
Lecture 5
Gram Negative rods related to the respiratory tract
Two medically important gram negative rods associated with
respiratory tract
Haemophilus influenzae
Bordetella pertussis
Haemophilus
Haemo= blood , philus= loving ie. Bacteria which like blood
in their growth, these are heterogenus group of bacteria.
Small gram –ve rods called coccobacilli, some time are
pleomorphic, facultative anaerobic which grow on enriched media,
non motile, non spore forming. Require X and V factors for their
growth.
Some of them are pathogenic while others are non
pathogenic, the group of coccobacilli include Bordetella and
Brucella. Haemophilus can be divided into:-
Haemophilus
Beta- haemolytic non-haemolytic
XV V
H. haemolyticus H. parahaemolyticus
XV V X
H. influenzae H. parainfluenza H.ducreyi
H. aegyptius H. haemoglobinophilus
H. suis H. aphrophilus
H. gallinarum
Haemophilus influenzae called (pfeiffer’s bacilli)
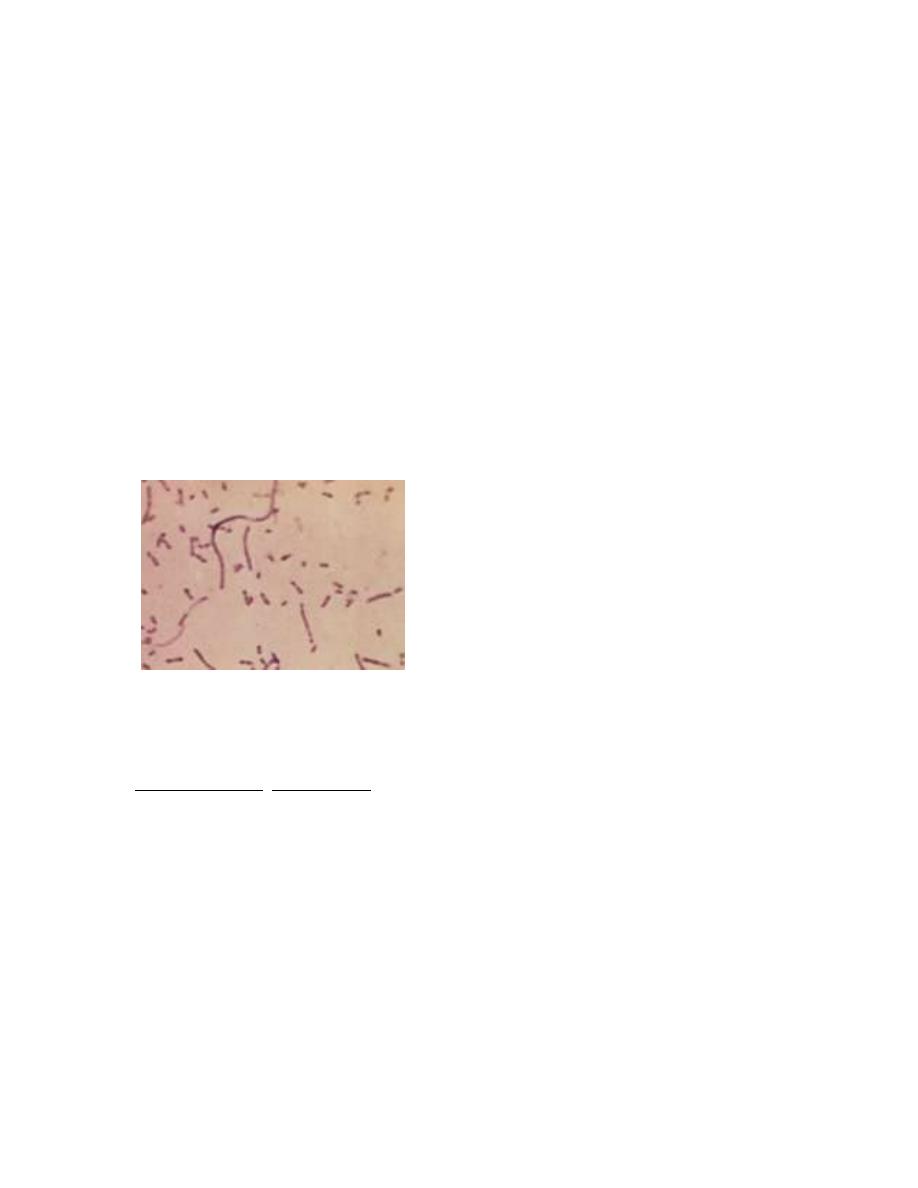
Morphology: G-ve, short coccobacilli. In young culture i.e. after
6-8 hour, the m.o. will be capsulated, in old culture i.e. after 18
hour, the m.o. becomes long, filamentous and lose the capsule, so
the m.o. described as pleomorphic m.o.
