
Pathogenicity
:
Factors affecting the severity of infection depends on:
1- Host factors.
2- Parasite factors.
3- Enviromental factors.
The first step in the pathogenicity of E. histolytica infection includes
colonization of the trophozoites on intestinal mucosa.
Factors affecting colonization of the trophozoites:
1- Infective dose: Number of active trophozoites in contact with intestinal
mucosa depend on number of viable mature cysts ingested by the host.
2- Amount of food: Bulky food does not give opportunity for the parasite to be
colonize.
3- Hypermotility of bowel (stasis) give less chance for the parasite to become
in contact with mucosa, this explains the high rate of colonization in cecal
area because of reduced peristalsis.
After establishment of colonies in intestinal mucosa, the trophozoite starts to
penetrate intestinal wall.
Factors affecting invasion and destruction of intestinal wall:
1- Motility of the parasite: more active parasite give more chance for
penetration. Amoebae enter intestinal mucosa by their pseudopodial
movements which cause displacement of the cells.
2- Bacteria: number of bacteria present in the intestine enhanced enterance of
amoebae in the wall of intestine.
3- Enzymes: virulence strain of E. histolytica has the ability to secret enzymes
e.g. cytolytic enzymes which cause lysis of epithelial cells.
أ
.
صباح النجار
Lec. 2
Pathologic anatomy of intestinal amoebiasis:
The trophozoites multiply and colonize in glandular crypts of large intestine
and adher to intestinal mucosa which leads to the formation of early lesion.
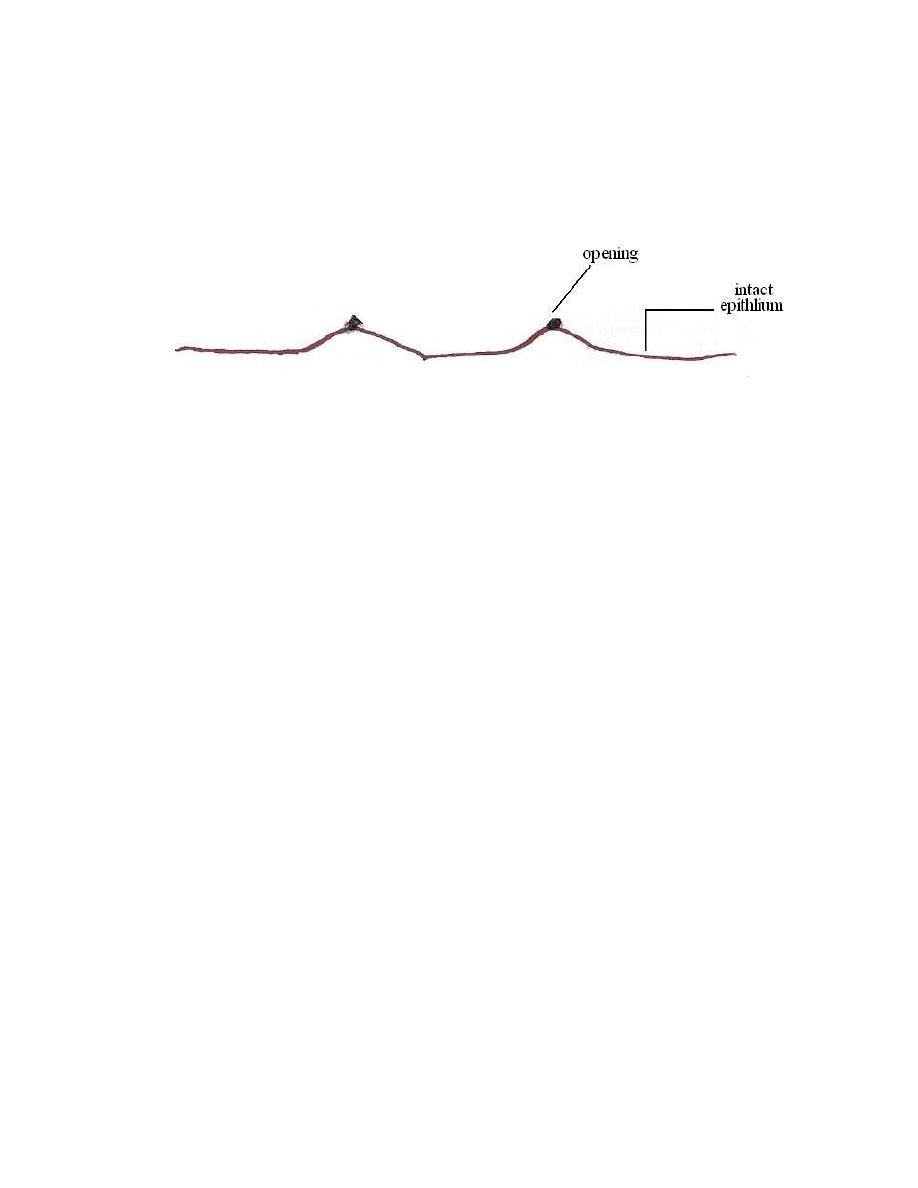
Early lesion: Nodular elevation with tiny opening
Early lesion is a tiny area of necrosis on superficial mucosa with minute entry
site and exhibiting a nodular elevation. These lesions seperated from one
another by intact epithelium.
