THYROID HORMONE
s
& ANTITHYROID
DRUGS
The thyroid secretes 2 types of hormones:
1- Iodine containing amino acids (are important for growth, development and
metabolism) and these are: triodothyronine, tetraiodothyronine,( thyroxine)
2- Calcitonin is important in the regulation of calcium level.
BIOSYNTHESIS, TRANSPORT & PERIPHERAL METABOLISM OF
THYROID HORMONES:
The iodine necessary for the synthesis of T3 & T4 is derived from food or iodine
supplement. Iodine uptake is an active process. Once taken up by the thyroid gland,
iodine undergoes a series of enzymatic reactions that convert it into active
hormone.
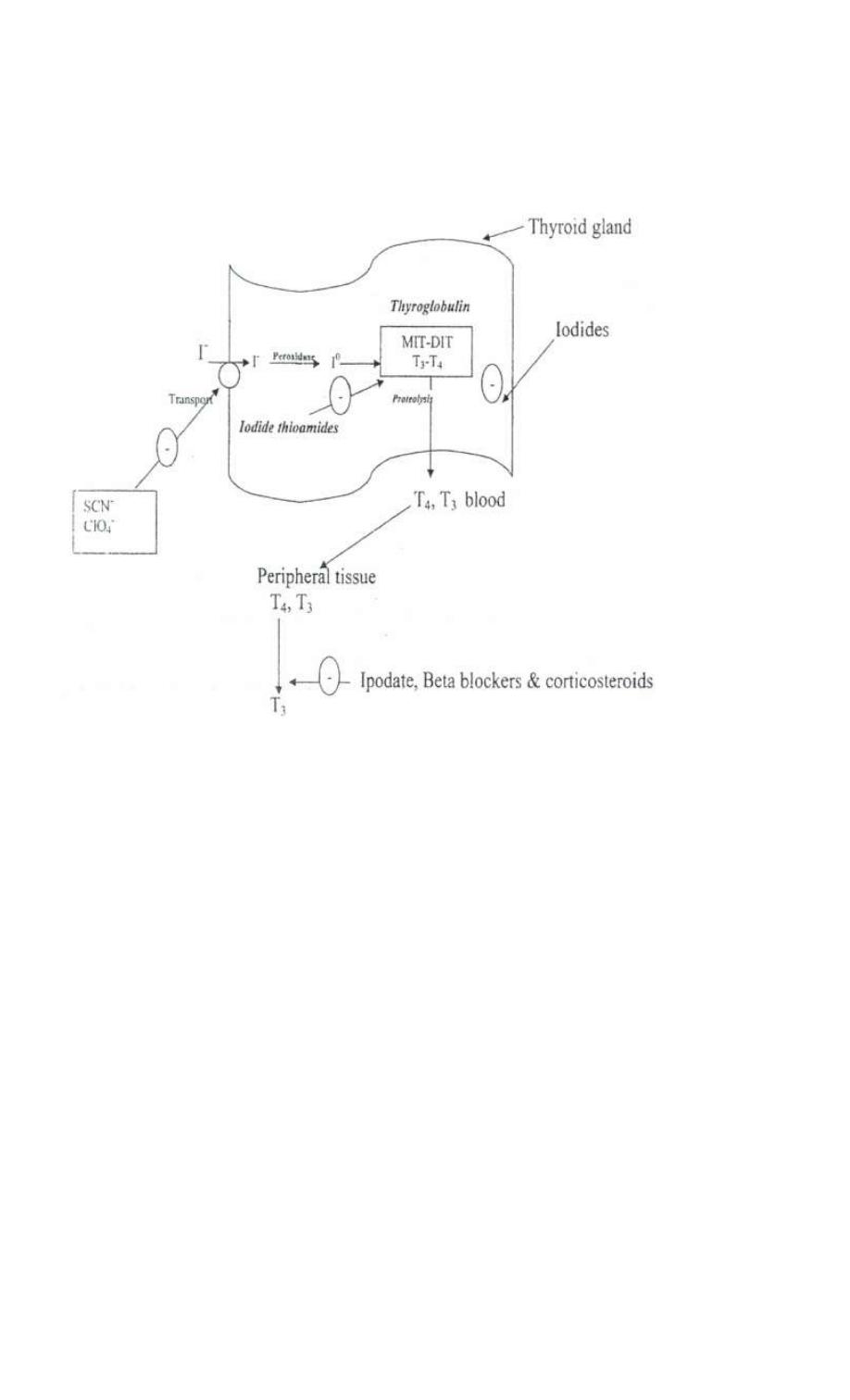
1- The 1st step is the transport of the iodine into the gland by intrinsic follicle cell
basement membrane protein called sodiurn/iodine symporter(NIS). This step is
inhibited by SCN & CLO
4
-
2- Iodide is oxidized by thyroid peroxidase to iodine.
