
1
Diagnosis
Diagnosis of amoebiasis depend on:
1- Physical signs and symptoms.
2- Sigmoidoscopy or colonoscopy;is not recommended as a
routine diagnostic approuche .
Diagnosis by sigmoidoscopic image should always be supplemented by
microscopic examination of aspirated and biopsied specimens.
3- X-ray, U.S., C.T. scan and MRI are helpful methods if there is
obstruction amoeboma, perpitonitis,and
extraintestinal
infections and also to assess chemotherapy..
4- Laboratory diagnosis: either by:
a-
Direct demonstration of the parasite in stool specimen, liver abscess
aspirate, colonic biopsy and sputum by microscopic examination,
cultivation, animal inoculation and antigen detection test.
b-
Indirect demonstration of the parasite by:
1- Serological tests.
2- Blood picture.
3- Liver function test.
Methods of direct demonstration of the parasite:
1-
Stool examination:
Usually more than one specimen is recommended at 3 – 4 days intervals and
almost trophozoites are seen in liquid warm fresh stool, while cysts are seen in
formed and semi -formed stool.
General stool examination include macroscopic and microscopic examination.
ﺃ . ﺻﺒﺎﺡ ﺍﻟﻨﺠﺎﺭ
Lec. 3

2
a- Macroscopically the stool specimen in amoebic dysentery contains
exudates ,mucus and blood.
b- Microscopic examination include:
1- Direct wet smear preparation of saline and iodine solutions to look for
the trophozoites, cysts and charcot-leyden crystals.We need to
differentiate between E.histolytica and other amoebae and
macrophages.
2- Indirect concentration method by flotation or sedimentation of the cysts
in case of light infection.
3- Permenante stained smear.
Microscopic examination is unable to distinguish pathogenic E.histolytica
from morphologically identical and non pathogenic E.dispar .
Erythrophagocytic amoeba are more likely to be E. histolytica.
Microscopy is still the most widespread method of diagnosis around the
world .However is not as sensitive or accurate in diagnosis as the
other tests available.
2-
Cultivation of the parasite on specific media.
3-
Animal inoculation: experimental infections of animals to demonstrate the
parasite.
4-
Antigen detection test: it gives indication that the parasite is still present.It is
more sensitive method than microscopy and it is specific for E.histolytica
infection.This test is recently developed and include a kit that detects the
presence of amoebae proteins or DNA of amoeba in feces.These tests are not
in widespread use due to their expense.

3
Methods of indirect demonstration of the parasite:
1- Serological tests: to detect specific antibodies against E. histolytica.
Antibodies will be detectable within 5 – 7 days of acute infection and may
persist for years.
Serological tests are positive in 90 – 95% of patients with extra-intestinal
infection. Several serological tests are used e.g. Indirect haemagglutination,
ELISA and Indirect fluorecent antibody test.The levels of antibodies are much
higher in individual with liver abscess.
2- Blood picture: leukocytosis with eosinophilia is observed in 80% of cases
and mild anemia also observed.
3- Liver function test: In amoebic liver abscess, alkaline phosphatase shows
slight elevation.
Occult blood test usually positive in acute bloody diarrhia cases.
In patients with amoebic dysentery ,it is necessary to differentiate between
infectious causes including amoebiasis ,shigellosis ,campylobacter and non –
infectious causes including inflammatory bowel disease and ischemic colitis.
Parasitic causes of dysentery include E.histolytica,Balantidium coli and
Schistosoma mansoni.
4
Differential diagnosis of amoebic and bacillary dysentery:
Amoebiasis
Shigellosis
- Chronic disease may persist from 1 –
14 weeks or even years.
- Acute disease with short
incubation period
- Flask – shaped ulcer involving all
coats of intestine.
- Superficial infection with
necrosis of mucous membrane
- Stool consisting of blood, mucus and
fecal materials but with few leukocyts.
- Stool filled with cellular
exudates, numerous pus cells.
- RBCs may be agglutinated.
- RBCs not agglutinate
- Charcot – leyden crystals usually
present.
- Not present.
- E. histolytica troph. may have ingested
RBCs.
- No E. histolytica troph.
- Localized abdominal pain over cecum.
- Generalized abdominal pain.
- No fever
- Fever usually present.
- Response to antiamoebic drug.
- Response to antibiotic.
Entamoeba coli
It is non pathogenic amoebae, world widely distributed, usually the most
common amoebic parasite of man. Although it is a harmless, commensal found
in the lumen of cecum and lower levels of large intestine, its presence in the
stool of man indicates that the patient has ingested fecal contaminated food.