The capsule is important in typing by a reaction using antisera
similar to quelling reaction, also the capsule can be detected by
(CCE) counter current electrophoresis or by immunoflourescent
test. So the m.o. with capsule are virulent and form mucoid smooth
colony and these without capsule form rough colony.
Antigenic structure:
1) Capsule: composed of polyribose ribitol phosphate (PRP) so
Haemophilus influenzae can be typed into 6 types from A-F. The
most important one and pathogenic is type B, while the others are
rarely pathogenic.
2) Somatic Ag which are proteins and one of two types M,P
3) Endotoxin.
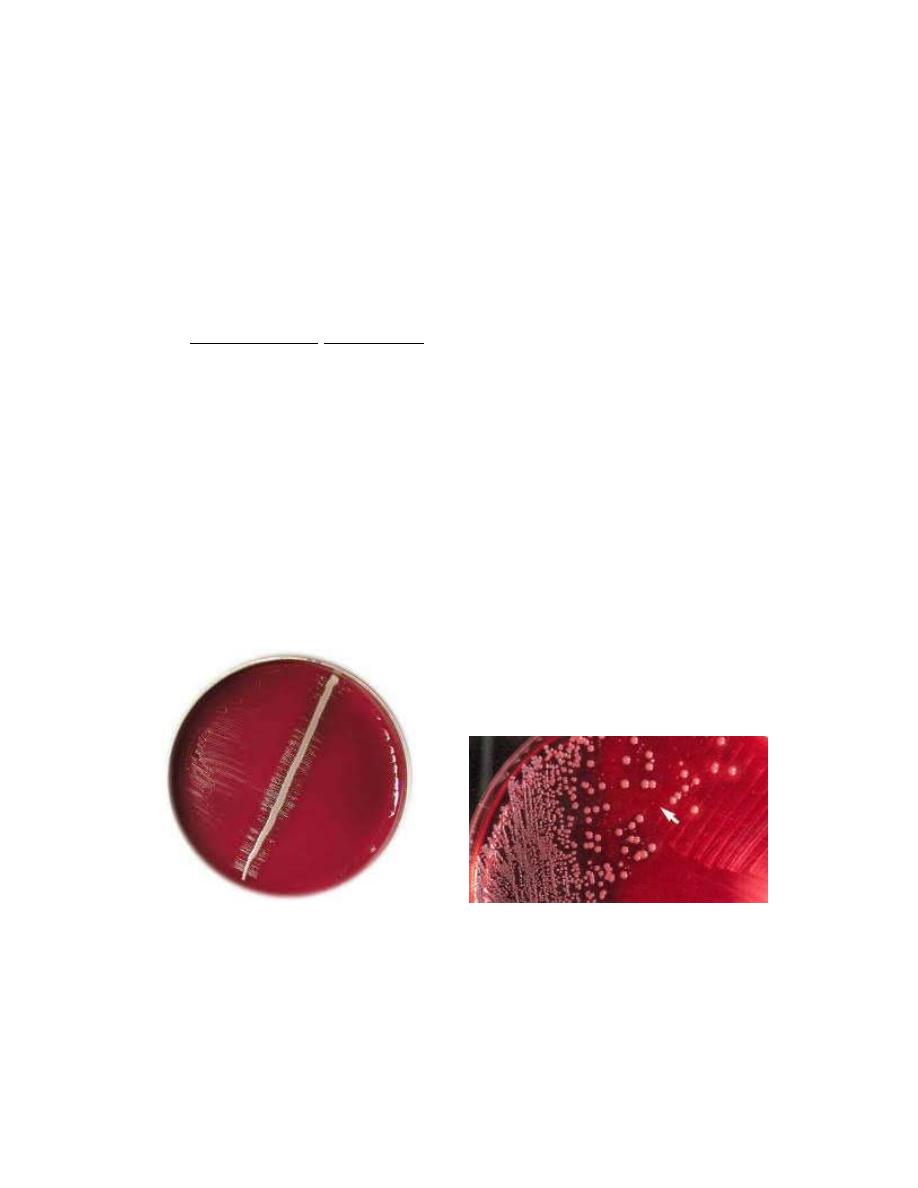
Cultural Characteristics:
Media used:
Brain heart infusion agar with blood, colonies are small,
rounded, iridescent and dew like appearance.
