1
Dept. of Microbiology-Virology
Dr. Shatha F.Abdullah
Paramyxoviruses (Paramyxoviridae)
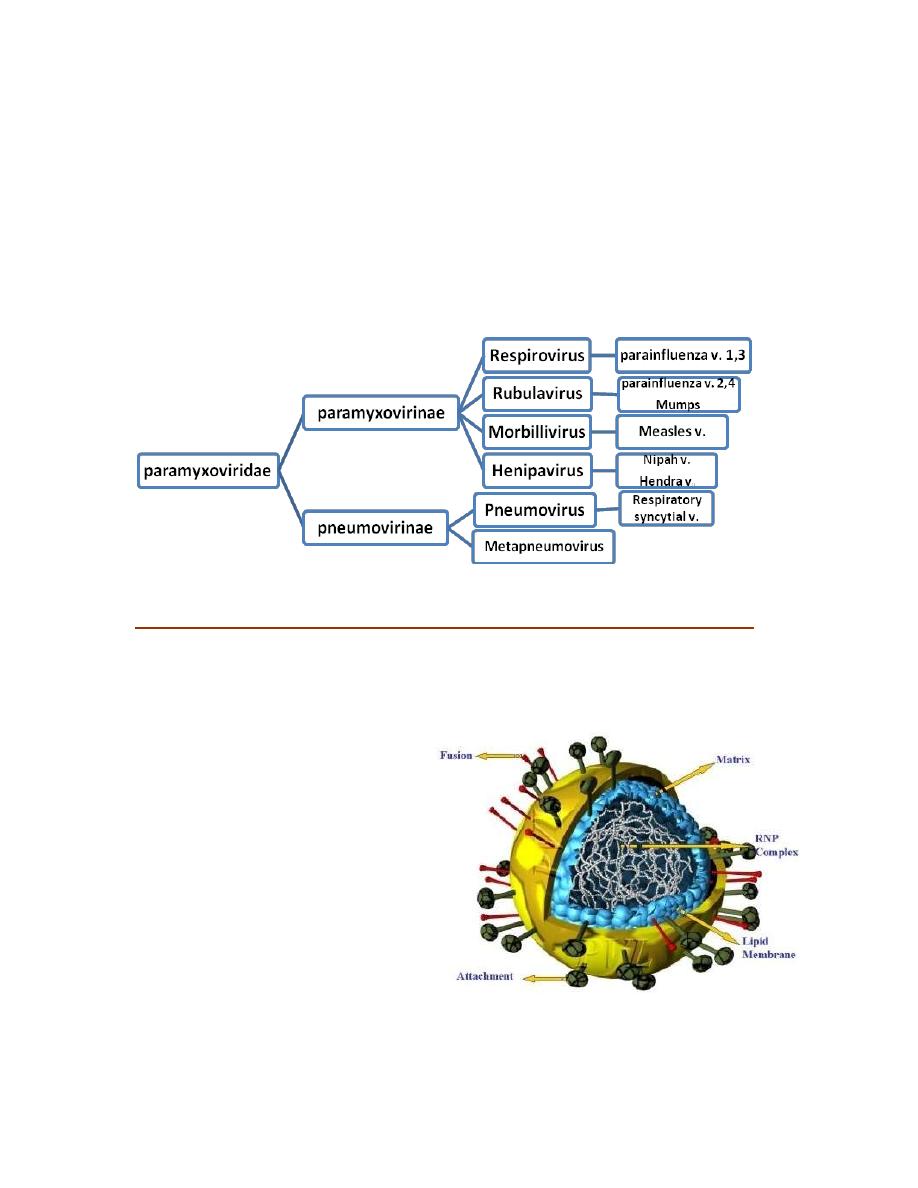
Paramyxoviruses are the major respiratory pathogens in children under 5 years of age;
this family is classified into 2 subfamilies
All members of the Paramyxoviridae family initiate infection via the respiratory tract.
Replication of the respiratory pathogens is limited to the respiratory epithelia
(Parainfluenzaviruses and RSV), whereas measles and mumps become disseminated
throughout the body and produce
generalized disease.