3- Iodination of tyrosine residues within the thyroglobulin molecule to form
monoiodotyrosine (MIT) & diodotyrosine (DIT) this process is called iodide
organifaction. Thyroidal peroxidase is transiently blocked by high levels of
intrathyroidal iodide & thioamide drugs.
4- Two molecules of DIT combine within the thyroglobulinto form L-thyroxine (T4)'
One molecule of MIT & one molecule of DIT combine to form T3
5- T4, T3, MIT & DIT are released form thyroglobulin by exocytosis & proteolysis of
thyroglobulin. The DIT & MIT are deiodinated within the gland & the iodine is
reutilized. This process of proteolysis is blocked by high levels of intrathyroidal
iodide.
The ratio of T4 to T3 within the thyroglobulin is 5:1 so that most of the hormone
released is thyroxine. Most of circulating T3 in the blood is derived from
peripheral metabolism of thyroxine.

TRANSPORT
T3 & T4 in the plasma are reversibly bound to thyroxine binding globulin (TBG) a
transport protein in the blood.
PERIPHERAL METABOLISM
The primary pathway of peripheral metabolism is deiodination. Deiodination of T4 may
occur by monoiodination of the outer ring producing 3,5,3 triiodothyronine (T3).
Alternatively deiodination of the inner ring produces 3,3,5 triiodothyronine (reverse T3
or rT3) which is inactive.
Drugs such as ipodate, beta-blockers & corticosteroids and severe illness or starvation
inhibit the 5-deiodinase necessary for the conversion of T4 to T3 resulting in low T3 &
high rT3.
CONTROL OF THYROID FUNCTION
Hypothalamic cells secrete thyrotrooin releasing hormone (TRH) into the
capillaries of the pituitary portal system. TRH stimulates the synthesis & release of
thyroid stimulating hormone (TSH). TSH stimulates an adenylyl cyclase-mediated
mechanism in the thyroid gland to increase the synthesis& release of T4 & T3·
T4 & T3 act in a negative feedback fashion (mechanism) to block the action of
TRH on the pituitary gland & on the hypothalamus to inhibit the synthesis &
release of TRH. In Grave's disease; lymphocytes secrete a TSH receptor
stimulating Ab which binds to the TSH receptor.
The thyroid gland also regulates its uptake of iodide & thyroid hormone synthesis
by intrathyroidal mechanism that are independent of TSH. These mechanisms
primarily related to the level of iodine in the blood. High concentration of iodide
inhibits iodide organification, and effect that is useful in the treatment of thyroid
disease. Inadequate iodine intake results in diffuse enlargement of the thyroid
(Goitre)
MECHANISMS OF ACTION OF T4 & T3
T3 is 10 times more potent than T4 and since T4 is converted to T3 in target cells( the
liver & kidneys), most of the effect of circulating T4 is probably due to T3.
Thyroid hormone binds to receptors in the nucleus that control the expression of genes
responsible for many metabolic processes. These receptors when activated by T3 bind to
DNA response elements & control synthesis of RNA which codes for specific proteins
that mediate the action of thyroid hormones.
The proteins synthesized differ depending on the tissue involved. These proteins include
Na+/K+ ATPase, specific contractile protein in smooth muscles & the heart, enzymes
involved in lipid metabolism, important developmental components in the brain .... Etc.
EFFECTS OF THYROID HORMONE
Include normal growth & development of the nervous, skeletal, reproductive
systems & control of metabolism of fat, CHO, proteins & also metabolism of
drugs.
Thyroid deprivation in early life results in irreversible mental retardation &
dwarfism (congenital cretinism), thyroid hyperactivity results in thyrotoxicosis.
Conversely a decrease in thyroid activity results in hypothyroidism (myxedema).
PHARMACOKINETICS
All of the naturally occurring T4 & T3 exist in Levo form (L-isomers}, the Dextro
form of Thyroxine has only 4% of the biological activity of the L-isomer.