Chocolate agar: contain a substance called isovital ex.
Haemophilus influenzae requires X and V factors.
X haemin, heat stable needed in the synthesis of respiratory
enzymes like cytochrome oxidase, catalase and peroxidase.
V heat labile, can be provided by a substance called NAD
(nicotinamide adenine dinucleotide). Needed for oxidation-
reduction system.
Sattelite phenomena
Other characteristics:
Poorly ferment CHO, need 5-10% co2 in their growth, m.o.
are able to transform DNA extract from one generation to
another in order to transfer the resistance to antibiotics, e.g
penicillin, chloramphenicol and this is by plasmid.
Pathogenesis:
Haemophilus influenzae infect only human and there is no
animal reservoir, it enters the body through the URT, resulting in
either asymptomatic infection or infection as otitis media, sinusitis
and pneumonia. The m.o. produce IgA protease that degrade
secretory IgA, thus facilitate attachment to the respiratory mucosa.
After establishment in the URT, the organism enters the blood
stream and spread to the meninges causing meningitis.
Meningitis caused by encapsulated strain 95% of which
posses type B capsule. Pathogenesis involves the antiphagocytic
capsule and endotoxin No exotoxin is produced.
Most infection occurs in children between the age of (6
months - 6 years) with a peak between 6 months – 1 year. This
may be due to decline in maternal IgA and inability of child to
generate Ab against the polysaccharide capsular Ag.
Diagnosis:
1) Direct examination of naso- pharyngeal swab, swab, blood,
CSF by immunoflourescent technique
2) Quelling reaction for typing and counter currant
electrophoresis.
Immunity:
Infants below 3 months are usually immune because of the
antibodies from the mother (natural passive immunity), after that
sub clinical infection will induce Abs, thus in children 3-5 years
have Abs are resistant to infection. Adult after 25 years of age the
immunity becomes low against Haemophilus influenzae so they
need vaccination.
Treatment:
Mortality rate in meningitis due to this m.o. is high up to
90% in young children. The m.o. is sensitive to ampicillin, about
30% of strain may produce B- lactamase enzyme, all strain are
susceptible to new generation cephalosporins.
Immediate treatment is essential in order to prevent the late
neurological complication, however patient with meningitis which
does not improve very well remain a source of infection, so that
people in contact with the patient if they are adult then no
treatment but in children give prophylactic dose of rifampicin for 9
days.
Notes:
Type A causes chronic sinusitis, type E,F are important post
operatively.
Haemophilus aegyptius important in acute conjunctivitis which is
highly infectious called Koch week bacilli.
Haemophilus haemolyticus normally presenting throat and it is
important in acute and chronic R.T.I (respiratory tract infection)
Haemophilus parainfluenza: present in the throat, causes acute,
chronic R.T.I and sub acute bacterial endocarditis.
Haemophilus ducreyi: causes chancroid i.e. soft chancher which
is STD (sexually transmitted disease) with irregular ulcer on
genitalia, swelling, tender, lymphadenopathy, it should be
differentiated from other STD e.g Syphlis, herpes simplex.
Diagnosis:- scraping from ulcer, culture.
Treatment:- cotrimoxazol, erythromycin.
Haemophilus aphrophilus: found in normal flora of mouth, it is
important in endocarditis and pneumonia.