Morphology:
150-300 nm, enveloped
SS RNA of –ve polarity
Not segmented
6 proteins these are:
- Glycoproteins - do not form such prominent spikes as on influenza virus:
HN - haemagglutinin + neuraminidase activities;
Measles - referred to as H protein - no neuraminidase activity;
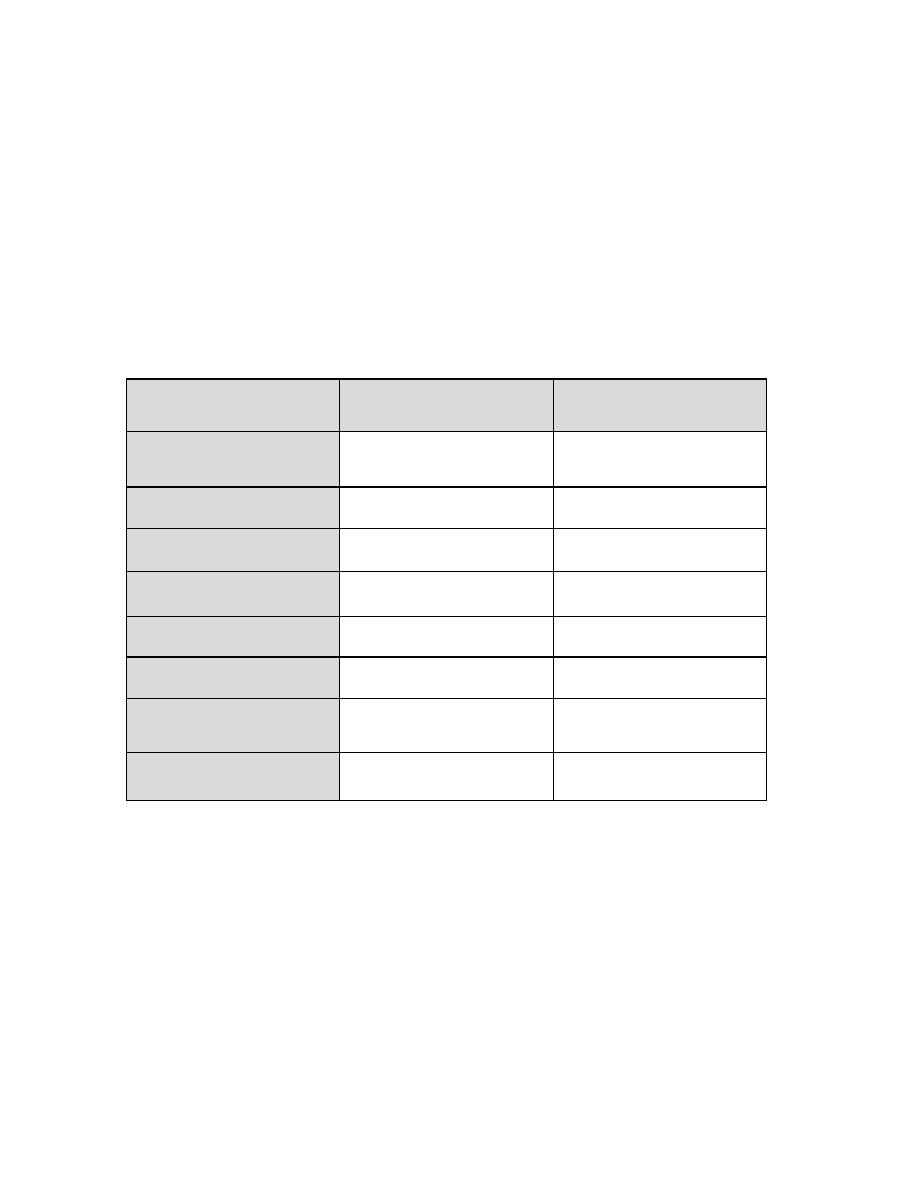
2
RSV - G protein - neither activity.
F - consists of 2 disulphide- linked subunits (F1 + F2) - responsible for cell fusion +
haemolytic function.
- Other proteins:
The M (matrix) protein lines the inner surface of the envelope.
NP - nucleoprotein.
L and P - polymerase activity
Replication occurs in the cytoplasm, excess nucleocapsid formation (inclusion bodies),
Syncytium formation is quite common (F- glycoprotein).