In older lesion the amoebae assisted by bacteria may break through
muscularis mucosa infiltrated to sub-mucosa, extend laterally and leading to the
formation of
Flask- shaped ulcer
with narrow mouth and wide base. The cavity
of ulcer usually contains yellowish brown necrotic materials consisting of
cytolysed cells, mucus and dead amoebae. Living amoebae are found on
margins or pheriphery of ulcer.
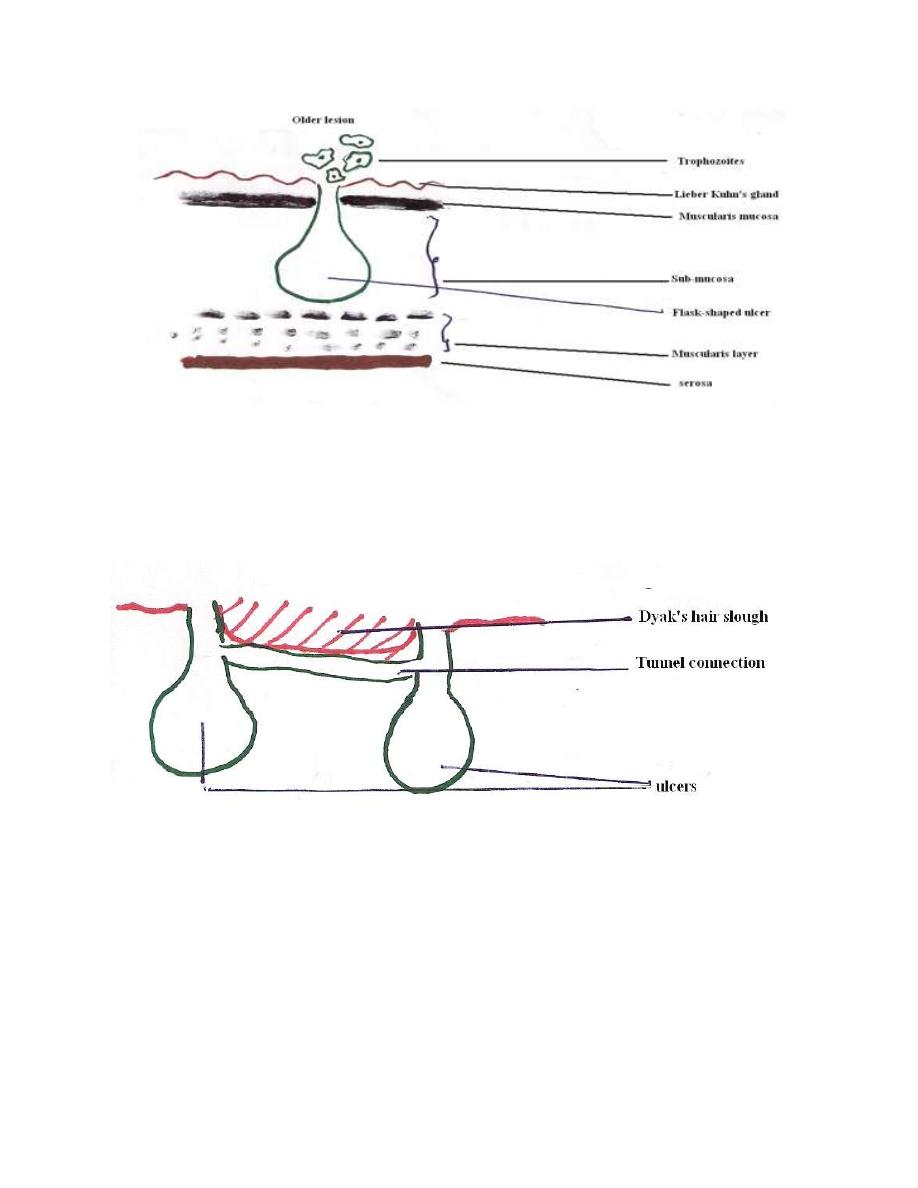
Sometime the dissolution of tissues may become so extensive resulting in a
tunneled connection which occurs between two or more lesions, which lead to
cutting off the blood supply to the overlying layers, the surface sloughs off and
this sloughed area is called Dyak's hair slough.