Bordetella
Bordetella pertussis: which is the commonest type
Bordetella parapertussis: causes a disease similar to whooping
cough but mild and subclinical.
Bordetella brochiseptica : which is small gram –ve bacilli that
found in the respiratory tract of canines.
Bordetella pertussis:
It causes a highly important communicable disease in human
being which is pertussis (whooping cough). The disease has
duration of 1-2 months, it affects children with a catarrhal
inflammation of respiratory tract with a characteristic of
paroxysmal cough that end in whoop.
Bordetella pertussis is a small gram –ve coccobacilli, strictly
aerobic, encapsulated, the capsule can be identified by using
immunoflourescent method.
Staining with tolidine blue shows bipolar metachromatic granules
the causative m.o. named bordet- Gengou bacilli according to the
scientists which observe the bacilli in the sputum of a patient with
whooping cough.
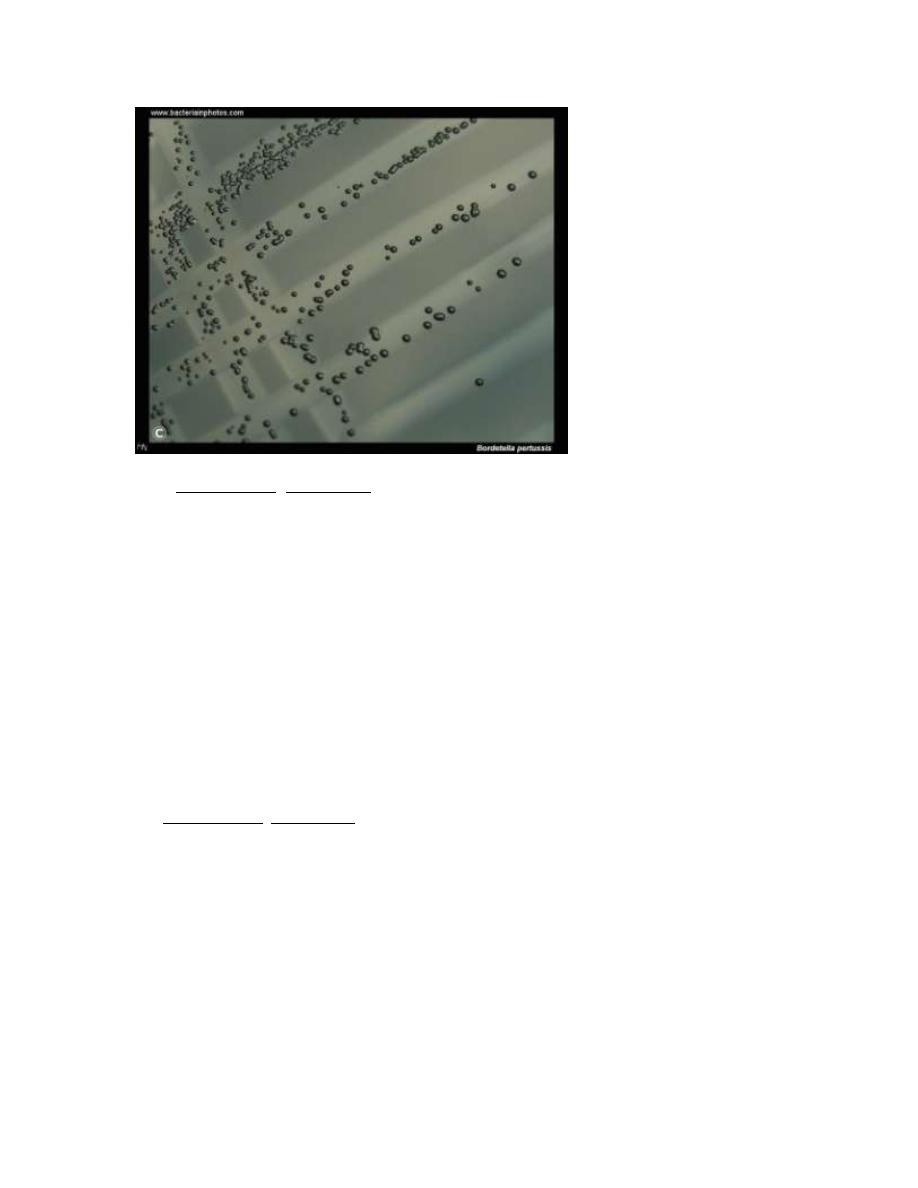
Cultural characteristics: Grow on enriched media
1) Bordet- Gengou agar: composed of blood- potato- glycerol) and
penicillin G (0.5 Mg/L)
2) blood- choclate agar.