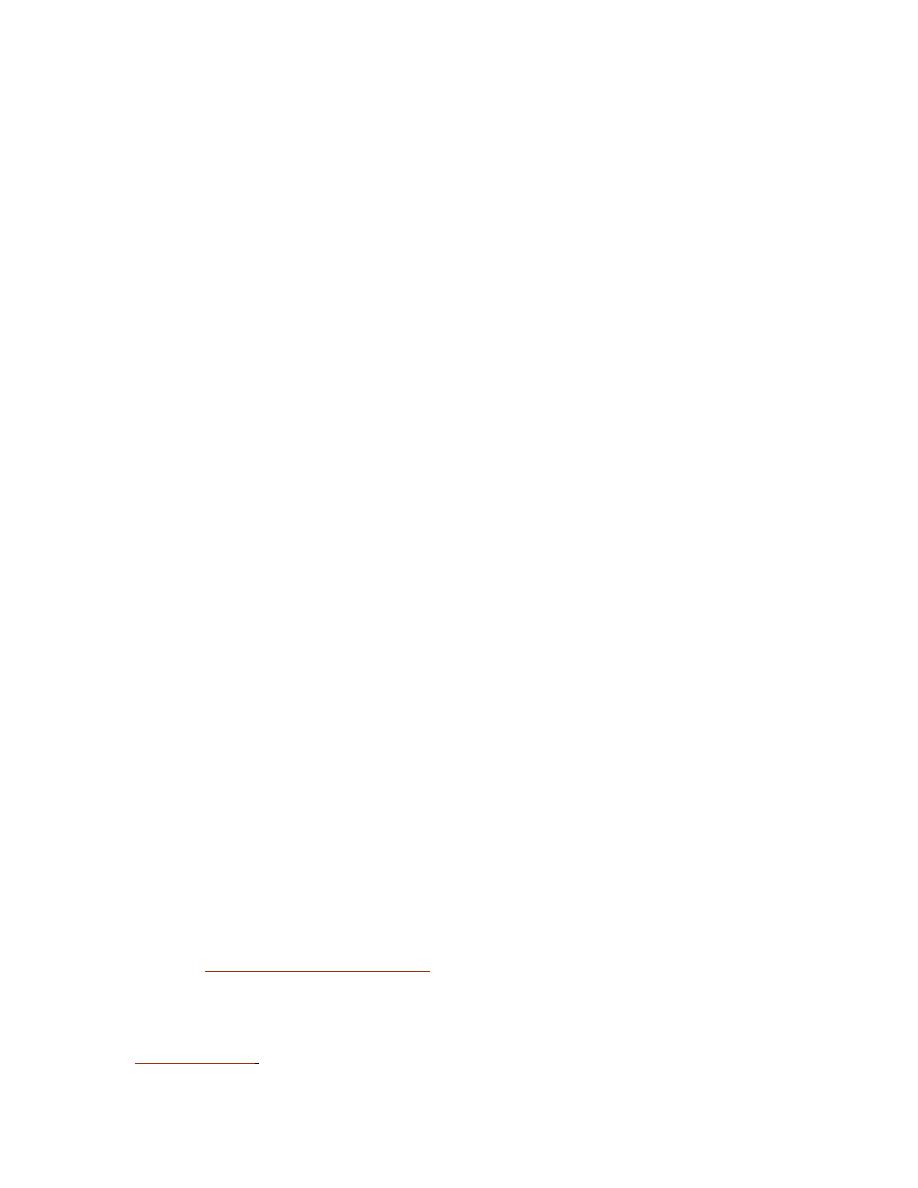
Differences between Orthomyxoviruses & Paramyxoviruses
Property
Orthomyxoviruses
Paramyxoviruses
Diseases caused in
humans
Influenza types A, B &C
Parainfluenza 1-4, RSV,
Mumps &Measles
Genome
Ss RNA, segmented
(8 pieces)
Ss RNA in a single piece
Inner ribonucleoprot.
helix
9 nm in dia.
18 nm in dia.
RNA in nucleocapsid
RNase-sensitive
RNase-resistant
Fusion of virus with cell
Endosome
Plas ma me mbrane
Transcription of viral
RNA
Host cell nucleus
Host cell cytoplasm
Genetic reassortment
Frequent
Rare
Rate of antigenic change
High
Low
Pathogenesis:

3
Parainfluenzaviruses 1-4:
Transmitted by ae rosols (respiratory droplets); world wide, Type 3 is endemic, with
some increase during the spring, whereas types 1 and 2 tend to cause epidemics dur ing
the fall or winter, frequently on a 2-year cycle.
Virus is usually limited to U.R.T. (no viraemia).Little serological variation, therefore rare
infection in adults. Reinfections with parainfluenza viruses are common.
Factors that determine the severity of parainfluenza virus disease are unclear but include
both viral and host properties, such as:
1. Susceptibility of the protein to cleavage by different proteases,
2. Production of an appropriate protease by host cells,
3. Immune status of the patient, and
4. Airway hyper reactivity.
The production of virus-specific IgE antibodies during primary infections has been
associated with disease severity. The mechanism may involve release of mediators of
inflammation which alter airway function.