Thyroxine is well absorbed from the duodenum & ileum when taken orally; oral
bioavailability of L- Thyroxine is about 80% absorbed while T3 is almost
completely absorbed. T4 & T3 can also be given intravenously.
In patients with hyperthyroidism, the clearance of T4 & T3 is & the opposite is
true in hypothyroidism. Drugs that induce hepatic microsomal enzymes (e.g.
rifampicin phenytoin & Phenobarbital} the metabolism of T4 & T3 & patients
receiving T4 replacement therapy may require modification ( dosage) to
maintain clinical effectiveness.
If TBC binding sites are increased (this is caused by pregnancy, estrogens, oral
contraceptives) there is an initial shift of the hormone from the free to the bond
state & α in the rate of elimination until the normal hormone concentration is
restored thus the total & bound hormone will increase but the concentration of free
hormone will remain normal. The reverse occurs when TBG sites are
THYROID PREPARATION
These preparations are synthetic
1. Levothyroxine (is the best which is T4).
2. Liothyronine (T3, is faster acting but has shorter half-life & more expensive).
3. Liotrix (is a mixture of Thyroxine & liothyronine. It is never required).
ANTI- THYROID DRUGS
Reduction of thyroid & hormone effects can be accomplished by agents that
interfere with the production of thyroid hormones, by agents that modify the tissue
response to thyroid hormones or by glandular destruction with radiation or
surgery. The anti-thyroid compounds used clinically include the thioamides,
iodides & radioactive iodine.
THIOAMIDES
Methimazole (carbimazole) Propyl thiouracil (PTU)
These 2 are the major drugs used in the treatment of thyrotoxicosis {Carbimazoles
converted to methimazole in vivo).
The most important effect of these drugs is to block iodination of tyrosine. Also
these drugs may block the coupling of DIT & MIT.
These drugs are given by oral route. Since the synthesis of thyroid hormones rather
than release is inhibited, the onset of activity of these drudges is usually slow
requiring 3-4 weeks for full effect.
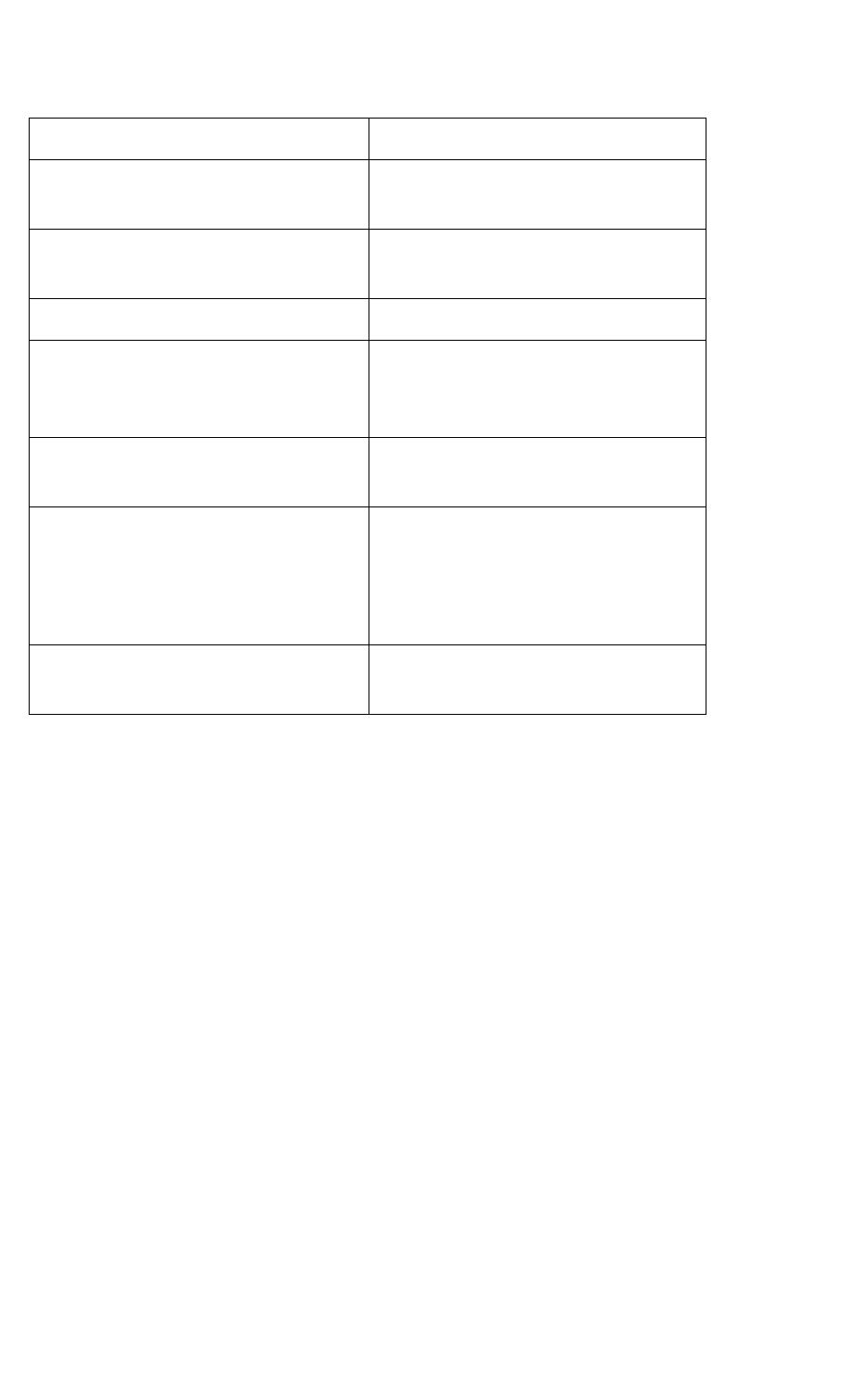
Carbimazole
Propyl thiouracil ( PTU)
1- More potent given in a single daily
Does is 10 times that of Carbimazole
dose.
given every 6-8 hrs.
2-Completely absorbed & readily
Rapidly absorbed with a bioavailability
accumulated in thyroid gland.
of50-80 %
3-Excreted in urine but slower than PTU. Excreted in urine within 24 hrs
4-Has some immunosuppressive action