The m.o. grows at 37c and need 3-7 days for their cultivation in
moist environment. The colonies are 1-2 mm. in diameter and
appear like mercury drop or a pearl colony, and iridescent with
narrow zone of haemolysis. No need for X and V factors.
All Bordetella pertussis are alike when they are freshly isolated
from the body but when cultivated they will resolve into four
phases:-
Phase I: which represent the freshly isolated virulent and
encapsulated pathogen.
Phase VI: is the completely non pathogenic form ( a virulent stage)
Phase II and III: are intermediate.
Antigenic structure:
1) Bordetella pertussis: serotyped on the basis of K- agglutinogen
three serotyping are known:
Type 1,2
Type 1,2,3
Type 1,3
2) Cell wall contain lipopolysaccharide
3) 4 biologically active substances

a- pertussis toxin: (major virulence factor) which is an exotoxin
and is responsible for prolonged immunity. It has a histamine
sensitizing properties and is responsible for the paroxysmal cough
which is the characteristic of the disease.
b- 2 hemagglutinin: one is filamentous haemagglutinin, the other
causes leucocytosis particularly lymphocytosis.
c- Adenylate cyclase complex
d- Heat labile toxin: found in the protoplasm of the cell.
Pathogenesis:
Bordetella pertussis is a pathogen only for humans
transmission is by the respiratory route from early cases and
carriers. The organisms attach to the ciliated epithelium of the
URT but do not invade the underlying tissue. It causes decreased
ciliated activity followed by death of the ciliated epithelial cells.
Factors which play a role in the pathogenesis:-
1) Attachment of the organism to the cilia of the epithelial cells
mediated by protein called filamentous hemagglutinin.
2) Pertussis toxin: stimulate adenylate cyclase and help the
addition of ADP ribose to form AMP, the toxin also mediates its

binding on the receptors of the epithelial cells, pertussis toxin also
causes lymphocytosis in blood because it causes failure of the
lymphocytes to enter the lymphoid tissues.
3) The organism synthesize adenylate cyclase which inhibit the
phagocytic activity.
4) Tracheal cytotoxin is a fragment of bacterial peptidoglycan
leading to damage of the ciliated cells.
Laboratory diagnosis:
1) Throat swab taken during paroxysmal stage
a- direct examination: by immunofluorescent technique which can
give false (+ve) result.
b- culture: on appropriate media, then the identification by slide
agglutination test with specific antisera or fluorescent antibody
stain which is more useful than direct examination.
2) Cough modified plate method.
3) Serological diagnosis of little importance because antibodies do
not occur until the 3
rd
week of illness.
Prevention:
Two vaccines:
1) a cellular vaccine contain purified proteins from the organism.
(pertussis toxoid).
2) Killed vaccine contain inactivated Bordetella pertussis organism
(pertussis toxin)
* The acellular vaccine consists of five Ag, purified from the
organism. The main immunogen in this vaccine is inactivated
pertussis toxin (toxoid). This vaccine has been inactivated
genetically but retains its antignicity.
The acellular vaccine has few side effects than the killed vaccine.
The killed vaccine is usually given combined with diphtheria and
tetanus toxoid (DTP) in three doses beginning at the 2 months of
age, a booster dose at 12-15 months of age and another at the time
of entering school.
The killed vaccine is no longer recommended because it’s
suspected to cause side effects including post vaccine
encephalopathy.
Treatment:
1) the m.o. are susceptible to many antibiotics however
erythromycin used in catarrhal stage and can be used as
prophylaxis for the contact individuals because it reduces the
number of organism in the throat and decrease the risk of
secondary complication.
2) Sedation used to prevent convulsinon.
3) O2 also used.
4) Suction of mucus during paroxysmal stage especially in infants.
