spinal shock
N.B. Spinal shock
Immediately after injury, regardless of the level, there is a stage of flaccid paralysis with numbness below the level of the injury that lead to bladder overfilling to the point of overflow incontinence & rectal impaction.
It last few weaks up to 6 months
Feature:
UMNL : reduced bladder capacity , involuntary detrusor contraction , high intravesical & detrusor pressure , spasticity of pelvic striated M. , autonomic dysreflexia in cervical cord lesionsLMNL : large bladder capacity, lack of voluntary detrusor contraction, low intravesical pressure, deceased tone in external sphincter.
N.B.: full neurologic exam. is required for those patients to assess the
level of sensory and motor loss
Investigations
Urinalysis
Renal function test
Imaging study (U/S-IVU)
Instrumental exam. Cystoscopy
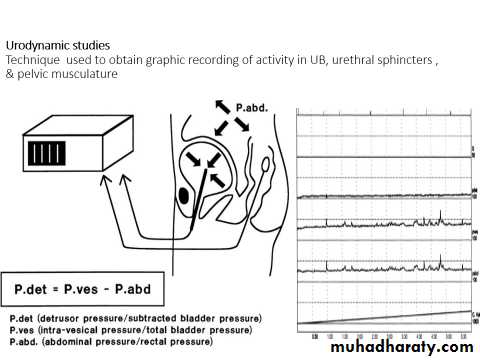
Urodynamic studies
Differential diagnosis
CystitisChronic urethritis
Vesical irritation 2ry to psychic disturbance
Interstitial cystitis
Cystocele
BOO
Treatment :
The treatment is guided by the need to restore low pressure activity & to empty the bladder effectively in order to preserve renal function, continence, & control infection-Spinal shock
-Bladder drainage by clean self intermittent catheterisation(CSIC) , indwelling catheter or suprapubic cystostomy
-UDS
- Increase fluid intake to 2 – 3 l/day
- Prophylaxis for calculus formation by reducing calcium & oxalate intake
- Spastic neuropathic bladder
Voiding by trigger technique.
Anticholinergic medications (parasympatholytic drugs) like Detrositol , ditropan (oxybutynin)
CSIC ( clean self intermittent catheterization ) or Indwelling catheter
Condom catheter & leg bag
Sphinterotomy to decrease outlet resistance
Sacral rhizotomy at S 3-4
Neurostimulation
Urinary diversion\
- Flaccid neuropathic bladder
Crede maneuver ( manual suprapubic pressure) accompanied by strainingBladder training & care , voiding every 2hr
CSIC every 3-6 hr
TUR in hypertrophied bladder neck or BPH
Parasympathmimetic drugs like bethanecol chloride( Urecholine) 5 – 50 mg every 6-8hr
Complications
Infection : cystitis, periurethritis, prostatitis, epididymoorchitis, pyelonephritisHydronephrosis
Calculus formation
Renal amyloidosis
Sexual dysfunction
Autonomic dysrelexia: sympathetically mediated reflex behavior, in patients with cord lesion above T1
symptoms include dramatic elevation in systolic &/or diastolic pressure, increase pulse pressure, bradycardia, headache, piloerection.
symptoms brought by overdistention of the bladder
Treatment:
Immediate catheterisation
Oral nifedipine (20mg) 30 min before cystoscopy as prophylaxis
Alpha adrenergic blockers
Prognosis
The greater threat to those patients is progressive renal damage caused by pyelonephritis , calculosis, hydronephrosis