5
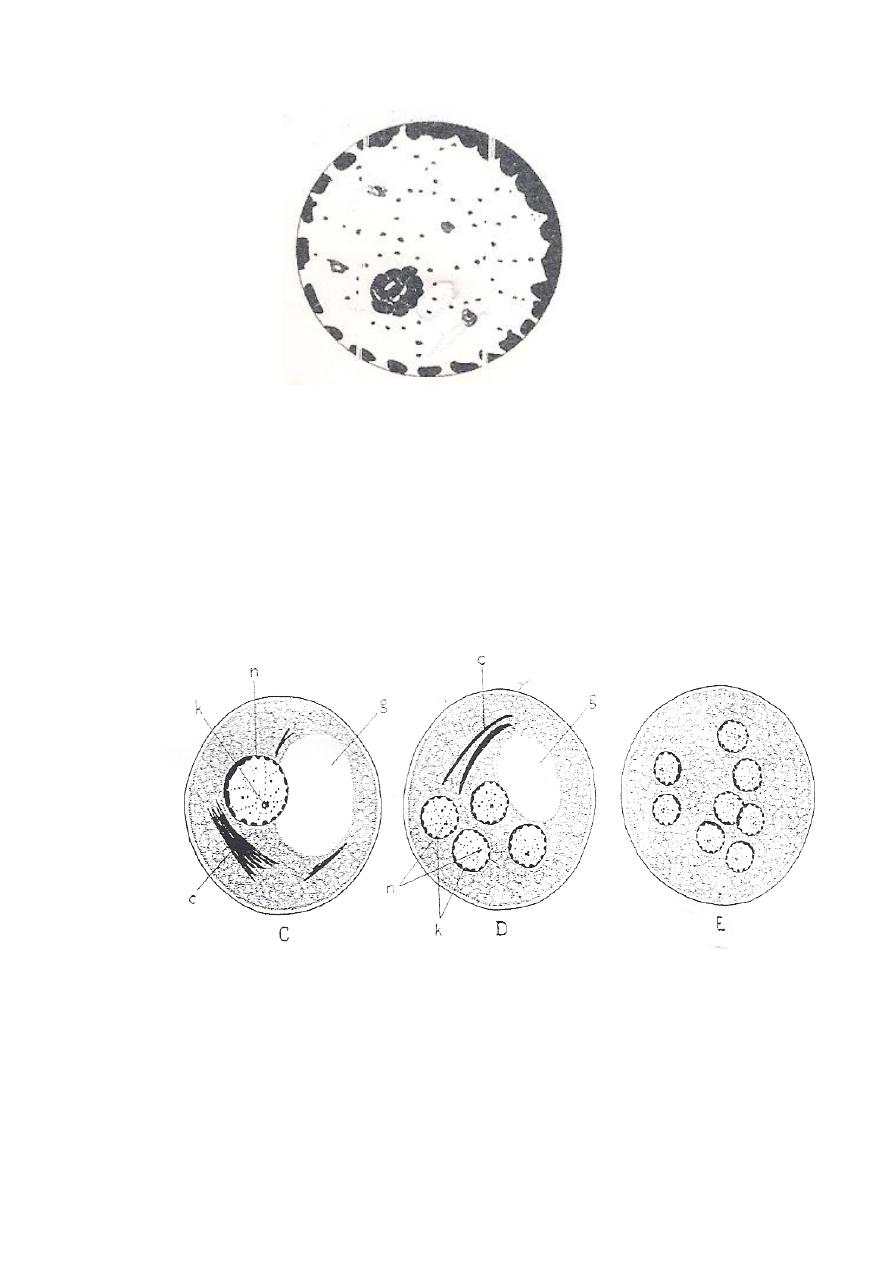
Morphology
Trophozoite: 15 - 50µ in diameter that is larger than that of E. histolytica troph.,
ectoplasm non – granular and not well differentiated from the coarsely –
granular endoplasm. Pseudopodia are short, broad and extend in different
directions.
Motility: non progressive, non directional and sluggish movement.
Within the endoplasm there are many food vacuoles containing bacteria
and food debris, but no RBCs. The trophozoite contain single nucleus which is
larger than E. histolytica nucleus, relatively with thick nuclear membrane which
is lined by irregularly distributed chromatin granules. Karyosome is eccentric
and surrounded by a halo-like capsule connected to the nuclear membrane by
thin fibrils and there is small chromatin granules scattered on these fibrils. This
type of nucleus is called coli-type nucleus.
6
Coli type nucleus
Cyst: spherical, larger than E. histolytica, when it is immature, it is usually
contain one nucleus than as it become mature it posses 8 or 16 or even 32 nuclei.
Within the cytoplasm of immature cyst there is relatively large, sharply defined
glycogen mass, this mass disappear after the maturation of the cyst.
There are numerous chromatoidal bodies, thread like or splinter – shaped
with pointed ends, usually found in bundles.
Diagnosis: by identify trophozoites or cysts by wet saline or iodine preparation,
or by demonstrate only in concentration method.