The infection is usually *subclinical, or cause **acute respiratory infections : ranging
from mild influenza- like illness or "common cold" syndrome, pharyngitis, laryngitis to
more serious otitis media, bronchitis, croup and pneumonia.
Croup (laryngotracheobronchitis) is characterized by respiratory obstruction due to
swelling of the larynx and related structures .The incubation period appears to be 5–6
days.
Parainfl.1 & 2 → croup in children below 5 years of age. Duration of parainfluenza
virus shedding is about 1 week after onset of illness; some children may excrete virus
several days prior to illness.
Parainfl. 3 → L.R.T. Infection (e.g. in very young children) lead to more serious
symptoms. Type 3 may be excreted for up to 4 weeks after onset of primary illness. This
persistent shedding from young children facilitates spread of infection. Prolonged viral
shedding may occur in children with compromised immune function and in adults with
chronic lung disease.
4
Parainfl. 4 → rare, common cold.
The most common complication of parainfluenza virus infection is otitis media.
Laboratory Diagnosis:
1. Rapid diagnosis: by antigen detection methods in exfoliated nasopharyngeal cells by
direct or indirect immunofluorescence tests.
2. Definitive diagnosis: through
a- Viral isolation from appropriate specimens or
b- Detection of viral RNA by reverse transcription-polymerase chain reaction (RT-
PCR).
Treatment & Prevention
1. Contact isolation precautions are necessary to manage nosocomial outbreaks of
parainfluenza virus.
2. Ribavirin has been used with some benefit in treatment of immunocompromised
patients
3. No vaccine is available.
RSV (Respiratory Syncytial Virus)
First isolated in 1956 and subsequently recognized as a major cause of L.R.T. disease in
infants and young children. Infects man, monkeys and some rodents with disease
production, but unapparent infections (resulting in spread of virus) may occur in many
mammals.
I.P. 4-5 days
Viral shedding may persist for 1–3 weeks from infants and
young children, whereas adults shed for only 1–2 days.
In culture, causes characteristic syncytial masses - hence the name. Highly infectious,
transmission by respiratory secretions.
Primary multiplication occurs in epithelial cells of U.R.T. producing a mild illness.
In ~50%
children less than 8 months old
, virus subsequently spreads into the L.R.T.
causing
bronchitis, pneumonia
(1/4 of cases) and
croup
(1/2 of cases). Has been
suggested as a possible factor in cot death.
In older children
→ U.R.T.infection.
5
In adult
→ common cold.
In elderly or ICP
→ pneumonia
Lab.Diagnosis
Spp.
Nasopharyngeal swab or Nasal swab.
Culture:
Hela cell (giant cell or syncytia)
Serology:
IF , ELISA, CF & NT.
Prevention
Currently no vaccine! Also, infection does not result in lasting protection therefore
repeated infections ('colds') occur throughout life.
Ribavirin (aerosol) 3- 6 days + hyperimmunoglobulin.
Mumps
Recognized by the ancient Greeks, virus first isolated in 1934.Humans are believed to be
the only natural reservoir for the virus .Trans mission via saliva and respiratory
secretions; less infectious than measles/chickenpox - more adult cases.
I.P. 18 days (7-25 days).
Typically causes painful swelling of parotid glands 16-18
days after infection. This is preceded by primary replication of the virus in epithelial cells
of the U.R.T. and local lymph nodes, spread to →distant L.N.& spleen → viraemia
→generalized spread to salivary & other glands→ other body sites.
Clinical Findings:
~1/3
rd
of cases (unapparent infection)
In children
(usually at age of 5-9 years), mumps is usually self- limited
In adults
(post-puberty) a proportion of cases have more serous sequalae:
(complications)
orchitis (20-30% of males - rarely resulting in sterility); aseptic
meningitis(10-15%), encephalitis, pancreatitis(10% of all cases), myocarditis, nephritis -
<1% adult cases.

6
Rare complications:
1. Self limited polyartheritis
2. Pancreatitis (D.M.)
3. Thyroditis
4. unilat. Nerve deafness (hearing loss)
Lab.Diagnosis
Spp.
Saliva, CSF, urine
Culture:
embryonated egg or MKC (monkey kidney cell)
Identifications:
hemadsorption inhibition, IF.
Serology:
CFT,HAI, ELISA, mumps specific IgM /IgG Abs.
Prevention:
one invariant serotype therefore vaccines are viable
*formalin- inactivated and
** Live attenuated (widely used)95% effective with 10 years protection.
Given to →over 1-year age in one dose S.C.
→ Adult Who had no previous infection.
Treatment:
none (passive immunization has been used).