leading to decrease in serum TSH
No such effect
receptor antibodies.
5-Has little effect on conversion of T4 to It inhibits the peripheral conversion of T4
T3·
to T3•
6-Crosses placenta.
Crosses placenta less readily Preferable
in pregnancy
7-Sufficient quantity is excreted in breast Not excreted in sufficient quantities to
milk.
preclude breast feeding.
ADVERSE EFFECTS OF THIOAMIDES occur in 3-12% of treated patients.
Most reactions occur early. The most common adverse effect is maculopapular pruritic
rash, sometimes accompanied by fever.
RARE ADVERSE EFFECTS INCLUDE:
1. Urticarial rash.
2. Vasculitis.
3. Arthralgia.
4. A lupus like reaction
5. Cholestatic jaundice.
6. Lymphadenopathy.
7. Hyperprothrombinemia, aplastic anemia & aqranutocytosis the most dangerous
complication)
8. All these adverse effects are reversible.

IODIDE SALTS AND IODINE:
Iodide salts inhibit. organification (iodination of tyrosine) and thyroid hormone
release. These salts also decrease the size & vascularity of the hyperplastic:
thyroid gland. Since iodide salts inhibit the release as well as the synthesis of the
hormone, their onset of action occurs rapidly within 2-7 days. However the
effect is transient because the thyroid gland escapes from iodide block after
several weeks of treatment.
Iodide salts are used in thyroid storm(severe thyrotoxicosis) & to prepare the
patient for surgical resections of the hyperactive thyroid. The usual forms of this
drug are lugol's solution(iodine & potassium iodide) and saturated solution of
potassium iodide.
IODINATED CONTRAST MEDIA (IPODATE):
It suppresses the conversion of T4 to T3 via 5 deiodinase in the liver, kidney and
other peripheral tissues. Inhibition of hormone release from thyroid gland may
also play a part.
Ipodate has proved very useful in rapidly reducing T3 concentration in
thyrotoxicosis (in thyroid storm)
RADIOACTIVE IODINE 1
st
(ADMINSITERED ORALLY)
It is taken up & concentrated in the thyroid gland. A dose large enough to
severely damage the gland can be given without endangering other tissues .
An effective dose of. I
131
(single) can produce permanent cure of thyrotoxicosis
without surgery. I
131
shouldn't be used in pregnancy or nursing mother.
β-blockers:
Propranolol is used as an effective therapeutic adjuvant in the management of
thyrotoxicosis. Since many of these symptoms mimic these associated with
sympathetic stimulation (particularly tachycardia) propranolol ilnhibits 5- deiodinase
(the conversion of T4 to T3).