As a result of inflammatory process, fibrous thickening may result due to
degenerative proliferation of connective tissues which make the surface of intestine
irregular and this shape of intestine surface is called Sea Anemone ulcer.
Sometimes invasion of serosa may result by further penetration which leads to
perforation of large intestine.

Complications of Intestinal Amoebiais
1- Appendicitis.
2- Perforation.
3-Peritonitis.
3- Amoeboma or amoebic granuloma: a tumor-like mass in
the wall of intestine it is firm, nodular inflammatory
thickening around an ulcer occuring mostly in cecum and
may lead to intestinal obstruction. Amoeboma may be
confused with neoplastic growth, tuberculosis or
actinomycotic granulomas, but may be diagnosed by
biopsy, serology and response to antiamoebic treatment.
4- Extra-intestinal amoebiasis.
Extra – intestinal amoebiasis
Extra – intestinal amoebiasis is secondary to intestinal infection, this may
occurs in patients with clinical dysentery and in those with mild infections and
only trophozoites are found in infected tissues.
Usually trophozoites are disseminated by blood stream or by direct
extension from intestinal lesion or through fistula. The liver is the most frequent
involved, although the amoebae may be carried to any organ of the body.
Early amoebic infection in the liver lead to amoebic hepatitis and the patient
complain of enlarged tender liver, irregular fever, leucocytosis and disturbances of
liver function and occasional jaundice, this may give rise to amoebic liver abscess.

Amoebic liver abscess:
Amoebic liver abscess usually result by direct extension from intestinal
ulcer.or by hematogenous spread. The early liver abscess is small, oval or rounded
mass, usually solitary and occurs in right lobe of the liver. As the lesion increase in
size, the center liquefied and the wall thickened and the contents become
chocolate-brown in color resembling Ancovy Sauce.
The following three zones may be recognized grossly and under the microscope:
1- An inner necrotic center containing dead liver cells, dead amoebae mixed
with bile, fat, and RBC.
2- Median zone of connective tissue strands.
3- Outer zone of living liver cells invading by amoebae.
Amoebic lung abscess:
Pulmonary amoebiasis may usually result from direct extension of hepatic abscess
through the diaphragm and less frequently from blood stream.It is usually occurs in
right lung.
Amoebic brain abscess:
This infection rarely occurs and it is very difficult to diagnosed.
Trophozoites can reach the brain through blood stream and cause amoebic brain
abscess and amoebic meningoencephalitis.
Cutaneous amoebiasis:
Cutaneous amoebiasis is a rare reported complication of amoebic infection ,it
involve abdominal wall as aresult of syrgical interference of colostomy or amoebic
liver abscess aspirate or directly from fistulous tracts that arise from intestinal ulcer
or hepatic abscess.Also it involve anal and perianal areas by direct extention of
rectal lesion .Genetal organs may involved mainly in homosexuals.

Symptomatology
The incubation period E. histolytica varies from few days to 3 months or
even a year. The clinical symptoms are variable which depend on strain of E.
histolytica, location of amoebic infection and resistance of the host.
There are two types of infection, symptomatic and asymptomatic. The
majority of patients are asymptomatic cyst passing carrires and they are complain
of vague abdominal discomfort.Cyst pasing carriers are able to spread the parasite
to others through poor hygienic practices .
Symptomatic infection :1-Intestinal amoebiasis;
a- Acute intestinal amoebiasis: present as dysentery (blood,and mucus-
containing diarrhea) accompaned by localized abdominal pain, flatulence,
6 – 8 bowel motion per day, anemia loss of weight and low grade fever.
b- Chronic intestinal amoebiasis: with lower-grade symptoms e.g.
constipation alternating with diarrhea, anorexia, gas of abdomen, weight
loss and fatigue.
2-Extra-intestinal amoebiasis:
It depends of the type of tissue invaded by trophozoites.
Amoebic liver abscess: enlarged tender liver, irregular fever ,localized abdominal
pain(right upper quadrent), slight elevation of alkaline phosphatase.
Amoebic lung abscess: chest pain, tachycardia cough and haemoptesis and signs of
pneumonia or lung ca.
Amoebic brain abscess: signs of brain tumor or brain hydatid cyst.
Cutaneous amoebiasis:.it cause skin ulceration and if it complicated by bacterial
infection it will lead to dermatitis .
